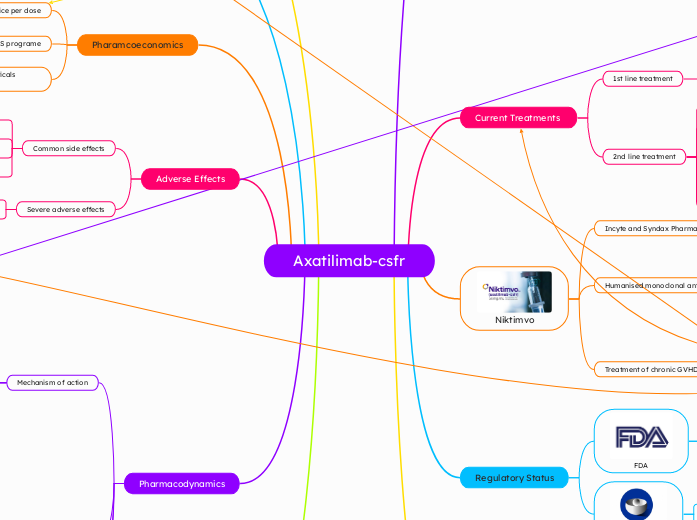
Axatilimab-csfr
Graft Versus Host Disease
Complication of HSCT for various autoimmune diseases and cancers
Acute GVHD
Presents within first 100 days post HSCT
35% - 50% of recipients
Symptoms
Rash
Diarrhoea
Nausea and vomiting
Jaundice
Treatment
Topical or systemic steroids
Chronic GVHD
Presents after 100 days post HSCT
40% - 70% of recipients
Symptoms
Dry mouth, gum disease, mouth sores
Dry eyes and visual disturbances
Dry persistent cough
Skin tightness, swelling
Similar pathology to sclerosis
Pathophysiology
Donor CD8 T-cell induced immune response
Type IV hypersensitivity reaction
Overactive B cell response characteristic of cGVHD
CSF-1 in cGVHD
Colony stimulating factor 1 binds to CSF-1R
CSF-1R signalling promotes macrophage differentiation
M1 induced inflammation
M2 induced fibrosis
Current Treatments
1st line treatment
Glucocorticoids
50% success rate
2nd line treatment
Combined glucocorticoid and calcineurin inhibitors
Monoclonal antibodies
Rituximab
TK inhibitor
Ruxolitinib
Ibrutinib
ROCK inhibitor
Belumosudil
Chemotherapeutics
Methotrexate

Niktimvo
Incyte and Syndax Pharmaceuticals
Humanised monoclonal antibody
CSF-1 receptor antibody
IgG4 monoclonal antibody
Produced in CHO cell lines
MW: 150kDa
Treatment of chronic GVHD
Approved for adults and children
weighing > 40kg
Approved for use as a 3rd line
treatment for cGVHD
Novel treatment approach
First drug of it's kind
Regulatory Status
FDA
50mg vial approved on 14/08/2024
9mg and 22mg vial sizes
approved on 15/01/2025

EMA
Phase II trial ongoing as of 26/02/2025
Same objectives as AGAVE-201 Trial
Estimated end date 31/12/2025
AGAVE-201 Trial
Phase II, open-label, randomised,
multi centre trial
Inclusion criteria
> 2 years old (7-79)
Allogenic HSCT recipients
Active cGVHD requiring systemic
immune suppression
Recurrent or refractory active cGVHD despite 2 lines of systemic treatments
241 participants
0.3mg/kg (Q2W)
1mg/kg (Q2W)
3mg/kg (Q4W)
Primary efficacy endpoint was objective response rate in first 6 cycles (24 weeks)
Secondary endpoint was proportion of patients reporting a clinically significant reduction in symptoms
Primary end point was achieved in all groups
Highest ORR 74% and lowest toxicity
observed in 0.3mg group
Considerations and caveats
Caters to steroid refractory patients
Long term efficacy yet to be determined
Frequency and method of administration
Future studies
Use in pregancy
Pregnant women excluded from AGAVE-201 trial
No pre-clinical trials assessing reproductive
and developmental toxicity
Ongoing phase III trials
Use as 1st line treatment
Combination of Ataxilimab and corticosteroids
Alternative route of administration
Treatment of other diseases
Pharamcoeconomics
Price per dose
9mg vial - $4,725
22mg vial - $11,500
50mg vial - $21,500
IncyteCARES programe
Royalty Pharma and Syntax Pharmaceuticals partnership
$350 million in exchange for 13.8% royalties of US sales
Adverse Effects
Common side effects
Muscle or joint pain
Headache
Fatigue
Nausea
Severe adverse effects
Liver toxicity (increased AST and ALT)
Infusion related bacterial or viral infection
Pharmacodynamics
Mechanism of action
Blocks CSF-1 and IL-34 binding
Prevents macrophage activation
Subtopic
Inhibits inflammation and fibrosis

Dose-dependent increase in CSF-1 and IL-34
Dose-dependent decrease in circulating
non-classical monocytes
No known drug interactions or contraindications
Pharmacokinetics
Administration
IV administration
0.3mg/kg (max 35mg/kg)
30 minutes Q2W
Absorption
No systemic accumulation
observed
Distribution
VD: 6.06L
Metabolism
Expected to be metabolised into small
peptides by catabolic pathways
Half-life
T 1/2: 10.7hrs - 108hrs
(0.15mg/kg - 3mg/kg)
Elimination
Total clearance: 0.07L/h
Randomisation of AGAVE-201 was stratified based on the use of these drugs
T and B cell response is the primary
therapeutic target