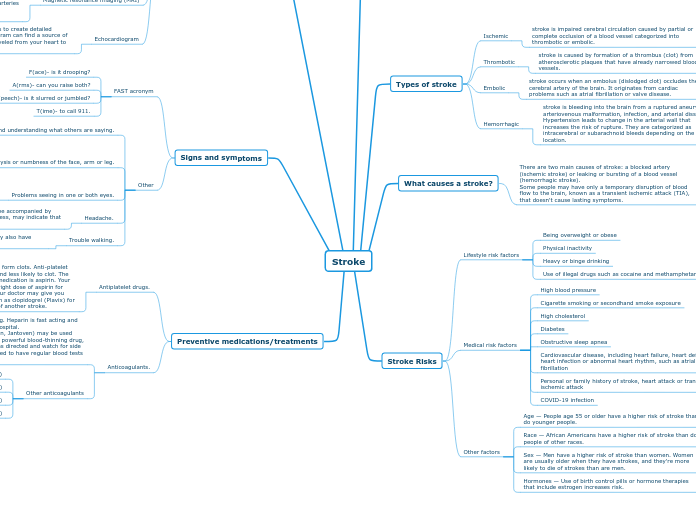
Stroke
What is a stroke?
A stroke occurs when the blood supply to part of your brain is interrupted or reduced, preventing brain tissue from getting oxygen and nutrients. Brain cells begin to die in minutes.
Types of stroke
Ischemic
stroke is impaired cerebral circulation caused by partial or complete occlusion of a blood vessel categorized into thrombotic or embolic.
Thrombotic
stroke is caused by formation of a thrombus (clot) from atherosclerotic plaques that have already narrowed blood vessels.
Embolic
stroke occurs when an embolus (dislodged clot) occludes the cerebral artery of the brain. It originates from cardiac problems such as atrial fibrillation or valve disease.
Hemorrhagic
stroke is bleeding into the brain from a ruptured aneurysm, arteriovenous malformation, infection, and arterial dissection. Hypertension leads to change in the arterial wall that increases the risk of rupture. They are categorized as intracerebral or subarachnoid bleeds depending on the location.
What causes a stroke?
There are two main causes of stroke: a blocked artery (ischemic stroke) or leaking or bursting of a blood vessel (hemorrhagic stroke).
Some people may have only a temporary disruption of blood flow to the brain, known as a transient ischemic attack (TIA), that doesn't cause lasting symptoms.
Stroke Risks
Lifestyle risk factors
Being overweight or obese
Physical inactivity
Heavy or binge drinking
Use of illegal drugs such as cocaine and methamphetamine
Medical risk factors
High blood pressure
Cigarette smoking or secondhand smoke exposure
High cholesterol
Diabetes
Obstructive sleep apnea
Cardiovascular disease, including heart failure, heart defects, heart infection or abnormal heart rhythm, such as atrial fibrillation
Personal or family history of stroke, heart attack or transient ischemic attack
COVID-19 infection
Other factors
Age — People age 55 or older have a higher risk of stroke than do younger people.
Race — African Americans have a higher risk of stroke than do people of other races.
Sex — Men have a higher risk of stroke than women. Women are usually older when they have strokes, and they're more likely to die of strokes than are men.
Hormones — Use of birth control pills or hormone therapies that include estrogen increases risk.
Medical testing/diagnosis
A physical exam
Your doctor will do a number of tests you're familiar with, such as listening to your heart and checking your blood pressure. You'll also have a neurological exam to see how a potential stroke is affecting your nervous system.
Blood tests
You may have several blood tests, including tests to check how fast your blood clots, whether your blood sugar is too high or low, and whether you have an infection.
Computerized tomography (CT) scan
A CT scan uses a series of X-rays to create a detailed image of your brain. A CT scan can show bleeding in the brain, an ischemic stroke, a tumor or other conditions. Doctors may inject a dye into your bloodstream to view your blood vessels in your neck and brain in greater detail (computerized tomography angiography).
Magnetic resonance imaging (MRI)
An MRI uses powerful radio waves and magnets to create a detailed view of your brain. An MRI can detect brain tissue damaged by an ischemic stroke and brain hemorrhages. Your doctor may inject a dye into a blood vessel to view the arteries and veins and highlight blood flow (magnetic resonance angiography or magnetic resonance venography).
Echocardiogram
An echocardiogram uses sound waves to create detailed images of your heart. An echocardiogram can find a source of clots in your heart that may have traveled from your heart to your brain and caused your stroke.
Signs and symptoms
FAST acronym
F(ace)- is it drooping?
A(rms)- can you raise both?
S(peech)- is it slurred or jumbled?
T(ime)- to call 911.
Other
Trouble speaking and understanding what others are saying.
You may experience confusion, slur your words or have difficulty understanding speech.
Paralysis or numbness of the face, arm or leg.
You may develop sudden numbness, weakness or paralysis in your face, arm or leg. This often affects just one side of your body. Try to raise both your arms over your head at the same time. If one arm begins to fall, you may be having a stroke. Also, one side of your mouth may droop when you try to smile.
Problems seeing in one or both eyes.
You may suddenly have blurred or blackened vision in one or both eyes, or you may see double.
Headache.
A sudden, severe headache, which may be accompanied by vomiting, dizziness or altered consciousness, may indicate that you're having a stroke.
Trouble walking.
You may stumble or lose your balance. You may also have sudden dizziness or a loss of coordination.
Preventive medications/treatments
Antiplatelet drugs.
Platelets are cells in your blood that form clots. Anti-platelet drugs make these cells less sticky and less likely to clot. The most commonly used anti-platelet medication is aspirin. Your doctor can help you determine the right dose of aspirin for you. After a TIA or minor stroke, your doctor may give you aspirin and an antiplatelet drug such as clopidogrel (Plavix) for a period of time to reduce the risk of another stroke.
Anticoagulants.
These drugs reduce blood clotting. Heparin is fast acting and may be used short-term in the hospital.
Slower-acting warfarin (Coumadin, Jantoven) may be used over a longer term. Warfarin is a powerful blood-thinning drug, so you'll need to take it exactly as directed and watch for side effects of bleeding. You'll also need to have regular blood tests to monitor warfarin's effects.
Other anticoagulants
Dabigatran (Pradaxa)
Rivaroxaban (Xarelto)
Apixaban (Eliquis)
Edoxaban (Savaysa)