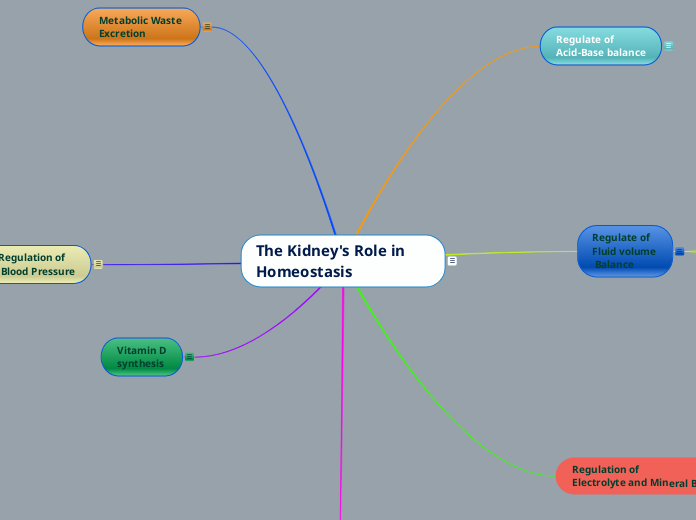
The Kidney's Role in Homeostasis
The Kidney's Role in HomeostasisThe kidneys are able to maintain homeostasis of body fluids despite extremes in dietary intake or change in metabolism. This important function is done through number of processes, such as ,regulation of fluid volume regulation of electrolyte and mineralregulation of blood pressureregulation of acid-base balanceregulation of hormone productionsynthesis of Vitamin Dexcretion of metabolic waste
Metabolic Waste
Excretion
Metabolic waste excretionMany unwanted end products from body's metabolism and other toxics will be excrete by the kidney.Creatinine ( waste product from muscle breakdown) freely filters at the glomerulus and more will secrete to filtrate at proximal convoluted tubule. Creatine will never be reabsorbed to the blood stream from any part of the nephron. Urea ( waste product of protein breakdown-at liver) freely filters at the glomerulus and reabsorb at proximal convoluted tubal and Loop of Henle.Apart from these, the kidney removes unused drugs in the filtrate, as well.
Regulation of
Blood Pressure
Blood pressure regulationWhen the blood pressure sensing cells in the afferent arteriole sense the low in blood pressure, they stimulate Renin releasing cells in the afferent arteriole to release the enzyme called Renin. Renin acts on the inactive Angiotensinogen (produced by the liver) in the blood and convert it into Angiotensin 1.The Angiotensin Converting Enzyme (ACE) from the lung converts the Angiotensin 1 into Angiotensin 2 which acts on the cortex of the Adrenal glands to produce the hormone Aldosterone. Aldosterone makes the increased reabsorption of sodium and water ( from distal tubule of the nephron) to the blood system thus make the arterial blood pressure high.Apart from stimulating Aldosterone production, Angiotensin 2 makes the vasoconstriction (hence increase in vascular resistance), which helps to increase the blood pressure in the vascular system.Not only that, but Angiotensin 2 makes the glomerular filtration low, thus helping the body to keep fluid within the cardiovascular system.
Regulate of
Acid-Base balance
Acid-base BalanceThe kidney regulates the acid -base balance in the Extra Cellular Fluid (ECF), by controlling the bicarbonate ion (acts as buffer) concentration there.Normal bicarbonate concentration in the ECF is 22-29 mEq/L.CO2 concentration is regulated by the lungs.When the pH increases (alkaline status in ECF), the nephron excrete more HCO3- into the filtrate at proximal convoluted tubule (PCT), while reducing secretion of the H+, thus bending the pH of ECF more towards acidic status.If this procedure was interrupted for any reason, it can be seen in many ways in the body and this condition is called alkalosis. Eg:Decreased level of consciousnessTachycardiaHypoventilationTremors muscle crampsWhen the pH decreases (ECF becomes more acidic),the body reabsorbs (at PCT) HCO3- in the filtrate into blood stream, while secrete more H+ into the filtrate, thus making pH of the ECF more alkaline.If this procedure was interrupted, many symptoms may appear in the body and this condition is called acidosis. Eg:possible hyperkalemia which may lead to fatal cardiac arrhythmiacomahyperventilation( Kussmaul's breathing)
Regulate of Fluid volume
Balance
Regulation of fluid volume is a very important function the kidney does, with the help of hormones like ADH, Aldosterone and Atrial Natriuretic Peptide (please see notes under above hormones).Fluid regulation is done either by excreting the excess water and sodium (from the plasma) as urine by the kidney, or it retains water following a number of procedures in case of any depletion like in dehydration.Signs and symptoms of of hypervolemia (accumulating of excess fluid in the body)edema.discomfort in the body-headache, bloating.HBP/HTN.organ failure-heart, lungs, kidney, liver.pulmonary edema.Signs and symptoms of of hypovolemia (critical decrease in body fluid)Anxiety or agitation.Confusion.Decreased or no urine output.Generalized weakness.Rapid breathing.
Contribution of
Anti-diuretic hormone (ADH)
ADHADH is produced at the Hypothalamus, as per the respond of high osmotic pressure(due to low water content) received at the osmoreceptors there.ADH is secreted at the posterior lobe of the Pituitary gland and acts on the collecting ducts of the nephron.The ADH receptors at the collecting ducts open (increased water permeability) and water releases to medulla of the kidney.The water will absorb to the blood stream from medulla, thus conserving the fluid in the body.Please refer the diagram for the action of ADH when the water content is high.
