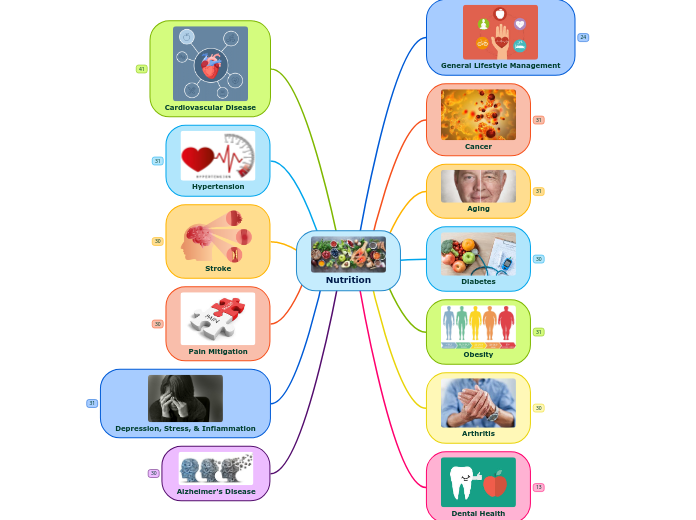
Nutrition
Alzheimer's Disease
Nutrition and AGE-ing: Focusing on Alzheimer's Disease
Abstract
Recently, the role of food and nutrition in preventing or delaying chronic disability in the elderly population has received great attention. Thanks to their ability to influence biochemical and biological processes, bioactive nutrients are considered modifiable factors capable of preserving a healthy brain status. A diet rich in vitamins and polyphenols and poor in saturated fatty acids has been recommended. In the prospective of a healthy diet, cooking methods should be also considered. In fact, cooking procedures can modify the original dietary content, contributing not only to the loss of healthy nutrients, but also to the formation of toxins, including advanced glycation end products (AGEs). These harmful compounds are adsorbed at intestinal levels and can contribute to the ageing process. The accumulation of AGEs in ageing ("AGE-ing") is further involved in the exacerbation of neurodegenerative and many other chronic diseases. In this review, we discuss food's dual role as both source of bioactive nutrients and reservoir for potential toxic compounds-paying particular attention to the importance of proper nutrition in preventing/delaying Alzheimer's disease. In addition, we focus on the importance of a good education in processing food in order to benefit from the nutritional properties of an optimal diet.
Does Treating Vascular Risk Factors Prevent Dementia and Alzheimer's Disease? A Systematic Review and Meta-Analysis
Abstract
Background: Epidemiological evidence has associated Alzheimer's disease (AD) with vascular risk factors (VRFs), but whether treatment of VRFs reduces the incidence of dementia and AD is uncertain.
Objective: To conduct a systematic review and meta-analysis to summarize available data on the impact of treatment of VRFs on dementia and AD incidence.
Methods: Pertinent studies published until 1 January 2018 were identified from PubMed. Both randomized controlled trials (RCT) and prospective studies that investigated the impact of treatment of VRFs on dementia or AD incidence were included.
Results: Eight RCTs and 52 prospective studies were identified. Antihypertensive treatment was associated with a non-significant reduced risk of dementia in RCTs (n = 5; relative risk [RR], 0.84; 95% confidence interval [CI], 0.69-1.02) and prospective studies (n = 3; RR, 0.77; 95% CI, 0.58-1.01) and with reduced AD risk in prospective studies (n = 5; RR = 0.78; 95% CI, 0.66-0.91). In prospective studies, treatment of hyperlipidemia with statins, but not nonstatin lipid-lowering agents, was associated with reduced risk of dementia (n = 17; RR, 0.77; 95% CI, 0.63-0.95) and AD (n = 13; RR, 0.86; 95% CI, 0.80-0.92). The single RCT on statins and dementia incidence showed no association. Data from one RCT and six prospective studies did not support a beneficial impact of antidiabetic drugs or insulin therapy on dementia risk.
Conclusion: Current evidence indicates that antihypertensives and statins might reduce the incidence of dementia and AD. Further trials to determine the effect of VRF on AD are needed.
Keywords: Alzheimer’s disease; dementia; meta-analysis; prevention; prospective studies; randomized controlled trials; risk factors; systematic review.
A meta‐analysis of nutrition interventions on mental development of children under‐two in low‐ and middle‐income countries
AbstractInterventions to improve nutritional status of young children in low‐ and middle‐income countries (LMIC) may have the added benefit of improving their mental and motor development. This meta‐analysis updates and goes beyond previous ones by answering two important questions: (1) do prenatal and postnatal nutritional inputs improve mental development, and (2) are effects on mental development associated with two theoretically interesting mediators namely physical growth and motor development? The meta‐analysis of articles on Medline, PsycINFO, Global Health and Embase was limited to randomized trials in LMICs, with mental development of children from birth to age two years as an outcome. The initial yield of 2689 studies was reduced to 33; 12 received a global quality rating of strong. Of the 10 prenatal and 23 postnatal nutrition interventions, the majority used zinc, iron/folic acid, vitamin A or multiple micronutrients, with a few evaluating macronutrients. The weighted mean effect size, Cohen's d (95% CI) for prenatal and postnatal nutrition interventions on mental development was 0.042 (−0.0084, 0.092) and 0.076 (0.019, 0.13), respectively. Postnatal supplements consisting of macronutrients yielded an effect size d (95% CI) of 0.14 (0.0067, 0.27), multiple micronutrients 0.082 (−0.012, 0.18) and single micronutrients 0.058 (−0.0015, 0.12). Motor development, but not growth status, effect sizes were significantly associated with mental development in postnatal interventions. In summary, nutrition interventions had small effects on mental development. Future studies might have greater effect if they addressed macronutrient deficiencies combined with child stimulation and hygiene and sanitation interventions.
A Review of Studies on the Effect of Iron Deficiency on Cognitive Development in Children
ABSTRACT
Studies on the effect of iron deficiency on children's cognition and behavior are selectively reviewed, looking for evidence of a causal relationship. Most correlational studies have found associations between iron-deficiency anemia and poor cognitive and motor development and behavioral problems. Longitudinal studies consistently indicate that children anemic in infancy continue to have poorer cognition, school achievement, and more behavior problems into middle childhood. However, the possible confounding effects of poor socioeconomic backgrounds prevent causal inferences from being made. In anemic children <2 y old, short-term trials of iron treatment have generally failed to benefit development. Most longer trials lacked randomized placebo groups and failed to produce benefits. Only one small randomized controlled trial (RCT) has shown clear benefits. It therefore remains uncertain whether the poor development of iron-deficient infants is due to poor social backgrounds or irreversible damage or is remediable with iron treatment. Similarly, the few preventive trials have had design problems or produced no or questionable benefits only. For children >2 y old, the evidence from RCT is reasonably convincing but not conclusive. RCT of iron treatment are warranted especially in younger children.
Dietary DHA and health: cognitive function ageing
Abstract
DHA is a key nutritional n-3 PUFA and needs to be supplied by the human diet. DHA is found in significant amounts in the retinal and neuronal cell membranes due to its high fluidity. Indeed, DHA is selectively concentrated in the synaptic and retinal membranes. DHA is deemed to display anti-inflammatory properties and to reduce the risk of CVD. Consumption of larger amounts of DHA appears to reduce the risk of depression, bipolar disorder, schizophrenia and mood disorders. Conversely, it has been shown that loss of DHA from the nerve cell membrane leads to dysfunction of the central nervous system in the form of anxiety, irritability, susceptibility to stress, dyslexia, impaired memory and cognitive functions, and extended reaction times. DHA plays an important role in ensuring a healthy ageing, by thwarting macular degeneration, Alzheimer’s disease, and other brain disorders at the same time as enhancing memory and strengthening neuroprotection in general. A reduced level of DHA is associated with cognitive decline during ageing. Different mechanisms for this fundamental DHA role have been put forward. Namely, neuroprotectin D1, a DHA derivative, may support brain cell survival and repair through neurotrophic, anti-apoptotic, and anti-inflammatory signalling. Many of the effects of DHA on the neurological system may be related to signalling connections, thus leading to the study of the related signalolipidomics. Therefore, the present review will focus on the influence of DHA deficiency upon ageing, with specific emphasis upon neurological disorders related to cognitive function and mental health.
Diet, nutrition and the ageing brain: current evidence and new directions
Abstract
Globally populations are ageing. By 2050, it is estimated that there will be two billion people aged 60 years or over, of which 131 million are projected to be affected by dementia, while depression is predicted to be the second leading cause of disability worldwide by 2020. Preventing or delaying the onset of these disorders should therefore be a public health priority. There is some evidence linking certain dietary patterns, particularly the Mediterranean diet, with a reduced risk of dementia and depression. Specific dietary components have also been investigated in relation to brain health, with emerging evidence supporting protective roles for n-3 PUFA, polyphenols, vitamin D and B-vitamins. At this time, the totality of evidence is strongest in support of a role for folate and the metabolically related B-vitamins (vitamin B12, vitamin B6 and riboflavin) in slowing the progression of cognitive decline and possibly reducing the risk of depression in ageing. Future studies incorporating new technologies, such as MRI and magnetoencephalography, offer much promise in identifying effective nutrition interventions that could reduce the risk of cognitive and mental disorders. This review will explore the ageing brain and the emerging evidence linking diet and specific nutrients with cognitive function and depression in ageing, with the potential to develop strategies that could improve quality of life in our ageing population.
Keywords: AD Alzheimer's disease; MCI mild cognitive impairment; RCT randomised controlled trial; Ageing; B-vitamins; Cognition; Depression; Nutrition.
Impact of Nutrition on Growth, Brain, and Cognition
Abstract
Brain development begins shortly after conception and continues throughout early childhood and into adolescence and early adulthood. During the first 1,000 days (conception to age 2), brain development is rapid, with nutrition playing an important role in the expression of the genetic code. Recent animal and human findings have illustrated that the timing, chronicity, and severity of nutritional deficiencies has differential effects on brain development and on subsequent cognitive and emotional processes. Evidence from intervention trials and longitudinal studies has shown the interactive nature of environmental influences on brain functioning and cognition over time, opening new opportunities for interventions to prevent or overcome potential adversities, including nutritional deficiencies. Strategies to enhance early brain development and promote children's cognitive functioning are based on integrated multisectoral interventions that prevent or alleviate nutritional deficiencies, while promoting developmental opportunities and responsive caregiving. Investing in early intervention based on evidence from brain development and ensuring nutritional adequacy throughout the first 1,000 days are effective means to ensure that children have the necessary health, cognition, creativity, and commitment to achieve the Sustainable Development Goals.
Neuroprotective Diets Are Associated with Better Cognitive Function: The Health and Retirement Study
AbstractObjectives
To evaluate the association between the Mediterranean diet (MedDiet) and the Mediterranean‐DASH diet Intervention for Neurodegeneration Delay (MIND diet) and cognition in a nationally representative population of older U.S. adults.
Design
Population‐based cross‐sectional study.
Setting
Health and Retirement Study.
Participants
Community‐dwelling older adults (N = 5,907; mean age 67.8 ± 10.8).
Measurements
Adherence to dietary patterns was determined from food frequency questionnaires using criteria determined a priori to generate diet scores for the MedDiet (range 0–55) and MIND diet (range 0–15). Cognitive performance was measured using a composite test score of global cognitive function (range 0–27). Linear regression was used to compare cognitive performance according to tertiles of dietary pattern. Logistic regression was used to examine the association between dietary patterns and clinically significant cognitive impairment. Models were adjusted for age, sex, race, educational attainment, and other health and lifestyle covariates.
Results
Participants with mid (odds ratio (OR) = 0.85, 95% confidence interval (CI) = 0.71–1.02, P = .08) and high (OR 0.65, 95% CI = 0.52–0.81, P < .001) MedDiet scores were less likely to have poor cognitive performance than those with low scores in fully adjusted models. Results for the MIND diet were similar. Higher scores in each dietary pattern were independently associated with significantly better cognitive function (P < .001) in a dose‐response manner (P trend < .001).
Conclusion
In a large nationally representative population of older adults, greater adherence to the MedDiet and MIND diet was independently associated with better cognitive function and lower risk of cognitive impairment. Clinical trials are required to elucidate the role of dietary patterns in cognitive aging.
Mediterranean-type diet and brain structural change from 73 to 76 years in a Scottish cohort
Abstract
Objective: To assess the association between Mediterranean-type diet (MeDi) and change in brain MRI volumetric measures and mean cortical thickness across a 3-year period in older age (73–76 years).
Methods: We focused on 2 longitudinal brain volumes (total and gray matter; n = 401 and 398, respectively) plus a longitudinal measurement of cortical thickness (n = 323), for which the previous cross-sectional evidence of an association with the MeDi was strongest. Adherence to the MeDi was calculated from data gathered from a food frequency questionnaire at age 70, 3 years prior to the baseline imaging data collection.
Results: In regression models adjusting for relevant demographic and physical health indicators, we found that lower adherence to the MeDi was associated with greater 3-year reduction in total brain volume (explaining 0.5% of variance, p < 0.05). This effect was half the size of the largest covariate effect (i.e., age). Cross-sectional associations between MeDi and baseline MRI measures in 562 participants were not significant. Targeted analyses of meat and fish consumption did not replicate previous associations with total brain volume or total gray matter volume.
