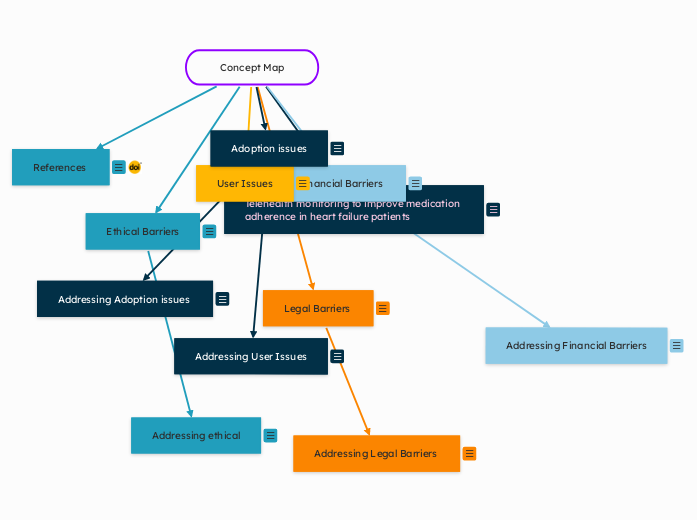
Concept Map
References
References
(Serrano et al., 2023) (Solimini et al., 2021) ("Financial Impact of Telehealth: Rural Chief Financial Officer Perspectives," 2022) (Kruse & Heinemann, 2022)
References
Financial impact of telehealth: Rural chief financial officer perspectives. (2022). The American Journal of Managed Care, 28(12), e436–e443. https://doi.org/10.37765/ajmc.2022.89279
Kruse, C., & Heinemann, K. (2022). Facilitators and barriers to the adoption of telemedicine during the first year of covid-19: Systematic review. Journal of Medical Internet Research, 24(1), e31752. https://doi.org/10.2196/31752
Serrano, L., Maita, K. C., Avila, F. R., Torres-Guzman, R. A., Garcia, J. P., Eldaly, A. S., Haider, C. R., Felton, C. L., Paulson, M. R., Maniaci, M. J., & Forte, A. J. (2023). Benefits and challenges of remote patient monitoring as perceived by health care practitioners: A systematic review. The Permanente Journal, 27(4), 100–111. https://doi.org/10.7812/tpp/23.022
Solimini, R., Busardò, F., Gibelli, F., Sirignano, A., & Ricci, G. (2021). Ethical and legal challenges of telemedicine in the era of the covid-19 pandemic. Medicina, 57(12), 1314. https://doi.org/10.3390/medicina57121314
Adoption issues
Some of the largest adoption issues with Telehealth, are technically challenged staff, resistance to change, cost reimbursement, and education level of patient (Kruse & Heinemann, 2022)
Addressing User Issues
Some issues that can arise are technology issues. We may have the internet down, or connection is slow. This can delay or even hinder patients appointments via Telehealth.
I think regular maintenance on the devices will help with technology issues we may face such as video quality issues or even with the program starting. Sometimes even with maintenance we can’t prevent these issues from happening. In the event that a telemedicine visit has to be cancelled, we will immediately schedule an in person visit with the patient within 48 hours from missed or interrupted visit to ensure patients needs are met and ensure they are still receiving quality of care.
Addressing Adoption issues
An issue that may arise within my practice environment is technically challenged staff and resistance to change. A lot of the staff are older and may have issues understanding how to complete the Telehealth visits.
Training will be implemented for each individual during startup and for a few months while the program is being implemented. This can have a positive impact on technically challenged staff and staff that is resistant to change because it gives them the support they need to feel confident in completing Telehealth visits and can allow them to be less resistance because they feel supported.
User Issues
Patients diagnosed with heart failure are typically aged 65 and older. This can be an issue when implementing the program if they are having a hard time using the service. They also may not have access to internet services or a smart phone.
Technology issues can also arise with Telehealth. There can be poor internet connectivity, visual or audio disturbances, privacy concerns and inability to create rapport with the provider.
