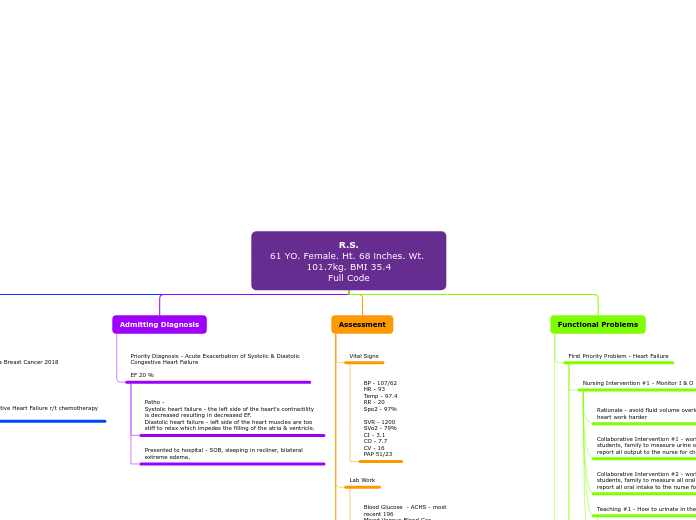
R.S.
61 YO. Female. Ht. 68 inches. Wt. 101.7kg. BMI 35.4
Full Code
Medical History
Type 1 Diabetes 2015
Atypical lobular hyperplasia Breast Cancer 2018
Right Mastectomy 2019
Anxiety
Asthma (Chronic)
Hypertension
Hypotension
Hypothyroid (chronic)
Systolic & Diastolic Congestive Heart Failure r/t chemotherapy from breast cancer
Admitting Diagnosis
Priority Diagnosis - Acute Exacerbation of Systolic & Diastolic Congestive Heart Failure
EF 20 %
Patho -
Systolic heart failure - the left side of the heart's contractility is decreased resulting in decreased EF.
Diastolic heart failure - left side of the heart muscles are too stiff to relax which impedes the filling of the atria & ventricle.
Presented to hospital - SOB, sleeping in recliner, bilateral extreme edema,
Assessment
Vital Signs
BP - 107/62
HR - 93
Temp - 97.4
RR - 20
Spo2 - 97%
SVR - 1200
SVo2 - 79%
CI - 3.1
CO - 7.7
CV - 16
PAP 51/23
Lab Work
Blood Glucose - ACHS - most recent 196
Mixed Venous Blood Gas -
ABE - 7.3
PCO2 - 55
pH - 7.41
PO2 - <43
SVO2 - 75.2
Abnormal Lab Findings
BUN - 29
CREAT - 1.19
Na - 135
K+ - 3.1
Protein - 6.3
GFR - 52
Proth - 14.6
RBC - 3.76
Plat - 133
Lump - 0.39
High
Low
normal
Cardiovascular
Warm to the touch, normal color, no odor, skin turgor is normal, hair is normal, nails are normal - cap refill delayed
Heart WNL - sinus rhythm - auscultation - no extra heart sounds
normal JV - no distention - Swanline in R- IJ
Radial Pulses - WNL Pedal Pulses - +1 weak
Right Arm has lymphedema
Left Arm edema has decreased
Lower extremities - mild edema - bilaterally
Pain 9/10 - headache causing nausea, sleep makes it better
Respiratory
Thorax is symmetrical, lung sounds diminished No crackle heard See vital signs for RR/Spo2
bowel sounds hypoactive
See SBAR for more information
Functional Problems
First Priority Problem - Heart Failure
Nursing Intervention #1 - Monitor I & O
Rationale - avoid fluid volume overload - do not make a sick heart work harder
Collaborative Intervention #1 - work with other nurses, techs, students, family to measure urine output for the patient - report all output to the nurse for charting
Collaborative Intervention #2 - work with other nurses, techs, students, family to measure all oral intake for the patient - report all oral intake to the nurse for charting
Teaching #1 - How to urinate in the hat
Rationale - We need to collect the urine in a hat for measurement
Teaching #2 - Do not dump urine with out measuring
Rationale - We need to measure all urine to be able to identify and prevent fluid volume overload
Nursing Intervention #2 - Prevent atelectasis
Rationale - CHF patients are at risk for atelectasis when they are in the hospital due to being sedentary
Collaborative Intervention #1 - encourage the patient to work with PT/OT, techs, students, or other nurses to ambulate as much as possible
Collaborative Intervention #2 - encourage patient to utilize deep breathing / incentive spirometer alone, with family or staff help
Teaching #1 - benefits of movement
rationale - to prevent atelectasis and work the edema out of the interstitial spaces.
Teaching #2 - safety when ambulating - non slip socks, utilize any assistive devices, walk with someone not alone
Rationale - to prevent falls
SMART goal - keep systolic blood pressure over 100 for entirety of hospital stay and once at home.
systolic blood pressure over 100 the entirety of my shift, this is a continued goal.
Second Priority Problem - At risk for further complications hypokalemia & AKI
Nursing Intervention#1 - Monitor Lab Work
Rationale - monitoring lab work will tell the nurse what interventions need to be done to fix the specific lab levels
Collaborative Intervention #1 - work with doctor and pharmacy to provide potassium supplementation.
Collaborative Intervention #2 - work with patient and family for at home medication adherence
Teaching #1 - teach patient organization for medication times, make a calendar/schedule
rationale - medication adherence
Teaching #2 - Teach patient about medication resources
rationale - medication adherence
Nursing Intervention#2 - Regulate Patient Nutrition
Rationale - keep potassium and sodium levels under control
Collaborative Intervention #1 - work with dietary to provide a low sodium, high potassium, cardiac diet
Collaborative Intervention #2 - work with patient and family to implement a heart healthy, kidney healthy diet.
Teaching #1 - teach patient which foods are high in potassium leafy greens, nuts, etc. - teach patient about low sodium - salt substitutes
rationale - regulate labs, prevent dysrhythmias, lead a healthy life
Teaching #2 - Teach patient to read nutrition labes
rationale - teach the patient to take charge of their nutrion
SMART goal - bring potassium level to normal limits (3.5-5) before discharge.
Goal continued, medicated during my shift with 40meq potassium po and 10meq IV. Brought level up to 3.2.