TSIg
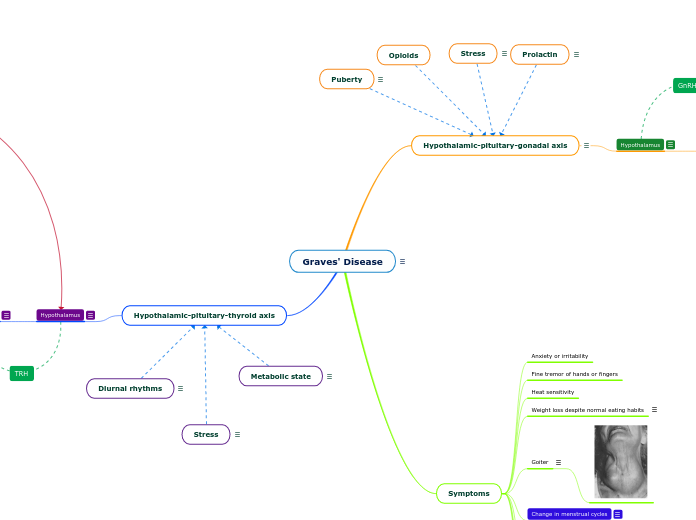
In Graves' disease, thyroid-stimulating immunoglobulins (TSIg) over-stimulate the TSH receptors found in the thyroid gland and are unregulated by the HPT axis.
Opioids
Prolactin
Hypothyroidism impacts the release of TRH and can induce hyperprolactinemia which causes amenorrhea, oligomenorrhea, and infertility in females.
Puberty
.
Stress
Conditions of starvation or infection can induce the HPT axis.
Metabolic state
Thyroid hormones play a large role in regulating internal body temperature.
Diurnal rhythms
Diurnal rhythms are synonymous with circadian rhythms that are synced with the day and night.
Graves' Disease
Graves' disease is a type of hyperthyroidism caused by autoimmune dysfunction in the body. The immune system produces antibodies called Thyroid Stimulating Immunoglobulin (TSI), which bind the TSH receptors in the thyroid gland and directly stimulate it. This causes elevated levels of T3 and T4. Levels of thyrotropin-releasing hormone (TRH) and thyroid-stimulating hormone (TSH) are lower due to more negative feedback from T3 and T4.
Hypothalamic-pituitary-thyroid axis
Thyrotropin-releasing hormone (TRH) is released from TRH neurons in the paraventricular nucleus (PVN) of the hypothalamus.
T4/T3 feeds back to act on TRß2 receptors in the PVN of the hypothalamus. This negative feedback decreases the secretion of TRH.
TRH binds to a G-protein coupled receptor in the AP thyrotrope cell and activates the phospholipase C (PLC) pathway. Second messenger PLC converts PIP2 into IP3 and DAG. IP3 and DAG activate the production of protein kinase C and the release of intracellular calcium. It is the calcium release that allows for TSH synthesis and secretion from the anterior pituitary (AP) thyrotrope cells.
The AP is stimulated by TRH to release TSH onto the butterfly-shaped thyroid gland in the neck region.
T4/T3 feeds back onto TRß2 receptors on the AP thyrotrope cells. This negative feedback leads to less secretion of TSH.
Thyroid Gland
TSH binds to TSH receptors on thyroid epithelial cells causing the increased activation of adenylate cyclase (AC) which increases intracellular cAMP and activates protein kinase A (PKA). PKA helps increase the synthesis and secretion of thyroid hormones and causes cell growth.
In Graves' disease, over-stimulation of the TSH receptors on the thyroid gland by TSIgs leads to increased secretion of T4/T3 from the thyroid gland. Because more thyroid hormones are being synthesized and secreted, the thyroid gland is stimulated to grow. This growth causes people with hyperthyroidism to develop a goiter (bilateral enlargement of the thyroid gland).
T4
T4 undergoes deiodination to become the active form of the thyroid hormone, T3.
In Graves' disease, increased stimulation of TSH receptors by TSIgs leads to an increased production of T4 hormone. More T4 hormone means that there is increased production of T3 hormone via deiodinase activity. Additionally, increased levels of T4/T3 will cause there to be more negative feedback on the hypothalamus and AP.
