Lisinopril
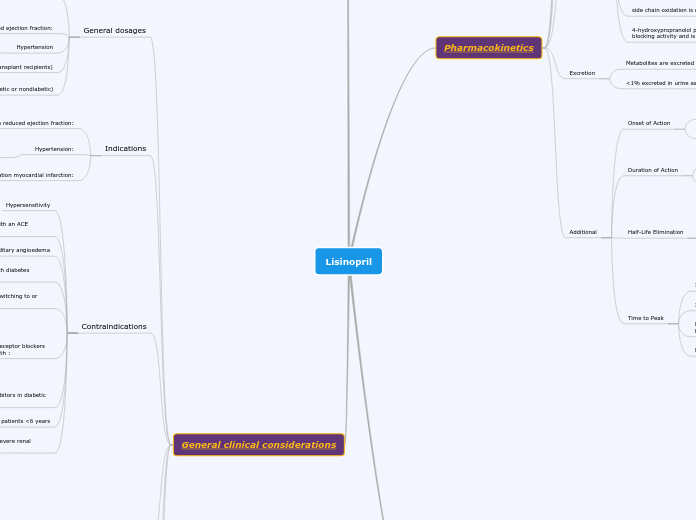
Pharmacokinetics
Absorption
Oral
Rapid and Complete
Bioavailability
~25% reaches systemic circulation due to high first-pass metabolism
oral bioavailability may be increased in Down syndrome children
protein-rich foods increase bioavailability by ~50%
Distribution
Vd: 4 L/kg in adults
crosses the blood-brain barrier
Metabolism
Extensive first-pass effect, hepatically metabolized to active and inactive compounds
the 3 main metabolic pathways include: Aromatic hydroxylation (primarily 4-hydroxylation), N-dealkylation followed by further side-chain oxidation and direct glucuronidation
the 4 primary metabolites include: Propranolol glucuronide, naphthyloxylactic acid, and sulfate and glucuronic acid conjugates of 4-hydroxy propranolol
Note: Aromatic hydroxylation is catalyzed primarily by isoenzyme CYP2D6
side chain oxidation is mainly via CYP1A2, but also CYP2D6
4-hydroxypropranolol possesses beta-adrenergic receptor blocking activity and is a weak inhibitor of CYP2D6.
Excretion
Metabolites are excreted primarily in urine (96% to 99%)
<1% excreted in urine as unchanged drug
Additional
Onset of Action
Beta-blockade: Oral: 1 to 2 hours; IV: ≤5 minutes
Peak effect: Hypertension: A few days to several weeks.
Duration of Action
Immediate release: 6 to 12 hours
Extended-release formulations: ~24 to 27 hours
Half-Life Elimination
Neonates: Possible increased half-life
Infants (35 to 150 days of age): Median 3.5 hours; Children: 3.9 to 6.4 hours
Adults: Immediate release formulation: 3 to 6 hours; Extended-release formulations: 8 to 10 hours
Time to Peak
Immediate release: Adults: 1 to 4 hours
Infants: ≤2 hours (Hemangeol)
Extended release capsule (Inderal XL, InnoPran XL): 12 to 14 hours
Long acting capsule (Inderal LA): 6 hours
Molecular Pharmacodynamics
Competitive inhibitor of angiotensin-converting enzyme (ACE)
prevents conversion of angiotensin I to angiotensin II,
potent vasoconstrictor
results in lower levels of angiotensin II which causes
results in lower levels of angiotensin II which causes
a reduction in aldosterone secretion
a CNS mechanism may also be involved in hypotensive effect as angiotensin II increases adrenergic outflow from CNS
vasoactive kallikreins may be decreased in conversion to active hormones by ACE inhibitors
reducing blood pressure
Dental applications and considerations
General clinical considerations
General dosages
Acute coronary syndromes:
Non-ST-elevation acute coronary syndrome
Oral: Initial: 2.5 to 10 mg once daily (depending on initial blood pressure)
ST-elevation myocardial infarction:
Oral: Initial: 2.5 to 5 mg once daily initiated within 24 hours of presentation
Heart failure with reduced ejection fraction:
Oral: Initial: 2.5 to 5 mg once daily
Hypertension
Oral: Initial: 5 to 10 mg once daily
Posttransplant erythrocytosis (renal transplant recipients)
Oral: Initial: 2.5 or 5 mg once daily
Proteinuric chronic kidney disease (diabetic or nondiabetic)
Oral: Initial: 2.5 to 10 mg once daily depending on blood pressure
Indications
Heart failure with reduced ejection fraction:
Adjunctive therapy to reduce signs and symptoms of systolic heart failure.
Hypertension:
Management of hypertension in adult and pediatric patients ≥6 years of age.
ST-elevation myocardial infarction:
Treatment of acute MI within 24 hours in hemodynamically stable patients to improve survival.
Contraindications
Hypersensitivity
angioedema related to previous treatment with an ACE inhibitor
idiopathic or hereditary angioedema
concomitant use with aliskiren in patients with diabetes mellitus
coadministration with or within 36 hours of switching to or from a neprilysin inhibitor
Ex: sacubitril
concomitant use with aliskiren, angiotensin receptor blockers (ARBs), or other ACE inhibitors in patients with :
moderate to severe renal impairment (GFR <60 mL/minute/1.73 m2)
hyperkalemia (>5 mmol/L)
with heart failure who are hypotensive
concomitant use with ARBs or other ACE inhibitors in diabetic patients with end organ damage
pediatric patients <6 years
pediatric patients 6 to 16 years of age with severe renal impairment
Toxicities
gasping syndrome
large amounts of benzyl alcohol
In neonates
consists of:
metabolic acidosis
respiratory distress
gasping respirations
CNS dysfunction (including convulsions, intracranial hemorrhage)
hypotension
cardiovascular collapse
Drug interactions
Avoid
bromperidol
grass pollen allergen extract
sacubitril
Monitor
sodium phosphates
dose dependent
amphetamine
aspirin
bupivacaine
heparin
ibuprofen
Pregnancy Categories and Implications
Lisinopril crosses the placenta
Exposure to an angiotensin-converting enzyme (ACE) inhibitor during the first trimester of pregnancy may be associated with an increased risk of fetal malformations
Box warning
[US Boxed Warning]: Drugs that act on the renin-angiotensin system can cause injury and death to the developing fetus. Discontinue as soon as possible once pregnancy is detected.
use in pregnant women should only be considered for cases of hypertension refractory to other medications