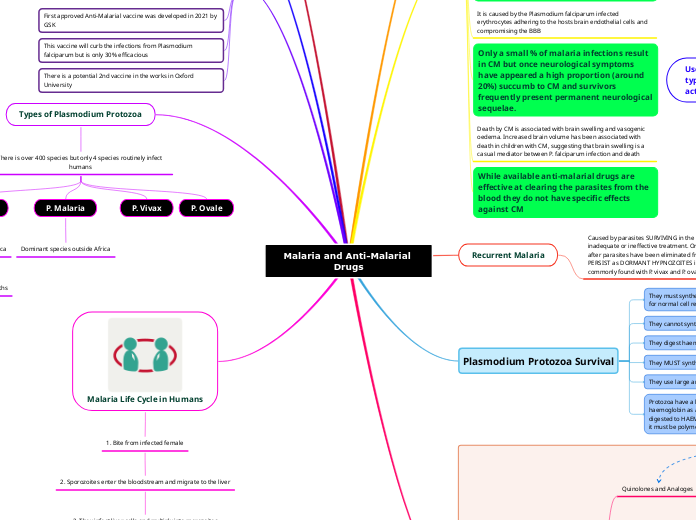
Malaria and Anti-Malarial Drugs
What is Malaria?
Vector-born disease caused by Plasmodium Protozoa
Transmitted from human to human through the bite of an infected female mosquito of the Anopheles species
Effects of Malaria
World's most devastating parasitic infection, effecting 40% of the world's population
According to the WHO: approx. 229 million cases of malaria globally in 2019 and 409,000 deaths
Children account for 2/3 of these deaths
Kills more people than AIDS
There is increasing resistance to established drugs
New Research into the Area
First approved Anti-Malarial vaccine was developed in 2021 by GSK
This vaccine will curb the infections from Plasmodium falciparum but is only 30% efficacious
There is a potential 2nd vaccine in the works in Oxford University
Types of Plasmodium Protozoa
There is over 400 species but only 4 species routinely infect humans
P. Falciparum
Dominant species in Africa
Accounts for 95% of deaths
P. Malaria
Dominant species outside Africa
P. Vivax
P. Ovale
Malaria Life Cycle in Humans
1. Bite from infected female
2. Sporozoites enter the bloodstream and migrate to the liver
3. They infect liver cells and multiply into merezoites
4. They then rupture the liver cells and enter the bloodstream and infect red blood cells
5. The multiply in RBC, lyse cells and then infect more RBC
6. Some develop into gametocytes
7. Gametocytes are taken up by a mosquito and infect the insect and continue on the life cycle
Symptoms of Malaria
Central: Headache
Systemic: fever
Muscular: fatigue and pain
Back pain
Skin: chills and sweating
Respiratory: dry cough
Spleen enlargement
Stomach: Nausea and vomitting
Cerebral Malaria
CM is the most virulent and deadliest manifestations of malaria.
It is caused by the Plasmodium falciparum infected erythrocytes adhering to the hosts brain endothelial cells and compromising the BBB
Only a small % of malaria infections result in CM but once neurological symptoms have appeared a high proportion (around 20%) succumb to CM and survivors frequently present permanent neurological sequelae.
Death by CM is associated with brain swelling and vasogenic oedema. Increased brain volume has been associated with death in children with CM, suggesting that brain swelling is a casual mediator between P. falciparum infection and death
While available anti-malarial drugs are effective at clearing the parasites from the blood they do not have specific effects against CM
Recurrent Malaria
Caused by parasites SURVIVING in the blood as a result if inadequate or ineffective treatment. Or symptoms reappear after parasites have been eliminated from the blood but PERSIST as DORMANT HYPNOZOITES in liver cells. This is most commonly found with P. vivax and P. oval infections!