Conclusions: Lower adherence to the MeDi in an older Scottish cohort is predictive of total brain atrophy over a 3-year interval. Fish and meat consumption does not drive this change, suggesting that other components of the MeDi or, possibly, all of its components in combination are responsible for the association.
Nutrients and bioactives in green leafy vegetables and cognitive decline
Abstract
Objective To increase understanding of the biological mechanisms underlying the association, we investigated the individual relations to cognitive decline of the primary nutrients and bioactives in green leafy vegetables, including vitamin K (phylloquinone), lutein, β-carotene, nitrate, folate, kaempferol, and α-tocopherol.
Methods This was a prospective study of 960 participants of the Memory and Aging Project, ages 58–99 years, who completed a food frequency questionnaire and had ≥2 cognitive assessments over a mean 4.7 years.
Results In a linear mixed model adjusted for age, sex, education, participation in cognitive activities, physical activities, smoking, and seafood and alcohol consumption, consumption of green leafy vegetables was associated with slower cognitive decline; the decline rate for those in the highest quintile of intake (median 1.3 servings/d) was slower by β = 0.05 standardized units (p = 0.0001) or the equivalent of being 11 years younger in age. Higher intakes of each of the nutrients and bioactives except β-carotene were individually associated with slower cognitive decline. In the adjusted models, the rates for the highest vs the lowest quintiles of intake were β = 0.02, p = 0.002 for phylloquinone; β = 0.04, p = 0.002 for lutein; β = 0.05, p < 0.001 for folate; β = 0.03, p = 0.02 for α-tocopherol; β = 0.04, p = 0.002 for nitrate; β = 0.04, p = 0.003 for kaempferol; and β = 0.02, p = 0.08 for β-carotene.
Conclusions Consumption of approximately 1 serving per day of green leafy vegetables and foods rich in phylloquinone, lutein, nitrate, folate, α-tocopherol, and kaempferol may help to slow cognitive decline with aging.
A Periodic Diet that Mimics Fasting Promotes Multi-System Regeneration, Enhanced Cognitive Performance, and Healthspan
Summary
Prolonged fasting (PF) promotes stress resistance, but its effects on longevity are poorly understood. We show that alternating PF and nutrient-rich medium extended yeast lifespan independently of established pro-longevity genes. In mice, 4 days of a diet that mimics fasting (FMD), developed to minimize the burden of PF, decreased the size of multiple organs/systems, an effect followed upon re-feeding by an elevated number of progenitor and stem cells and regeneration. Bi-monthly FMD cycles started at middle age extended longevity, lowered visceral fat, reduced cancer incidence and skin lesions, rejuvenated the immune system, and retarded bone mineral density loss. In old mice, FMD cycles promoted hippocampal neurogenesis, lowered IGF-1 levels and PKA activity, elevated NeuroD1, and improved cognitive performance. In a pilot clinical trial, three FMD cycles decreased risk factors/biomarkers for aging, diabetes, cardiovascular disease, and cancer without major adverse effects, providing support for the use of FMDs to promote healthspan.
High Low-Density Lipoprotein Cholesterol Inversely Relates to Dementia in Community-Dwelling Older Adults: The Shanghai Aging Study
Background: The relationship between cholesterol and cognitive function is unclear from the previous studies. This study was conducted to explore this association in older Chinese adults.
Methods: Data were from the Shanghai Aging Study, comprising 3,836 residents aged 50 years or over in an urban community. Diagnoses of dementia and mild cognitive impairment were established according to the fourth edition of diagnostic and statistical manual of mental disorders (DSM-IV) and Petersen criteria. Multivariate logistic regression models, non-matched and propensity score (PS) matched, were used to examine the association between cholesterol levels and cognitive function.
Results: There was a significantly higher proportion of participants with low levels of total cholesterol (TC) and low density lipoprotein cholesterol (LDL-C) in the dementia group than in groups without dementia (P < 0.05). High LDL-C level was inversely associated with dementia, with a negative trend in the PS matched model. TC and high density lipoprotein cholesterol (HDL-C) were not significantly related to dementia in either non-matched models or PS matched models.
Conclusion: Our result indicates that high level of LDL-C is inversely associated with dementia. High level of LDL-C may be considered as a potential protective factor against cognition decline.
Rivastigmine improves patients’ appetite by increasing serum active ghrelin and cortisol in Alzheimer’s disease
Background: Weight loss accelerates the cognitive decline and increases the mortality of patients with dementia. While acetylcholinesterase inhibitors are known to cause appetite loss, we have sometimes experienced that changing the medication from donepezil (acetylcholinesterase inhibitor) to rivastigmine (acetyl- and butyrylcholinesterase inhibitor) improves patients’ appetite.
Appetite Regulation and the Peripheral Sink Amyloid beta Clearance Pathway in Diabetes and Alzheimer’s Disease
Abstract
The peripheral sink amyloid beta clearance pathway in diabetes and Alzheimer’s disease is defective. Appetite control and intact Sirtuin 1 are critical to prevent inactivation of the peripheral sink amyloid beta clearance pathway. Factors such as drugs, caffeine, Indian spices, LPS, mycotoxins and environmental xenobiotics determine longevity in various species when compared to man. Sirt 1 and circadian regula¬tion of the adipose tissue-liver interaction are essential to determine toxic antigenic Aβ structures with immune dysregulation connected to diabetes and Alzheimer’s disease.
A Phase IIa Randomized Control Trial of VEL015 (Sodium Selenate) in Mild-Moderate Alzheimer’s Disease
Abstract: Background: There is increasing interest in targeting hyperphosphorylated tau (h-tau) as a disease modifying approach for Alzheimer’s disease (AD). Sodium selenate directly stimulates the activity of PP2A, the main enzyme responsible for h-tau dephosphorylation in the brain. Objective: This study assessed the safety and tolerability of 24-week treatment with VEL015 (sodium selenate) in AD. Investigating the effects of VEL015 on cognitive, CSF, and neuroimaging biomarkers of AD were secondary, exploratory objectives. Data were used to identify biomarkers showing most promise for use in subsequent efficacy trials. Methods: A 24-week, multicenter, Phase IIa, double-blinded randomized controlled trial. Forty patients aged ≥55 y with mild-moderate AD (MMSE 14–26) were randomized to supranutritional (VEL015 10 mg tds [n = 20]) and control (VEL015 320μg tds [n = 10] or placebo [n = 10]) groups. Patients were regularly monitored for safety, adverse events (AEs), and protocol compliance. Exploratory biomarkers included cognitive tests, neuroimaging (diffusion MR), and CSF (p-tau, t-tau, and Aβ1-42). Results: Thirty-six (90%; [supranutritional n = 18, control/placebo n = 18]) patients completed the trial. There were no differences in the incidence of specific AEs between groups. Only one secondary biomarker, diffusion MR measures, showed group differences, with less deterioration in the supranutritional group (p < 0.05). Conclusion: Treatment with VEL015 at doses up to 30 mg per day for 24 weeks was safe and well-tolerated in patients with AD. Diffusion MR measures appear to be the most sensitive biomarkers to assess disease progression over 24 weeks.
Sodium selenate activated Wnt/β-catenin signaling and repressed amyloid-β formation in a triple transgenic mouse model of Alzheimer's disease
Abstract
Accumulating evidences show that
selenium
dietary intake is inversely associated with the mortality of
Alzheimer's disease
(AD).
Sodium selenate
has been reported to reduce
neurofibrillary tangles
(NFT) in the tauopathic mouse models, but its effects on the Wnt/β-catenin
signaling pathway
and APP processing remain unknown during AD formation. In this paper, triple transgenic AD mice (3 × Tg-AD) had been treated with sodium selenate in drinking water for 10 month before the detection of hippocampal pathology. Increased Aβ generation, tau
hyperphosphorylation
and
neuronal apoptosis
were found in the
hippocampus
of AD model mouse. Down-regulation of Wnt/β-catenin signaling is closely associated with the alteration of AD pathology. Treatment with sodium selenate significantly promoted the activity of
protein phosphatases
of type 2A (PP2A) and repressed the hallmarks of AD. Activation of PP2A by sodium selenate could increase active
β-catenin
level and inhibit GSK3β activity in the
hippocampal tissue
and primarily
cultured neurons
of AD model mouse, leading to activation of Wnt/β-catenin signaling and
transactivation
of target genes, including positively-regulated
genes c-myc
,
survivin
, TXNRD2 and negatively-regulated gene BACE1. Meanwhile, APP
phosphorylation
was also reduced on the Thr668 residue after selenate treatment, causing the decreases of APP cleavage and Aβ generation. These findings reveal that the Wnt/β-catenin signaling is a potential target for prevention of AD and sodium selenate may be developed as a new drug for AD treatment.
Sodium oligomannate therapeutically remodels gut microbiota and suppresses gut bacterial amino acids-shaped neuroinflammation to inhibit Alzheimer’s disease progression
Abstract
Recently, increasing evidence has suggested the association between gut dysbiosis and Alzheimer’s disease (AD) progression, yet the role of gut microbiota in AD pathogenesis remains obscure. Herein, we provide a potential mechanistic link between gut microbiota dysbiosis and neuroinflammation in AD progression. Using AD mouse models, we discovered that, during AD progression, the alteration of gut microbiota composition leads to the peripheral accumulation of phenylalanine and isoleucine, which stimulates the differentiation and proliferation of pro-inflammatory T helper 1 (Th1) cells. The brain-infiltrated peripheral Th1 immune cells are associated with the M1 microglia activation, contributing to AD-associated neuroinflammation. Importantly, the elevation of phenylalanine and isoleucine concentrations and the increase of Th1 cell frequency in the blood were also observed in two small independent cohorts of patients with mild cognitive impairment (MCI) due to AD. Furthermore, GV-971, a sodium oligomannate that has demonstrated solid and consistent cognition improvement in a phase 3 clinical trial in China, suppresses gut dysbiosis and the associated phenylalanine/isoleucine accumulation, harnesses neuroinflammation and reverses the cognition impairment. Together, our findings highlight the role of gut dysbiosis-promoted neuroinflammation in AD progression and suggest a novel strategy for AD therapy by remodelling the gut microbiota.
Sodium rutin ameliorates Alzheimer’s disease–like pathology by enhancing microglial amyloid-β clearance
Abstract
The accumulation of aggregated amyloid-β (Aβ) in the brain is the first critical step in the pathogenesis of Alzheimer’s disease (AD), which also includes synaptic impairment, neuroinflammation, neuronal loss, and eventual cognitive defects. Emerging evidence suggests that impairment of Aβ phagocytosis and clearance is a common phenotype in late-onset AD. Rutin (quercetin-3-rutinoside) has long been investigated as a natural flavonoid with different biological functions in some pathological circumstances. Sodium rutin (NaR), could promote Aβ clearance by increasing microglial by increasing the expression levels of phagocytosis-related receptors in microglia. Moreover, NaR promotes a metabolic switch from anaerobic glycolysis to mitochondrial OXPHOS (oxidative phosphorylation), which could provide microglia with sufficient energy (ATP) for Aβ clearance. Thus, NaR administration could attenuate neuroinflammation and enhance mitochondrial OXPHOS and microglia-mediated Aβ clearance, ameliorating synaptic plasticity impairment and eventually reversing spatial learning and memory deficits. Our findings suggest that NaR is a potential therapeutic agent for AD.
[Prevention of Alzheimer's Disease and Nutrients].
Abstract
The dietary recommendations for the prevention and management of Alzheimer's disease (AD), are the Mediterranean diet and the Japanese-style diet, both of which contain well-balanced nutrients from fish and vegetables. These diets are rich in vitamin E, carotenes, antioxidant flavonoids, vitamin B12, folate, and n-3PUFA. According to recent review supplementation of folate and vitamin E may protect against elderly people's cognitive decline when the serum folate is <12 nmol/L or the vitamin E intake is <6.1 mg/day. Another nutritional topic with regard to dementia and diet is the association of type-2 diabetes and hyperinsulinemia with AD. Expression array data of the brain tissue of AD patients in the Hisayama study strongly suggests a disturbance in insulin signaling in the AD brain. The dysfunction of insulin signaling could directly lead to disrupted glucose utilization in the AD brain. Instead of improperly utilized glucose, the medium chain triglyceride ketone bodies can be an alternative energy resource for the AD brain. In conclusion, the dietary recommendations for the prevention and management of AD are a high consumption of fish, vegetables, and low glycemic index fruits; a moderate amount of meat and dairy products; and a lower amount of carbohydrates and refined sugar.
Sugary beverage intake and preclinical Alzheimer's disease in the community
Abstract
Introduction
Excess
sugar consumption
has been linked with Alzheimer's disease (AD) pathology in animal models.
Methods
We examined the cross-sectional association of sugary beverage consumption with neuropsychological (N = 4276) and
magnetic resonance imaging
(N = 3846) markers of preclinical Alzheimer's disease and vascular brain injury (VBI) in the community-based Framingham Heart Study. Intake of sugary beverages was estimated using a
food frequency questionnaire
.