T3
In Graves' disease, more T3 hormone production leads to more negative feedback of T3 onto the hypothalamus and AP. More negative feedback onto these parts of the endocrine axis means that the axis will stop producing high levels of TSH. TRH levels will also decrease due to negative feedback by increased levels of T4/T3 on the hypothalamus. Although T3 is telling the HPT axis to decrease its activity through negative feedback mechanisms, the TSIg are unregulated and will continue to stimulate the thyroid gland to release thyroid hormones.
Digestive system
Increases carbohydrate absorption in the gut.
Binds to TRß1 receptors in the liver. Initiates formation of LDL receptors in the liver.
Whole body
Thyroid hormones have a calorigenic effect on the entire body. Cause increased oxygen consumption, metabolic rate, and temperature (exceptions: testes, uterus, lymph nodes, spleen, AP).
Heart
Binds to TRa1 receptors.
Effects:
Increases ß-adrenergic receptors
Increases response to catecholamines
Increases % of alpha-myosin heavy chain
Promotes normal growth, skeletal development, and bone turnover.
Binds to TRa1 receptors. Increases protein breakdown.
Adipose tissue
Increases lipolysis.
Nervous system
Binds to TRß1 receptors. Promotes normal brain development and appetite.
Symptoms
Dermopathy
Fatigue
Tachycardia
Exophthalmos
Bulging eyes.
Change in menstrual cycles
Since thyroid hormones impact estrogen levels, which regulate the monthly menstrual cycle in females, hyperthyroidism and increased estrogen levels can delay menstruation and cause oligomenorrhea or amenorrhea. At the end of the luteal phase, a drop in estrogen levels, among other hormonal changes, initiates the onset of menstruation. Prolonged elevated levels of estrogen in hyperthyroid females may cause irregular menstruation cycles. Graves' disease has been associated with infertility, increased follicular atresia, menstrual irregularity, and ovarian cysts.
Silva, S. F., Ocarino, N. M., Serakides, R. Thyroid hormones and female reproduction. (2018). Biology of Reproduction. 99(5):907-921. doi:10.1093/biolre/ioy115
Goiter
Enlargement of the thyroid gland. Increased TSH secretion causes and increase in the level of T4 and T3. Excess T4 and T3 stimulate hypertrophy of the thyroid gland.
Weight loss despite normal eating habits
Since thyroid hormones have a calorigenic effect on the entire body, overstimulation of TSH in Graves' disease causes an increase in metabolism and oxygen consumption.
Heat sensitivity
Fine tremor of hands or fingers
Anxiety or irritability
Hypothalamic-pituitary-gonadal axis
Hyperthyroidism and increased levels of T4/T3 production has consequences on the female reproductive system via several mechanisms.
Firstly, increased levels of T4/T3 in the body cause an increase in the production of thyroxine binding globulin (TBG) and sex hormone binding globulin (SHBG). More TBG and SHBG increases the levels of total circulating steroid hormones and can decrease the levels of free hormones. Increased TBG and SHBG also leads to a decrease in the metabolic clearance of sex steroids in hyperthyroidism.
Secondly, hyperthyroidism causes increased levels of sex steroid hormones such as estrogen, androstenedione, and testosterone. Since estrogen can regulate the monthly menstrual cycle in females, hyperthyroidism and increased estrogen levels can delay menstruation, cause oligomenorrhea, or cause amenorrhea. At the end of the luteal phase, a drop in estrogen levels initiates the onset of menstruation. Prolonged elevated levels of estrogen in hyperthyroid females may cause irregular menstruation. Graves' disease has been associated with infertility, increased follicular atresia, menstrual irregularity, and ovarian cysts.
Silva, S. F., Ocarino, N. M., Serakides, R. Thyroid hormones and female reproduction. (2018). Biology of Reproduction. 99(5):907-921. doi:10.1093/biolre/ioy115
Hypothalamus
The hypothalamus releases GnRH from the median eminence (specifically the arcuate nucleus of the pre-optic area) onto the anterior pituitary (AP) gonadotrope cells in a pulsatile fashion.
In Graves' disease, increased levels of estrogen, progesterone, and testosterone can have negative feedback onto the hypothalamus causing less GnRH release and less synthesis of sex steroid hormones.