Plasmodium Protozoa Survival
They must synthesise pyrimidines for normal DNA synthesis, for normal cell replication
They cannot synthesis purines
They digest haemoglobin as a source of amino acids
They MUST synthesis folates
They use large amounts of glucose for their own replications
Protozoa have a large food value where it digests the haemoglobin as a source of amino acid. Haemoglobin is digested to HAEM. A buildup of harm is toxic to the parasite so it must be polymerised into non-toxic harm.
MALARIA CHEMOTHERAPY
Quinolones and Analoges
Quinine
Chloroquine
Mefloquine
Primaquine
Protein Synthesis Inhibitors
Cytotoxic Antibiotics
Doxyclycine
Clindamycin
Anti-folates
sulphadoxine
Pyrimethamine
Atovaquone and Proganaul
Artemisinin and derivatives
Artemisinin
Artesunate
Arteflene
Artemether
ACT
Quinolones and Analogs
Used for:
treatment of acute attacks - targeting the parasite in the blood stage
Treatment of prophylaxis - targeting merozites emerging from the liver cells and breaking the link between liver and blood stage
RADICAL CURE
some act on gametocytes and prevent transmission by the mosquito
Mechanism of action

CHLOROQUININE, QUININE, MEFLOQUININE
HAEMOGLOBIN is degraded to HAEM which is polymerised to NON-TOXIC HAEM in the food vacuole of the parasite. These drugs inhibit the enzyme HAEM POLYMERASE so that there is a build up of TOXIC HAEM in the parasite
Chloroquinine is also a DMARD
Quinine is found in sparkling water and anadin tablets
QUININE
1st effective treatment against malaria and effective against all 4 species
Kills gametocytes of P. Vivax and P. Malariae, used in treatment of severe illness
Usually taken with 1 of 3 other drugs - doxycycline, tetracycline or clindamycin
SIDE EFFECTS: hypoglycaemia, bitter taste, cinchonism, hypotension, cardiac arrhythmias
CHLOROQUININE
More Effective than Quinine
Side effects are usually less severe than quinine: nausea and vomitting, dizziness and blurring of vision
RESISTANCE is a major problem - P. Falciparum
Mefloquinine
Used when there is chlorquinine resistant P. Falciparum
Long half-life , only drug that can be taken during pregnancy
SAFETY LABEL - NEUROLOGICAL EFFECTS CAN OCCUR DURING AND PERMANENTLY AFTER USE!!!
Side effects: NEUROPSYCHIATRIC SYMPTOMS
PRIMAQUININE
Radical Cure for vivax and ovale
Mechanism unclear - ROS involvement
G6PD metabolic disorder - individuals that suffer with this can develop haemolytic anaemia if taking primaquine
PROTEIN SYNTHESIS INHIBITORS
Use of cytotoxic antibiotics to work as protein synthesis inhibitors
MOA: Reversible binding of the 30S ribosome and inhibits peptide synthesis
Clindamycin
DOXYCYCLINE - tetracycline antibiotic
Used in acute attack, slow acting drug so typically used in combination with fast acting
ANTI-FOLATES
Malaria parasites need to synthesise folates de novo.
Acute Attacks - chloroquinine resistant P falciparum
Anti-folate drugs target 2 enzymes
ATOVAQUONE
Inhibits the mitochondrial electron transport chain
Use both prophylaxis and treatment. Activity against blood stage and the non-dormant liver form P. Falciparum
Used with proguanil as proguanil potentiates the action of atovaquone and prevents the development of resistance
ARTEMISININ
First line therapy now for the treatment of malaria is combination of artemisinin and its semi-synthetic derivatives with other drugs mentioned
Poorly soluble in water - poor bioavailability
MOA: Appears to act by binding to iron, causing the breakdown of peroxide bridges, leading to formation of free radicals that damage parasite proteins.
1. Haeme interacts with endoperoxide bridge in artemisinin
2. Release of free radicals
3. Binds with membrane protein
4. Causes lipid peroxidation
5. Damages ER
6. Inhibits protein synthesis
7. Lysis of the parasite