Chapter 5: Lecture notes
PSY 341: Abnormal Psychology
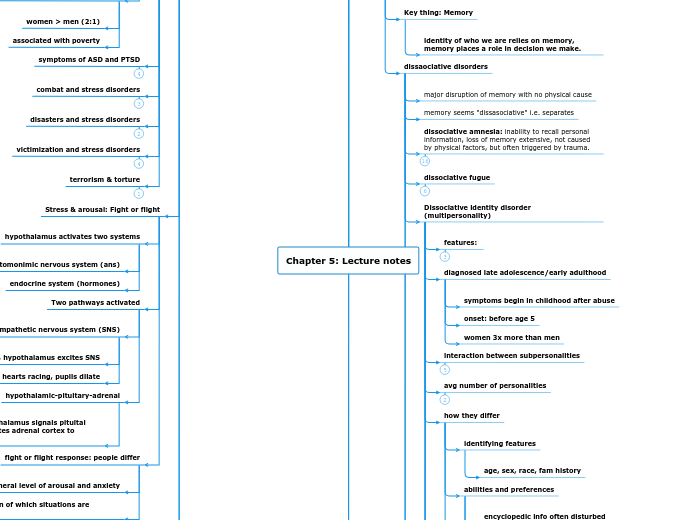
Disorders of Trauma and Stress
Part 2: Dissociative Disorders
Key thing: Memory
identity of who we are relies on memory, memory places a role in decision we make.
dissaociative disorders
major disruption of memory with no physical cause
memory seems "dissasociative" i.e. separates
dissociative amnesia: inability to recall personal information, loss of memory extensive, not caused by physical factors, but often triggered by trauma.
dissociative fugue
Dissociative identity disorder (multipersonality)
features:
diagnosed late adolescence/early adulthood
symptoms begin in childhood after abuse
onset: before age 5
women 3x more than men
interaction between subpersonalities
avg number of personalities
how they differ
identifying features
age, sex, race, fam history
abilities and preferences
encyclopedic info often disturbed
Key words
Key words
physiloogical responses
ans activity, BP, allergies
how common?
psychodynamic view
behavior view
Dissociative Disorders Treatment
Depersonalization-Derealization Disorder
Dissosociative Disorders Summary
am
Our memories make up who we are as a person and influences the decisions we make.
When someone has a dissociative disorder, they have a major disruption in their memory affecting their identity and ability to make decisions.
Notes
Dissociative amnesia (DA) is when the patient is unable to recall any memory of an event. This can be localized (all memory is lost), selective (remembers beginning event, but may forget friends and family), and continuous (when future memory loss is regularly occurs). Continous is really rare.
Dissociative fugue - an extreme version of Dissociative amnesia. following an extreme traumatic event, a person may lose their identity and memory. Some may even leave and adopt a new identity without realizing it. When they do become aware of it, the dissociation will abruptly stop. This usually occurs when the patient's safety was extremely threatened.
Treatment for DA: often resolves on their own. It can also be done through psychodynamic therapy guides the client to explore the unconscious mind and bring the event to the subconscious. Hypnotic therapy helps a client recall the memory. truth serum - drug therapy that calms the client's mind to free their inhibition. Often very successful.
Dissociative Identity Disorder aka multipersonality disorder is when two or more distinct subpersonalities exist within a client as a form of protecting them after experiencing some kind of traumatic event. This is usually diagnosed before the age of 5, during late adolescent and early adulthood. The subpersonalities often switch from the primary and can have distinct personalities, emotions, and behaviors.
DID's subpersonalities interact in three ways: mutually amnesic personalities (all personalities are not aware that each other exist), cognizant amnesic personalities (all personalities are aware that each other exists), one-way amnesic personalities (some personalities are aware of each other, but it is not mutual.)
Treatment for DID can be complex and difficult. The ultimate goal is for the subpersonalities to merge into one. However, the first step is for the therapist to recognize the existence of subpersonalities. There, they will feel safe enough to explore the reasons why there was a split in the first place. It's a continuous treatment, but ultimately, the final merge deteremines the treatment was successful. undefined
Depersonalization-derealization-disorder (DDD) is when someone is dissociative, they are experiencing an out-of-body experience, which is when the mind separates from the body, and the person sees them from the outside looking within (3rd POV). Unlike DID, DDD does not have any memory impairments. Instead clients with DDD experience a mental separation from their physical bodies. Their experience becomes unreal from the real world.
Just because someone may experience some depersonalization or derealization, does not mean they have DDD. In order to be classified as having DDD, the person needs to have recurring events and it must be affecting their job and interpersonal relationships. This usually shows up in adolescents/young adults. It is long-lasting and sudden.
