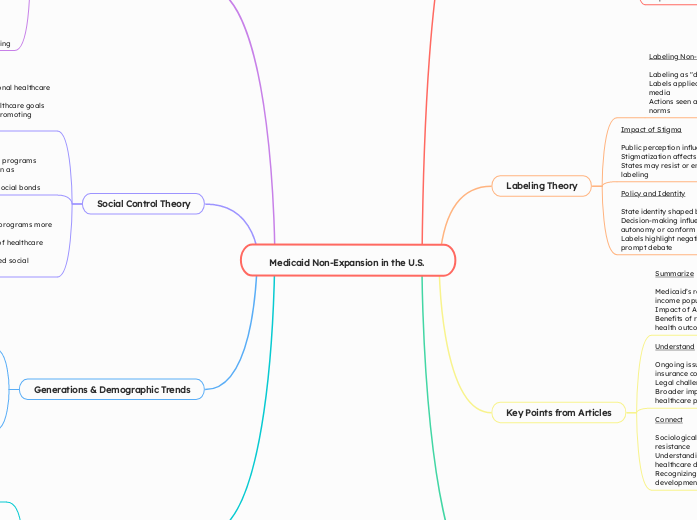
Medicaid Non-Expansion in the U.S.
Reasons for Non-Expansion
Ideological Opposition
Belief in limited government
Fear of increased federal control
Emphasis on self-reliance
Financial Concerns
Long-term cost worries
Budgetary impacts
Potential increase in state expenses
Administrative Challenges
Complexity of program management
Increased bureaucratic demands
Resource allocation issues
Economic & Health Consequences
Higher emergency care costs
Poor health outcomes
Increased uninsured rates
Work Incentives
Concerns about reducing work incentives
Debate over "able-bodied" adults
Impact on labor market participation
Labeling Theory
Labeling Non-Expanding States
Labeling as "deviant" or "outliers"
Labels applied by proponents of expansion and media
Actions seen as contrary to broader healthcare norms
Impact of Stigma
Public perception influenced by labels
Stigmatization affects political pressure
States may resist or entrench further based on labeling
Policy and Identity
State identity shaped by labels
Decision-making influenced by desire to maintain autonomy or conform
Labels highlight negative consequences and prompt debate
Key Points from Articles
Summarize
Medicaid’s role in providing healthcare to low-income populations
Impact of ACA on expanding Medicaid
Benefits of reducing uninsured rates and improving health outcomes
Understand
Ongoing issues with healthcare access and insurance coverage
Legal challenges to restrictive policies
Broader implications for social equity and healthcare policy
Connect
Sociological theories provide insights into policy resistance
Understanding structural and conflict dynamics in healthcare debates
Recognizing the role of social change in policy development
Population Change & Demographic Transition
Current Demographic Context
Aging Population: Increased demand for healthcare services
Racial and Ethnic Diversity: Addressing healthcare disparities
Impact of Demographic Transition
Economic Implications: Supporting economic stability and growth
Stage of Transition: Adapting healthcare to support an aging and diverse population
Differential Association Theory
Learning Resistance
Interaction with similar ideological groups
Influence from conservative networks
Adoption of anti-expansion narratives
Reinforced Beliefs
Policy decisions shaped by peer influence
Continuous reinforcement through social and political channels
Resistance becomes a shared norm among like-minded states
Implications
Collective stance against Medicaid expansion
Ideological conformity within networks
Perpetuation of resistance through social learning
Social Control Theory
Weak Bonds to Norms
Indicating weak attachment to national healthcare values
Lack of integration with federal healthcare goals
Limited connections to institutions promoting Medicaid
Encouraging Conformity
Strengthening social ties to national programs
Federal incentives and public opinion as mechanisms
Advocacy efforts to build stronger social bonds
Policy Dynamics
States with stronger ties to federal programs more likely to expand
Efforts to reinforce societal norms of healthcare equity
Potential shift in policy with increased social pressure
Generations & Demographic Trends
Generational Impact
Older Generations: Increased need for healthcare services
Younger Generations: Higher uninsured rates, need for safety net
Healthcare Access Across Generations
Elderly: Access to long-term care and chronic disease management
Middle-aged: Preventive care and chronic condition treatment
Young Adults and Children: Pediatric and mental health services
Demographic and Social Change
Social Equity and Healthcare Access
Reducing Health Disparities: Leveling the playing field in healthcare
Economic Stability: Supporting low-income workers and economic growth
Specific Aspects in Context
Generational Needs: Rural vs. urban healthcare access
Improving Health Outcomes: Increased access to preventive care and better long-term outcomes