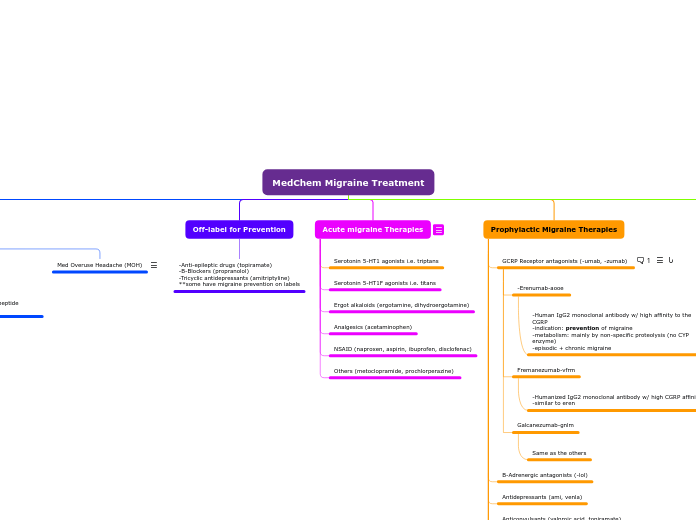
MedChem Migraine Treatment
Migraine Treatment
Ergot alkaloids
-broad spectrum of activity on receptors (5HT, alpha, dopamine)
-inhibit trigeminal neurotransmission peripherally + centrally
-vasoconstriction
-similar to triptans
-indole group
Agents: Ergotamine/Dihydroergotamine
CI:
-Renal/hepatic failure
-coronary, cerebral, peripheral vascular disease
-uncontrolled hypertension
-pregnancy
-nursing mother
-less efficacious vs. triptans
-very low oral bio, +caffeine to improve rate/extent of absorption
-N/V, chest tightness, ergotism
Serotonin 5-HT1F agonists (ditans)
Lasmiditan
-inhibit release of CGRP
-inhibit cAMP signaling cascade
-NO constriction
Serotonin 5-HT1 agonists (triptans)
2nd gen has higher oral bioavailability (basically all except suma)
SAR: Indole group
Agents
Suma:
-significant 1st pass effect
-chest discomfort/tightness/pressure/pain
-CI w/ CAD & angina
-selective agonists of 5HT1B & 5HT1D receptors
-vasoconstriction (makes it effective in early attack)
-inhibition of vasoactive peptide release from trigeminal neurons (these cause inflammation so it inhibits it)
-inhibition of transmission thru 2nd order neurons
-all triptans have greater efficacies vs. ergot alkaloids
Prophylactic Migraine Therapies
Transcranial Magnetic Stimulation
TMS is not effective for chronic but for acute it has shown to be effective.
Others (histamine, Mg, MIG-99, riboflavin (B2))
Botox
Neurotoxin for chronic migraine. Injection, prevent attacks up to 90 days
-interferes with ACh by breaking a protein req for its release. Stops the activation of pain-receptors
Serotonin 5HT1 agonists (triptans)
NSAIDs
-block COX2 --> reduce prostaglandins
-PGE2/PGI2 --> reduce threshold to stimulation for nociceptors --> peripheral sensitization
Anticonvulsants (valproic acid, topiramate)
Antidepressants (ami, venla)
B-Adrenergic antagonists (-lol)
GCRP Receptor antagonists (-umab, -zumab)
- abortive + preventative migraine treatment
