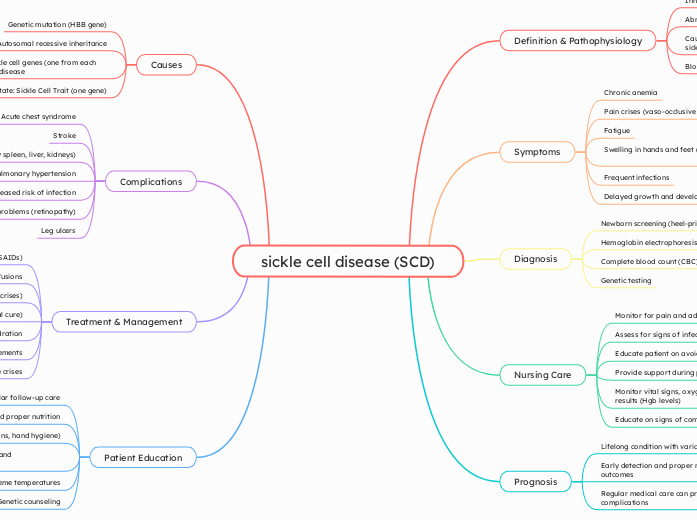
sickle cell disease (SCD)
Definition & Pathophysiology
Inherited blood disorder
Abnormal hemoglobin (Hemoglobin S)
Causes red blood cells to become rigid, sticky, and sickle-shaped
Block blood flow and cause ischemia
Symptoms
Chronic anemia
Pain crises (vaso-occlusive episodes)
Fatigue
Swelling in hands and feet (dactylitis)
Frequent infections
Delayed growth and development
Diagnosis
Newborn screening (heel-prick test)
Hemoglobin electrophoresis
Complete blood count (CBC)
Genetic testing
Nursing Care
Monitor for pain and administer medications
Assess for signs of infection
Educate patient on avoiding triggers
Provide support during pain crises
Monitor vital signs, oxygen saturation, and lab results (Hgb levels)
Educate on signs of complications
Prognosis
Lifelong condition with variable severity
Early detection and proper management improve outcomes
Regular medical care can prevent or manage complications
Causes
Genetic mutation (HBB gene)
Autosomal recessive inheritance
Must inherit two sickle cell genes (one from each parent) to have the disease
Carrier state: Sickle Cell Trait (one gene)
Complications
Acute chest syndrome
Stroke
Organ damage (especially spleen, liver, kidneys)
Pulmonary hypertension
Increased risk of infection
Eye problems (retinopathy)
Leg ulcers
Treatment & Management
Pain management (opioids, NSAIDs)
Blood transfusions
Hydroxyurea (reduces crises)
Bone marrow transplant (potential cure)
Hydration
Folic acid supplements
Oxygen therapy during acute crises
Patient Education
Importance of regular follow-up care
Hydration and proper nutrition
Infection prevention (vaccinations, hand hygiene)
Recognizing early signs of crises and complications
Avoiding high altitudes and extreme temperatures
Genetic counseling