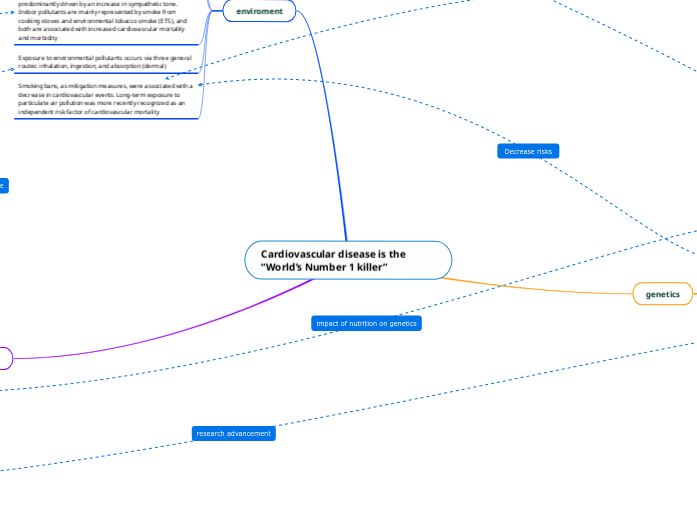
Cardiovascular disease is the “World’s Number 1 killer”
genetics
when discussing CV, Adaptive genetic variations interacting with environment modulate disease susceptibility but the level to which those variants contribute to dyslipidemia and obesity and how environmental factors, especially diet, alter the genetic association is not yet completely known. (
An important area of research in this topic is to identify genetic targets for the purpose of personalized medicine and personalized nutrition. The interaction between dietary habits and genes is extremely complex and can go both ways: Specific genetic characteristics can influence the effect of the diet on biochemical or anthropometrical characteristics (nutrigenetics); however, what we eat may also have an impact on gene expression (nutrigenomics)
All smoking measures showed significant associations with 3 major atherosclerotic diseases, with the strongest effect size for incident PAD. The risk due to smoking lasted up to 30 years for PAD and 20 years for CHD
Advances in technology, such as the development of ‘gene chips’ may allow us to study 100 000 genes at a time on a single chip. Such advances will amplify the power available to us in the realms of research into genetic physiology and interaction with environmental stimuli. The insights that these novel approaches may yield are eagerly awaited.
We know that this is not the case. For example, some individuals exposed to cigarette smoke with an otherwise identical risk factor profile will go on to develop CHD, whilst others will not. Therefore, the well accepted view is that CHD is a multifactorial disorder, with both environmental and genetic factors contributing. (environment)
enviroment
High contemporary risk of CVD may also be due to a mismatch between ancient human genes and current human environments. This mismatch may be because rapid changes in human environments have outpaced genetic adaptation. Ancestral alleles adapted to ancient environments have become maladapted to modern environments therefore confer disease risk.
Long-term exposure to natural environments, such as residing in areas with high greenness or in diverse landscapes, has been associated to reduced all-cause, respiratory, cardiovascular and cancer mortality4,21 and to improved respiratory and mental health.
Air temperature has a strong influence on cardiovascular mortality characterized by a V-like relationship confirming that both cold and hot periods have negative cardiovascular impacts. Cardiovascular reactions to air temperature are predominantly driven by an increase in sympathetic tone. Indoor pollutants are mainly represented by smoke from cooking stoves and environmental tobacco smoke (ETS), and both are associated with increased cardiovascular mortality and morbidity
Exposure to environmental pollutants occurs via three general routes: inhalation, ingestion, and absorption (dermal)
Smoking bans, as mitigation measures, were associated with a decrease in cardiovascular events. Long-term exposure to particulate air pollution was more recently recognized as an independent risk factor of cardiovascular mortality
health and lifestyle
Over the past 5 decades, a substantial accumulation of epidemiological and experimental data has established a causal relationship between low levels of occupational and/or leisure-time and an increased risk of CVD.
All smoking measures showed significant associations with 3 major atherosclerotic diseases, with the strongest effect size for incident PAD. The risk due to smoking lasted up to 30 years for PAD and 20 years for CHD
Prolonged TV viewing and total screen time during leisure time in adolescence, and increases in these behaviours, are associated with unfavourable levels of several cardiovascular risk factors in young adulthood.
The Mediterranean diet (fish, monounsaturated fats from olive oil, fruits, vegetables, whole grains, legumes/nuts, and moderate alcohol consumption) has been shown to reduce the burden, or even prevent the development, of cardiovascular disease, breast cancer, depression, colorectal cancer, diabetes, obesity, asthma, erectile dysfunction, and cognitive decline. (nutrigenetics)
Further understanding of specific pathophysiological pathways linking sleep disorders to cardiovascular disease is important for developing therapeutic strategies and may have important implications for cardiovascular chronotherapeutics.