Parkinson's Disease
Side effect Management
Drug-induced hallucination and psychosis
Pimavanserin
-FDA approved (5HT-2A inverse agonist) for hallucinations and delusions assoc. w/ PD
-metabolized by CYP3A4/3A5
-DDI: decrease dose by 50% if combined with CYP inhibitors, increase if inducers
-can cause QTc prolongation
What agent is FDA approved for the txt of PD psychosis? Pimavanserin
-Correct electrolyte imbalance
-simply drug regimen
-consider low-dose atypical antipsychotics (Quetiapine, Clozapine)
-consider antidepressants
N/V W/ Apomorphine
Pre-dose w/ timethobenzamide
Treatment
- Carbidopa/L-DOPA, DA agonist or amantadine for bradykinesia, moderate tremors or rigidity
Others:
Apomorphine SQ:
-extensive 1st pass metabolism
-used as rescue/PRN
-N/V common, prepose w/ trimethobenzamide to minimize
-severe hypoTN when w/ 5HT-3 blockers (ondansetron). careful monitoring
DA Agonists
Agents: Ergotamine (bromocriptine, old, not used, pulmonary fibrosis) Nonergotamine (pramipexole/ropinirole)
-reduce levo exposure, delay need to start levo tx
-used as initial tx, in young adult pts or adjunct in older
-Ropini: CYP1A2, used for RLS (restless leg syndrome), causes pts to fall asleep suddenly
-Prami: sudden falling asleep, renal elimination
-AEs: n, confusion, sedation, edema, vivid dreams
-Uses:
-younger pts (<65): for motor fluctuations
-older (>65): hallucinations/ortho HypoTN
COMT Inhibitors
Can COMT inhibitors and dopamine agonists be used in combination to treat PD? Yes
Agents: Entacopone, Tolcapone
-combo w/ carb/levo
-also indicated for "off" eps
-Tol causes liver problems, monitor LFTs
-Delayed diarrhea, brownish-orange urine discoloration
MAO-B Inhibitors
Agents: Selegiline & Rasagiline
-used early in tx, neuroprotective
-sele: metab by CYP2B6/2C19 to L-methamphetamine. ODT bypasses GI and dec formation of the agent
-AE's: N, dec appetite, ortho HypoTN, hallucinations, dyskinesias, insomnia
-Rasa: metab by CYP1A2 to inactive metabolite. Ads like placebo.
Adjunct for "Off" Episodes
Istradefylline:
-Adenosine A2 receptor antagonist
-adj w/ levo/carb for "off" eps
-max dose for smokers >20 cig/d
-DDI: metabolized by CYP1A1/CYP3A4
Safinamide:
-selective, reversible MAO-B inhibitor
-approved for adj txt w/ levo/carb for "off" eps
-may also improve motor function
Amantadine
-mild disease +tremors
-renal elimination, dec dose w/ dec creatinine clearance
-ADEs: confusion, dry mouth, dizziness, hallucinations
-skin discoloration, molting
-limited use in tx
-MOA: DA release, also implicated inhibition of glutamate
-useful in suppressing L-dopa induced dyskinesias
Anticholineragics
-Most useful for tremors
-careful in geriatrics (>65), inc confusion and drying
-other disease: BPH, glaucoma, constipation, Alzheimer's
Carbidopa/L-DOPA
What does carbidopa do in the formulation with levodopa?? Prevent the GI effects of DOPA decarboxylase to allow increase L-Dopa absorption
What are the 4 motor complications assoc. w/ levo/carb therapy? End of dose wearing "off", delayed "on", freezing, and dyskinesias
Tx Levodopa-induced Dyskinesia
PK:
-meals delay
-antacids inc emptying
-absorbed in duodenum by LNAA
-not protein bound
-L-Dopa is the precursor to Dopamine
-it crosses BBB, but carbidopa DOES NOT
-Carbodpa dec conversion of L-dopa to DA = > inc amount to the CNS and reduces GI ADEs
-Need at least 75mg carbidopa
-Max dose of L-dopa unknown, limited by ADEs (N, HTN, sedation, vivid dreams, vomiting)
-Cornerstone of PD tx
-Preferred for geriatrics who are cog + functionally impaired
-Honeymoon period of 5-7yrs
Dyskinesias: L-dopa "on" periods
-assoc. w/ peak DA lvls
-lower drug dose = balance with AE vs. symptoms
-add amantadine
"off-period" dystonia: muscle contractions
-feet, early morning hours, improvs w/ first drug dose
-HS use of CR products L-Dopa or DA agonist
-Baclofen and botox (??)
Delayed On: due to delayed gastric emptying or reduced absorption
-chewing or crushing tabs/ODT on empty stomach
-apopmorphine SQ, possible drug holidays
Freezing: feeling like stuck to the floor
-physiotherapy or walking devices
-increase drug dose, MAO B inhibitor or DA agonist
Issues to be aware of.
