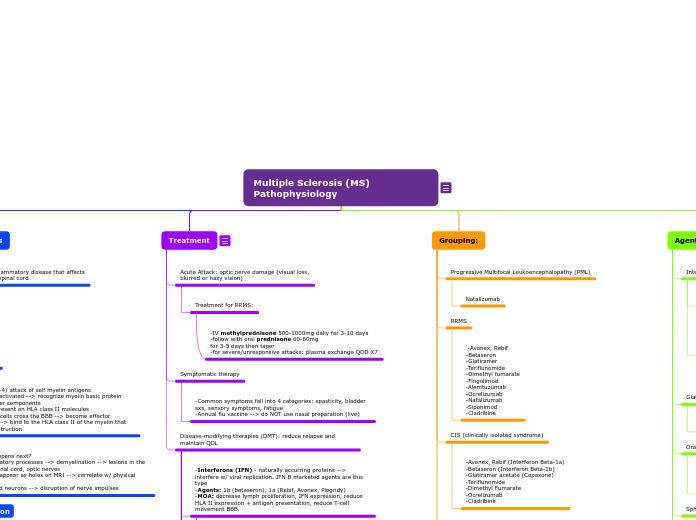
Multiple Sclerosis (MS) Pathophysiology
- Autoimmune disease
- Reduction in T-cell suppressor activity
- Role of cytokines and their contribution to the disease
- TNF-a: demyelination, direct cell injury or promote BBB breakdown
- TH1, Th2, Th17 & Treg --> either pro or anti-inflammatory
- INF-gamma(y): enhances MHC class II expression on macrophages, microglia, and astrocytes promoting inflammatory response + facilitate T-cell across the BBB
- T- cell differentiation & plasticity, APC initiates the process that forms T helper cell subtypes
- IL-2 also contributes to the disease
Questions:
- Does where you live in the USA contribute towards a risk factor for MS?
- Yes, above or below the 37th parallel
- What part of the neuron is damaged by MS?
- Myelin sheet
- What diagnostic tool is used to identify persons w/ MS?
- MRI scan
Agents by class:
Pyrimidine Synthesis inhibitor
Cladribine
CD20-Directed cytolytic antibodies
Ocrelizumab
Monoclonal Antibodies:
Ocrelizumab
Natalizumab
Alemtuzumab
Sphingosine-1-Phosphate (S1P) receptor modulators:
Fingolimod (1st oral agent)
Siponimod
Oral Immunomodulators
-Dimethyl fumarate
-Teriflunomide
-Cladribine
Glatiramer Acetate
Copaxone
Interferons:
Beta-1b
Beta-1a
Avonex, Rebif
Grouping:
When + a corticosteroid is needed:
RRMS acute attack leading to optic nerve damage
IV methylprednisone QD for 3-10D followed by oral prednisone for 3-5D then taper
Start methylprednisone for 3 days and just prior to infusion
PPMS/SPMS (Primary/Secondary progressive type MS)
-Ocrelizumab (only one approved for both RRMS/PPMS)
CIS (clinically isolated syndrome)
-Avonex, Rebif (Interferon Beta-1a)
-Betaseron (Interferon Beta-1b)
-Glatiramer acetate (Copaxone)
-Teriflunomide
-Dimethyl Fumarate
-Ocrelizumab
-Cladribine
RRMS
-Avonex, Rebif
-Betaseron
-Glatiramer
-Teriflunomide
-Dimethyl fumarate
-Fingolimod
-Alemtuzumab
-Ocrelizumab
-Natalizumab
-Siponimod
-Cladribine
Progressive Multifocal Leukoencephalopathy (PML)
Treatment
- What class of agents were originally used to treat persons with MS?
- Interferons
- What MS agent was the first oral product that can also be used in the pediatric population?
- Fingolimod
- Why does the effect of interferons decrease over time?
- Development of neutralizing antibodies (NABs)
- What warning is included for natalizumab usage and also mentioned for similar agents in this category?
- Progressive multifocal leukoencephalopathy (PML)
- What agent requires thyroid function tests for monitoring during treatment?
- Alemtuzumab
- What agent is FDA approved for CIS, RRMS, and SPMS?
- Siponimod
Therapeutic Algorithm:
- Monitor w/ annual MRI or sooner with attacks.
- Failure --> consider conversion to SPMS
- Change to another interferon, newer oral agents or copaxane agent + adj therapy (methotrexate, azathiopurine, etc.)
- mitoxantrone as LAST LINE agent
- Which agent to choose?
