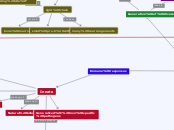
Immune responses
Innate
Phagocytes
Natural killer
Generalized, non specific pathogens
inflammation
Swelling
Heat
pain
redness
consists of Pathogen
recognition receptors
-membrane bound signaling receptors
-membrane bound phagocytic receptors
-cytotoxic signaling receptors
-free receptors
compliment cacase
(3 pathways)
Lectin Pathway
C4b2a
Mannose binding lectin
C4b2a3b
Alternative pathway
C3b from other pathways
C3bBb3b
C3bBb
Classical pathway
C1
Adaptive
Lymphocytes
B lymphocytes
Bone marrow
Activation Of B-cell
Plasma cell
Memory B cell
affinity maturation
germinal center
Centrocytes
centroblasts
somatic hypermutation
point mutation
FDC's --> better selection
isotype switching
T cell
Positively selected B cell
negatively selected B cell
APOPTOSIS
affinity for antigen
T cell help
B cell cross linking
plasma cells or memory cells
cross-link antigen
CR2
B cell
CD3 on antigen
MHC class II
alpha 1
T cell
CD40
beta 1
more than 10 AA
MHC class I
alpha 1 and 2
T lymphocytes
(activate B cells)
Memory cells
cytotoxic T cells
Helper cells
Thymus
APC
dendritic cell, macrophage
present antigen
Clonal expansion
activation
MHC:TCR
survival
CD28:B7
differentiation
cytokines
TYPES of what cell can turn into
TReg
inhibits immature DCs
TFH
aid in isotype
switching of B cells
TH17
enhance neutrophil response
TH2
parasitic/allergies
help B cells produce Ab
CD8 cyto t cells
kill infected cells
ways to activate CD8
cytotoxic T cells
CD4 T cell
IL-2
CD8 proliferation
CD4 T cell
ADC
B7 & IL-2
Dendritic Cell
B7--> activate CD8
TH1
activate macrophages
help B cells produce Ab
Lymphoid tissues
T cell trafficking
(4 steps)
Rolling
selection
L selection
adhesion
integrins
LFA-1
activation
chemokine
CCL21
diapedesis
chemokines
CCL21 & CXCL12
ACTIVATION of T cell
need inflammatory response
activate Macrophage
and dendritic cells
Process MHC class II
2ndary lymphoid tissue
CD4 T cells
CD40L:CD40
CD28:B7
IL-2 binds to IL-2R
Proliferation
antibodies
bone marrow
Generation of diversity
B cell development
heavy chain
2 (4 if counting DJ and VD seperate)
bone marrow
Lambda5, VproB
early pre B to large pre B cell
Large preB--is chain functional?
light chain
bone marrow
small pre-b cell stage
many rearrangements
Immature B: do heavy/light chain produce functional binding site?
T cell development
Beta chain
DN2
pTalpha
thymus
2 on each chromosome
alpha chain
thymus
DN4--> DP
rearrange many times
selection process
T cell development
Positive selection
occurs in thymus
Recognize self MHC
Lives
dies
negative selection
receptor editing
thymus, DC, Macrophages
MHC present self antigen
dies
lives
B cell development
Positive selection
2ndary lymphoid organ
B cell follice
FDCs
postitive life signal;
otherwise die in 3 days
immature to mature B cell
no receptor editing
negative selection
if responds to self cells: either apoptosis or receptor editing
immature B cell
bone marrow
any cell in bone marrow
Naive T cell---> CD8 T cell killing virally infected cells
Naive T cell interacts with DC presenting its specific antigen
plc-gamma cleaves PIP2 to DAG and IP3
DAG:
activated protein kinase C
activates NFkappaB
changes pattern of gene expression
CELL DIVISION, PROLIF., DIFFERENTIATION TO EFFECTOR T CELLS
activates RasGRP, activates MAP kinase cascade
RAS-induced kinase induces and activates Fos
IP3
ip3 increases Ca2+-->activates calcineurin
NFAT activated
complement pathway
fixation of complement
C3 cleaved to produce a large C3b and small C3a fragments
C3b is reactive and becomes attached to pathogen surface (thioester bond), marking the pathogen as dangerous
C3a recruits phagocytic cells to site of infection
Alternative pathway
C3 is hydrolyzed which activates C3 and binds factor B. Cleavage of B by serine protease factor D produces a soluble C3 convertase called IC3Bb
iC3Bb activates C3 molecules by cleavage into C3b and C3a. C3b can become attached to microbial surface
Properdin (factor P) binds to C3bB to extend its lifetime on microbial surface
Factor H binds to C3b and changes conformation to cleavage by factor I
iC3b fragment of C3 remains attached to the pathogen surface but cannot form a c3 convertase
recruitment of inflammatory cells
DAF and MAP distrust C3 convertase C3bBb on human cell surface. causes C3b to dissociate and leads to inactivation
C5 activation by C5 convertase
C3b2Bb on pathogen surface, C5 binds to C3b component and is cleaved into C5a and C5b fragments.
