作者:Kaila Mammen 3 年以前
384
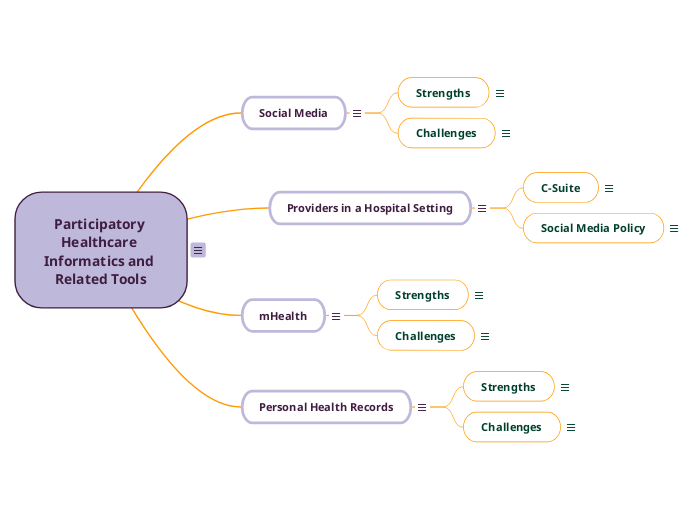
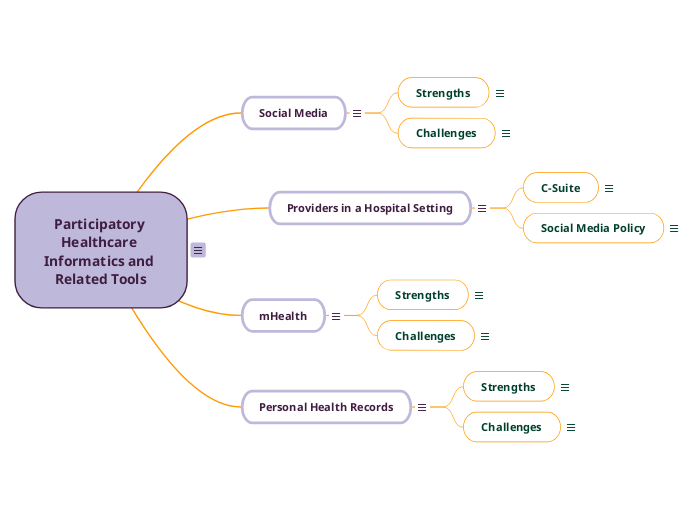
Participatory Healthcare Informatics and Related Tools
作者:Kaila Mammen 3 年以前
384
更多类似内容
Having immediate access to healthcare information is valuable. As the access to the internet expands, so does the availability of health information. Health Informatics: An Interprofessional Approach describes the "ePatient" as a patient who is active in their healthcare. This term was first used in the 1960s and has since evolved with the use of new technology. Now, an ePatient is someone who uses technology to seek information and is active in their health. (Nelson & Staggers, 2018, pp. 203-205)
References
Nelson, R., & Staggers, N. (2018). Health Informatics An Interprofessional Approach. St. Louis: Elsevier.
According to Health Informatics: An Interprofessional Approach, personal health record does not have one single definition. Personal health records serve to collect and store personal information and can be used as a tool to manage one's health. Typically, patients with multiple chronic conditions are more likely to use personal health records. Personal health records allow patients to keep track of their diagnoses, medications, lab results, imaging results, and more. As personal health records evolve, they have the potential to improve patient care and create more personalized care. (Nelson & Stagger 2018 pp. 240, 248, 250)
References
Nelson, R., & Staggers, N. (2018). Health Informatics An Interprofessional Approach. St. Louis: Elsevier.
Despite the known benefits of personal health records, many barriers prevent the adoption of this practice. Health Informatics: An Interprofessional Approach outlines many obstacles to the adoption of personal health records. These barriers include awareness, usability, privacy concerns, access to and knowledge of digital records, provider engagement, and interoperability. (Nelson & Staggers, 2018, pp. 249-250)
A significant barrier is the interoperability of the system, especially with patients that see many providers that use different systems. For patients to adopt and use PHRs, they must be able to see all of their health information in one place. Patients must also be made aware of the program, and these programs must be secure to protect patient privacy. Access to the internet and computer literacy are also concerns that prevent patients from using personal health records.
References
Nelson, R., & Staggers, N. (2018). Health Informatics An Interprofessional Approach. St. Louis: Elsevier.
The benefits of personal health records include patient satisfaction and quality of patient care. According to Health Informatics: An Interprofessional Approach, patients generally have a positive attitude toward personal health records and report having an improved experience in care. Data suggests that personal health records also improve the quality of patient care. (Nelson & Staggers, 2018)
References
Nelson, R., & Staggers, N. (2018). Health Informatics An Interprofessional Approach. St. Louis: Elsevier.
Health Informatics: An Interprofessional Approach describes mobile health or "mHealth" as a subcategory of eHealth. Telemedicine differs from mHealth in that mHealth is meant to be unwired and mobile. (Nelson & Staggers, 2018) Mobile health should be used in conjunction with current health systems. This is intended to increase the availability of care to people through technology that many people have access to.
References
Nelson, R., & Staggers, N. (2018). Health Informatics An Interprofessional Approach. St. Louis: Elsevier.
While there are clear benefits of mHealth, there are many challenges. Nelson & Staggers (2018) describes barriers to mHealth, including misinterpretation of data, privacy risks, legal risks, and funding. There are also concerns about consistently reaching patients, especially those from low-income backgrounds. (p. 264) To overcome these barriers, we must continue to educate patients that mHealth should be used in conjunction with healthcare, not as a replacement for healthcare. Clear guidelines for providers should be in place for privacy and to maintain appropriate legal bounds.