Anterior Pituitary
GnRH binds to a G-protein coupled receptor in the pituitary gonadotrope cell and activates the phospholipase C (PLC) pathway. Second messenger PLC converts PIP2 into IP3 and DAG. IP3 and DAG activate the production of protein kinase C and the release of intracellular calcium. The pituitary gonadotrope then differentially synthesizes peptide hormones LH and FSH based on the speed of GnRH pulses. If the pulsatile release of GnRH is slow, then the anterior pituitary (AP) synthesizes and secretes FSH. If the pulsatile release of GnRH is fast, then the AP synthesizes and secretes LH.
In Graves' disease, increased levels of estrogen, progesterone, and testosterone can negatively feedback onto the AP causing less LH and FSH release and less synthesis of sex steroid hormones.
Gonads
Gonadal cells have receptors that bind LH and FSH, respectively. Following hormone binding, the gonadal cell activates adenylate cyclase (AC) which increases intracellular cAMP and increases production of protein kinase A (PKA). PKA permits steroidogenesis (synthesis of estrogen, progesterone, and testosterone) and gametogenesis.
In Graves' disease, the negative feedback effects from estrogen, progesterone, and testosterone on the hypothalamus and AP would cause the gonads to produce less sex steroid hormones.
Ovaries
The ovaries in females secrete sex steroid hormones. LH binds to LH receptors on theca cells (TCs) of ovarian follicles and stimulates TCs to synthesize progestins and androgens. Androgens enter the granulosa cells (GCs) and convert to estrogens through aromatization. FSH binds to FSH receptors on GCs of ovarian follicles and stimulates GCs to increase the production of steroidogenic enzymes, activins, and inhibins.
Activin
FSH binds to receptors on GCs to increase the production of steroidogenic enzymes, activins, and inhibins.
FSH binds to receptors on granulosa cells to increase the production of steroidogenic enzymes, activins, and inhibins.
Progesterone
Negative feedback onto hypothalamus and AP. Regulates release of GnRH, LH, and FSH.
In Graves' disease, increased levels of T4/T3 causes an increase in steroidogenesis. Increased progesterone causes increased negative feedback onto the release of GnRH, FSH, and LH. Dysregulation of the HPG and HPO axes can impact normal, monthly reproductive function in females.
Silva, S. F., Ocarino, N. M., Serakides, R. Thyroid hormones and female reproduction. (2018). Biology of Reproduction. 99(5):907-921. doi:10.1093/biolre/ioy115
Estrogen
Negative feedback and positive feedback onto hypothalamus and AP. Regulates release of GnRH, LH, and FSH.
In Graves' disease, increased levels of T4/T3 causes an increase in steroidogenesis. Increased estrogen causes increased negative feedback onto the release of GnRH, FSH, and LH. This consequence has an impact on the initiation of the normal menstrual cycle and can cause menstruation to be irregular, delayed, or absent. Note that a small spike in estrogen in the follicular phase of the ovarian cycle helps to induce the large LH surge that causes ovulation. A chronically high or low level of estrogen may fail to initiate the LH surge and other important events in the ovarian and endometrial cycles. This can have negative impacts on ovulation and therefore fertility.
Reproductive tract and glands
Breast tissue
Muscle
Bone
CNS
Testes
The seminiferous tubules within the testes in males secrete sex steroid hormones. LH binds to LH receptors on Leydig cells in the testes and activates them to secrete testosterone. Testosterone enters Sertoli cells and is converted to estrogen via aromatization. This estrogen acts on Leydig cells. Testosterone also promotes the production of growth factors in Sertoli cells which then go on to act on Leydig cells and stimulate more testosterone production. FSH binds to FSH receptors on Sertoli cells and stimulates them to secrete inhibin, androgen binding protein, and developing sperm. The reciprocal interactions between Leydig and Sertoli cells is called crosstalk.
Inhibin
Negative feedback onto FSH release from the AP.
Anterior pituitary
Negative feedback onto AP to reduce the release of FSH.
Testosterone
Negative feedback onto hypothalamus and AP.
In Graves' disease, increased levels of T4/T3 causes an increase in steroidogenesis. Increased testosterone causes increased negative feedback onto the release of GnRH, FSH, and LH.
Silva, S. F., Ocarino, N. M., Serakides, R. Thyroid hormones and female reproduction. (2018). Biology of Reproduction. 99(5):907-921. doi:10.1093/biolre/ioy115