C5b initiates the assembly of terminal complement to form membrane-attack complex
C5b, C6, C7 bind to pathogen surface. C8 and C7 undergo conformational change to expose hydrophobic sites...insert into membrane
induces polymerization of C9 to generate transmembrane channel
RLR/interferon pathway
recognition of viral nucleic acid by RIG-1-like receptors (RLR) initiate inflammatory response
viral replication in cytoplasm produces uncapped RNA with a 5' triphosphate
RLR binding to viral RNA induces association with MAVs and dimerization
One site on MAVs engages TRAF6 which leads to activation of IRF3 and secretion of type 1 interferon.
Type 1 interferons (INFalpha and INFbeta) cause interferon response
3 major functions.
1. induce resistance to viral replication in all cells
2. increase expression of ligands for receptors on NK cells
3. Activate NK cells to kill virus-infected cells
FADD/TRADD activate NFkappaB
NFkappa B causes synthesis and secretion of inflammatory cytokines
Heavy chain/light chain rearragnemtn
Generation of junctional diversity during gene rearrangement:
1. Generation of junctional diversity
2. RAG complex cleaves the heptamer RSS from D and J segments to yield DNA hairpins
3. RAG complex opens hairpins by nicking one strand of DNA, generating palindromic P-nucleotides
4. N-nucleotide additions by TdT
5. Pairing of strands
6. Unpaired nucleotides are removed by exonuclease
7. Gaps are filled by DNA synthesis and ligation to form coding joint
Heavy chain rearranges first
productive
There is always a leader and a transcription start site
One of the J’s rearranges to one of the Ds anything between that DNA rearrangement gets lost.
Vh, Vh, Vh, Vh, Dh, Dh, Dh, Dh, Jh, Jh,
One the Ds can bind to the Vh variable too but everything between gets cut out
not always productive
• Reading frame is not always correct
• Unproductive rearrangement (wrong)
• Productive rearrangement (right)→H chain protein
Naive Immature B cell
bloodstream
lymph nodes HEV L selection (b-cell)
primary follicle of B cell region (FDC)
secrete CXCL13 (B cells move to FDCs)
FDC b-cell interaction
FDCs bind to LT produced by B cells to produce B-Aff
maturation and survival B cells (IgM/IgD)
encounters Ag away from FDC then Ag has C36 on surface
encounters Ag on FDC
start of process B cell activation
coreceptor Cd8+, CD19, CR2
CR2 binds iC3b
CD19 activated
CD19 phosphorylated by SYK
signal
BCR multiple receptor complex Igalpha and Igbeta and tryp
SYK binds adjacent IgB
signal
antigen activated B cell
Move to B-T cell margin due to production of CCL219 by TFH bind CCR7
B cell internalize Ag through RME process and present peptide on MHC class II
Activated TFH
TFH more CD40 binds to CD40 on B cell
LFA-1 on TFA bind ICAM-1 on B cell
synapse forms conjugate pair
END
B lymphocyte development
in bone marrow, stroll cells interact with very early B cells (homatopoietic stem cells that turn into B or T lymphocytes)
Early pro-B then D-->J rearrangement due to Pax5...heavy chain always rearrange first
TDT expressed.
After D-->J then V-->DJ
apoptosis
large pre-B cell stage
lambda5 PreV
Mu combining with surrogate light chain and IgBeta/IgAlpha
signal sent that results in positive selection...survival
Rag1 and Rag2 stop being produced
proliferation/cell division
pre B cell stage and get light chain rearrangement starting...RAG1 and 2 expressed
apoptosis
production of IgM to surface by Igalpha and beta
sends signal to survive and RAG 1 and 2 not expressed
immature B lymphocyte
T lymphocyte development
derive from Bm and must undergo gene rearrangement to produce antigen receptors
T cells go to thymus from BM before rearrange t-cell receptor genes
gene rearrangment: one alphabet and one lambda:gamma receptor
Driven by Notch1
induces protease to cleave intracellular domain/release from plasma membrane. translocated to nucleus and turn on expression of genes for T cell development by removing repressive transcription factors
IL-7 receptor
double negative thymocyte (no CD4 OR CD8)
Notch1 rearrangement
rearrange Beta, gamma, delta
first allele, then second...still not productive then no further rearrangements
pre-T cell receptor (forms complex with CD3)
CD3 sends signals for proliferation (RAG 1 AND 2)
alpha chain rearrangement (gamma, delta)
Alpha:beta TCR--> MHC and self peptides
more alpha rearrangement if possible free Vs and Js still availalbe
apoptosis
back to MHC and self peptides
strong binding/moderate binding (best)
dendritic cells expressing AIRE (which turns on tissue specific genes) and macrophages
test for tissue specific self-peptides
lives
cell dies
Primary Response B cell
Cognate pair or conjugate pair (B-T cell margin to medullary cords)
B-cell and TFH cell
MHC class II and antigen peptide
TCR complex
CD40L gets expressed on TFH and CD40L goes to CD40 on B cell
LFA-1 and ICAM synapse
TFH cytokines and cytokine receptors on B cells
Proliferation and differentiation of B cells then to either plasma, memory cells or migrate to 2ndary follicle in B cell zone
Plasma cells: IL59, IL-6 come from TFH BLIMP-1-bell to stay in lymph node or bone marrow to plasma
Migrate to 2ndary follicle
proliferation of B cells
centroblasts rapidly divide
somatic hypermutation and isotope switching (AID) associated with dark zone of germinal center
centroblasts-->centrocytes in light zone along with FDC
these 2 interact due to AG on extension of FDC and BCR...affinity maturation occurring
competition between centrocytes to bind to antigen on FDCs...ones able to bind have highest affinity
BCR bind to antigen?
