MedChem of MS
Clinical Course Categories of MS
Relapsing-Remitting MS (RRMS)
The most common form, characterized by temporary
periods of relapses and remissions
Secondary Progressive MS (SPMS)
Sxs worsen more steadily over time w/wo the
occurrence of relapses and remissions
-most ppl who are diagnosed w/ RRMS will --> SPMS
Primary progressive MS (PPMS)
Uncommon, slowly worsening sxs from the onset w NO relapses or remissions
Progressive Relapsing MS (PRMS)
Rare form of MS, steadily worsening disease
state from the onset
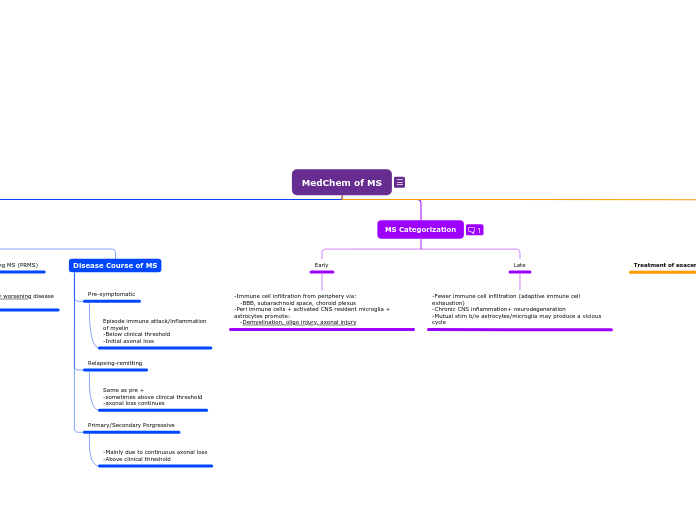
Disease Course of MS
Pre-symptomatic
Episode immune attack/inflammation
of myelin
-Below clinical threshold
-Initial axonal loss
Relapsing-remitting
Same as pre +
-sometimes above clinical threshold
-axonal loss continues
Primary/Secondary Porgressive
-Mainly due to continuous axonal loss
-Above clinical threshold
MS Categorization
Early
-Immune cell infiltration from periphery via:
-BBB, subarachnoid space, choroid plexus
-Peri immune cells + activated CNS resident microglia + astrocytes promote:
-Demyelination, oligo injury, axonal injury
Late
-Fewer immune cell infiltration (adaptive immune cell exhaustion)
-Chronic CNS inflammation+ neurodegeneration
-Mutual stim b/w astrocytes/microglia may produce a vicious cycle
Treatment :D
Treatment of exacerbations (early RRMS):
Disease modification treatment
Interferon-B1a/B1b
Indication: Relapsing MS
-Reduce MRI lesion activity
-reduce brain atrophy
-inc time to reach clinic def MS
-decrease relapse rate
-reduce risk of sustained disability progression
MOA:
-Immunomodulation
-reduces inflammatory response
Agents:
B1a (glycosylated):
-Avonex, Rebif
B1b (non-glycol):
-Betaseron, Extavia
Pegylated-IFNB1a:
-Plegridy
ADEs:
-Flu-like sxs
-depression
-Caution: dev. of neutralizing antibodies (NABs) --> dec efficacy overtime
Antibodies
Alemtuzumab
Indication: High efficacy for relapsing MS
-Use after inadeq response to 2 other drugs
MOA:
-CD52 monoclonal antibody
-depletes T+B cells
ADEs:
-Infusion Associated Rxn (IAR) in 90% of pts
-Mild-mod: headache, rash, pyrexia, N, resp/urinary tract infections
-Increased herpes infection risk (prophylactic acyclovir txt)
-secondary autoimmune disease mainly changing thyroid func (30-40% of pts)
Natalizumab
Indication: Relapsing MS
MOA:
-Humanized IgG monoclonal antibody
-binds to interns, reduces lymphocyte entry through BBB
ADEs:
-IAR
-Risk of PML (progressive multifocal leukoencephalopathy) due to human polyomavirus (check pts)
-risk of immune reconstitution inflammation syndrome (IRIS) when D/C due to PML
-depression, infection, fatigue
Ocrelizumab
Indication: MS or PPMS
MOA:
-IgG monoclonal antibody
-Target CD20 on surface of B cells
-Induce B cell self-destruction
ADEs:
-Infused-related reaction
-Infections
Ofatumumab
Indication: Relapsing MS or SPMS
MOA:
-IgG, CD20
-Bind to CD20 --> Ab-depnd cytolysis
ADEs:
-Hepatitis B reactivation
-Progressive PML
S1P Receptor modulators
MOA:
-Sphingosine 1-phosphate receptor modulators
-Bind to S1P1R/S1P5R --> sequesters lymphocytes in lymph nodes/thymus/GI tract --> reduces circ. T cells/macrophages --> reduce CNS infiltration of immune cells
Fingolimod: Relapsing MS
ADEs:
-Heart toxicity:
-Bradycardia (1st dose monitor)
-QTc prolongation, other arrhythmias, need heart monitor for 6h after 1st dose
-CI: I/III anti arrhythmic drugs, 2/3 AV block, prolonged QTc, recent cardiac diseases
Siponimod: MS/SPMS
** similar to Fingolimod
Ozanimod: MS/SPMS
ADEs:
-somnolence, fatigue, headache, dizziness, bradycardia, HTN, liver injury, N
Other classes:
Glatiramer Acetate (Copaxone)
MOA:
-Mimics myelin basic protein of the myelin sheath --> decoy to T-cell attack
-Mixture of polypeptides containing L-Glu, L-Lys, L-Ala, L-Tyr
Indication: Relapsing MS
Teriflunomide
Indication: Relapsing MS
MOA:
-Reduce inflammation
-Reduce pyrimidine synthesis --> reduce T/B cell proliferation --> reduce lymphocytes in CNS
ADEs:
-Liver toxicity (CI in hepatic imp)
-Teratogenicity
Mitoxantrone
Indication: SPMS, PRMS, or worsening RRMS (LAST RESORT)
MOA:
Binds to+ breaks DNA --> reduce lympho proliferation
ADEs:
-Bone marrow suppression
-Neutropenia
-Menstrual disorder
Cladribine
Indication: MS, SPMS (used when other txt unacceptable)
MOA:
-Adenosine analog --> inhibits nucleoside metabolism --> toxic to B/T cells --> red lympho counts
ADEs:
-Cytotoxic
-Malignancies
-Lymphopenia/hematologic toxicity
-Infections
-Liver injury
-Cardiac failure
-Risk of teratogenicity
Fumarates:
Dimethyl fumarate: Relapsing MS, SPMS
Metabolized by esterase in liver and GI tract to active MMF
Diroximel fumarate: Relapsing MS, SPMS
Less likely to cause GI ADEs due to substitution of methanol with inert 2-hydroxyethyl succinamide
Monomethyl fumarate: Relapsing MS, SPMS
Unknown MOA, may decrease blood vessel permeability. Eliminated mainly as CO2.
Symptomatic therapies