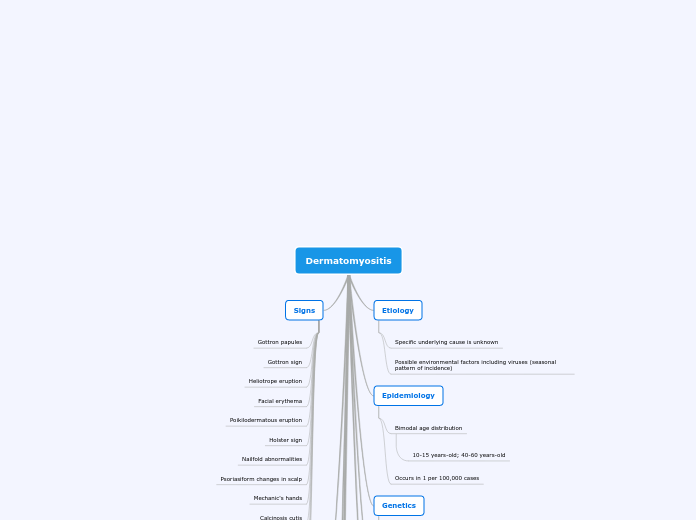
Dermatomyositis
Etiology
Specific underlying cause is unknown
Possible environmental factors including viruses (seasonal pattern of incidence)
Epidemiology
Bimodal age distribution
10-15 years-old; 40-60 years-old
Occurs in 1 per 100,000 cases
Genetics
Possible links to HLA alleles
Genetic component may be less than in other autoimmune disorders
Pathophysiology
Inflammatory myopathy
Antigen specific antibodies
Attack against muscle capillaries and endothelium
Perivascular and perimysial infiltration
Laboratory Testing
Elevated CK, aldolase, AST, ALT, LDH
Elevated ESR and CRP
Myositis-specific autoantibodies
Anti-jo-1
Anti-Mi-2
Anti-SRP
Signs
Gottron papules
Gottron sign
Heliotrope eruption
Facial erythema
Poikilodermatous eruption
Holster sign
Nailfold abnormalities
Psoriasiform changes in scalp
Mechanic's hands
Calcinosis cutis
Periungual telangiectasia
Reduced proximal muscle strength
Muscle atrophy
Symptoms
Myalgias and muscle tenderness
Joint pain and swelling
Muscle weakness
Insidious onset
Symmetrical proximal muscle weakness
Difficulty rising from a low chair
Difficulty walking upstairs
Difficulty washing hair
Difficulty getting out of a car
Difficulty reaching overhead
Difficulty combing hair
Treatment
Systemic glucocorticoids (prednisone)
Glucocorticoid sparing immunosuppressive agents
Mycophenolate mofetil
Rituximab
Vitamin D and calcium supplementation
If taking 5mg/day or more of steroids for more than 3 months
Physical therapy
Health Promotions
Daily exercise to maintain and restore normal function
Smoking cessation
Healthy diet
Fruits, vegetables, whole grains, lean protein
Additional Testing
Muscle biopsy
Confirms diagnosis
Detects muscle inflammation and damage
Electromyography