Hyperprolactinemia summary
GH deficiency summary
GH excess summary
*PHARM
*Cabergoline
DOC for management of prolactinomas
CANT BE USED IN PREGNANCY
superior efficacy, besster GI ADE, less frequent dosing
DOC for fertility or pregnancy
NON-PHARM
Radiation
ONLY IN CONJUNCTION WITH SURGERY
Transsphenoidal surgery
reserved for patients who are refractory to or cannot
tolerate dopamine agonists, or large tumor that could
cause severe compression of adjacent tissues
*less affective than medical therapy with dopamine
agonist for sx control!!
For drug induced hyperprolactinemia, medical therapy with dopamine agonists can be considered if a therapeutic alternative does not exist
GOALS
correction of visual defects (macroadenomas)
tumor shrinkage (macroadenomas)
re-establish gonadotropin secretion
restore fertility, and reduce risk of osteoporosis
normalize serum prolactin
DX Criteria
IDENTIFY UNDERLYING CAUSE
CT or MRI to determine presence of tumor
presence of hypothyroidism, renal failure, hepatic dysfunction
obtain med history
check multiple serum prolactin levels in pts w/ modest elevations
SERUM PROLACTIN > 25 mcg/L OBSERVED ON MULTIPLE OCCASIONS
clinical sequelae (downstream effects)
increased risk of ischemic heart disease if left untreated
significant risk for development of osteoporosis
normal values
levels do not typically rise to > 150 mcg/L in drug induced disease
if > 150 probably due to tumor
males: <15 mcg/L
non-pregnant females:
< 25 mcg/L
*menstrual irregularities
seen at > 60 mcg/L
pregnant females:
34-386 mcg/L
fasting prolactin serum concentrations
at rest > 25 mcg/L (elevated)
Signs/Symptoms
males: decreased libido, infertility
visual loss
females: oligomenorrhea, amenorrhea,
galactorrhea (nipple discharge), infertility
sx related to local effects of prolactin-secreting
tumor (HA, visual disturbances) resulting from
tumor compression of optic chiasm
background
other etiologies
unable to determine cause: idiopathic hyperprolactinemia
renal or hepatic impairment causing
decreased clearance of prolactin
increased TRH in hypothyroidism
CNS lesions physically compress pituitary stalk
and interrupt tonic hypothalamic dopamine
secretion
usually effects women of reproductive age
most common causes
drug induced
Prolactin Stimulators
Methyldopa, Reserpine, SSRIs, 5-HT1 receptor
agonists (triptans), Estrogens, Progestins, Protease
inhibitors, GnRH analogs, Benzodiazepines, TCAs,
MAOI, opioids, cocaine
Verapamil
Dopamine antagonists
Domperidone
Metoclopramide
Phenothiazine
Antipsychotics
prolactin secreting benign pituitary tumors (prolactinomas)
persistently elevated serum prolactin
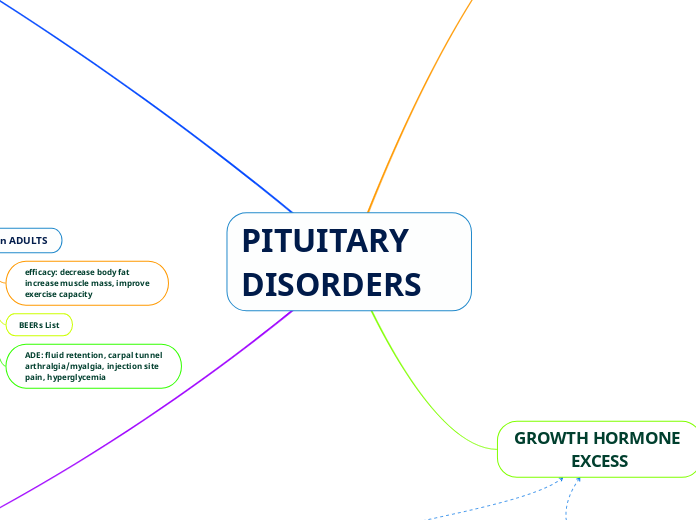
recombinant GH in ADULTS
fixed dosing
avoid GH therapy in adults
EXCEPT AS REPLACEMENT FOLLOWING
PITUITARY GLAND REMOVAL
ADE: fluid retention, carpal tunnel
arthralgia/myalgia, injection site
pain, hyperglycemia
BEERs List
efficacy: decrease body fat
increase muscle mass, improve
exercise capacity
recombinant GH in CHILDREN
ADE (rare): intracranial HTN, slipped
capital femoral epiphysis, scoliosis
progression
Responders
