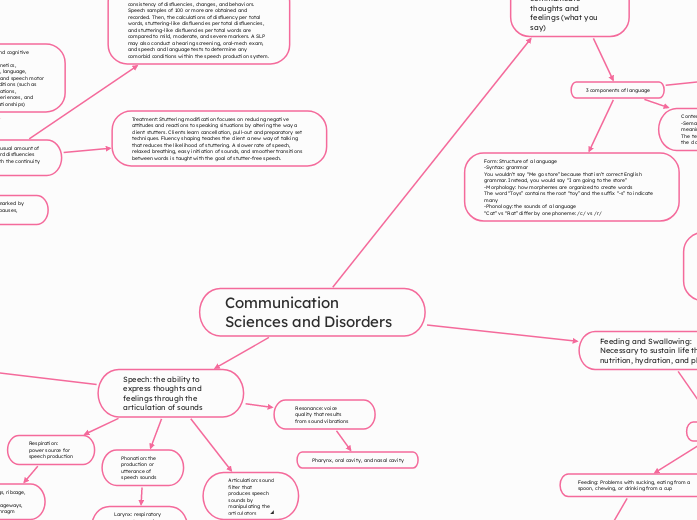
Communication Sciences and Disorders
Speech: the ability to express thoughts and feelings through the articulation of sounds
Respiration: power source for speech production
Lungs, ribcage, air passageways, diaphragm
Phonation: the production or utterance of speech sounds
Larynx: respiratory energy to sound energy and vocal folds: vibrate to create sound
Tongue, lips, teeth, jaw, alveolar ridge, hard palate, velum, pharynx, larynx, oral cavity
Resonance: voice quality that results from sound vibrations
Pharynx, oral cavity, and nasal cavity
Disorders
Childhood Apraxia of Speech: Severe speech disorder with words dominated by simple syllable shapes (CV, CVC, VC), vowel errors, and sounds that develop early (/m/, /p/, /b/)
Etiology: No significant sensory loss, abnormalities or emotional disorders, implying possible neurological and genetic factors as causes.
Evaluation: Identification is difficult because clinicians don’t agree on differentiating from other disorders such as a severe articulation delay. Speech and Language screenings are necessary alongside ruling out other possible conditions such as muscle weakness or phonological disorders.
Treatment: Focus on speech motor movements (auditory, visual and tactile cueing), prosodic deficits, and phonological awareness. The use of Augmentative and Alternative Communication (AAC) is common with CAS. Development is very slow despite intensive speech therapy.
Acquired Apraxia of Speech: Disorder in planning and programming of speech movements due to left frontal lobe damage.
Etiology: Stroke or traumatic brain injury
Evaluation: Identify core symptoms (prosodic impairment, disfluency, and speech sound errors). Diagnosis is controversial and difficult due to possible overlap with other conditions such as Broca’s area aphasia
Treatment: Improve the motor programming of increasingly more demanding syllables, words, and phrases. Focus is on rate and rhythm control.
Dysarthria: Central and peripheral nervous system pathways are damaged leading to muscle dysfunction in speech production.
Etiology: Dysarthria in children is most commonly associated with cerebral palsy, a condition characterized by weak, paralyzed, or uncoordinated muscles. Acquired dysarthria occurs after speech and language development as a result of conditions such as Bulbar palsy, cerebellar damage, and Parkinson’s disease.
Treatment: SLPs, occupational therapists, audiologists, special educators, neurologists and physical therapies work together. Surgery and drugs may work for patients where dysarthria is a symptom (such as parkinson’s). Clients may also use a postural support to be in the best position for speaking and speech therapy focusing on improving intelligibility.
Fluency Disorder: Speech that is marked by phrase repetitions, interjections, pauses, revisions, and word repetitions.
Stuttering: an unusual amount of tense, within-word disfluencies that interfere with the continuity of speech
Etiology: Neurological and cognitive factors (such as neural structures/functions, genetics, temperament, cognition, language, information processing, and speech motor control) or external conditions (such as culture, parental expectations, childrearing beliefs, experiences, and parent/sibling/peer relationships)
Evaluation: Interview and case study provides information about a patient's lifestyle, environment, consistency of disfluencies, changes, and behaviors. Speech samples of 100 or more are obtained and recorded. Then, the calculations of disfluency per total words, stuttering-like disfluencies per total disfluencies, and stuttering-like disfluencies per total words are compared to mild, moderate, and severe markers. A SLP may also conduct a hearing screening, oral-mech exam, and speech and language tests to determine any comorbid conditions within the speech production system.