Results
Relative to consuming less than one sugary beverage per day, higher intake of sugary beverages was associated with lower total brain volume (1–2/day, β ± standard error [SE] = −0.55 ± 0.14 mean percent difference, P = .0002; >2/day, β ± SE = −0.68 ± 0.18, P < .0001), and poorer performance on tests of
episodic memory
(all P < .01). Daily fruit juice intake was associated with lower total brain volume, hippocampal volume, and poorer episodic memory (all P < .05). Sugary beverage intake was not associated with VBI in a consistent manner across outcomes.
Discussion
Higher intake of sugary beverages was associated cross-sectionally with markers of preclinical AD.
Refined carbohydrate‐rich diet is associated with long‐term risk of dementia and Alzheimer's disease in apolipoprotein E ε4 allele carriers
AbstractIntroduction
In animal models, refined carbohydrates (RF) worsen Alzheimer's disease (AD). However, the long‐term effects of high RF intake on the risk of dementia and AD are poorly described in epidemiological studies. Moreover, the interaction between RF and the apolipoprotein E ε4 allele (APOE‐ε4) is unknown. Our study investigated whether RF‐rich diets are associated with the risk of dementia and AD.
Methods
The glycemic load (GL) was quantified in 2777 elderly participants from the French Three‐City Study to estimate RF intake. Then, the associations between GL and risk of dementia and AD, and the interaction with APOE‐ε4 over a 12‐year period were assessed using proportional hazards models.
Results
After adjustment for potential confounders, high afternoon‐snack GL was associated with increased dementia and AD risk in APOE‐ε4 carriers (hazard ratio = 1.27 [1.03–1.56]).
Discussion
This study highlights that RF‐rich diets are a risk factor for dementia and AD in APOE‐ε4 carriers.
Alterations in cholesterol metabolism as a risk factor for developing Alzheimer’s disease: Potential novel targets for treatment
Abstract
Alzheimer's disease (AD) is the most common form of dementia and it is characterized by the deposition of
amyloid-β
(Aβ) plaques and
neurofibrillary tangles
in the brain. However, the complete pathogenesis of the disease is still unknown. High level of serum cholesterol has been found to positively correlate with an increased risk of dementia and some studies have reported a decreased prevalence of AD in patients taking cholesterol-lowering drugs. Years of research have shown a strong correlation between blood
hypercholesterolemia
and AD, however cholesterol is not able to cross the Blood Brain Barrier (BBB) into the brain. Cholesterol lowering therapies have shown mixed results in cognitive performance in AD patients, raising questions of whether brain
cholesterol metabolism
in the brain should be studied separately from peripheral cholesterol metabolism and what their relationship is. Unlike cholesterol, oxidized cholesterol metabolites known as
oxysterols
are able to cross the BBB from the circulation into the brain and vice-versa. The main oxysterols present in the circulation are 24S-hydroxycholesterol and
27-hydroxycholesterol
. These oxysterols and their catalysing enzymes have been found to be altered in AD brains and there is evidence indicating their influence in the progression of the disease. This review gives a broad perspective on the relationship between hypercholesterolemia and AD, cholesterol lowering therapies for AD patients and the role of oxysterols in pathological and non-pathological conditions. Also, we propose cholesterol metabolites as valuable targets for prevention and alternative AD treatments.
Cholesterol-metabolizing enzyme cytochrome P450 46A1 as a pharmacologic target for Alzheimer's disease
Abstract
Cytochrome P450 46A1
(CYP46A1 or cholesterol 24-hydroxylase) controls cholesterol elimination from the brain and plays a role in higher order brain functions. Genetically enhanced CYP46A1 expression in mouse models of
Alzheimer's disease
mitigates the manifestations of this disease. We enhanced CYP46A1 activity pharmacologically by treating 5XFAD mice, a model of rapid amyloidogenesis, with a low dose of the anti-HIV medication
efavirenz
. Efavirenz was administered from 1 to 9 months of age, and mice were evaluated at specific time points. At one month of age, cholesterol homeostasis was already disturbed in the brain of 5XFAD mice. Nevertheless, efavirenz activated CYP46A1 and mouse cerebral cholesterol turnover during the first four months of administration. This treatment time also reduced
amyloid
burden and
microglia
activation in the cortex and
subiculum
of 5XFAD mice as well as protein levels of
amyloid precursor protein
and the expression of several genes involved in inflammatory response. However, mouse short-term memory and long-term
spatial memory
were impaired, whereas learning in the context-dependent fear test was improved. Additional four months of drug administration (a total of eight months of treatment) improved long-term spatial memory in the treated as compared to the untreated mice, further decreased
amyloid-β
content in 5XFAD brain, and also decreased the mortality rate among male mice. We propose a mechanistic model unifying the observed efavirenz effects. We suggest that CYP46A1 activation by efavirenz could be a new anti-Alzheimer's disease treatment and a tool to study and identify normal and pathological brain processes affected by cholesterol maintenance.
Ketogenic diets and Alzheimer’s disease
Abstract
Alzheimer’s disease (AD) is a progressive neurodegenerative disorder characterized by decline in
cognitive functions
and associated with the neuropathological hallmarks of
amyloid
β-peptide plaques and
neurofibrillary tangles
. Cerebral
glucose uptake and metabolism
deteriorate in AD and this hypometabolism precedes the onset of clinical signs in AD. The early decline in brain glucose metabolism in AD has become a potential target for therapeutic intervention. This has led to investigations assessing the supplementation of the normal glucose supply with
ketone bodies
which are produced by the body during glucose deprivation and can be metabolized by the brain when
glucose utilization
is impaired. The present review provides a synopsis of
preclinical studies
and clinical trials assessing the efficacy of
ketogenic diets
in the treatment of AD. Both the direct administration of ketone bodies and the use of high-fat, low-carbohydrate ketogenic diets have been shown to be efficacious in animal models of AD and clinical trials with AD patients. The mechanism underlying the efficacy of ketogenic diets remains unclear, but some evidence points to the normalization of aberrant energy metabolism. At present there is only limited evidence of the usefulness of ketogenic diets in AD. However, this dietary approach seems to be promising and deserves further clinical investigations.
Association of Nutrients with Biomarkers of Alzheimer’s Disease
Abstract
Prospective cohort studies, cross-sectional surveys, autopsy studies and intervention clinical trials that investigated the association between nutrients and Alzheimer’s disease (AD) have been reviewed. To estimate the relationship between specific nutrient intake and the risk of AD, Cochrane Library, PubMed, EMBASE, and the Fisher Center for Alzheimer’s Research Foundation were searched for this purpose. Most published observational studies found an inverse relationship between vitamins, n-3 fatty acids and AD. The majority of intervention studies support the beneficial effect of combined vitamins and n-3 fatty acids providing them in the early stages of the disease. Only vitamin E and Zn supplementation failed to show any significant difference on the study population. On the other hand, high dietary intake of saturated fat and brain metal accumulation were positively associated with the incidence of AD.
Dietary Fat Intake and Risk of Alzheimer's Disease and Dementia: A Meta-Analysis of Cohort Studies
Background: Epidemiological studies showed that dietary fat intake is associated with Alzheimer's disease (AD) and dementia risk, however, the association remain inconsistent. This metaanalysis aimed to systematically examine the association of dietary fat intake with AD and dementia risk.
Methods: We have systematically searched PubMed, Embase and the Cochrane Library up to May 1st 2017. Prospective cohort studies were included if they reported on the association of dietary fat intake with AD and dementia risk. Multivariate-adjusted relative risks (RRs) for the highest versus lowest category were pooled by using a random-effects model.
Results: A total of 8630 participants and 633 cases from four independent prospective cohort studies were included in the present meta-analysis. A higher dietary saturated fat intake was significantly associated with an increased risk of 39% and 105% for AD (RR: 1.39; 95% CI: 1.00, 1.94) and dementia (RR: 2.05; 95% CI: 1.06, 3.98), respectively. Dose-response analysis indicated a 4 g/day increment of saturated fat intake was related to 15% higher risk of AD (RR: 1.15; 95% CI: 1.01, 1.31). However, there was no significant association found between dietary intake of total, monounsaturated, polyunsaturated fat and AD or dementia risk.
Conclusions: This meta-analysis provides significant evidence of positive association between higher saturated fat intake and AD and dementia risk.
Vitamin C, Aging and Alzheimer's Disease
Abstract
Accumulating evidence in mice models of accelerated senescence indicates a rescuing role of ascorbic acid in premature aging. Supplementation of ascorbic acid appeared to halt cell growth, oxidative stress, telomere attrition, disorganization of chromatin, and excessive secretion of inflammatory factors, and extend lifespan. Interestingly, ascorbic acid (AA) was also found to positively modulate inflamm-aging and immunosenescence, two hallmarks of biological aging. Moreover, ascorbic acid has been shown to epigenetically regulate genome integrity and stability, indicating a key role of targeted nutrition in healthy aging. Growing in vivo evidence supports the role of ascorbic acid in ameliorating factors linked to Alzheimer's disease (AD) pathogenesis, although evidence in humans yielded equivocal results. The neuroprotective role of ascorbic acid not only relies on the general free radical trapping, but also on the suppression of pro-inflammatory genes, mitigating neuroinflammation, on the chelation of iron, copper, and zinc, and on the suppression of amyloid-beta peptide (Aβ) fibrillogenesis. Epidemiological evidence linking diet, one of the most important modifiable lifestyle factors, and risk of Alzheimer's disease is rapidly increasing. Thus, dietary interventions, as a way to epigenetically modulate the human genome, may play a role in the prevention of AD. The present review is aimed at providing an up to date overview of the main biological mechanisms that are associated with ascorbic acid supplementation/bioavailability in the process of aging and Alzheimer's disease. In addition, we will address new fields of research and future directions.
Keywords: Alzheimer’s disease; aging process; ascorbic acid.
Depression, Stress, & Inflammation
Health relevance of the modification of low grade inflammation in ageing (inflammageing) and the role of nutrition
Abstract
Ageing of the global population has become a public health concern with an important socio-economic dimension. Ageing is characterized by an increase in the concentration of inflammatory markers in the bloodstream, a phenomenon that has been termed "inflammageing". The inflammatory response is beneficial as an acute, transient reaction to harmful conditions, facilitating the defense, repair, turnover and adaptation of many tissues. However, chronic and low grade inflammation is likely to be detrimental for many tissues and for normal functions. We provide an overview of low grade inflammation (LGI) and determine the potential drivers and the effects of the "inflamed" phenotype observed in the elderly. We discuss the role of gut microbiota and immune system crosstalk and the gut-brain axis. Then, we focus on major health complications associated with LGI in the elderly, including mental health and wellbeing, metabolic abnormalities and infections. Finally, we discuss the possibility of manipulating LGI in the elderly by nutritional interventions. We provide an overview of the evidence that exists in the elderly for omega-3 fatty acid, probiotic, prebiotic, antioxidant and polyphenol interventions as a means to influence LGI. We conclude that slowing, controlling or reversing LGI is likely to be an important way to prevent, or reduce the severity of, age-related functional decline and the onset of conditions affecting health and well-being; that there is evidence to support specific dietary interventions as a strategy to control LGI; and that a continued research focus on this field is warranted.
Nutrition, inflammation and liver-spleen axis
Abstract
Chronic low-grade systemic inflammation represents a mechanism common to many diseases linked to atherosclerosis-related pathways. There is a growing body of evidence indicating that the combination of food quantity and quality along with genetic susceptibility are able to induce the aberrant activation of innate immune signalling, which initially contributes to chronic low-grade inflammation. Liver represents the central player to inflammatory response. Dietary/metabolic factors contribute to the pathogenesis of Non-alcoholic Fatty Liver Disease (NAFLD), the main causes of liver disease in the Western world. Enlargement of the spleen, central organ in regulating the inflammation-related immune response, is commonly seen in patients with of NAFLD, depicting the so called "liver-spleen axis." The aim of this review was to provide an at-a-glance overview of the possible bi-directional mechanisms linking nutrition and inflammation, particularly pinpointing the inflammatory effects stemmed by nutrition on "liver-spleen axis." In particular, the role of unhealthy diet, healthy dietary patterns, such as the Mediterranean diet style, dietary vitamins and micronutrients, such as vitamin D or Magnesium, and Glucagon-Like Peptide-1, a well-known incretin released in response to meal intake, will be discussed. The highly variability of the inflammatory response highlights the role of expert nutritionists in refining methodologies apt to assess nutritional epidemiology and to apply appropriate dietary intervention to counteract diet-induced inflammation mechanisms.
Depressed gut? The microbiota-diet-inflammation trialogue in depression
Abstract
Purpose of review: According to the WHO reports, around 350 million people worldwide suffer from depression. Despite its high prevalence, the complex interaction of multiple mechanisms underlying depression still needs to be elucidated.