continue tx until satisfactory adult
height or growth velocity has decreased
< 2-2.5 cm/year after pubertal growth suprt
monitoring: blood glucose, BP
non responders
if growth rate < 2-2.5 in 1 year
DOUBLE DOSE FOR 6 MONTHS
if still no satisfactory response, dc therapy
AGENTS (contain somatropin)
Zorbtive
Tev-Tropin
Serostim
Saizen
Omnitrope
Nutropin AQ
Norditropin
Humatrope
Genotropin
Recombinant insulin-like
growth factor-1
Mecasermin (Increlex)
ADE: hypoglycemia
pregnancy category C
WEIGHT BASED DOSING
increase growth velocity in children with short stature
who have low IGF-1 AND resistance to GH
ONLY INDICATED FOR TREATMENT OF SHORT
STATURE DUE TO SEVERE PRIMARY IGF-1 DEFICIENCY
Goals
adults: increase muscle mass and reduce adiposity
children: achieve normal adult height
initiate ASAP
Recombinant GH
1 mg contains 2.6 IU of GH
potency is expressed as
international units/mg
dosing is WEIGHT BASED
SC or IM injections
mainstay of therapy
Clinical Presentation
Factors to consider for DX
pubertal stage: Tanner Scale
percentile of anthropometric
measurements
growth velocity
bone age
provocation test
Lab Tests
+/- loss of other pituitary hormones
(hypoglycemia or hypothyroidism)
+/- reduced IFG-1 and binding protein
peak GH concentrations < 10 mcg/L
during a 2 hour period following a GH
provocation test (subnormal response)
provocative stimuli to induce GH secretion: insulin, clonidine,
L-dopa, arginine, glucagon, GHRH
Signs
central obesity, prominence
of forehead, immaturity of
face
average birth rate
delayed skeletal maturation
reduced growth velocity
Physical height is >2
SD below population
mean
DOPAMINE AGNOIST
Contraindications:
- ischemic heart disease
- peripheral vascular disease
- uncontrolled HTN
Bromocriptine
monitor: orthostatic HOTN
Cabergoline
monitor: increased LFTs
(check monthly x 6 months)
Drug-Drug interactions
- ritonavir
- indinavir
- ketoconazole
- irtaconazole
- clarithromycin
take with food to improve GI sx
efficacy: improvement in s/sx
and random GH < 1mcg/L
after 4-8 weeks
Agents
GH receptor Antagonist
Pegvisomant
increased LFTs (check monthly for 6 months then q6 months)
*dc if transaminases > 3x ULN
diarrhea
USE OF GH VALUES FOR TITRATION IS NOT HELPFUL!!
DOES NOT INHIBIT GH PRODUCTION BECAUSE IT BLOCKS GH RECEPTORS (DOES NOT DECREASE TUMOR SIZE)
use if high IGF-1 levels and refractory
to somatostatin analogs
Somatostatin Analog
MOA: mimic endogenous
somatostatin's inhibition
of GH secretion
Pasireotide
Drug-Drug Interactions
- concominant cispride
- dronedar
- pimozide
- thioridazine
ADE: higher incidence
of hyperglycemia
most effective
Lanreotide
ADE: same as octreotide
Octreotide- moderate
to severe DOC
ADE
cholelithiasis
hyper OR hypoglycemia
injection site reaction
N/V/D/GI cramps
(subsides 2 weeks after tx)
Drug-Drug interactions
cyclosporine
BB and CCB
formulations
Long Acting Release (LAR)- IM injection
*use for adherence
Immediate Release (IR)- SQ injection
Dopamine Agonist
MOA: paradoxical reduction
in GH production
*Cabergoline
(1st choice)
Bromocriptine
preferred in
pregnancy
TREATMENT
PHARMACOLOGIC
Who gets it?