Treatment: Stuttering modification focuses on reducing negative attitudes and reactions to speaking situations by altering the way a client stutters. Clients learn cancellation, pull-out and preparatory set techniques. Fluency shaping teaches the client a new way of talking that reduces the likelihood of stuttering. A slower rate of speech, relaxed breathing, easy initiation of sounds, and smoother transitions between words is taught with the goal of stutter-free speech.
Voice Disorder: Dysfunction occurring in the larynx
Carcinoma: cancer of the larynx
Etiology: Tobacco/alcohol use, older age, family history, exposure to chemicals or viruses such as human papillomavirus (HPV)
Evaluation: Videoendoscopy is when a clinician threads a long camera down the pharynx, allowing for direct visualization of the vocal folds and larynx. They may identify abnormalities with this examination. Patients will also be asked for a case history to determine any genetic links or pre dispositions such as a family history of cancer. A biopsy may also be taken to examine the tissue of the larynx under a microscope.
Treatment: A team including surgeons, speech pathologists, physicians, and otolaryngologists work together to treat cancer of the larynx. It may be possible to simply remove the cancerous tissue and proceed with chemotherapy or radiation therapy. In some cases, complete removal of the larynx may be necessary, known as a laryngectomy. Post-operative, the team counsels their patient to decide if an artificial larynx, esophageal speech, or tracheoesophageal speech is the best fit for them to improve phonation and fit with their lifestyles.
Language: Symbols and ways of combining them into words, sentences, phrases, and texts to communicate thoughts and feelings (what you say)
Receptive: ability to understand spoken, written, and/or signed language
Recognizing and following instructions: Mom says: “Take out the trash” and you understand what is being commanded of you.
Expressive: ability to use spoken, written, and/or signed language to express thoughts and feelings
Communicating wants and needs: “I don’t like broccoli”
Spoken: Language that is conveyed through speech as opposed to writing, signing, or other non-verbal means
Conversations, reading out loud, singing, telling stories
Written: Ability to read and write as a mode of expressive and receptive language skills
My name is Shelby. I can spell it and recognize it when I see it written.
3 components of language
Form: Structure of a language
-Syntax: grammar
You wouldn’t say “Me go store” because that isn’t correct English grammar. Instead, you would say “I am going to the store”
-Morphology: how morphemes are organized to create words
The word “Toys” contains the root “toy” and the suffix “-s” to indicate many
-Phonology: the sounds of a language
“Cat” vs “Rat” differ by one phoneme: /c/ vs /r/
Content: Meaning of a language
-Semantics: Ability to understand the meaning of words and sentences
The teacher says, “Time for recess!” and the class gets excited to go play outside.
Use: Social aspects
-Pragmatics: Using language appropriately in different social contexts
You would not sing Happy Birthday at a funeral
Disorders
Developmental Language Disorders: Significant delays or deficits in comprehension or production of language form, content, or use not attributed to hearing, intellectual, emotional, or acquired neurological impairments
Etiology: Believed to be a result of genetic, neurological, and/or environmental factors
Evaluation: Norm-referenced tests compare a child’s skill in a given area to other children of the same chronological age. Criterion referenced tests measure a child’s performance in comparison to predetermined standards. An SLP can also conduct a language sample through play, asking the child to look at pictures and create a story around them. This is an opportunity to examine most aspects of language.
Treatment: Child centered approach is where the clinician and child engage in conversation during play to increase the number and type of words a child uses. This includes self-talk, parallel talk, expansion, extension, and recast. The clinician centered model is more structured, aiming to teach a specific skill in form, function, or pragmatics. The hybrid approach is a combination of the clinician and child centered. This includes focused stimulation and vertical structure.