- No vasoconstriction
- Telcagepant, Rimegepant, Ubrogepant
- MOA: Reversibly blocks CGRP receptor
Antibodies Against CGRP:
-Eptinezumab
- MOA: binds to CGRP and blocks its binding to the receptor
- humanized monoclonal antibody
- ADEs: angioedema, urticaria, facial flushing, rash
Galcanezumab-gnlm
Same as the others
Fremanezumab-vfrm
-Humanized IgG2 monoclonal antibody w/ high CGRP affinity
-similar to eren
-Erenumab-aooe
-Human IgG2 monoclonal antibody w/ high affinity to the CGRP
-indication: prevention of migraine
-metabolism: mainly by non-specific proteolysis (no CYP enzyme)
-episodic + chronic migraine
Acute migraine Therapies
Use of opioid analgesic drugs to treat migraine is controversial
Others (metoclopramide, prochlorperazine)
NSAID (naproxen, aspirin, ibuprofen, disclofenac)
Analgesics (acetaminophen)
Ergot alkaloids (ergotamine, dihydroergotamine)
Serotonin 5-HT1F agonists i.e. titans
Serotonin 5-HT1 agonists i.e. triptans
Off-label for Prevention
-Anti-epileptic drugs (topiramate)
-B-Blockers (propranolol)
-Tricyclic antidepressants (amitriptyline)
**some have migraine prevention on labels
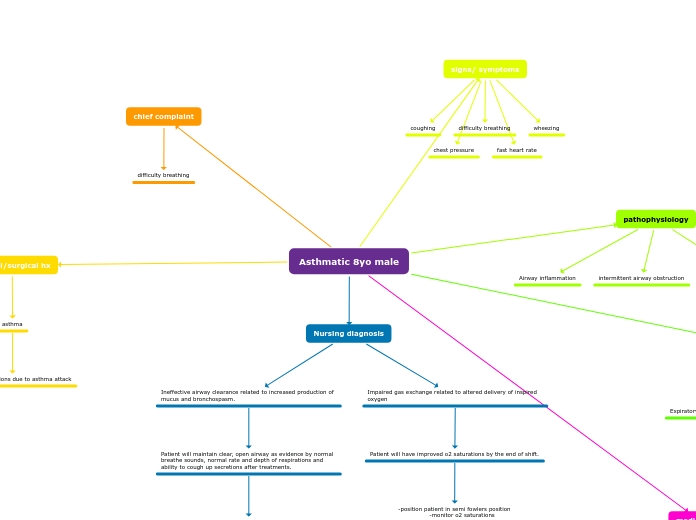
Etiology & Pathophys
- Trigeminal nerves release vasoactive peptides that:
- Induce intracranial vasodilation
- plasma protein extravasation
- neurogenic inflammation
Med Overuse Headache (MOH)
- Deterioration of pre-existing headache syndrome due to overusing acute painkilling txt
- episodic --> daily
- prolongation of migraine w/ ergots, triptans, opioids, NSAIDs, analgesics, combos
- abrupt withdrawal preferred
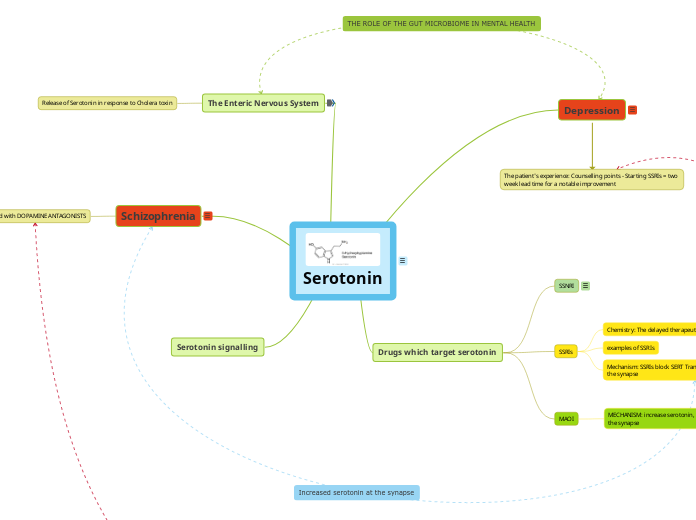
Serotonin Receptors
-Vascular smooth muscle cells (constriction)
-trigeminal fiber presynaptic boutons (modulate peptide release)
Vasoactive peptides
-Calcitonin gene-related peptide (CGRP)
-Neurokinin A
-Substance P
-Pituitary adenylate cyclase-activating peptide (PACAP)
CGRP & PACAP
-Induce migraine when IV
-cause dilation of cephalic arteries