preference for medical therapy
inadequate response to surgery
poor surgical candidates
NON-PHARMACOLOGIC
radiation therapy
for poor surgical candidates and those who refuse
or dont respond to surgical or medical interventions
TREATMENT OF CHOICE: TRANSSPHENODIAL SURGICAL RESECTION OF GH-SECRETING ADENOMA
GOAL: GH CONCENTRATION = < 1 mcg/L after standard OGTT in the presence of normal IGF-1 concentrations
Treatment Goals
decrease mortality (CV causes)
improve clinical signs and symptoms
normalize IGF-1 concentrations
reduce GH concentrations
Clinical sequlae (downstream effects)
increased risk
for cancer development
stomach
colon
esophageal
T2DM
respiratory disorders and
sleep apnea
osteoarthritis and
joint damage
Cardiovascular disease
left ventricular hypertrophy
cardiomyopathy
CAD
HTN
CLINICAL PRESENTATION
LAB TESTS
following oral glucose tolerance test (OGTT): elevated GH > 1mcg/L and elevated IFG-1 levels
SYMPTOMS
local effects of GH-secreting tumor: HA, visual disturbances
elevated GH and IGF-1 concentrations: excessive sweating, neuropathies, joint pain, parasthesis
SIGNS
increased hand volume, ring size, shoe, size
enlarged tongue
various dermatologic conditions
coarsening of facial features
PITUITARY DISORDERS
Hyperprolactinemia
Feedback Loop
Prolactinomas produce prolactin
macroadenomas: > 10 mm in diameter; continue to grow and may invade other issues
microadenomas: < 10 mm in diameter; no increase in size
measure levels when pt is at rest in supine position or in
a chair for > 2 hours
transient elevations: sleep, exercise, coitus, eating, stress
regulated by hypothalamic inhibitory effects of dopamine
concentrations peak during sleep
secreted by ANTERIOR pituitary in a pulsatile manner
GROWTH HORMONE DEFICIENCY
New Growth Hormone Dificiency Test
Macimorelin (Macrilen)
GH insufficiency
any age during growth development
acquired condition
drugs (transient): glucocorticoids, methylphenidate,
dextroamphetamine
poorly controlled T2DM
hypothyroidism
psychosocial deprivation
various CNS infections
pituitary infarction
head trauma
hypothalamic/pituitary disorders
Absolute GH deficiency
6 months-3 years
conginital disorder
genetic abnormalities: GHRH
deficiency, GH gene deletion
developmental disorders: pituitary
aplasia, hypoplasia
short stature = patients who are > 2 SD below population mean
GROWTH HORMONE EXCESS
Gigantism
excess secretion of GH PRIOR TO EPIPHYSEAL CLOSURE IN CHILDREN
Acromegaly
caused by excess GH
MAIN CAUSE
GH-secreting pituitary adenoma
growth hormone patho
GH is secreted by ANTERIOR pituitary in a pulsatile fashion
concentration highest- night
concentration lowest- waking hours
several short bursts- mostly at night
GH stimulates formation of IGF-1 in the liver and pripheral tissues
growth promoting effects of GH are mediated by IGF-1 (before and after birth) and IGF-2 (in utero)
growth hormone
secretion
peak = during first 1-2 hours of sleep
daytime pulses after: meals, exercise, stress
anabolic peptide that directly stimulates cell proliferation and growth
Anatomy and Physiology
PITUITARY GLAND
"hypophysis"
POSTERIOR PITUITARY
"Neurohypophysis"
2 main hormones produced: vasopressin & oxytocin
Oxytocin
contracts smooth muscle in breast during lactation
uterine contractions
Vasopressin
main function
antidiuretic hormone, acts on the
renal collecting ducts to conserve
water
secretes hormones through direct nerve stimulation
extension of neurons of the periventricular
and super optic nuclei of the hypothalamus. Cell
bodies rest in the hypothalamus and end in the
axon terminals that comprise the PP
ANTERIOR PITUITARY
"Adenohypophysis"
"Master Gland"
hormones produced
LH
(lutenizing hormone)
stimulates testosterone synthesis in testes and ovulation, corpus luteum formation, estrogen and progesterone synthesis in the ovaries
FSH
(follicle stimulating hormone)
sperm maturation- testes
follicle growth- ovaries
TSH
(thyroid stimulating hormone)
iodine uptake and thyroid hormone systhesis
ACTH
(adrenocorticotropic hormone)
stimulates synthesis and secretion of adrenocortical hormones
Prolactin
in women (in the ovary) can block follicular genesis and lead to decreased estrogen & an-ovulation
promotes lactation and inhibits gonadal function
GH (somatotropin)
stimulates protein synthesis and overall growth in all body tissues
controlled by specific hypothalamic releasing
and inhibitory hormones (not by direct nerve stimulation
like the PP)
hormones synthesized in the hypothalamus reach the
anterior pituitary via the hypothalamic-hypophyseal portal
vessels
HYPOTHALAMUS
What does it regulate?
Diurnal rhythms (circadian rhythm)
CV function/Resp function
body temp
food and water intake
limbic functions (emotion,memory,arousal)
Median eminence = inferior boundary of pituitary gland that connects hypothalamus to the pituitary
neurons lead to production of: vasopressin, oxytocin, GHRH, Somatostatin
receives autonomic nervous system input from different areas of the brain