Part 1: Stress and Arousal
Stress in the Brain
Stress has two components
stressors: event that creates demands
stress responses: one's reaction
Key systems activated during stress include: ANS and endocrine system
Autonomic nervous system (ANS): controls involuntarily bodily functions
endocrine system: releases hormones (cortisol) during stress response.
arousal and fear when stressor is perceived as threatening
fear is a package of responses: physical, emotional, cognitive responses.
plays a central role in two psychological stress disorders
acute stress disorder
4 weeks from the event
lasts for less than one month
PTSD
precipitating event = actual or threatened serious injury to self or others
begins either shortly after event or months or years afterward
current prevalence: 3.5%; lifetime: 7-9%
women > men (2:1)
associated with poverty
symptoms of ASD and PTSD
combat and stress disorders
disasters and stress disorders
victimization and stress disorders
terrorism & torture
Stress & arousal: Fight or flight
hypothalamus activates two systems
automonimic nervous system (ans)
endocrine system (hormones)
Two pathways activated
sympathetic nervous system (SNS)
during danger, hypothalamus excites SNS
hearts racing, pupils dilate
hypothalamic-pituitary-adrenal
during stress, hypothalamus signals pituital gland which stimulates adrenal cortex to release
fight or flight response: people differ
general level of arousal and anxiety
their perception of which situations are threatening
state anxiety, situation based: fear of flying when flying, you will have this feeling
development of stress disorders
biological and genetic factors
trauma > physical changes
abnormal Neurotransmitter & hormone activity
neuroprenipine and cortisol are related
once someone develops a stress disorder, it sets in forth further damage in the mind and body, esp in the amygdala and hippocampus
biological/genetic predisposition
personality factors
pre-existing high anxiety
trait anxiety
negative worldview
resiliency
childhood experiences that increase risk
psychological disorders
assault, abuse, catastrophe
parent divorce before age 10
weak social support
some cultural groups more vulnerable
latinos are more vulnerable - cultural beliefs and trauma and social relationships and social support.
Treatment of stress disorder
general goals
end lingering stress reactions
gain perpsecitve on painful experiences
return to constructive living
specific to combat veterans
drug therapy
antidepressant / anti-anxiety
behavioral exposure techniques: reduce specific symptoms, flood & relaxation, EMDR
insight therapy
Stress and Arousal Summary
Stress is the event that creates demands. It has two components: one's reaction, and how the event is judged. We have our own capacity to react to events, and it happens differently for everyone. When
Stress triggers arousal and fear (flight or fight). Fear is a package of emotions that affect physical, emotional, and cognitive responses. Both arousal and fear play the central role in two psychological stress disorders: Acute Stress Disorder and PTSD.
Acute Stress Disorder has an onset of four weeks and usually disappears after 1 month. PSTD occurs when the precipitating event was very traumatic or stressful. It shows up weeks after the event or months or years even.
Combat Stress Disorders - "shell shock" and "combat fatigue."
Disasters and stress disorder occurs during natural disasters, airplane crashes, car accidents, etc. Most common and 10 times more at risk.
Victimized and stress disorders: impact may be immediate and longterm, ongoing victimization and abuse.
Terrorism and torture stress disorders usually result from survivors of war, or civilians.
When the fight or flight response is activated, the hypothalamus activates two systems: automated nervous system (ANS) and the endocrine system (hormones). In danger, the hypothalamus excites the sympathetic nervous system (SNS), which activates cortisol and nopreniprine, causing symptoms like pupils dilating and heart racing. Then the SNS kicks in to help calm the ANS and bring it back to a homeostasis state.
People have different fight or flight responses, which result from a generalized level of arousal and anxiety. It depends on the person on how events may be perceived as threatening, whereas for others it is not. Then there is situational-based, state anxiety like when you have a fear of flying while in the airplane.
Abnormal neurotransmitter and hormone activity: cortisone and noprenprine. Once you develop a stress disorder, damage and shrink in the mind, especially in the amygdala and hippocampus. The trauma is greater than the physical symptoms, and it can also cause physical pain (somatic pain) that your body has enveloped from the trauma.
People with different personalities are more likely to develop PTSD than others. Often the anxious types can contribute a chronic state of heightened anxiety or trauma aka trait anxiety, if someone has a negative worldview, not as resilient, or has some sort of childhood trauma, then PTSD is more likely to occur. Other factors include, rape/assault, war/violence, abuse/childhood abuse/catastrophe, personality disorders, biological/genetic predisposition, or experiencing your parents' divorce before the age of 10. Hispanic culture, and other cultural groups are at a higher risk than others, and a weak social support.
Treatment to Stress Disorders: Therapy goals: ending the lingering stress reactions, acknowledging and giving a different perspective the traumas experienced, return to constructive living. Combat Stress Disorder Treamtent: drug therapy: antidepressant and anti-anxiety, reduce behavioral exposure techniques: flood & relaxation, EMDR, and reduce specific symptoms, and insight therapy.
Post traumatic growth - being able to use that kind of trauma as something more positive change and growth for yourself and others. undefined