Recent findings: Over the course of the last few years, several neurobiological alterations have been linked to the development and maintenance of depression. One basic process that seems to link many of these findings is inflammation. Chronic inflammation has been associated with both biological factors such as excessive neurotransmitter concentrations as well as psychological processes such as adult stress reactivity and a history of childhood trauma. As a balanced microbial community, modulated by diet, is a key regulator of the host physiology, it seems likely that gut microbiota plays a role in depression.
Summary: The review summarizes the existent literature on this emerging research field and provides a comprehensive overview of the multifaceted links between the microbiota, diet, and depression. Several pathways linking early life trauma, pharmacological treatment effects, and nutrition to the microbiome in depression are described aiming to foster the psychotherapeutic treatment of depressed patients by interventions targeting the microbiota.
Cognitive Frailty and Its Association with Nutrition and Depression in Community-Dwelling Older People
Abstract
Background: Cognitive frailty is a condition where physical frailty and mild cognitive impairment (MCI) co-exist. It is associated with increased risk of dementia and dependency. Previous studies reported that malnutrition and depression are associated with physical frailty and MCI; however, their relationships with cognitive frailty remained to be explored. The aims of this study were to examine the association of nutrition and depression with cognitive frailty, in comparison to having physical frailty or MCI alone.
Methods: This study employed a cross-sectional design. Data collection was conducted in the community settings on the older people without dementia. Dependent variables were cognitive frailty, physical frailty, and MCI. The independent variables were depression and nutrition. Multi-nominal regression was employed to examine the relationships between the dependent and independent variables. The associations were adjusted by four known co-variates, including age, gender, education and APOE ε4 carrier status.
Results: A total of 185 participants were recruited from four community centres and one elderly hostel and completed the data collection. Approximately 44.9% of the older people with physical frailty and 82.5% of elderly with MCI belonged to cognitive frailty. Multi-nominal regression models showed that depression is positively associated with cognitive frailty and with physical frailty, but not associated with solely MCI. Nutrition is negatively associated with cognitive frailty, but not associated with physical frailty or MCI alone.
Conclusion: Cognitive frailty is associated with malnutrition and depression. Therapeutic interventions managing depression and malnutrition may focus the older people with cognitive frailty to improve efficacy and cost-effectiveness.
Abstract
Background: Major depressive disorder is a common, chronic condition that imposes a substantial burden of disability globally. As current treatments are estimated to address only one-third of the disease burden of depressive disorders, there is a need for new approaches to prevent depression or to delay its progression. While in its early stages, converging evidence from laboratory, population research, and clinical trials now suggests that dietary patterns and specific dietary factors may influence the risk for depression. However, largely as a result of the recency of the nutritional psychiatry field, there are currently no dietary recommendations for depression.
Aim: The aim of this paper is to provide a set of practical dietary recommendations for the prevention of depression, based on the best available current evidence, in order to inform public health and clinical recommendations.
Results: Five key dietary recommendations for the prevention of depression emerged from current published evidence. These comprise: (1) follow 'traditional' dietary patterns, such as the Mediterranean, Norwegian, or Japanese diet; (2) increase consumption of fruits, vegetables, legumes, wholegrain cereals, nuts, and seeds; (3) include a high consumption of foods rich in omega-3 polyunsaturated fatty acids; (4) replace unhealthy foods with wholesome nutritious foods; (5) limit your intake of processed-foods, 'fast' foods, commercial bakery goods, and sweets.
Conclusion: Although there are a number of gaps in the scientific literature to date, existing evidence suggests that a combination of healthful dietary practices may reduce the risk of developing depression. It is imperative to remain mindful of any protective effects that are likely to come from the cumulative and synergic effect of nutrients that comprise the whole-diet, rather than from the effects of individual nutrients or single foods. As the body of evidence grows from controlled intervention studies on dietary patterns and depression, these recommendations should be modified accordingly.
The Impact of Nutrition and Intestinal Microbiome on Elderly Depression-A Systematic Review
Abstract
The aim of this review is to systematically review the evidence whether proper nutrition has a positive impact on the prevention or decline of depressive symptoms among elderly people. In addition, possible connections between nutrition, microbiome, and serotonin molecules and its tryptophan precursor are discussed. The methodology follows the PRISMA guidelines, including the PRISMA flow chart. The authors systematically reviewed peer-review, English-written articles published in Web of Science and PubMed between 2013 and 2018. The findings of six original articles, detected on the set inclusion and exclusion criteria, indicate that there is an association between nutrition and depressive symptoms in the target group, i.e., that proper nutrition has a positive impact on the prevention or reduction of depressive symptoms among elderly people. The findings also reveal that there is a considerable correlation between the intakes of vitamin B and a decrease in the prevalence of depressive symptoms. Furthermore, sufficient nutrient intake of tryptophan appears to be an important factor in terms of nutrition and serotonin levels in the body. The authors consider it important to explore associations between the overall dietary intake and depression since diets are not consumed as individual nutrients. Returning to preventive approaches seems to be a rational way to promote the mental health of seniors. Future studies thus need to include interdisciplinary collaboration: from a good diagnosis of the disease by a psychiatrist, through an analysis of the need for nutrient metabolism by a biochemist to the development of a nutritional plan by a nutritional therapist. The limitations of this review consist in a relatively small number of the studies on this topic, including just few randomized controlled trials, which are a guarantee of efficacy and objectivity in comparison with cross-sectional studies.
Evaluation of the physical activity level, nutrition quality, and depression in patients with metabolic syndrome
Abstract
Metabolic syndrome (MetS) is a complex problem that contains risk factors related with obesity, cardiovascular diseases, and type-II diabetes. The incidence of MetS is increasing every year throughout the world.
The aim of this study was to evaluate and compare physical activity levels, nutrition quality, and depression status of the individuals who are diagnosed with and without MetS.
International Physical Activity Questionnaire (IPAQ), Mediterranean Diet Adherence Screener (MEDAS), Beck Depression Inventory (BDI) was used. In addition, biochemical analysis and anthropometric measurements were also taken.
According to IPAQ, 81.1% of the MetS group is inactive, 6.8% is active, and 5.1% is highly active, whereas 22.3% of the non-MetS group is inactive, 46.2% is active, and 31.5% is highly active. MEDAS was found to be lower in the MetS group. BDI levels were also determined high in the MetS group.
Sedentary lifestyle, depression, and unhealthy nutrition habits are among the significant factors for the development of MetS. The knowledge levels of the people should be increased by developing national physical activity and nutrition guidelines.
Keywords: depression, metabolic syndrome, nutrition, physical activity, public health
Serum lipid levels in depression and suicidality: The Korea National Health and Nutrition Examination Survey (KNHANES) 2014
Abstract
Background
The level of serum lipids has been reported to be associated with depression and suicidality, but the exact relationship between these factors remains controversial. The aim of this study was to investigate the association between lipid levels and depression with suicidality in large sample.
Methods
We examined the association between serum lipid levels and the existence of mild depression measured using Patient Health Questionnaire 9 (PHQ-9) in a national sample of Korean. The data of 2055 men and 2894 women who participated in the 6th Korea National Health and Nutrition Examination Survey (KNHNES VI) were used. The serum concentration of high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), triglyceride, and total cholesterol were dichotomized and complex samples logistic regression was employed in the analysis.
Results
There was a significant association between high level of HDL-C (≥40 mg/dl) and depression in adult men, and between high level of triglyceride (≥150 mg/dl) and depression in adult women. In middle-aged adults 45–64 year), increased level of depression and suicidality was related to high level of triglyceride, respectively. (depression, OR=2.20 (95% CI 1.26–3.85); suicidality, OR=3.66 (95% CI 1.41–9.51). Furthermore, we found that the increased number of abnormal lipids level was significantly associated with the increased prevalence of depression in women (OR =1.34, 95% CI =1.12–1.60) and in middle-aged adults (OR=1.43, 95% CI =1.12–1.82).
Limitations
As this study had a cross-sectional design, it was hard to investigate causation between lipid levels and depression, and the assessment of suicidality needs more validation.
Conclusion
Our findings support a significant association between the high level of HDL-C, triglyceride and depression in large sample data. Triglyceride was highly associated with suicidality in younger and middle-aged adults, but not in elderly adults. Further assessment could delineate relationship between serum lipid levels and depression with suicidality in other ethnic groups.
An association of health behaviors with depression and metabolic risks: Data from 2007 to 2014 U.S. National Health and Nutrition Examination Survey
Abstract
Background
Both depression and
metabolic syndrome
(MetS) confer an increased risk of developing type 2 diabetes (T2D) and cardiovascular disease. Accumulating evidence suggests healthy behaviors are crucial to maintain, improve and manage chronical disease and mental health; and
unhealthy diet
and sedentary behavior were found two major risk factors of MetS. The objective of this study was to investigate whether health behaviors (alcohol consumption, smoking, diet and recreational physical activity) are associated with depression and metabolic syndrome simultaneously.
Methods
This study included 1300 participants aged 20 years and over who had answered mental health-depression screener questions (PHQ-9) and finished examinations and laboratory tests related to five risk factors of MetS during the U.S. National Health and
Nutrition
Examination Survey (NHANES) 2007–2014. A set of series of weighted
logistic regression
models were used to investigate the aforementioned relationship.
Results
The prevalence of depression among U.S. adults is 15.08%. The two most often reported depression symptoms were “Trouble sleeping or sleeping too much” and “Feeling tired or having little energy”, with rates of14.68% and 13.09%, respectively. Participants who engaged in only light physical activity were more likely to have been identified as experiencing depression and MetS than those who engaged in vigorous physical activity with odd ratios 3.18 (95% CI: 1.59, 6.37) and 3.50 (95%CI: 2.17, 5.63), respectively. Individuals in the study having poor diets were more likely to suffer from depression than those eating good diets (OR=2.17, 95%CI: 1.47, 3.22).
Conclusion
Physical activity is strongly and inversely associated with depression and MetS. Diet is significantly associated with depression rather than MetS in this study.
Nutrition and depression: Summary of findings from the EU‐funded MooDFOOD depression prevention randomised controlled trial and a critical review of the literature
Abstract
This paper discusses the emerging field of nutritional psychology and provides an update on the now completed EU‐funded MooDFOOD depression prevention randomised controlled trial that assessed the effects of two nutrition‐based interventions for the prevention of depression in overweight or obese adults with at least mild symptoms of depression. We first outline the problem of major depression, the most common form of psychopathology and the largest contributor to global disability, and then give an overview of the connection between nutrition and depression; separating the evidence according to prevention and treatment of depression. The extant literature is reviewed, and we examine the implications for both prevention and treatment. Questions are posed for further research in this emerging and important area.
Nutrition and behavioral health disorders: depression and anxiety
Abstract
Suboptimal nutrition has been implicated in the underlying pathology of behavioral health disorders and may impede treatment and recovery. Thus, optimizing nutritional status should be a treatment for these disorders and is likely important for prevention. The purpose of this narrative review is to describe the global burden and features of depression and anxiety, and summarize recent evidence regarding the role of diet and nutrition in the prevention and management of depression and anxiety. Current evidence suggests that healthy eating patterns that meet food-based dietary recommendations and nutrient requirements may assist in the prevention and treatment of depression and anxiety. Randomized controlled trials are needed to better understand how diet and nutrition-related biological mechanisms affect behavioral health disorders, to assist with the development of effective evidence-based nutrition interventions, to reduce the impact of these disorders, and promote well-being for affected individuals.
Ultra-processed food consumption and the incidence of depression in a Mediterranean cohort: the SUN Project
Abstract
Purpose: A growing body of evidence shows that consumption of ultra-processed foods (UPF) is associated with a higher risk of cardiometabolic diseases, which, in turn, have been linked to depression. This suggests that UPF might also be associated with depression, which is among the global leading causes of disability and disease. We prospectively evaluated the relationship between UPF consumption and the risk of depression in a Mediterranean cohort.
Methods: We included 14,907 Spanish university graduates [mean (SD) age: 36.7 year (11.7)] initially free of depression who were followed up for a median of 10.3 years. Consumption of UPF (industrial formulations made mostly or entirely from substances derived from foods and additives, with little, if any, intact food), as defined by the NOVA food classification system, was assessed at baseline through a validated semi-quantitative 136-item food-frequency questionnaire. Participants were classified as incident cases of depression if they reported a medical diagnosis of depression or the habitual use of antidepressant medication in at least one of the follow-up assessments conducted after the first 2 years of follow-up. Cox regression models were used to assess the relationship between UPF consumption and depression incidence.
Results: A total of 774 incident cases of depression were identified during follow-up. Participants in the highest quartile of UPF consumption had a higher risk of developing depression [HR (95% CI) 1.33 (1.07-1.64); p trend = 0.004] than those in the lowest quartile after adjusting for potential confounders.
Conclusions: In a prospective cohort of Spanish university graduates, we found a positive association between UPF consumption and the risk of depression that was strongest among participants with low levels of physical activity.
Keywords: Depression; Food processing; Prospective study; SUN cohort; Ultra-processed food.
Fast-food and commercial baked goods consumption and the risk of depression
Abstract
Objective: Whereas the relationship between some components of diet, such as n-3 fatty acids and B-vitamins, and depression risk has been extensively studied, the role of fast-food or processed pastries consumption has received little attention.