Contribution of
Aldosterone hormone
AldosteroneWhen the blood pressure sensing cells in the afferent arteriole (of the glomerulus) sense the low in blood pressure( when the water content is low, Eg. dehydration), they stimulate Renin producing cells in the afferent arteriole to release Renin. Renin acts on the Angiotensinogen(produced by the liver) in the blood and convert it into Angiotensin 1.The Angiotensin Converting Enzyme(ACE) from the lungs, converts the Angiotensin 1 into Angiotensin 2 which affects on the cortex of the Adrenal glands to produce the hormone Aldosterone. Aldosterone makes the increased reabsorption of sodium and water ( from distal tubule of the nephron) to the blood system , thus conserving the fluid in the body.
Contribution of
Atrial natriuretic peptide
Atrial natriuretic peptideAtrial natriuretic peptide is released (from cardiac atrial cells) as a respond to increased atrial stretch ( due to high blood pressure/ high blood volume)Atrial natriuretic peptide work on kidney encouraging excretion of sodium and water hence releasing excess water from the body, as urine.reducing Aldosterone secretion (by Adrenal glands) reducing releasing of Renin (by kidney)
Regulation of
Electrolyte and Mineral Balance
Sodium
Regulation
Sodium RegulationSodium is a very important electrolyte in the blood which helps to conduct nerve impulses, contract and relax muscles and maintain the proper balance of water and minerals. Normal blood sodium level is 135-145 mEq/L.Depending on the sodium level in the extracellular fluid , sodium may reabsorb or excrete from the body. Sodium is mainly reabsorbed at the proximal convoluted tubular (60%-65%) by passive and active transport mechanism.The amount of sodium reabsorption at the distal convoluted tubular will be determined by hormones such as ADH and Aldosterone. Atrial natriuretic peptide hormone inhibits the sodium reabsorption.Hypernatremia : increase of sodium in the ECF above 145mEq/L. Signs and symptoms:Muscle weakness.Restlessness.Extreme thirst.Confusion.Lethargy.Irritability.Seizures.Unconsciousness.Hyponatremia: decrease in sodium in the ECF below 135mEq/L. Signs and symptoms:Nausea and vomiting.Headache.Confusion.Loss of energy, drowsiness and fatigue.Restlessness and irritability.Muscle weakness, spasms or cramps.Seizures.Coma.
Potassium
Regulation
Potassium RegulationPotassium is the main intracellular cation. Only 2% in extracellular portion of the body. Important in maintaining the membrane potential of nerve and muscle sells.Freely filtrate at glomerulus. Reabsorption at proximal convoluted tubule(65%) by active transportIf any increase in extracellular potassium , Aldosterone secretes and increases the secretion of potassium from the distal convoluted tubule.
Calcium
Regulation
Calcium RegulationCalcium is one of the main mineral constituent of bone. Calcium is vital in controlling nerve and muscle cells' conduction. Calcium is freely filtrate at glomerulus, in the nephron. As per requirement of the body , reabsorption of calcium happens at ,proximal convoluted tubule -control by active transport(65%)ascending limb of the Loop of Henle(20%-25%)distal convoluted tubule(10%-12%)-control by Parathyroid Hormone(PTH) -depends on body's need.
Magnesium
Regulation
Magnesium RegulationMagnesium is an important intracellular electrolyte involve in energy storage and production. Most of the magnesium is found within bones.Most of filtered magnesium is reabsorbed at proximal convoluted tubule and under the influence of PTH, while some of the magnesium will be reabsorbed at distal convoluted tubule.
Phosphate
Regulation
Phosphate RegulationImportant as a vital buffer agent to regulate pH in the ECF.Normal phosphate level in ECF is 0.97-1.45 mmol/L.Phosphate is freely filtered at the glomerulus.If Phosphate level is low,100% reabsorption-at proximal convoluted tubule. If phosphate level is high, filtered phosphate will excrete in the urine and further secretion of phosphate from the blood will happen at distal convoluted tubal (control by PTH) until the phosphate level reaches to the the desired point.
Chloride
Regulation
Chloride RegulationChloride is a very important anion that is responsible for maintaining the acid- base balance in the body, regulating fluid and transmitting nerve impulse. The normal range for chloride in adults is between 98 -107 mEq/L.Chloride will be freely filtered at glomerulus and reabsorb at proximal convoluted tubal by active transport.
Vitamin D
synthesis
Vitamin D synthesisOne of the kidney's function is to help body to synthesize vitamin D. Vitamin D comes from two sources in people. It could either be by exposure to the sun's ultraviolet B radiation or, it is absorbed from food or food supplements. However, during the initial stage, this vitamin D is in an inactive form, in the body.To become activate, the inactive vitamin D should undergo 2 metabolic conversions. One in the liver and the other one in the kidney (PTH, secret from parathyroid gland stimulates the process inside the kidney ).The produced Vitamin D helps the body absorb and retain calcium and phosphorus, both critical for building bones.
Regulation of
Hormone production
Erythropoietin
synthesis
Erythropoietin synthesisErythropoietin production, done by the kidney, is stimulated by low oxygen level ( in an event where RBC count become low-eg: blood loss) in the blood.When the Erythropoietin was released to the blood, it reaches the RBC production sites (bone marrow of flat bones / bone marrow sites at the proximal and distal sides of long bones) and increase the RBC production and release them to blood stream. The newly released RBC carry more oxygen and compensate the low oxygen status of the body.
Renin
synthesis
Renin synthesisWhen the blood pressure sensing cells in the afferent arteriole (of the glomerulus) sense the low in blood pressure, they stimulate Renin producing cells in the afferent arteriole to release Renin. Renin helps to produce Aldosterone in the Adrenal gland, which affects on the collecting ducts to increase reabsorption of water from distal convoluted tubule and conserve fluid in the body.