Cardiovascular Drugs
Pipes (blood vessels)
HMG-CoA
Statins
Blocks cholesterol synthesis
Monitor liver
Rhabdo & cataracts
bile acid sequesterase
Cholestyramine
Binds with bile
4-6x/day
Pt. compliance issues
Limits fat sol. Vitamin absorption
cholesterol absorp. inhibitors
Ezetimibe
lower cholesterol absorption
Take alone. 2-4 hrs.
bloating, cramping
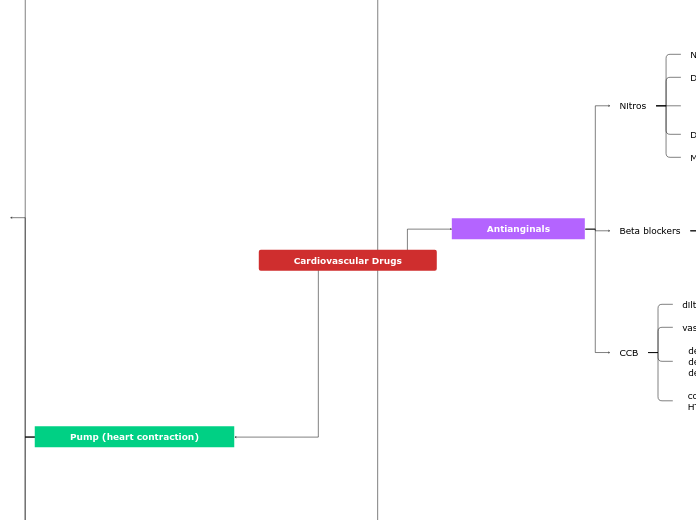
Antianginals
Nitros
Nitroglycerin, Nitro paste
Dilates blood vessels
decrease preload
decrease workload
Dizziness, headache, SOB
Monitor HR & BP
Beta blockers
-lol, metoprolol
Tx. for HTN, angina
decrease HR
decrease contractility
decrease BP
Subtopic
CCB
diltiazem, verapamil, -pine
vasodilation
decrease workload
decrease HR
decrease O2 needs
coronary artery spasms
HTN, angina
Plasma (blood)
Antiplatelets
Slippery platelets
CVD, CAD, PAD
Know pt. hx.
Good pt. teaching
Aspirin, Plavix, Brillinta
Anticoagulants
Interferes w/ clotting cascade
PE, DVT, A-fib
Know pt. hx.
Antidotes: warfarin=Vit. K
heparin=protamine sulfate
Eliquis & Xarelto=Andexxa
Anemia Tx.
iron deficiency
ferrous-
elevate serum iron
Z-track or PO
Diarrhea, dark stools
Other anemias
Megaloblastic: Folic acid, Vit. B12
sickle cell: hydroxyurea, ABX
Monitor GI & bone marrow
Epo stimulation
epoetin alfa
CKD, dialysis, cancer
IV or subq only
Monitor: HTN, seizures, Hgb level
Pump (heart contraction)
AntihypoTN
Increase BP, blood volume,
& heart contraction
Stimulate SNS response
Short term: Norepi, epi,
phenylephrine (all IV)
Long term: midodrine (PO)
AntiHTN
ACE inhibitors
-pril
block angiotensin-converting
enzyme=no Angiotensin II
decrease BP
decrease aldosterone
treats HTN
take on empty stomach
ARBs
-sartan
block angiotensin II
receptors
lowers BP
AE: low BP S&S
renal damage
CCB
-dipine
inhibit movement of Ca+
in action potential Phase 2
slows contractility & impulses
dilates arteries
AE: low BP S&S
vasodilators
hydralazine, minoxidil, nitroprusside
used in severe HTN emergencies
lower BP, causes tachycardia
monitor pt. w/ CAD, CHF, tachycardia
Diuretics
hydrochlorothiazide, spironolactone
increase Na+ & water excretion
frim kidneys
1st line med for HTN
Pt. ed. reasons for med
& compliance
SNS blockers
Beta-blockers -lol
Block SNS response
lower BP, lower HR
check HR before administering
CHF
HCN blockers
Ivabradine
slows SA node
improves cardiac output
AE: bradycardia, HTN, a-fib
caution w/ A-fib
& heart block
PDE inhibitors
Milrinone. IV only
increase contraction &
increase SNS stim.
AE: ventricle arrhythmias
Don't give with Lasix
Cardiac Glycosides
Digoxin
make heart beat
slower & harder
check heart rate
dig toxicity
Antiarrhythmics
Class I
Lidocaine, flecainide
Phase 0: block Na+
channels
Tx for V-tach
Class II
Beta blockers -lol
Phase 4: prolongs rest phase
decrease BP, workload
Tx for SVT, PVC
Class III
amiodarone, sotolol
Phase 3: block
K+ channels
Tx for V-fib, pulseless v-tach,
cardiac arrest
Class IV
diltiazem, verapamil (CCB)
Phase 2: block calcium channels,
delay phase 1&2
Tx for HTN, angina