Design: Consumption of fast food (hamburgers, sausages, pizza) and processed pastries (muffins, doughnuts, croissants) was assessed at baseline through a validated semi-quantitative FFQ. Participants were classified as incident cases of depression if they reported a physician diagnosis of depression or the use of antidepressant medication in at least one of the follow-up questionnaires. Cox regression models were fit to assess the relationship between consumption of fast food and commercial baked goods and the incidence of depression.
Setting: The SUN (Seguimiento Universidad de Navarra - University of Navarra Follow-up) Project, Spain.
Subjects: Participants (n 8964) from a Spanish cohort.
Results: After a median follow-up of 6·2 years, 493 cases of depression were reported. A higher risk of depression was associated with consumption of fast food (fifth (Q5) v. first quintile (Q1): hazard ratio (HR) = 1·36; 95 % CI 1·02, 1·81; P trend = 0·003). The results did not change after adjustment for the consumption of other food items. No linear relationship was found between the consumption of commercial baked goods and depression. Participants belonging to consumption quintiles Q2-Q5 showed an increased risk of depression compared with those belonging to the lowest level of consumption (Q1; HR = 1·38; 95 % CI 1·06, 1·80).
Conclusions: Fast-food and commercial baked goods consumption may have a detrimental effect on depression risk.
The role of vitamin D in the prevention of late-life depression
Abstract
Background: In this article, we review current evidence regarding potential benefits of vitamin D for improving mood and reducing depression risk in older adults. We summarize gaps in knowledge and describe future efforts that may clarify the role of vitamin D in late-life depression prevention.
Methods: MEDLINE and PsychINFO databases were searched for all articles on vitamin D and mood that had been published up to and including May 2015. Observational studies and randomized trials with 50 or more participants were included. We excluded studies that involved only younger adults and/or exclusively involved persons with current depression.
Results: Twenty observational (cross-sectional and prospective) studies and 10 randomized trials (nine were randomized placebo-controlled trials [RCTs]; one was a randomized blinded comparison trial) were reviewed. Inverse associations of vitamin D blood level or vitamin D intake with depression were found in 13 observational studies; three identified prospective relations. Results from all but one of the RCTs showed no statistically significant differences in depression outcomes between vitamin D and placebo groups.
Limitations: Observational studies were mostly cross-sectional and frequently lacked adequate control of confounding. RCTs often featured low treatment doses, suboptimal post-intervention changes in biochemical levels of vitamin D, and/or short trial durations.
Conclusion: Vitamin D level-mood associations were observed in most, but not all, observational studies; results indicated that vitamin D deficiency may be a risk factor for late-life depression. However, additional data from well-designed RCTs are required to determine the impact of vitamin D in late-life depression prevention.
Efficacy of fasting and calorie restriction (FCR) on mood and depression among ageing men
Abstract
Objective: An intervention study on the FCR (Fasting and Calorie Restriction) dietary regime was carried out to determine its efficacy in improving mood states and depression status among ageing men.
Subjects: A total of 32 healthy males (Mean±SD), aged 59.7±6.3 years, with a BMI of 26.7±2.2 kg/m2 were recruited to the study.
Method: Participants were randomized to either the FCR group (and were instructed to follow a calorie restricted dietary regime with intermittent fasting) or to the control group (in which individuals were asked to maintain their current lifestyle), for a 3 month period. Mood was assessed using the Profile of Mood States and depression was assessed using Beck Depression Inventory-II and Geriatric Depression Scale-15 at baseline, week 6 and week 12 of the intervention.
Results: A total of 31 subjects completed the study (n=16, FCR and n=15, control). Significant decreases in tension, anger, confusion and total mood disturbance and improvements in vigor were observed in participants in the FCR group compared to the control group (p<0.05). No significant changes in mean depression scores were observed. Weight, BMI and percent body fat were reduced by 3.8%, 3.7% and 5.7% respectively in the FCR group.
Conclusions: Our findings show that a FCR dietary regime is effective in improving mood states and nutritional status among ageing men.
Fruit and vegetable consumption and the risk of depression: A meta-analysis
Abstract
Objective: Epidemiologic investigations evaluating the association of fruit and vegetable consumption with depression risk have yielded controversial results. Therefore, a meta-analysis was carried out to qualitatively summarize the evidence regarding association of fruit and vegetable intake with risk of depression in the general population.
Methods: PubMed, Embase, and Web of Knowledge were searched for relevant articles published up to June 2015. To evaluate the association of fruit and vegetable intake with depression risk, combined relative risks were calculated with the fixed or random effects model. Meta-regression was conducted to explore potential sources of heterogeneity. Publication bias was estimated by the Egger's test and the funnel plot.
Results: Ten studies involving 227 852 participants for fruit intake and eight studies involving 218 699 participants for vegetable intake were finally included in this study. The combined relative risk (95% confidence interval) of depression for the highest versus lowest category of fruit and vegetable intake was 0.86 (0.81, 0.91; P < 0.01) and 0.89 (0.83, 0.94; P < 0.01), respectively. In subgroup analyses stratified by study design, the inverse association of fruit (0.83 [0.77, 0.91; P = 0.006]) and vegetable (0.88 [0.79, 0.96; P = 0.007]) intake with risk of depression was also observed in the cohort study.
Conclusions: This meta-analysis indicated that fruit and vegetable consumption might be inversely associated with the risk of depression, respectively.
Keywords: Depression; Fruit; Meta-analysis; Vegetable.
Possible relation between consumption of different food groups and depression
Abstract
Background: Diverse studies have investigated the relationship between diet and depression. In fact some cross-sectional studies suggested that a healthy diet reduced the risk for depression. The main objective of this study was to assess the relationship of consumption of different food groups with depression. The food groups were selected based on their content of substances that were precursors to neurotransmitters (tryptophan or inositol) or their effect on oxidative stress.
Methods: This observational retrospective study compared the diets of individuals who were with depressive symptoms (Beck Depression Inventory Questionnaire [BDI] ≥ 10; 53 women, 23 men, age 38+/- 11) and with no depressive levels (BDI < 10; 33 women, 23 men, age 41+/- 13). Dietary data were collected from a questionnaire that asked about consumption of legumes, nuts, whole-grain foods, fruits and vegetables, chocolate, and sweet foods and refined sugars.
Results: Depressed individuals consumed significantly lower amounts of legumes, fruits, and vegetables, but higher amounts of sweets and refined sugars (p < 0.05 for all comparisons). After statistical adjustment for age and sex, the consumption of no legumes (adjusted odds ratio [aOR] = 2.60, 95% confidence interval [CI] = 1.19-5.67), low consumption of fruits and vegetables (aOR = 2.69, 95% CI = 1.18-6.13), and high consumption of sweet foods and refined sugars (aOR = 1.91, 95% CI = 1.23-2.99) were significantly associated with depression. The two groups had no significant differences in the consumption of chocolate.
Discussion: The results indicate significant relationships of the consumption of certain foods with depression, although the study design precludes any conclusions regarding causality. Further studies are necessary to determine the causal relationships of the consumption of specific foods with depression, and of depression with the consumption of specific foods.
Conclusion: In spite of the limitations, we find that individuals without depression consumed more legumes, fruits, and vegetables, but fewer sweets and pastries than those with depression.
Keywords: Depression; Food; Oxidative stress; Precursors to neurotransmitters.
Diet quality and depression risk: A systematic review and dose-response meta-analysis of prospective studies
Abstract
Background: It has been claimed that the quality of a diet is associated with the incidence of depressive disorders. We sought to investigate the evidence for this claim.
Methods: Systematic searches were performed up to March 6th, 2017 in order to identify prospective cohort studies that reported on exposure to dietary patterns or food groups and the incidence of depression/depressive symptoms. Data from 24 independent cohorts (totalling 1,959,217 person-years) were pooled in random-effects meta-analyses.
Results: Adherence to a high-quality diet, regardless of type (i.e., healthy/prudent or Mediterranean), was associated with a lower risk of depressive symptoms over time (odds ratios ranged 0.64-0.78 in a linear dose-response fashion [P < 0.01]). A relatively low dietary inflammatory index was also associated with a somewhat lower incidence of depressive symptom (odds ratio = 0.81), although not in a dose-response fashion. Similar associations were found for the consumption of fish and vegetables (odds ratios 0.86 and 0.82 respectively) but not for other high quality food groups (e.g., fruit). Studies that controlled for depression severity at baseline or that used a formal diagnosis as outcome did not yield statistically significant findings. Adherence to low quality diets and food groups was not associated with higher depression incidence.
Limitations: Our ability to detect confounders was only limited.
Conclusion: There is evidence that a higher quality of a diet is associated with a lower risk for the onset of depressive symptoms, but not all available results are consistent with the hypothesis that diet influences depression risk. Prospective studies that control for relevant confounders such as obesity incidence and randomized controlled prevention trials are needed to increase the validity of findings in this field.
Dietary recommendations for the prevention of depression
Abstract
Background: Major depressive disorder is a common, chronic condition that imposes a substantial burden of disability globally. As current treatments are estimated to address only one-third of the disease burden of depressive disorders, there is a need for new approaches to prevent depression or to delay its progression. While in its early stages, converging evidence from laboratory, population research, and clinical trials now suggests that dietary patterns and specific dietary factors may influence the risk for depression. However, largely as a result of the recency of the nutritional psychiatry field, there are currently no dietary recommendations for depression.
Aim: The aim of this paper is to provide a set of practical dietary recommendations for the prevention of depression, based on the best available current evidence, in order to inform public health and clinical recommendations.
Results: Five key dietary recommendations for the prevention of depression emerged from current published evidence. These comprise: (1) follow 'traditional' dietary patterns, such as the Mediterranean, Norwegian, or Japanese diet; (2) increase consumption of fruits, vegetables, legumes, wholegrain cereals, nuts, and seeds; (3) include a high consumption of foods rich in omega-3 polyunsaturated fatty acids; (4) replace unhealthy foods with wholesome nutritious foods; (5) limit your intake of processed-foods, 'fast' foods, commercial bakery goods, and sweets.
Conclusion: Although there are a number of gaps in the scientific literature to date, existing evidence suggests that a combination of healthful dietary practices may reduce the risk of developing depression. It is imperative to remain mindful of any protective effects that are likely to come from the cumulative and synergic effect of nutrients that comprise the whole-diet, rather than from the effects of individual nutrients or single foods. As the body of evidence grows from controlled intervention studies on dietary patterns and depression, these recommendations should be modified accordingly.
Keywords: Depression; Diet; Mental disorder; Prevention.
Omega-3 long-chain polyunsaturated fatty acids supplementation on inflammatory biomakers: a systematic review of randomised clinical trials
Abstract
Inflammation is part of the normal host response to infection and injury. Eicosanoids, cytokines, chemokines, adhesion molecules and other inflammatory molecules are frequently produced during this process. Numerous studies in humans have documented the inflammation-limiting properties of omega-3 fatty acids, but only a few have been randomised clinical trials. The aim of this study was to perform a systematic search of randomised clinical trials on omega-3 fatty acids and inflammatory biomarkers in all subjects including healthy and ill persons up to February 2011 using PubMed and LILACS databases, defined by a specific equation using MeSH terms and limited to randomised clinical trials; there was no any a priori decision to include some diseases and not others. The quality of each publication was validated by using the JADAD scale and the CONSORT checklist. Inflammatory biomarkers were considered as primary outcomes. Twenty-six publications of the last 10 years were selected. Studies included healthy subjects and patients with cardiovascular disease and other chronic and acute diseases; all reported the number of subjects, type of study, type and doses of omega-3 fatty acids, main outcomes and major inflammatory biomarkers. Dietary omega-3 fatty acids are associated with plasma biomarker levels, reflecting lower levels of inflammation and endothelial activation in cardiovascular disease and other chronic and acute diseases, including chronic renal disease, sepsis and acute pancreatitis. However, further research is required before definitive recommendations can be made about the routine use of omega-3 fatty acids in critically ill patients or with neurodegenerative or chronic renal disease.
Vitamin D and inflammation
Abstract
Several studies found an inverse relationship between 25-hydroxyvitamin D [25(OH)D] and markers of inflammation. A controversy exists as to whether vitamin D lowers inflammation or whether inflammation lowers 25(OH)D concentrations. Certainly 25(OH)D concentrations fall after major surgery. However, is this due to inflammation lowering 25(OH)D or is 25(OH)D being metabolically cleared by the body to quell inflammation. We searched the literature and found 39 randomized controlled trials (RCT) of vitamin D and markers of inflammation. Seventeen found significantly reduced inflammatory markers, 19 did not, one was mixed and one showed adverse results. With few exceptions, studies in normal subjects, obesity, type 2 diabetics, and stable cardiovascular disease did not find significant beneficial effects. However, we found that 6 out of 7 RCTS of vitamin D3 in highly inflammatory conditions (acute infantile congestive heart failure, multiple sclerosis, inflammatory bowel disease, cystic fibrosis, SLE, active TB and evolving myocardial infarction) found significant reductions. We found baseline and final 25(OH)D predicted RCTs with significant reduction in inflammatory markers. Vitamin D tends to modestly lower markers of inflammation in highly inflammatory conditions, when baseline 25(OH)D levels were low and when achieved 25(OH)D levels were higher. Future inquiries should: recruit subjects with low baseline 25(OH)D levels, subjects with elevated markers of inflammation, subjects with inflammatory conditions, achieve adequate final 25(OH)D levels, and use physiological doses of vitamin D. We attempted to identify all extant randomized controlled trials (RCTs) of vitamin D that used inflammatory markers as primary or secondary endpoints.
