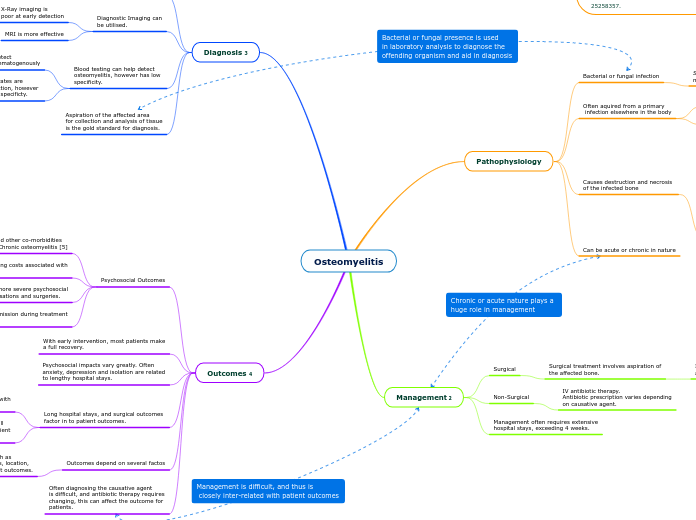
Osteomyelitis
Pathophysiology
Bacterial or fungal infection
Staphylococcus Aureus is the
most common causative agent (70%) 1
Often aquired from a primary
infection elsewhere in the body
Hematogenous spread
Spread directly from open wound
Causes destruction and necrosis
of the infected bone
Can be acute or chronic in nature
Management 2
Surgical
Surgical treatment involves aspiration of
the affected bone.
Includes removal of dead tissue, purulent matter
and amputation.
Non-Surgical
IV antibiotic therapy.
Antibiotic prescription varies depending
on causative agent.
Management often requires extensive
hospital stays, exceeding 4 weeks.
Diagnosis 3
Diagnosis is complex
often requires several
diagnostic procedures
Patient presentation plays a huge
role in diagnosis.
Fever, local pain and refusal
to use affected limb are all
common presentations.
Diagnostic Imaging can
be utilised.
X-Ray imaging is
poor at early detection
MRI is more effective
Blood testing can help detect
osteomyelitis, however has low
specificity.
Blood culture is can detect
pathogens if spread hematogenously
ESR and CPR rates are
useful in detection, however
they have low specificty.
Aspiration of the affected area
for collection and analysis of tissue
is the gold standard for diagnosis.
Outcomes 4
Psychosocial Outcomes
Increased levels of depression and other co-morbidities
are associated with diagnosis of Chronic osteomyelitis [5]
Early detection is key in minimising costs associated with
treatment
Chronic Osteomyelitis has a more severe psychosocial
impact with multiple hospitalisations and surgeries.
Cost of hospital admission during treatment
is significant.
With early intervention, most patients make
a full recovery.
Psychosocial impacts vary greatly. Often
anxiety, depression and isolation are related
to lengthy hospital stays.
Long hospital stays, and surgical outcomes
factor in to patient outcomes.
Surgical intervention is associated with
poor outcomes and recovery.
If amputation is required this will
have a significant impact on patient
quality of life.
Outcomes depend on several factos
Predisposing factors such as
diabetes, early diagnosis, location,
early intervention impact outcomes.
Often diagnosing the causative agent
is difficult, and antibiotic therapy requires
changing, this can affect the outcome for
patients.