Literacy Disorders: Impairments in reading and writing
Etiology: In most cases, the disorder is idiopathic (cause is unknown) but can also occur as a result of genetics, environmental factors, brain injury, or mental illness.
Evaluation: Language and writing samples are used to identify deficits in expressive language and asking the child to read a passage, marking errors, gives a baseline for deficits of receptive language. The SLP can identify what area(s) their client needs the most improvement in, whether it is grammar, semantics, vocabulary, ect.
Treatment: Focus on phonological awareness, sight word knowledge, reading, writing or retelling stories, and social linguistic skills through play or conversation as it is age appropriate to each client.
Aphasia: Language disorder affecting phonology, grammar, semantics, and pragmatics as well as reading and writing.
Etiology: Left hemisphere brain damage as a result of a cerebrovascular accident (stroke) or traumatic brain injury (TBI)
Evaluation: Boston Diagnostic Aphasia Examination is a body functions and structures approach characterizing strengths and weaknesses of specific linguistic skills (naming, fluency, auditory comprehension, and repetition)
Treatment: The primary goal of aphasia therapy is to reduce language deficits by restoring linguistic skills and developing compensatory strategies to increase communication effectiveness. Constraint-Induced Language Therapy is a body structure and function restorative approach. Promoting Aphasiac Communicative Effectiveness and Supported Communication for Aphasia promotes communication outputs and increasing conversational abilities. Group therapy can offer a setting to practice communication skills in a non-threatening environment
Traumatic Brain Injury: Neurological damage caused by an injury to the head
Etiology: Motor vehicle accidents, falls, blast trauma, assaults, or foreign object penetration
Evaluation: Levels of Cognitive Functioning Scale monitors behavioral changes throughout TBI recovery. SLPs obtain language samples to understand deficits across cognition and communication (word finding, grammar, spelling, reading, writing, taking turns, maintaining topics, understanding facial/body expressions, sarcasm, attention span, problem solving, judgment, planning, and goal setting)
Treatment: Focus on restoring the deficits revealed in the assessment. This can be accomplished through games working on memory, reasoning and problem solving.
Dementia: Deterioration of cognitive and language abilities resulting from progressive deterioration of the brain
Etiology: Alzheimer’s disease, Huntington’s Chorea, hereditary disorders, vascular disease
Evaluation: Understanding the decline of functioning and it’s interference with one’s independence. Identify core symptoms such as attention, executive function, learning, memory, language, social cognition, and motor functions.
Treatment: Since dementia is progressive and there is no “cure”, the primary focus is retaining as much independence as possible while improving the patient’s quality of life. This can be accomplished through reminiscence therapy, using old pictures, objects, or videos with important meaning to trigger long-term memory or spaced retrieval training where the SLP presents new information and gradually increases the length of time in which the information is remembered.
Feeding and Swallowing: Necessary to sustain life through nutrition, hydration, and pleasure
-Lips: Keep bolus from falling out of the mouth
-Soft palate: Closes off entry to the nasal cavity to prevent nasal regurgitation
-Bolus: Food after it has been chewed and mixed with saliva
-Epiglottis: Meets with the larynx and bends backwards, closing off the opening to the windpipe to prevent aspiration.
-Esophagus: Tube that transports food to the stomach
-Teeth: Chews food for safe swallowing, preventing choking by large pieces blocking off the airway.
-Tongue: Moves bolus around in the mouth towards the pharynx
Disorders
Feeding: Problems with sucking, eating from a spoon, chewing, or drinking from a cup
Etiology: Medical conditions such as GERD, heart disease and respiratory conditions, structural abnormalities such as cleft lip or palate, neurological disorders such as cerebral palsy, sensory issues with the taste, smell, texture, or color of food, behavioral issues such as tantrums or resistance to mealtime, prematurity, medications that alter appetite, and autism.
Evaluation: An oral mech exam is carried out to understand muscular deficits such as the lips being unable to fully close and keep food in the mouth. SLPs will ask what sensory issues the patient has to create a treatment plan that gradually exposes them to their aversions. SLPs will work with the patient and their caregivers to obtain a complete medical history including birth complications, medical conditions, and medications.