Apoptosis
internalizes receptor mediated endocytosis
processing and presentation of MHC class II
move to T cell area, interacts with TFH cells (same as above with CD40 etc.)
signals for survival for
1. return to GC
2. plasma cell using IL-10 to alumina propria, medulla cords or bone marrow
3. IL-4 to memory cell
can also bind to self antigen
energy and possible apoptosis
B7-CD28 monovalent binding of BCR
Naïve B cells→ travel to lymph node→Find TFH cell also specific for pathogen→BINDING HAPPENS BETWEEN MHC/TCR, B7/CD28, MHC/CD4) cognate pair B + T cells (medullary cords) → proliferate→ moves from medullary cords to B cell region→ TFH and B cell disconnect→ Centroblasts (isotype switching, somatic hypermutation, Ig poor on surface→ proliferate→ centrocytes→ competing for AG sites on FDCs (to increase infinity for antigen)
Leave the germinal center to find TFH again with all the receptors again mhc and tcr→cognate pair again→ cytokine signals to either go to memory cells (IL-4), plasma cells (IL-10) or back to centroblasts.
FC receptors
• FcgammaR1
IgG
Monocytes, MO, DC
During inflammation, also neutrophils and eosinophils
IgG3→IgG1→IgG4
Main purpose is to help phagocytosis
Antibody mediated opsonization
FcgammaRII
3 have lower affinities for IgG than FcGammaR1
FcgammaRIII
NK cells, ADCC (antibody dependent cell mediated, cytotoxicity…using antibodies to help use cells to kill other cells), IgG1 or G3
ADCC only used on NK cells, why? Why not CD8?
NK cells part of innate/nonspecific. T cells have TCR and because of all different proliferation and differentiation they go through, they have highly specific TCR. NK cells use Fc receptors and get specificity through antibodies. CD8 T cells use TCR to find cells vs. NK cells nonspecific and just have Fc receptor which binds to constant region of antibody and variable region decides where to attack
FcgammaRIIA
activating-->phagocytosis
FcgammaRIIB
inhibiting
B1: mast cells, B cells
MO, neuts, eosinophils
FcalphaRI
monomeric IgA
Activation B/T cells in one mucosal tissue committed to defending all musosal tissues
Naïve b and t cells enter blood-naïve lymphocytes enter 2ndary tissues peyers patch and mesenteric lymphnodes release CCL21 and CCL19→bind chemokind CCr7(naïve b and t cell) →endothelial venules→2ndary lymphoid tissues
•Effector cells (active B/T cells) →recirculate from lymph nodes (PP) → alpha4:beta7 expressing B and T cells (big part to take it to mucosa) →attach MADCAM1 on endothelial tissues in blood stream near mucosa→CCR9 follows CCL25→attachment to mucosal epithelium
T cell entering lymph node--> effector T cell
Circulating T cell enters high endothelial venue in lymph node
binding of L-selectin to GlyCAM-1 and CD34 allows rolling interaction
LFA-1 activated by cytokines bound to extracellular matrix
LFA-1 bind tightly to ICAM-1
diapedesis: lymphocyte leaves blood and enters lymph node and goes to T cell region where Das are
from T cell region, 2 possible directions
No binding of TCR to MHC class II + peptide
has receptor for S-1-P moves to efferent lymphatic vessel
goes to next lymph node ends up in duct and blood stream where it can go to 2ndary lymphoid tissue
Binding: T cell Receptor+ CD3+ CD4+ CD28 (co receptor binds to C7)
CD3, CD4, CD28 binding MHC molecule + peptide
SMAC T cell synapse
signals produced by CD4 to activate Lck
once interaction occurs, Lck is a kinase
LCK interacts with Zap70
phosphorylation of tyrosines CD3 group
DAG
PCK-OMEGA
NFkB
RAS
MAPK pathway
FOS
IP3
NFAT
Need CD28 to produce Jun...Jun and Fos together form AP-1
proliferation, differentiation of T cell --> effector T cell
*****If it was CD8, it would be the same thing. End would be cyto T lymphocyte. binds all same structures but MCH class I and CD8