Nutrition and diet in inflammatory bowel disease
Abstract
Purpose of review
Diet is known to have a major role in the expression of inflammatory bowel disease (IBD). The role of dietary interventions and enteral nutrition in the management of IBD remains unelucidated. This study was to review the current evidence for dietary risk factors for the development of IBD and the efficacies of dietary and enteral interventions.
Recent findings
High dietary intakes of total fats, polyunsaturated fatty acids, omega-6 fatty acids, and meat are associated with an increased risk of Crohn's disease and ulcerative colitis. Further prospective studies are required to confirm these observations. Among various dietary interventions, none has shown striking efficacy. Meta-analyses have shown enteral nutrition to be inferior to corticosteroids in adults with active Crohn's disease. However, in children, a meta-analysis has shown no significant difference in the remission rates between enteral nutrition and corticosteroid therapy. Although the evidence level is not striking, enteral nutrition may be useful for maintaining remission in patients with quiescent Crohn's disease.
Summary
Dietary risk factors for IBD and the therapeutic benefit of dietary and enteral interventions need to be confirmed by further well designed studies in large cohorts of patients.
Effect of ω-3 polyunsaturated fatty acid-supplemented parenteral nutrition on inflammatory and immune function in postoperative patients with gastrointestinal malignancy
Abstract
Background
: There are no consensus regarding the efficacy of omega-3polyunsaturated fatty acids (PUFAs) on inflammatory and immune function in postoperative patients with gastrointestinal malignancy.
Methods:
The literatures published randomized control trials (RCT) were searched in PubMed, Embase, Scopus, Cochrane Library, CNKI, Weipu, and Wanfang Databases. The immune efficacy outcomes of ω-3 polyunsaturated fatty acid-supplemented parenteral nutrition in patients with gastrointestinal malignancy were compared.
Results:
Sixteen RCTs involving 1008 patients (506 in the omega-3 group, 502 in the control group) were enrolled into the analysis. The results of meta-analysis: the cell immunity: The proportions of CD3+, CD4+, CD4+/CD8+ in the omega-3 group were significantly higher than those in the control group (CD3+: WMD = 4.48; 95% CI, 3.34–5.62; P < .00001; I2 = 0%; CD4+: WMD = 5.55; 95% CI, 4.75–6.34; P < .00001; I2 = 0%; CD4+/CD8+: WMD = .28; 95% CI, 0.13–0.44; P = .0004; I2 = 81%). In the humoral immunity: The levels of IgA, IgM and IgG in the omega-3 group were significantly higher than those in the control group (IgA: WMD = 0.31; 95% CI, 0.25–0.37; P < .00001; I2 = 0%; IgM: WMD = 0.12; 95% CI, 0.06–1.81; P < .00001; I2 = 0%; IgG: WMD = 1.19; 95% CI, 0.80–1.58; P < .00001; I2 = 0%). The count of lymphocyte in the omega-3 group was significantly higher than that in the control group (WMD = 0.22; 95% CI, 0.12–0.33; P < .0001; I2 = 40%). In the postoperative inflammatory cytokine: The levels of interleukin-6, tumor necrosis factor (TNF)-α and C-reactive protein in the omega-3 group were significantly lower than those in the control group (IL-6: WMD = −3.09; 95% CI, −3.91 to 2.27; P < .00001; I2 = 45%; TNF-α: WMD = −1.65; 95% CI, −2.05 to 1.25; P < .00001; I2 = 28%; CRP: WMD = −4.28; 95% CI, −5.26 to 3.30; P < .00001; I2 = 37%). The rate of postoperative infective complications in the omega-3 group was significantly lower than that in the control group (OR = 0.36; 95% CI, 0.20–0.66; P = .0008; I2 = 0%).
Conclusion:
This meta-kanalysis confirmed that early intervention with Omega -3 fatty acid emulsion in gastrointestinal cancer can not only improve the postoperative indicators of immune function, reduce inflammatory reaction, and improve the postoperative curative effect but also improve the immune suppression induced by conventional PN or tumor. Therefore, postoperative patients with gastrointestinal cancer should add omega-3 unsaturated fatty acids in their PN formula. Further high-quality RCTs are needed to verify its efficacy.
Keywords: gastrointestinal malignancy, meta-analysis, omega-3 polyunsaturated fatty acid, parenteral nutrition
Nutritional support and the role of the stress response in critically ill children
Purpose of review
Nutrition impacts outcome in critically ill children. Based on evolving neuro-endocrine, immunologic and metabolic alterations, three different phases can be proposed during the course of illness. The different phases each demand for tailored macronutrient intakes in critically ill children.
Recent findings
Early enteral nutrition is associated with decreased morbidity and mortality, but several misconceptions concerning the provision of enteral nutrition prevent adequate intake. Parenteral nutrition in critically ill children is associated with potential disadvantages, as nosocomial infections, but evidence on the effect on clinical outcome is lacking. Nutrient restriction early during critical illness might be beneficial for short and long-term outcomes by decreasing the incidence of side-effects and possibly by amplifying the acute catabolic stress response and stimulating autophagy and muscle integrity. Higher caloric and protein intake via the enteral route are associated with higher 60-day survival, asking for a more aggressive feeding approach in subsequent phases.Summary
Understanding the stress response to critical illness and its phases is essential for nutritional recommendations in critically ill children. Although parenteral nutrient restriction during the acute phase might be beneficial, inclining requirements ask for a more aggressive approach during the stable and recovery phase to enable recovery, growth and catch-up growth.
The Emerging Field of Nutritional Mental Health: Inflammation, the Microbiome, Oxidative Stress, and Mitochondrial Function
Abstract
We live in a transformational moment for understanding the etiology of mental disorders. The previous leap in understanding occurred 60 years ago, which led us to incorporate psychopharmacology into our curricula to address the chemical basis of neurotransmitter function, especially as explained through the then-popular catecholamine hypothesis. The current revolution is broader, consisting of the rapidly accumulating knowledge of how inflammation, microbiome imbalance (gut dysbiosis), oxidative stress, and impaired mitochondrial output affect brain function. Suitable interventions for fighting inflammation, restoring normal gut function, reducing oxidative stress, and improving mitochondrial metabolism incorporate lifestyle variables, including nutrients and probiotics. This article invites readers to stay abreast of this emerging model of the biological basis of mental illness, given that it has particular relevance for those readers interested in alleviating the suffering of individuals with mental disorders. This overview describes the basis for a new field in mental health: nutritional psychiatry/psychology.
Stress ulcer prophylaxis in intensive care unit patients receiving enteral nutrition: a systematic review and meta-analysis
Abstract
Background
Pharmacologic stress ulcer prophylaxis (SUP) is recommended in critically ill patients with high risk of stress-related gastrointestinal (GI) bleeding. However, as to patients receiving enteral feeding, the preventive effect of SUP is not well-known. Therefore, we performed a meta-analysis of randomized controlled trials (RCTs) to evaluate the effect of pharmacologic SUP in enterally fed patients on stress-related GI bleeding and other clinical outcomes.
Methods
We searched PubMed, Embase, and the Cochrane database from inception through 30 Sep 2017. Eligible trials were RCTs comparing pharmacologic SUP to either placebo or no prophylaxis in enterally fed patients in the ICU. Results were expressed as risk ratio (RR) and mean difference (MD) with accompanying 95% confidence interval (CI). Heterogeneity, subgroup analysis, sensitivity analysis and publication bias were explored.
Results
Seven studies (n = 889 patients) were included. There was no statistically significant difference in GI bleeding (RR 0.80; 95% CI, 0.49 to 1.31, p = 0.37) between groups. This finding was confirmed by further subgroup analyses and sensitivity analysis. In addition, SUP had no effect on overall mortality (RR 1.21; 95% CI, 0.94 to 1.56, p = 0.14), Clostridium difficile infection (RR 0.89; 95% CI, 0.25 to 3.19, p = 0.86), length of stay in the ICU (MD 0.04 days; 95% CI, −0.79 to 0.87, p = 0.92), duration of mechanical ventilation (MD −0.38 days; 95% CI, −1.48 to 0.72, p = 0.50), but was associated with an increased risk of hospital-acquired pneumonia (RR 1.53; 95% CI, 1.04 to 2.27; p = 0.03).
Conclusions
Our results suggested that in patients receiving enteral feeding, pharmacologic SUP is not beneficial and combined interventions may even increase the risk of nosocomial pneumonia.
High dietary ratio of omega‐6 to omega‐3 polyunsaturated acids during pregnancy and prevalence of post‐partum depression
AbstractObservational studies suggest association between low concentrations of omega‐3 family fatty acids and greater risk for post‐partum depression (PPD). The objective was to investigate the effect of unbalanced dietary intake of omega‐6/omega‐3 ratio >9:1 in the prevalence for PPD. The study comprises a prospective cohort with four waves of follow‐up during pregnancy and one following delivery. PPD was evaluated according to the Edinburgh Post‐partum Depression Scale (PPD ≥ 11) in 106 puerperae between 2005 and 2007, in Rio de Janeiro, Brazil. Independent variables included socio‐demographic, obstetric, pre‐pregnancy body mass index (BMI) and dietary intake data, which were obtained by means of a food frequency questionnaire in the first trimester of pregnancy. Statistical analysis involved calculation of PPD prevalence and multivariate Poisson regression with robust variance. PPD prevalence amounted to 26.4% [n = 28; confidence interval (CI) 95%: 18.0–34.8], and higher prevalences of PPD were observed in women who consumed an omega‐6/omega‐3 ratio >9:1 (60.0%) and in those with pre‐pregnancy BMI <18.5 kg/m2 (66.7%). These variables held as factors associated to PPD in the multivariate model, elevating the chances of occurrence of the outcome in 2.50 (CI 95%: 1.21–5.14) and 4.01 times (CI 95%: 1.96–8.20), respectively. Analyses were adjusted for age, schooling, pre‐pregnancy BMI, lipids consumption and time elapsed since delivery. It verified an association between omega‐6/omega‐3 ratio above 9:1, the levels recommended by the Institute of Medicine, and the prevalence of PPD. These results add to the evidence regarding the importance of omega‐6 and omega‐3 fatty acids in the regulation of mental health mechanisms.
Perinatal nutrition interventions and post-partum depressive symptoms
Abstract
Background
Postpartum depression
(PPD) is the most prevalent mood disorder associated with
childbirth
. No single cause of PPD has been identified, however the increased risk of
nutritional deficiencies
incurred through the high
nutritional requirements
of pregnancy may play a role in the pathology of depressive symptoms. Three nutritional interventions have drawn particular interest as possible non-invasive and cost-effective prevention and/or treatment strategies for PPD; omega-3 (n-3) long chain
polyunsaturated fatty acids
(LCPUFA),
vitamin D
and overall diet.
Methods
We searched for meta-analyses of randomised controlled trials (RCT's) of nutritional interventions during the
perinatal period
with PPD as an outcome, and checked for any trials published subsequently to the meta-analyses.
Results
Fish oil: Eleven RCT's of prenatal fish oil supplementation RCT's show null and positive effects on PPD symptoms. Vitamin D: no relevant RCT's were identified, however seven
observational studies
of maternal vitamin D levels with PPD outcomes showed inconsistent associations. Diet: Two Australian RCT's with dietary advice interventions in pregnancy had a positive and null result on PPD.
Limitations
With the exception of fish oil, few RCT's with nutritional interventions during pregnancy assess PPD.
Conclusions
Further research is needed to determine whether nutritional intervention strategies during pregnancy can protect against symptoms of PPD. Given the prevalence of PPD and ease of administering PPD measures, we recommend future prenatal nutritional RCT's include PPD as an outcome.
Major depressive disorder and nutritional medicine: a review of monotherapies and adjuvant treatments
Abstract
A literature review was conducted to examine the evidence for nutritional interventions in depression. It revealed a number of significant conclusions. Interestingly, more positive clinical trials were found to support adjuvant, rather than monotherapeutic, use of nutrients to treat depression. Much evidence exists in the area of adjuvant application of folic acid, S-adenosyl-methionine, omega-3, and L-tryptophan with antidepressants. Current evidence does not support omega-3 as an effective monotherapy to treat depression. However, this may be due, at least in part, to olive oil being used as the control intervention, some studies using docosahexaenoic acid alone or a higher docosahexaenoic acid to eicosapentaenoic acid ratio, and significant heterogeneity regarding depressive populations. Nevertheless, adjunctive prescription of omega-3 with antidepressants, or in people with dietary deficiency, may be beneficial. Inositol lacks evidence as an effective antidepressant and cannot be currently recommended. Evidence on the use of L-trytophan for depression is inconclusive, and additional studies utilizing a more robust methodology are required.