- Initial: based upon lifestyle
- If severe depression, interferons are CI --> start anti-depressants
- Women who are preg/attempting/breastfeeding - Do Not Use
- If pt decompensates and has NAB --> stop interferons, rechallenge when other agents don't work
Cautions:
- Watch for progressive multifocal leukoencephalopathy (PML)
- Potentially fatal opportunistic infection caused by John Cunningham polyomavirus (JCV)
- Caused by weakened immune system --> demyelinating condition like MS but there's no mylin regeneration
- Risk: tx >24 mo; JCV, prior immunosuppression use
Disease-modifying therapies (DMT): reduce relapse and maintain QOL
Mitoxantrone
-SPMS, PRMS, RRMS
-lifetime cumulative dose is 140mg/mm due to CHF
-cyclophosphamide + cyclosporine can be used
-depression major issue -> starts antidepressants w/ IFN tx
Cladribine
-RRMS + SPMS
Ozanimod:
-RRMS
-S1P receptor modulator
-DI w/ CYP2C8 inhibitors and inducers
-CI: Cardiac MI or class III/IV HF; 2/3rd AV block
Siponimod:
-FDA for CIS, RRMS, and SPMS
-CYP2C9
Ofatumumab
-RRMS + active secondary progressive disease in adults
-MOA: anti-CD 20 antibody
-CI: persons w/ active HBV infection
Ocrelizumab
-first agent for primary progressive and relapsing MS
-give methylpred before
Alemtuzumab
-reserved for refractory pts > 2DMTs-watch before and after 2hrs
-monitor thyroid func q3m and then for 48mo after
last dose
Natalizumab
-MS/Crohn's disease
-Blocks leukocyte from crossing BBB
-Mono or given + IFNs
Dimethyl fumarate
-Unknown MOA, NKDI
-preg C
Teriflunomide
BLACK BOX WARNING:
-hepatotoxicity
-teratogenicity
-equal efficacy to IFNs and glatiramer
-prevents proliferation of peripheral lymphocytes
-inhibits CYP2C8, OATP1B1, OAT3. Induces CYP1A2
-warfarin use dec 25% INR
Fingolimod
ADEs:
-CI w/ class I/II anti arrhythmic drugs; 2nd/3rd AV block
-1st dose observ req
-metabolized by CYP3A4, avoid inhibitors!!
-1st oral agent
-acts on S1P: responsible for lymphocyte release
-depletes CD4/8 lymphocytes in the blood
-does NOT inhibit T or B cells in organs or lymphocyte recruits
which means no immunosuppression or inc infection risk!
- approved for adults/peds
Glatiramer (Copaxone)
-Copolymer 1
-MOA: MBP binding or mimics antigen actions of MBP, suppress T-cell activation and possibly migration
-ADEs: 10% chest tightness, flushing and dyspnea a few minutes after injection (<20mins). Flu-like/depression noted.
-Interferons (IFN) - naturally occurring proteins --> interfere w/ viral replication. IFN B marketed agents are this type
-Agents: 1b (betaseron), 1a (Rebif, Avonex, Plegridy)
-MOA: decrease lymph proliferation, IFN expression, reduce HLA II expression + antigen presentation, reduce T-cell movement BBB.
Rebif (SQ), Avonex (IM), Pelgridy (SQ)
-disability reduction: 30-40% (higher than glatiramer)
-development of neutralizing antibodies (NAB)
-time-dependent for INFs as NAB inc at 6 mo. + develop as early as 3 mo. Happens w/ all agents.
Betaseron
-reduces annual relapse rate/MRI burden of disease
-ADEs: inj site redness, flu-like, SOB, tachycardia, depression
-lower starting doses 1/4 to 1/2 for 1-2 mo. with increase to full dose @ 2 mo. to lessen flu-like.
To reduce inj site rxns, rotate sites and use ice cooling or topical steroids
To avoid flu-like, have a gradual dose increase, use NSAIDs and low-dose steroids
Symptomatic therapy
-Common symptoms fall into 4 categories: spasticity, bladder sxs, sensory symptoms, fatigue
-Annual flu vaccine --> do NOT use nasal preparation (live)
Acute Attack: optic nerve damage (visual loss,
blurred or hazy vision)
Treatment for RRMS:
-IV methylprednisone 500-1000mg daily for 3-10 days
-follow with oral prednisone 60-80mg
for 3-5 days then taper
-for severe/unresponsive attacks: plasma exchange QOD X7
The W's & H's
Presentation
Diagnosis:
-MRI, CBC, U/A
Primary signs+sxs:
-optic neuritis
-gait
-pain
-spasticity
-weakness
-ataxia
-speech problems
-fatigue
-sexual dysfunction
-bladder/bowel problem
-tremors
Clinical Presentation:
A. Primary - direct result of neuronal damage
B. Secondary - occurs when primary are affected
C. Tertiary - daily life changes
D. Clinical course and prognosis
- is divided into 4 categories by the patterns of exacerbations + remission
- at the onset of new attacks that last 24hrs, separated by other symptoms by 30 days followed by remission. -- called the relapsing-remitting type (RRMS)
- attacks are referred to as relapses or exacerbations
- 1st attack: clinically isolated syndrome (CIS)
- during RRMS --> direct correlation w/ brain MRI lesion/attack
- RRMS most common (85%)
- 10-20% of RRMS have benign course
- 20% of RRMS --> progressive phase --> attacks + remission difficult to identify --> AKA secondary progressive type (SPMS)
- 15% have primary progressive type (PPMS) --> slow onset w/o attacks + worsens over time
- fatality occurs due to complications, suicide rates 7x than normal
How:
1. T-cells (CD+4) attack of self myelin antigens
2. CD+4 cells activated --> recognize myelin basic protein (MBP) and other components
3. Antigents present on HLA class II molecules
4. Activated T-cells cross the BBB --> become effector macrophages --> bind to the HLA class II of the myelin that causes the destruction
What happens next?
-inflammatory processes --> demyelination --> lesions in the brain, spinal cord, optic nerves
-Lesions appear as holes on MRI --> correlate w/ physical disability
-damaged neurons --> disruption of nerve impulses
Why:
-geography
-age
-environment
-genetics
Who:
-15-45 yrs
-women
What: CNS inflammatory disease that affects
the brain and spinal cord