References
Nelson, R., & Staggers, N. (2018). Health Informatics An Interprofessional Approach. St. Louis: Elsevier.
There are many benefits that mHealth provides. According to Health Informatics: An Interprofessional Approach, mHealth increases accessibility to healthcare, decreases cost and increases efficiency, and improves patient outcomes. Mobile health allows access and empowers patients to be more involved in their care. Wearable sensors can give patients real-time information and enable patients to be proactive with their health. (Nelson & Staggers, 2018, pp. 262)
An example of a wearable mHealth sensor would be an Apple Watch. My mom was diagnosed with atrial fibrillation because she was wearing an Apple Watch. Her Apple Watch sent a notification that her heart was beating with an irregular rhythm. While this is not a diagnostic criterion of a-fib, she was able to be proactive and set up an appointment with her primary care physician. She was set up to wear a Holter monitor where they found she had paroxysmal atrial fibrillation.
References
Nelson, R., & Staggers, N. (2018). Health Informatics An Interprofessional Approach. St. Louis: Elsevier.
Healthcare providers are slow to adopt these PHI tools because of the barriers they face with each device. These technological advancements often have challenges regarding the safety of personal health information (PHI). The ethical and legal implications can cause providers to shy away from new technology. Also, many organizations have strict social media policies, which make providers fear repercussions. Healthcare providers may not know how to use specific PHI tools.
As outlined in other headings, the patient-provider relationship is positively impacted by using PHI tools. PHI tools increase open communication and have the ability to improve patient care. Providers need clear direction from the C-Suite and policies to allow and encourage the use of PHI. Providers also need education on the appropriate and safe use of PHI.
At my organization, we have a relatively strict social media policy. At the core of the social media policy is the protection of PHI. According to the MercyOne Code of Conduct, do not post any MercyOne confidential information or MercyOne property. Do not post anything that can associate you with MercyOne if you are endorsing outside business ventures, political campaigns, or religions. MercyOne-provided devices should not be used to post anything considered harassment, volatile, offensive, or degrading. If you have anything within your social media that can link you to MercyOne, you should act in a professional matter when conducting yourself online.
References
MercyOne, 2020, Code of Conduct
Questions I have for the Chief Executive Officer, Chief Financial Officer, and Chief Nursing Officer about using social media in their organizations. Did you know that social media can increase open communication between patients and providers? What can we do as an organization to increase provider involvement in social media? Social media is a great tool we can use to spread information to large amounts of people. Is there any way we can provide more education to our healthcare providers regarding social media? I feel our current social media policy scares our healthcare providers away from using social media. Can we educate our healthcare providers on safety practices when using social media?
Key questions from the C-Suite should be: What are we doing to promote safe and effective communication with patients using social media? How can we use social media to improve patient satisfaction and patient knowledge? Can we use social media to enhance the quality of patient care?
Social media is generally used as a way for people to maintain connections with friends, family, and colleagues. Social media should be user-friendly and allow relationships to flourish without being in person to connect. It enables friends who may otherwise lose touch; a chance to stay connected. Nelson & Staggers (2018) describe social media as a way to convey information and allow networking. There is a variety of different types of platforms that make up social media. (p.221)
References
Nelson, R., & Staggers, N. (2018). Health Informatics An Interprofessional Approach. St. Louis: Elsevier.
While there are many benefits to social media, there are also many challenges associated with healthcare and social media. Health Informatics: An Interprofessional Approach lists things such as not knowing how to use social media, fear of being seen as unprofessional, difficulty protecting patient confidentiality, and accidentally posting something against your organization's social media policy as potential barriers to social media. (Nelson & Staggers, 2018, pp. 225) Healthcare providers must protect personal health information (PHI) ethically and legally.
Another challenge patients and providers face with social media is the quantity and quality of information shared on these platforms. Many times false information is spread rapidly through social media. A new dimension of health care: Systematic review of the uses, benefits, and limitations of social media for health communication touches on this subject. They found the main concern regarding the information on social media is the lack of reliability of information shared. (Moorhead, et al. 2013)
To overcome these challenges, providers should be educated on how to use social media to improve patient care. This education should include protecting yourself and your patient's private information. Healthcare providers also need approval from the C-Suite and need to practice within their social media policy. There have been strides to improve and prevent the spread of misinformation with independent fact-checkers, but there is still a long way to go with the quality of information shared on social media sites.
References
Moorhead, S. A., Hazlett, D. E., Harrison, L., Carroll, J. K., Irwin, A., & Hoving, C. (2013). A new dimension of health care: Systematic review of the uses, benefits, and limitations of social media for health communication. Journal of Medical Internet Research, 15(4), e85. https://doi.org/10.2196/jmir.1933
Nelson, R., & Staggers, N. (2018). Health Informatics an Interprofessional Approach. St. Louis: Elsevier.
Social media has a multitude of strengths. Communication is at the heart of social media. It allows for accessible communication between providers and patients alike. Social media creates a more personal experience and allows for more open communication. Social media can also spread information regarding news in healthcare quickly to the masses. For example, during the pandemic, new articles and updates were constantly posted through social media.
Health Informatics: An Interprofessional Approach outlines many strengths of social media. One of the strengths mentioned is access to information and social support. People can connect with similar health concerns or goals using social media. (Nelson & Staggers, 2018, pp. 224) Chen & Wang (2021) found that nearly 80% of cancer patients used social media to connect.
References
Chen, J. & Wang, Y. (2021). Social media use for health purposes: Systematic review. Journal of Medical Internet Research, 23(5). doi:10.2196/17917
Nelson, R., & Staggers, N. (2018). Health Informatics An Interprofessional Approach. St. Louis: Elsevier.