Financial Barriers
Financial barriers can play a big factor in implementing telemedicine. Telehealth would play a big role in assisting individuals diagnosed with heart failure to adhere to their medication regimen but Telehealth is associated with limited reimbursement, low volumes, and an individuals preference for in person visits (“Financial Impact of Telehealth: Rural Chief Financial Officer Perspectives”, 2022)
Low reimbursement can be an issue when providing Telehealth visits for patients with heart failure. It is something that needs to be reviewed to determine if it will be costly to the practice or will the practice be able to sustain while providing Telehealth visits to ensure medication adherence in heart failure patients.
Addressing Financial Barriers
The community clinic is smaller and depends on reimbursement in order to stay in business. Some issues that may arise within the practice is the low reimbursement rates for telemedicine and the upkeep of the technology. Tablets and other smart devices will need to be updated to ensure we have functioning devices to perform the Telehealth visits daily.
An approach we can take with this is to possibly have a contract with the vendors who supplied the devices for certain discounts in order to keep budgets at a fixed price. We can also maintain in person visits as well as
Legal Barriers
Legal issues can also be of concern with Telemedicine. Some legal issues that may arise with telemedicine include costs of services and reimbursement, insurance coverage, virtual prescription of medication, accreditations, licensing, recording, and evaluation of the effectiveness of services including health outcomes and delivery, in terms of quality and cost, individual experience, and program implementation (Solimini et al., 2021)
Remote patients can either benefit or be disadvantaged by virtual care (lack of access to internet, smartphones, or other technology (Solimini et al., 2021)
Providers using Telehealth must be able to practice in the state that they are practicing medicine. Telemedicine can allow providers to cross jurisdictional boundaries. Telehealth can also lead to malpractice when there is breaches of standard of care or where there are unlicensed medical practices.
Telehealth involves increased liability for providers and we have to be aware of that.
Ethical and legal issues related to the practice of Telehealth or telemedicine services still need standard and specific rules of application in order to guarantee equitable access, quality of care, sustainable costs, professional liability, and respect of patient privacy, data protection, and confidentiality (Solimini et al., 2021)
Addressing Legal Barriers
In the practice environment, Telehealth can allow for providers to be at increased liability. Patients can misunderstand information, informed consent can be made without patient fully understanding, or there can be a disconnect between patient and provider due to not coming in for in person visits.
One way we can address this within my practice environment is to allow patients to still come in once a month or how often they desire for in person visits while still monitoring their medication adherence via telemedicine. Informed consent will only be able to be completed at in person visits. This strategy can help to alleviate some liability on the providers in certain situations while still allowing us to monitor patients on a 2 to 3 times per week basis.
Ethical Barriers
Telehealth can raise issues with confidentiality, informed consent, privacy and patient care.
Older adults are the majority of the population diagnosed with heart failure. Patients may not fully understand the nature of Telehealth services or risks involved (Solimini et al., 2021)
Providers can have a hard time protecting patient privacy via Telehealth visits. Privacy has to be maintained the same way it would during an in person visit.
WHO discovered that telemedicine presents special ethical issues such as maintaining the confidentiality of information and privacy of patients and safeguarding integrity of information systems (Solimini et al., 2021)
Confidentiality is a major importance in providing care to patients, patients data must be protected. This can cause a major issue in implementation of telemedicine within the clinic due to risks of breaching patient data and also with obtaining informed consent.
Addressing ethical
In my practice environment, patient confidentiality coulee an issue and also obtaining informed consent.
Patients may not fully understand what they are giving consent to and require additional information. This can lead to misunderstandings about medications and how they should be taking them
An approach we can take with this is to implement teach back methods, carefully explain to each patient about their own individualized care plan and have them confirm the education we taught by repeating it back. This can help to decrease any confusion and reinforce education if needed.
Telehealth monitoring to improve medication adherence in heart failure patients
Telehealth monitoring has been shown to have both benefits and barriers to healthcare management in patients.
Common benefits include continuous monitoring of patients to provide prompt care, improvement of patient self-care, efficient communication, increased patient confidence, and greater education (Serrano et al., 2023)
Today we will outline the barriers associated with implementing the Telehealth program in our outpatient clinic