a Lacey Cheek 4 éve
418
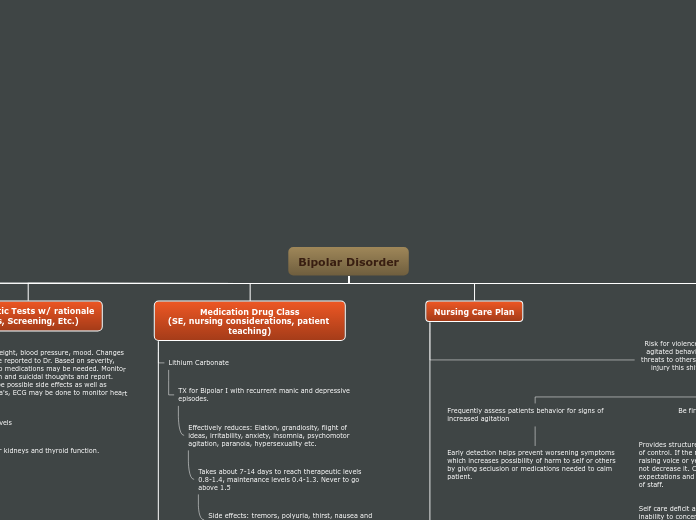
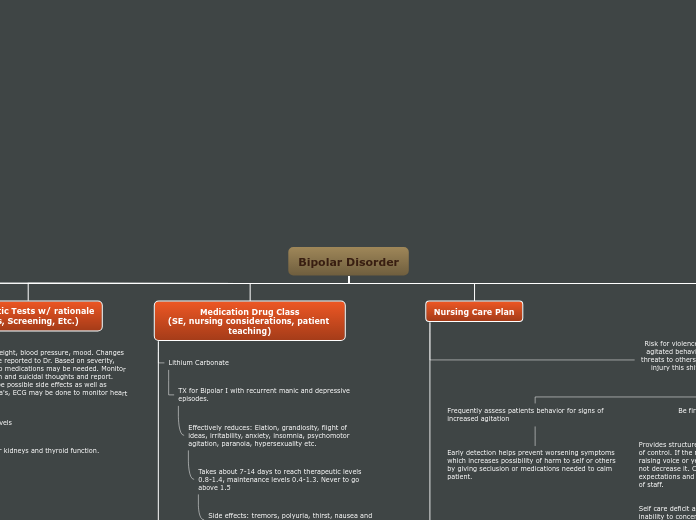
Mind Map Assignment Lacey Cheek
Final map
a Lacey Cheek 4 éve
418
Még több ilyen
Adults: irritable hypomanic episodes
Provide limits to what the patient can do, this provides structure and expectations for the patient. If they start to become agitated around others, move them to a quieter place until they calm and can return to group.
Walking, painting, coloring etc.. all help patient to focus on something else and release tension in a constructive manner.
If patient is escalating they may require medications to help ease symptoms and calm them. Or may need to move to a quieter dim lit area to reduce stimuli and help patient to self soothe.
Setting a schedule provides structure which provides the patient with expectations of what and how things will happen in the day to reduce anxiety and hopefully provide peaceful transitions between tasks.
Patients who are distracted and have poor concentration, are countered by simple and firm instructions. Ex. Here is your toothbrush, add toothpaste. Here is soap, put on sponge, scrub body, rinse.
Limiting options and providing only those appropriate clothes give patient ability to choose what they want, while staying appropriate, also makes the choice easier for them when they aren't thinking clearly and are easily distracted.
Providing a calming environment helps decrease escalation of anxiety and manic symptoms.
Provides structure and control when a patient is out of control. If the nurse tries to match the patient by raising voice or yelling, that escalates the problem not decrease it. Consistency provides limits and expectations and decreases chance of manipulation of staff.
Early detection helps prevent worsening symptoms which increases possibility of harm to self or others by giving seclusion or medications needed to calm patient.
Teaching: Be alert for signs of agranulocytosis (fever, sore throat) be alert for suicidal thoughts report immediately, monitor bp, may cause daytime drowsiness be careful operating vehicles.
Action: Decreases synaptic transmission in the CNS by affecting sodium channels in neurons. Decreased mania
Ataxia, weight gain, blurred vision, HTN, drowsiness, Be alert for signs of agranulocytosis
Teaching: Do not take with alcohol, don't stop taking without speaking to Dr. first, may cause day time sleepiness, be careful operating vehicles.
S/E: behavior changes, depression, drowsiness, insomnia, tremor, ataxia, blurred vision, photosensitivity.
Action: stabilizes neuronal membranes by inhibiting sodium transport
Teaching: monitor mood changes and thoughts of suicide and notify doctor. May cause daytime sleepiness, be careful driving.
More effective when no family HX. Superior for rapid cycling diminishing impulsive and aggressive behavior beneficial in controlling mania and depression
Valproate: tx lithium nonresponders who are in acute mania, dysphoric mania.
Action: Increase levels of gamma-aminobutyric acid (GABA), an inhibitory neurotransmitter in the CNS
S/E agitation, dizziness, headache, insomnia, sedation, confusion, depression, rash, alopecia, tremors, ataxia nvd.
Effectively reduces: Elation, grandiosity, flight of ideas, irritability, anxiety, insomnia, psychomotor agitation, paranoia, hypersexuality etc.
Takes about 7-14 days to reach therapeutic levels 0.8-1.4, maintenance levels 0.4-1.3. Never to go above 1.5
Side effects: tremors, polyuria, thirst, nausea and weight gain.
Toxicity. Early signs: Fine hand tremor, polyuria, mild thirst and nausea.
Advanced and severe Toxicity: Coarse tremors, persistent GI upset, AMS, muscle hyper irritability, sedation. Ataxia, giddiness, blurred vision, clonic movements, large dilute urine outputs. Seizures, severe hypotension. DEATH
Teaching: Monitor personality /behavioral changes Notify physician if these changes become problematic. Report tremors, ams, ataxia etc immediately. Drink lots of fluids, take as directed, do not chew.
Grandiosity: inflated self regard
Flight of ideas: Continuous flow of accelerated speech with abrupt changes from topic to topic.
Mania
To be considered mania, the elevated, expansive, or irritable mood must last for at least one week and be present most of the day, nearly every day. To be considered hypomania, the mood must last at least four consecutive days and be present most of the day, almost every day.
With 3 or more of the following present: Inflated self-esteem or grandiosity Decreased need for sleep Racing thoughts Distracted easily Increase in goal-directed activity or psychomotor agitation Engaging in activities that hold the potential for painful consequences, e.g., unrestrained buying sprees
Stress, stressful family life, excess stress daily.
Upper socioeconomic class
Genetics: diacylglycerol kinase eta and CRY2 gene commonly associated with bipolar.