Nutrition in chronic pancreatitis
Abstract
The pancreas is a major player in nutrient digestion. In chronic pancreatitis both exocrine and endocrine insufficiency may develop leading to malnutrition over time. Maldigestion is often a late complication of chronic pancreatic and depends on the severity of the underlying disease. The severity of malnutrition is correlated with two major factors: (1) malabsorption and depletion of nutrients (e.g., alcoholism and pain) causes impaired nutritional status; and (2) increased metabolic activity due to the severity of the disease. Nutritional deficiencies negatively affect outcome if they are not treated. Nutritional assessment and the clinical severity of the disease are important for planning any nutritional intervention. Good nutritional practice includes screening to identify patients at risk, followed by a thoroughly nutritional assessment and nutrition plan for risk patients. Treatment should be multidisciplinary and the mainstay of treatment is abstinence from alcohol, pain treatment, dietary modifications and pancreatic enzyme supplementation. To achieve energy-end protein requirements, oral supplementation might be beneficial. Enteral nutrition may be used when patients do not have sufficient calorie intake as in pylero-duodenal-stenosis, inflammation or prior to surgery and can be necessary if weight loss continues. Parenteral nutrition is very seldom used in patients with chronic pancreatitis and should only be used in case of GI-tract obstruction or as a supplement to enteral nutrition.
Keywords: Chronic pancreatitis, Malnutrition, Nutritional risk, Malabsorption, Nutritional risk screening, Metabolism, Nutritional assessment, Nutrition therapy
Depression, daily stressors and inflammatory responses to high-fat meals: when stress overrides healthier food choices
Abstract
Depression, stress and diet can all alter inflammation. This double-blind, randomized crossover study addressed the impact of daily stressors and a history of major depressive disorder (MDD) on inflammatory responses to high-fat meals. During two separate 9.5 h admissions, 58 healthy women (38 breast cancer survivors and 20 demographically similar controls), mean age 53.1 years, received either a high saturated fat meal or a high oleic sunflower oil meal. The Daily Inventory of Stressful Events assessed prior day stressors and the Structured Clinical Interview for DSM-IV evaluated MDD. As expected, for a woman with no prior day stressors, C-reactive protein (CRP), serum amyloid A (SAA), intercellular adhesion molecule-1 (sICAM-1) and vascular cell adhesion molecule-1 (sVCAM-1) were higher following the saturated fat meal than the high oleic sunflower oil meal after controlling for pre-meal measures, age, trunk fat and physical activity. But if a woman had prior day stressors, these meal-related differences disappeared—because the stressors heightened CRP, SAA, sICAM-1 and sVCAM-1 responses to the sunflower oil meal, making it look more like the responses to the saturated fat meal. In addition, women with an MDD history had higher post-meal blood pressure responses than those without a similar history. These data show how recent stressors and an MDD history can reverberate through metabolic alterations, promoting inflammatory and atherogenic responses.
Pain Mitigation
Nutraceuticals and osteoarthritis pain
Abstract
Arthritis is a chronic disease of joints. It is highly prevalent, particularly in the elderly, and is commonly associated with pain that interferes with quality of life. Because of its chronic nature, pharmacological approaches to pain relief and joint repair must be safe for long term use, a quality many current therapies lack. Nutraceuticals refer to compounds or materials that can function as nutrition and exert a potential therapeutic effect, including the relief of pain, such as pain related to arthritis, of which osteoarthritis (OA) is the most common form. Of interest, nutraceuticals have recently been shown to have potential in relieving OA pain in human clinical trials. Emerging evidence indicates nutraceuticals may represent promising alternatives for the relief of OA pain. In this paper, we will overview OA pain and the use of nutraceuticals in OA pain management, focusing on those that have been evaluated by clinical trials. Furthermore, we discuss the biologic and pharmacologic actions underlying the nutraceutical effects on pain relief based on the potential active ingredients identified from traditional nutraceuticals in OA pain management and their potential for drug development. The review concludes by sharing our viewpoints that future studies should prioritize elucidating the mechanisms of action of nutraceuticals in OA and developing nutraceuticals that not only relieve OA pain, but also mitigate OA pathology.
Guidelines for the understanding and management of pain in chronic pancreatitis
Abstract
Abdominal pain is the foremost complication of chronic pancreatitis (CP). Pain can be related to recurrent or chronic inflammation, local complications or neurogenic mechanisms with corresponding changes in the nervous systems. Both pain intensity and the frequency of pain attacks have been shown to reduce quality of life in patients with CP. Assessment of pain follows the guidelines for other types of chronic pain, where the multidimensional nature of symptom presentation is taken into consideration. Quantitative sensory testing may be used to characterize pain, but is currently used in a research setting in advanced laboratories. For pain relief, current guidelines recommend a simple stepwise escalation of analgesic drugs with increasing potency until pain relief is obtained. Abstinence from alcohol and smoking should be strongly advised. Pancreatic enzyme therapy and antioxidants may be helpful as initial treatment. Endoscopic treatment can be used in patients with evidence of ductal obstruction and may be combined with extracorporeal shock wave lithothripsy. The best candidates are those with distal obstruction of the main pancreatic duct and in early stage of disease. Behavioral interventions should be part of the multidisciplinary approach to chronic pain management particularly when psychological impact is experienced. Surgery should be considered early and after a maximum of five endoscopic interventions. The type of surgery depends on morphological changes of the pancreas. Long-term effects are variable, but high success rates have been reported in open studies and when compared with endoscopic treatment. Finally, neurolytical interventions and neuromodulation can be considered in difficult patients.
Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Pediatric Critically Ill Patient: Society of Critical Care Medicine and American Society for Parenteral and Enteral Nutrition
Abstract
This document represents the first collaboration between 2 organizations-the American Society for Parenteral and Enteral Nutrition and the Society of Critical Care Medicine-to describe best practices in nutrition therapy in critically ill children. The target of these guidelines is intended to be the pediatric critically ill patient (>1 month and <18 years) expected to require a length of stay >2-3 days in a PICU admitting medical, surgical, and cardiac patients. In total, 2032 citations were scanned for relevance. The PubMed/MEDLINE search resulted in 960 citations for clinical trials and 925 citations for cohort studies. The EMBASE search for clinical trials culled 1661 citations. In total, the search for clinical trials yielded 1107 citations, whereas the cohort search yielded 925. After careful review, 16 randomized controlled trials and 37 cohort studies appeared to answer 1 of the 8 preidentified question groups for this guideline. We used the GRADE criteria (Grading of Recommendations, Assessment, Development, and Evaluation) to adjust the evidence grade based on assessment of the quality of study design and execution. These guidelines are not intended for neonates or adult patients. The guidelines reiterate the importance of nutrition assessment-particularly, the detection of malnourished patients who are most vulnerable and therefore may benefit from timely intervention. There is a need for renewed focus on accurate estimation of energy needs and attention to optimizing protein intake. Indirect calorimetry, where feasible, and cautious use of estimating equations and increased surveillance for unintended caloric underfeeding and overfeeding are recommended. Optimal protein intake and its correlation with clinical outcomes are areas of great interest. The optimal route and timing of nutrient delivery are areas of intense debate and investigations. Enteral nutrition remains the preferred route for nutrient delivery. Several strategies to optimize enteral nutrition during critical illness have emerged. The role of supplemental parenteral nutrition has been highlighted, and a delayed approach appears to be beneficial. Immunonutrition cannot be currently recommended. Overall, the pediatric critical care population is heterogeneous, and a nuanced approach to individualizing nutrition support with the aim of improving clinical outcomes is necessary.
Physiology of Visceral Pain
Abstract
Pain involving thoracic, abdominal, or pelvic organs is a common cause for physician consultations, including one-third of chronic pain patients who report that visceral organs contribute to their suffering. Chronic visceral pain conditions are typically difficult to manage effectively, largely because visceral sensory mechanisms and factors that contribute to the pathogenesis of visceral pain are poorly understood. Mechanistic understanding is particularly problematic in "functional" visceral diseases where there is no apparent pathology and pain typically is the principal complaint. We review here the anatomical organization of the visceral sensory innervation that distinguishes the viscera from innervation of all other tissues in the body. The viscera are innervated by two nerves that share overlapping functions, but also possess notably distinct functions. Additionally, the visceral innervation is sparse relative to the sensory innervation of other tissues. Accordingly, visceral sensations tend to be diffuse in character, are typically referred to nonvisceral somatic structures and thus are difficult to localize. Early arguments about whether the viscera were innervated ("sensate") and later, whether innervated by nociceptors, were resolved by advances reviewed here in the anatomical and functional attributes of receptive endings in viscera that contribute to visceral pain (i.e., visceral nociceptors). Importantly, the contribution of plasticity (i.e., sensitization) of peripheral and central visceral nociceptive mechanisms is considered in the context of persistent, chronic visceral pain conditions. The review concludes with an overview of the functional anatomy of visceral pain processing. © 2016 American Physiological Society. Compr Physiol 6:1609-1633, 2016.
Effect of Branched-Chain Amino Acid Supplementation on Recovery Following Acute Eccentric Exercise
Abstract
This study investigated the effect of branched-chain amino acid (BCAA) supplementation on recovery from eccentric exercise. Twenty males ingested either a BCAA supplement or placebo (PLCB) prior to and following eccentric exercise. Creatine kinase (CK), vertical jump (VJ), maximal voluntary isometric contraction (MVIC), jump squat (JS) and perceived soreness were assessed. No significant (p > 0.05) group by time interaction effects were observed for CK, soreness, MVIC, VJ, or JS. CK concentrations were elevated above baseline (p < 0.001) in both groups at 4, 24, 48 and 72 hr, while CK was lower (p = 0.02) in the BCAA group at 48 hr compared to PLCB. Soreness increased significantly from baseline (p < 0.01) in both groups at all time-points; however, BCAA supplemented individuals reported less soreness (p < 0.01) at the 48 and 72 hr time-points. MVIC force output returned to baseline levels (p > 0.05) at 24, 48 and 72 hr for BCAA individuals. No significant difference between groups (p > 0.05) was detected for VJ or JS. BCAA supplementation may mitigate muscle soreness following muscle-damaging exercise. However, when consumed with a diet consisting of ~1.2 g/kg/day protein, the attenuation of muscular performance decrements or corresponding plasma CK levels are likely negligible.
Chronic Pancreatitis and Nutrition Therapy
Abstract
Chronic pancreatitis is a complex and irreversible disease of the pancreas and is associated with significant morbidity and mortality. Nutrition deficiencies in chronic pancreatitis are common and can be atypical in nature. As such, the management of these deficiencies can be individualized for patients. The aim of this review is to discuss the components of nutrition deficiencies in chronic pancreatitis, their management, and the current areas of research that are being explored. The clinical guidelines of major national and international societies were analyzed for recommendations on the nutrition management of chronic pancreatitis. The etiology of nutrition deficiencies in chronic pancreatitis is multifactorial and includes aspects of exocrine and/or endocrine dysfunction, significant abdominal pain, often persistent alcohol consumption, and increased metabolic activity. A large number of patients with nutrition deficiencies are underrecognized and undertreated. Although the majority of these patients can be managed by oral and pancreatic enzyme supplementation, some patients may require enteral tube feeding and, in rare cases, parenteral feeding. Current areas of research include the accurate identification of patients at risk for nutrition deficiencies, optimization of feeding regimens, and research into islet cell autotransplantation.
A systematic review and meta-analysis of nutrition interventions for chronic noncancer pain
Abstract
Background: This systematic review aimed to evaluate the impact of nutrition interventions on participant reported pain severity and intensity in populations with chronic pain.
Methods: Eight databases were systematically searched for studies that included adult populations with a chronic pain condition, a nutrition intervention and a measure of pain. Where possible, data were pooled using meta-analysis. Seventy-one studies were included, with 23 being eligible for meta-analysis.
Results: Studies were categorised into four groups: (i) altered overall diet with 12 of 16 studies finding a significant reduction in participant reported pain; (ii) altered specific nutrients with two of five studies reporting a significant reduction in participant reported pain; (iii) supplement-based interventions with 11 of 46 studies showing a significant reduction in pain; and (iv) fasting therapy with one of four studies reporting a significant reduction in pain. The meta-analysis found that, overall, nutrition interventions had a significant effect on pain reduction with studies testing an altered overall diet or just one nutrient having the greatest effect.
Conclusions: This review highlights the importance and effectiveness of nutrition interventions for people who experience chronic pain.
Pain regulation by gut microbiota: molecular mechanisms and therapeutic potential
Abstract
The relationship between gut microbiota and neurological diseases, including chronic pain, has received increasing attention. The gut microbiome is a crucial modulator of visceral pain, whereas recent evidence suggests that gut microbiota may also play a critical role in many other types of chronic pain, including inflammatory pain, headache, neuropathic pain, and opioid tolerance. We present a narrative review of the current understanding on the role of gut microbiota in pain regulation and discuss the possibility of targeting gut microbiota for the management of chronic pain. Numerous signalling molecules derived from gut microbiota, such as by-products of microbiota, metabolites, neurotransmitters, and neuromodulators, act on their receptors and remarkably regulate the peripheral and central sensitisation, which in turn mediate the development of chronic pain. Gut microbiota-derived mediators serve as critical modulators for the induction of peripheral sensitisation, directly or indirectly regulating the excitability of primary nociceptive neurones. In the central nervous system, gut microbiota-derived mediators may regulate neuroinflammation, which involves the activation of cells in the blood-brain barrier, microglia, and infiltrating immune cells, to modulate induction and maintenance of central sensitisation. Thus, we propose that gut microbiota regulates pain in the peripheral and central nervous system, and targeting gut microbiota by diet and pharmabiotic intervention may represent a new therapeutic strategy for the management of chronic pain.