End of Dose Wearing Off AKA On/Off: occurs prior to next dose
-happens due to inc loss of storage for DA and short L-DOPA 1/2 life
-peripheral PK effects >> CNS effects
-Give more frequently, add COMT or MAO B inhibitor. CR formulation can be useful
-consider DA agonist during day or HS use of PO products
Rasagiline:
-considered 1st line agent, (-) functional impairment, (+) DA agonist
**consider pt age (<65 or >65?)
What agent can be initially used in PD pts that have symptoms WITHOUT significant impairment? Rasagiline
Algorithm
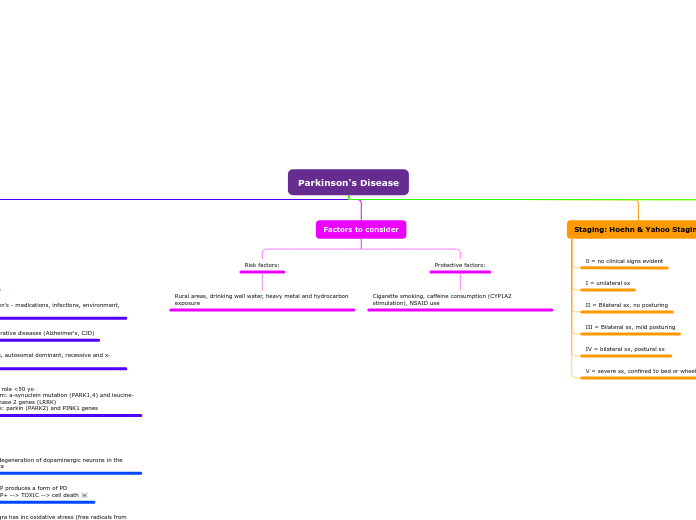
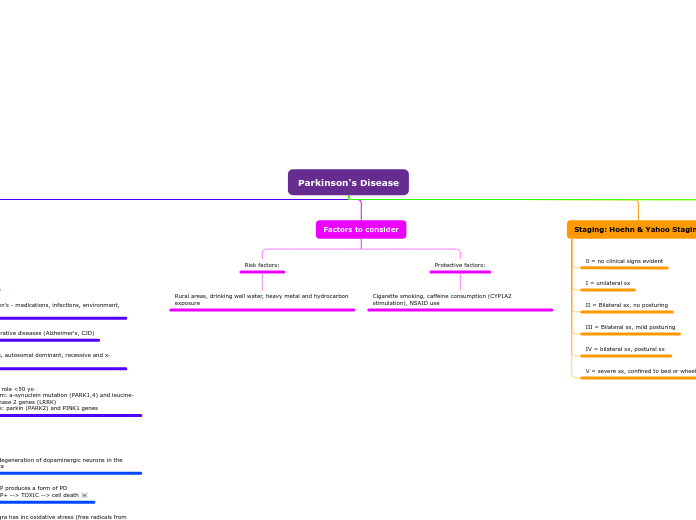
Staging: Hoehn & Yahoo Staging
What is stage IV of PD according to the Hoehn and Yahr staging of severity scale? Bilateral symptoms and postural instability
V = severe sx, confined to bed or wheelchair
IV = bilateral sx, postural sx
III = Bilateral sx, mild posturing
II = Bilateral sx, no posturing
I = unilateral sx
0 = no clinical signs evident
Factors to consider
Protective factors:
Cigarette smoking, caffeine consumption (CYP1A2 stimulation), NSAID use
Risk factors:
Rural areas, drinking well water, heavy metal and hydrocarbon exposure
Pathology
Pathways of DA neurons from SNc to the striatum
DA metabolism:
L-tyrosine --(TH)-> L-DOPA --(L-AAD)-> DA --> converted to metabolites by MAO-B and COMT
L-AAD can be blocked by drugs like carbidopa that do not pass the BBB, thereby increasing L-DOPA lvls from meds and reducing AEs. L-DOPA is also metabolized by L-AAD.
Cont: Nigrostriatal degeneration --> loss of inhibition by the direct path + activates GPi by the indirect path --> dec motor cortex activation --> dec motor output --> clinical symptoms
NTs involved:
-acetylcholine
-GABA
-Glutamate
-enkephalins
-Sub.P
-adenosine
-serotonin
Indirect: D2 inhibit inhibitory GABA/Enkephalin efferents --> projects inhibitory GABA to STN --> excitatory glutaminergic neurons project to the GPi
Direct: D1 receptors stim GABA/Sub.P efferents in the GPi
Etiology
Antioxidative molecules (glutathione) limits damage from free radicals BUT the system may be overwhelmed/impaired.
Free radical --> lipid peroxidation -->damage cell membranes --> slow cell death --> apoptosis
Substantia nigra has inc oxidative stress (free radicals from dopamine autoxidation)
Chemical MPTP produces a form of PD
-MPTP --> MPP+ --> TOXIC --> cell death ☠️
Key feature: degeneration of dopaminergic neurons in the substania nigra
Familial parkinson's, autosomal dominant, recessive and x-linked
Genetics - sig role <50 yo
Autosomal dom: a-synuclein mutation (PARK1,4) and leucine-rich repeat kinase 2 genes (LRRK)
Auto recessive: parkin (PARK2) and PINK1 genes
Other neurodegenerative diseases (Alzheimer's, CJD)
Secondary parkinson's - medications, infections, environment, tumors
Essential tremors
Idiopathic PD
Features
Non-Motor
Neuropsychiatric (depression), autonomic dysfunction (constipation), sleep disturbance (insomnia)
Motor
Why do these signs/sxs occur?
-Reduced DA lvls
-Inc ACh lvls (DA inhibits ACh, when it dec then ACh is inc, leading to tremors)
-DA cells cont. to be destroyed and DA production declines
-Progressive disease, sxs+severity will worsen
-upper extremity tremors at rest
-upper and lower extremity rigidity
-bradykinesia (slow movement)
-postural instability
-other psychiatric disorders can occur
Cardinal features/presentation: Bradykinesia, resting tremors, rigidity, postural instability
Symptoms:
-decreased dexterity
-dysarthria (difficulty speaking)
-dysphagia (diff swallowing)
-flexed posture
-freezing at movement initiation
-bladder problems
Autonomic symptoms:
-bladder problems
Mental status changes:
-dementia at later stages