CKD/renal failure
Monitoring and evaluation
Stages 1-3: 20-30 min 6 monthly
Stages 4-5 post transplant 20-30 min 3 monthly
Stage 5, D, PD- 45-60min monthly
SGA at all stages
Risk factors:
Diabetes+++, HTN, fam hx, obesity, smoking, >60yo, ATSI, Hx acute KD, recurring UTI's.
Anthro
Dry weight, wet weight
Pre and post dialysis. If continuing to lose dry weight= losing fat and muscle. If coming off dialysis and still "wet" = losing fat and muscle NOT fluid.
BW should be adjusted if wt is <95% or >115% of IBW
Biochem
K+ (3.5-5.5mmol/L)
Low= weakness, cellular impairement
High = irregular HB, nausea, weak pulse
PO4 (0.8-1.4mmol/L
High = itching, Ca+ and PO4 deposit in tissues
Diet
AGHE guidelines & HEHP
Na
Stage 1- 87mmol/L/day
Stage 2- 87mmol/L/day
Stages 3-5 <100mmol/day avoid salt substitutes (high in K)
Stage 5 <100mmol/L/day " "
Transplant <100mmol/L/day. If stable, restrict Na to 80-100mmol/L/day
Fluid
Fluid restriction? Dialysis? MUST meet restriction amount
K (Potassium)
Stage 1 & 2 = 2800-3800mg/day
Stage 3-5 Reduce to maintain normal serum level. Limit to 1mmol/kg IBW if serum is >6mmol/L
AJKD guideline: CKD 3-5D= 3 day food record preferred method to assess diet: on dialysis and NOT on dialysis
AJKD guidelines: CKD 3-5 or CKD5D(2D) 24hr recall, food frequency questionnaire = alternative methods
All stages= healthy eating
Stages 1-3= wt management and mx comorbidities
stages1-5 manage sodium
stage 3- moderate protein and malnutrition
stages 4-5 protein per DN prescritption- HIGHER if on dialysis!
PO4
foods high in PO4 = nuts, bacon, PB, cola and pepsi, beer, chocolate, muesli
PO4 from plant based = lower absorption (70%) from animal products = 100% absorption. FRESH is best, limit TA + animal proteins
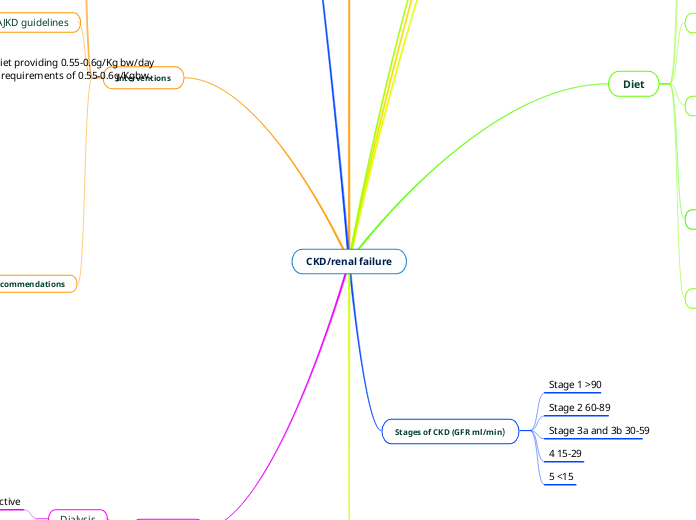
Stages of CKD (GFR ml/min)
Stage 1 >90
Stage 2 60-89
Stage 3a and 3b 30-59
4 15-29
5 <15
Management
Stage 3 = prevent volume depletion, prevent bone-mineral disease, prevent electrolyte disturbances, prevent malnutrition
Stage 4-5= manage metabolic disturbances, prevent anaemia, malnutrition and acidosis, manage HTN, nausea and fluid balance
Client hx
Medical
Previous and current: surgery, dialysis, stage of CKD
Medication:
Anti-hypertensives (ACE inhibitors) eg PRIL
Diuretics (frusemide)
Renins (to lower K+)
Immunosuppressants (Cyclosporin, mycophenolate, Azathioprine)
Iron supps (EPO)
Steroids ("one")
Calcitriol (Vit D)
Interventions
Fluid restriction
Remove excess fluid, swap cereal for toast (no milk), swap fresh fruit for dried fruit, break up water consumption throughout the day
Decrease sodium
Swap table salt for herbs and spices, swap convenience foods (T/A, servo food) for sandwiches, nut bars/un-slated trail mix, fruit, halve portions of meals eating out (eg pub)
Decrease K
Foods high in K+ = Sweetened beverages, muffins, hot chips, ice cream, sausage rolls.
If K+ is the problem, address discretionary. They're absorbed quicker, Therefore even if they're not as high as a fruit they're eating, whatever amount is in them will all be absorbed compared to a "healthier" food that's initially higher in K+.
Low K+ fruits = berries! passionfruit, apple, pear, melon, grapes, mandarin, watermelon
High K+ fruits = banana, dried fruit, pineapple, peach, mango, kiwi
Low K+ veg = cabbage, asparagus, tomato, carrots, capsicum, mushrooms, zucchini, onion, canned beetroot, cauliflower.
High K+ = avocado, corn, baked beans, veg juice, pumpkin
Limit to 1 starchy veg/day
AJKD guidelines
Fruits and vegetables to decrease BW, BP and net acid production. Mediterranean diet in CKD 1- NOT on dialysis, with or without dyslipidemia; improve lipid profiles
CKD 3-5D (2D) at risk of protein-energy wasting, minimum 3 month trial of ONS to improve nutritional status
Protein- NOT on dialysis, WITH diabetes- 0.6-0.8g/Kgbw + glycemic control
CKD 3-5 metabolically stable NOT on dialysis and WITHOUT diabetes= low protein diet providing 0.55-0.6g/Kg bw/day OR a very low protein diet 0.28-0.43g/Kgbw + additional AA analogs to meet protein requirements of 0.55-0.6g/Kgbw.
Nutrition recommendations
stages 1-3CKD
Energy= for ideal BW (if diab neuropathy: <50% CHO)
K+ 2800-3800mg/day
stage 4
Energy= minimum 146kJ/Kg IBW. 125-146kJ/kg IBW >60years of age
Protein 0.75-1.0g/Kg IBW
Stage 5 haemodialysis
Energy <60yo = 146Kj/Kg IBW >60yo = 125-146Kj/KgIBW
K+ = <100mmol/Kg IBW
Fluid 500ml
Stage 5 Peritoneal dialysis
energy= 146kJ/kg IBW + glucose from dialysis. Acute illness = >146kJ/Kg IBW
protein= 1.2g/Kg IBW. Acute illness >1.3g/Kg IBW
Fluid overloaded or HTN 800ml + PDUO
ONLY decrease K+ and PO4 if serum levels high
Protein requirements increase at commencement of dialysis
Treatment
Dialysis
Peritoneal (optimal as less restrictive diet)
Haemodialysis (machine) 3x 4-5hours / week. If at home= 7-9h per night
Transplant