Treatment: SLPs can work on an interdisciplinary team of gastroenterologists, psychiatrists, nutritionists, radiologists, and occupational therapists to meet the nutritional needs to grow and remain healthy in a safe way. Some alterations can include altering the position a patient is in when eating, using postural supports, adaptive feeding equipment, making the bolus thicker or thinner, and counseling families on how they can support their loved ones outside of their therapy sessions.
Dysphagia: Difficulty swallowing or inability to swallow
Feeding: The process of taking in and chewing food and/or liquid
Swallowing: The process of moving the food/liquid from the mouth to the stomach via the esophagus
Oral stage: leading up to the swallow
1) Oral-Prepatory: Bolus is being prepared for a safe swallow by breaking it down into smaller pieces
2) Oral: tongue pushes the bolus against the palate, moving it backwards towards the pharynx. This stage is complete when the bolus enters the pharyngeal area.
3) Oral stage: leading up to the swallow
4) Pharyngeal: epiglottis moves to protect the airway and direct the bolus towards the stomach.
5) Espohageal: lowering and backwards movement of larynx and resumption of breathing
Speech Sound Disorders
Articulation Disorder: Difficulty producing the sounds and sound sequences of a language (ie /w/ for /r/ "wabbit" for "rabbit")
Etiology: Functional: Cause can't be determined or organic: known root cause (ie otitis media, sensorineural hearing loss, cleft lip and palate, dysarthria, apraxia, structural insufficiency of articulators)
Evaluation: Oral-Mechanism examination to determine any physical structural insufficiencies. Standardized articulation screeners (child names pictures to assess ability to produce consonants in various words). It is also important to have a comprehensive medical history and hearing screening.
Treatment: Articulation approach focuses on improving control and use of articulators to produce accurate speech sounds relative to the child's chronological age
Phonological Disorder: Difficulty understanding and implementing the underlying rules for producing sounds and sequences. More pattern related (Ca__ for “cat”)
Etiology: Commonly functional (cause cannot be determined) but can also be a result of neurological disorders, hearing loss, or developmental delays)
Evaluation: Spontaneous speech sample (talking/playing with child to analyze their ability to produce speech sounds and sequences) It is important to determine if a child has a phonological delay due to lack of exposure to these language experiences or if it is a true phonological disorder.
Treatment: Focus on teaching the use of sounds appropriate with their chronological age and improving intelligibility. Phonological approach emphasizes use of correct sound sequences to communicate
https://navigate2.jblearning.com/course/view.php?id=54646 https://www.nichd.nih.gov/health/topics/reading/conditioninfo/causes#:~:text=There%20is%20no%20single%20known%20cause%20at%20this%20time.&text=Environmental%20factors%E2%80%94such%20as%20children's,linked%20to%20a%20person's%20genes. https://www.asha.org/practice-portal/clinical-topics/written-language-disorders/disorders-of-reading-and-writing/ https://www.expressable.com/learning-center/feeding-and-swallowing/the-definitive-guide-to-feeding-therapy-for-children
https://www.ncbi.nlm.nih.gov/books/NBK564306/#:~:text=Pediatric%20feeding%20disorder%20has%20multifactorial,Cleft%20lip
Etiology: Medical conditions such as cleft lip and palate, cerebral palsy, stroke, traumatic brain injury, dementia, neuromuscular disease, and cancer or psychological components such as anorexia nervosa or autism spectrum disorder.
Evaluation: SLPs will conduct a clinical bedside exam to evaluate cognitive and motor skills. They will collect a full medical history including a current list of medications and understanding how the patient currently obtains nutrients (oral, IV, nasogastric tube, or gastric tube).This may also include an oral mechanism exam. A Modified Barium Swallow Study is a moving x-ray picture of a swallow, obtained by consuming food dyed by barium. A videoendoscopy is a flexible scope inserted through the nose to visualize the pharynx and larynx.
Treatment: SLPs can work on an interdisciplinary team of gastroenterologists, psychiatrists, nutritionists, radiologists, and occupational therapists to meet the nutritional needs to grow and remain healthy in a safe way. Some alterations can include altering the position a patient is in when eating, using postural supports, adaptive feeding equipment, making the bolus thicker or thinner, and counseling families on how they can support their loved ones outside of their therapy sessions.