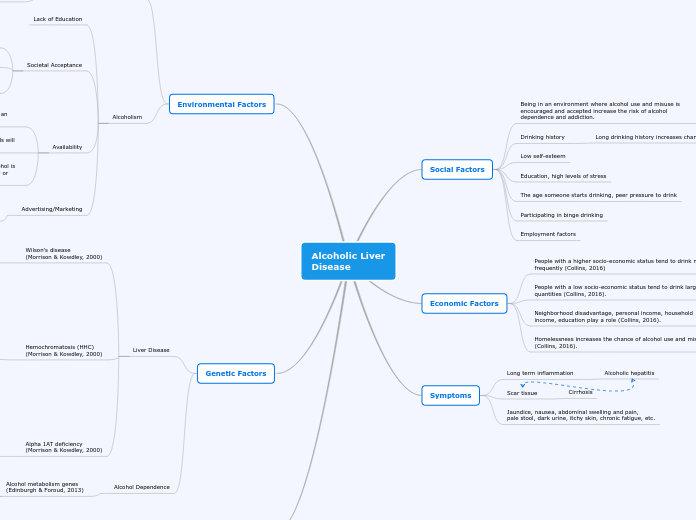
Alcoholic Liver
Disease
Social Factors
Being in an environment where alcohol use and misuse is encouraged and accepted increase the risk of alcohol dependence and addiction.
Drinking history
Long drinking history increases chance of alcohol dependence
Low self-esteem
Education, high levels of stress
The age someone starts drinking, peer pressure to drink
Participating in binge drinking
Employment factors
Economic Factors
People with a higher socio-economic status tend to drink more frequently (Collins, 2016)
People with a low socio-economic status tend to drink larger quantities (Collins, 2016).
Neighborhood disadvantage, personal income, household income, education play a role (Collins, 2016).
Homelessness increases the chance of alcohol use and misuse (Collins, 2016).
Symptoms
Long term inflammation
Alcoholic hepatitis
Scar tissue
Cirrhosis
Jaundice, nausea, abdominal swelling and pain,
pale stool, dark urine, itchy skin, chronic fatigue, etc.
Environmental Factors
Liver Disease
Pollutants
Lead, mercury, PCB, pesticides, etc.
(American Gastroenterological Association, 2009).
Increases risk for abnormal
liver enzymes
Alcoholism
Lack of Education
Societal Acceptance
Media glorifying drinking
Lack of consequences
high profile celebrities, sports star and local role models promoting alcohol with seemingly no adverse effects
Availability
The higher number of licensed liquor establishments in an area the more likely individuals are to drink
The lower the price of alcohol, it's more likely individuals will drink.
Underage individuals are more likely to drink when alcohol is freely available to them, either by purchasing it directly or when it's available at parties
Advertising/Marketing
Alcohol advertisements creates an environment that suggest alcohol consumption and over-consumption are normal activities.
Genetic Factors
Liver Disease
Wilson's disease
(Morrison & Kowdley, 2000)
Caused by mutation in
ATP7T gener
Provides instructions to
make copper-transporting ATPase 2
Transports copper from the
liver to other parts of the body
Hemochromatosis (HHC)
(Morrison & Kowdley, 2000)
Iron deposits collect in
liver and other organs
Type 1
Most common, symptoms begin in
adulthood; men between 40-60
and women after menopause,
Mutation in HFE gene
(Genetic Home Reference, 2019)
Produces surface cell marker for liver and intestinal cells that help detect the amount of iron in the body
Type 2
Juvenile onset, if untreated, potential
fatal heart disease is evident by age 30
Mutation in HJV or HAMP gene
(Genetics Home Reference, 2019)
HJV
Makes hemojuvelin protein, helps maintain proper iron levels by regulating hepcidin protein.
HAMP
Makes hepcidin, inhibits iron absorption when iron levels are too high
Type 3
Intermediate between type 1 and
type 2; symptoms usually appear
before the age of 30
Mutation in TFR2 gene
(Genetics Home Reference, 2019)
Makes transferrin receptor 2
Helps iron enter liver cells
Type 4
AKA ferroportin disease
Symptoms begin in adulthood;
men between 40-60 and
women after menopause
Mutation in SLC40A1 gene
Makes ferroportin proteins
Transports iron from food into cells
Alpha 1AT deficiency
(Morrison & Kowdley, 2000)
Mutation in SERPINA1 gene
(Genetics Home Reference, 2020)
Makes alpha 1AT proteins, protects
the body from neutrophil elastase enzyme
Neutrophil elastase released to fight infections, but can attack body tissues when not regulated by alpha 1AT proteins
Alcohol Dependence
Alcohol metabolism genes
(Edinburgh & Foroud, 2013)
ADH1B
ALDH2
Cause
Chronic heavy drinking
Alters liver's ability
to metabolize fats
Fat builds
up in the liver