Exercise interventions for the treatment of chronic low back pain: a systematic review and meta-analysis of randomised controlled trials
Abstract
Objective: To determine, for adults with chronic low back pain, which exercise interventions are the most effective at reducing pain compared to other treatments.
Data sources: A search of MEDLINE, CINAHL, EMBASE, SPORTDiscus, PsycINFO and The Cochrane Library was conducted up to October 2014.
Review methods: Databases were searched for published reports of randomised trials that investigated the treatment of chronic low back pain of non-specific origin with an exercise intervention. Two authors independently reviewed and selected relevant trials. Methodological quality was evaluated using the Downs and Black tool.
Results: Forty-five trials met the inclusion criteria and thirty-nine were included in the meta-analysis. Combined meta-analysis revealed significantly lower chronic low back pain with intervention groups using exercise compared to a control group or other treatment group (Standard Mean Deviation (SMD) =-0.32, CI 95% -0.44 to -0.19, P<0.01). Separate exploratory subgroup analysis showed a significant effect for strength/resistance and coordination/stabilisation programs.
Conclusions: Our results found a beneficial effect for strength/resistance and coordination/stabilisation exercise programs over other interventions in the treatment of chronic low back pain and that cardiorespiratory and combined exercise programs are ineffective.
Modulation of MicroRNAs Linked to Pain-migraine by Ketogenic Diet (P14-007-19)
Abstract
Objectives
Migraine is a neurovascular disorder with complex pathophysiology. The ketogenic diet (KD) it is well recognized to treat epilepsy drug-resistant as well as other neurological disorder including migraine. Our previous study showed that six weeks of biphasic KD influences circulating microRNAs (miRs) linked to energy metabolism (Cannataro R., Perri M. et al. MicroRNA (2019) 8: 1). At the end of the study, six female obese patients self-reported to had a better outcome of pain-migraine and migraine attack. Therefore, we analyzed miRs associated with pain-migraine.
Methods
The KD was planned depending on the dietary diary recorded by each subject for 14 days before starting the KD program and was set with less than 30 g of carbohydrate per day. Six female obese patients in stage 1 of the Edmonton Obesity Staging System (EOSS) parameter self-reporting suffering of migraine were analyzed for miRs linked to pain-migraine. 200 microL of blood/serum was used for the extraction of miRs and their expression profile was achieved by direct hybridization using the multiplexed NanoString nCounter-flex system. In silico bioinformatics approach (using miRWalk, miR target link, and target scan) were employed to detect target genes and miRNA-regulated biological function.
Results
The six female obese patients whose reduce their weight during the biphasic KD program, self-reported that migraines attack disappeared only during, and not outside, the cycles of biphasic KD program. Among the 7 miRs linked to pain-migraine (Gallelli L. et al. MicroRNA (2017) 6: 152), 6 were found substantially at the same levels before and after the KD program (Table 1). Even, the brain-enriched hsa-382–5p was confirmed to be unchanged according to previous finding (Andersen H.H. et al. Mol Neurobiol. (2016) 53: 1494) (Table 1). While the has-miR-590–5p and the emerging hsa -miR-660–3p were strongly affected by KD (Fig 1A-B). The validated target gene of this three latter miRs were 3, 2 and any respectively (Table 2).
Conclusions
KD thought miRs modulation could contribute to restore brain excitability and metabolism and to counteract neuroinflammation and pain-migraine, although the precise mechanism is still unclear.
The effects of probiotic supplementation on emotional memory and pain response
The human intestinal microbiota is the ecological community of micro-organisms that share our gastrointestinal tract(
1
). Increasing evidence suggests a mediating relationship exists between gut microbiota activity and the brain(
2
). Recent research has shown that probiotic administration is capable of affecting brain activity in regions controlling central processing of emotion and sensation(
3
). Developing on these findings, the aim of the present study was to assess the effect of probiotic administration on emotional memory (EM), anxiety and acute peripheral pain response (PR).
A randomised double-blind controlled trial, involving sixty participants aged 18–40 years, was conducted. Participants completed a six-week intervention, consuming either probiotic (Lactobacillus acidophilus CUL60 and CUL21, Bifidobacterium lactis CUL34, Bifidobacterium bifidum CUL20) or placebo (maltodextrin) capsules. Participants attended pre- and post-intervention sessions. Anxiety was assessed using the State-Trait Anxiety Inventory questionnaire at three time-points during each session (baseline, post-EM task, post-PR task), and again at weeks two and four during intervention. EM was assessed once in each session using a Remember, Know, Guess task; involving the presentation and recall of neutral and negative emotionally arousing images. A cold pressor test was used to assess PR; pain threshold, removal of hand and pain tolerance times were measured. A visual analogue scale was used to assess subjective pain. Finally, immune function was measured via salivary IgA, collected at three time-points in each session (baseline, post-EM task, post-PR task).
When comparing treatment groups in terms of EM, the probiotic group recalled significantly more negative images compared to placebo (P = 0·022, Figure 1.a). This effect was more pronounced in female participants (P = 0·009, Figure 1.b). For male participants only, pain threshold was significantly reduced at the second assessment under the placebo condition (−3·687 seconds, P = 0·027, Figure 1.c) but not following probiotic administration, potentially indicating a protective effect of probiotic treatment on pain threshold. No further significant results were observed.
Nutrition impact symptoms are related to malnutrition and quality of life – A cross-sectional study of patients with chronic liver disease
Summary
Background and aims
Patients with chronic liver disease often experience symptoms that affect their ability to eat. These symptoms can contribute to weight loss and malnutrition. We aimed to examine the prevalence of nutrition impact symptoms (NIS) in patients with chronic liver disease, and to investigate the relationships between NIS, malnutrition and health-related quality of life.
Methods
In a cross-sectional study on adult patients with chronic liver disease under evaluation for liver transplantation, we studied NIS with two questionnaires: the Eating Symptoms Questionnaire and the Disease-Related Appetite Questionnaire. Malnutrition was primarily assessed with the Global Leadership Initiative on Malnutrition (GLIM) criteria. Health-related quality of life (HRQOL) was assessed with the Chronic Liver Disease Questionnaire.
Results
Among the 133 included patients, 90% reported one or more NIS and 51% reported four or more NIS. The most common symptoms were dry mouth (61%), abdominal pain (58%), diarrhoea (45%) and nausea (41%). Malnutrition was present in 32% according to GLIM criteria. Malnourished patients reported more NIS (p = 0.004) and had lower HRQOL (p < 0.001). Certain NIS, such as pain, poor appetite, changes in taste and early satiety, were predictors for malnutrition.
Conclusions
NIS are common in patients with chronic liver disease and are associated with malnutrition and worse HRQOL. NIS should therefore be systematically assessed in patients with chronic liver disease. Whether identification and proper management of NIS can prevent malnutrition and improve quality of life deserves further exploration.
Exploring the Relationship Between Serum Magnesium, Inflammation, and Chronic Pain in a Vermont Primary Care Population
Abstract
Objectives
We sought to describe the relationship between serum magnesium, inflammation, and chronic pain in adult primary care patient.
Methods
We sought to describe this relationship utilizing a cross-sectional analysis of medical records from 5639 adults (mean age 59 years; 42% men) seen in The University of Vermont Medical Center primary care clinics between 2015 and 2018. Patients with at least one serum magnesium level, C-reactive protein (CRP, a measure of inflammation) level, and chronic pain score (self-reported visual analogue scale) were included.
Results
Univariate analysis confirmed the relationship between serum magnesium and chronic pain (−0.31 points/mg/dL; 95% CI −0.47, −0.14; P < 0.001). However, when serum magnesium and CRP were both included in the model, the relationship with pain is unclear (N = 1345; CI −0.003, 0.002; P = 0.69).
Conclusions
For adults seen in primary care, lower serum magnesium levels are associated with chronic pain. This inverse relationship is not explained by random noise, including age and gender. The complex relationship between serum magnesium, CRP, and pain is complex requires further exploration.
Omega-3 Endocannabinoid-Epoxides Are Novel Anti-inflammatory and Anti-Pain Lipid Metabolites (FS15-01-19)
Abstract
Objectives
Omega-3 fatty acid derived endocannabinoids are metabolized by cytochrome P450s to form bioactive endocannabinoid epoxides that are anti-inflammatory
Methods
Lipidomics, LC-MS/MS, microglial cells culture, lipid synthesis, extractions, enzymology
Results
Cannabinoids are found in marijuana and also are produced naturally in the body from ω-3 and ω-6 fatty acids. Exocannabinoids in marijuana, are known to be responsible for some of its euphoric effects, but they also exhibit anti-inflammatory benefits. Our study revealed a cascade of enzymatic reactions that convert ω-3 fatty acids into anti-inflammatory endocannabinoid epoxides that act through the same receptors in the body as marijuana (PNAS 2017). Endocannabinoids are ligands for cannabinoid receptor 1 and 2 (CB1 and CB2). CB1 receptor agonists exhibit psychotropic properties while CB2 receptor agonists have anti-inflammatory effects. Consequently, there is a strong interest in the discovery of CB2 selective agonists to mitigate inflammatory pathologies. The work details the discovery and characterization of naturally occurring ω-3–derived endocannabinoid epoxides that are formed via enzymatic oxidation of ω-3 endocannabinoids by cytochrome P450 epoxygenases. These dual functional ω-3 endocannabinoid epoxides exhibit preference towards binding to CB2 receptor and are anti-inflammatory and vasodilatory and reciprocally modulate platelet aggregation. Some of the other regioisomers of ω-3 endocannabinoid epoxides are partial agonists of CB1 and stop tumor cell metastasis (J. Med. Chem 2018). By virtue of their physiological properties, they are expected to play important roles in neuroinflammation and pain.
Conclusions
This finding demonstrates how omega-3 fatty acids can produce some of the same medicinal qualities as marijuana, but without a psychotropic effect. In summary, the ω-3 endocannabinoid epoxides are found at concentrations comparable to those of other endocannabinoids and are expected to play critical roles during inflammation in vivo
Funding Sources
American Heart Association Scientist Development award, National Institute of Health (NIH) R01, NIH R03, USDA, National Multiple Sclerosis Society.
Nutrition Status and Health‐Related Quality of Life Among Outpatients With Advanced Head and Neck Cancer
AbstractThis pilot study evaluated nutrition status and health‐related quality of life (HRQOL) outcomes among outpatients with head and neck cancer (HNC). Data were collected from 19 patients (18 males, 1 female) during 3 time points: once before chemoradiotherapy (CRT) initiation and 1 and 3 months after CRT. Nutrition status was evaluated using the Scored Patient‐Generated Subjective Global Assessment (PG‐SGA). Malnutrition was defined as PG‐SGA stage B (moderate/suspected malnutrition) or stage C (severely malnourished). HRQOL was assessed through the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire (EORTC QLQ‐C30) and its HNC‐specific module (QLQ‐H&N35). We found that well‐nourished patients reported having fewer issues with pain, fatigue, appetite loss, chewing, sticky saliva, coughing, and social eating than those categorized as malnourished (P < .05). The association between the global quality‐of‐life score and PG‐SGA score was statistically significant but weak in strength (r = −0.37, P = .012). Although PG‐SGA identified 70% as either moderately or severely malnourished before treatment initiation, the mean body mass index was in the overweight category (29 ± 5 kg/m2). Compared with pretreatment, patients reported more severe problems with chewing, swallowing, sticky saliva, dry mouth, speech, social eating, and taste and smell sensations at 1‐month follow‐up, although issues with dry mouth persisted 3 months post treatment (P = .003). In conclusion, malnourished patients reported having worse HRQOL symptoms compared with well‐nourished patients. Routine nutrition and psychosocial assessment through PG‐SGA and EORTC tools might help identify patients in need of nutrition and psychosocial care.
Combination treatment for migraine and other pain
Abstract
Disclosed herein are methods of treating pain, such as migraine, comprising administering meloxicam and rizatriptan to a human being suffering from pain, such as migraine. For migraine, these methods may be particularly useful when the meloxicam and rizatriptan are administered while the human being is suffering from an acute attack of migraine pain or migraine aura. In some embodiments, the combination of meloxicam and rizatriptan may be administered in a manner that results in a Tmax of meloxicam of 3 hours or less.
Fibromyalgia and nutrition: Therapeutic possibilities?
Abstract
Fibromyalgia (FM) is a complex chronic condition of unknown etiology, characterized by deep and widespread pain, sleep problems, cognitive impairment, fatigue, and other well-known functional symptoms. Recently, it has been proposed that an imbalance of nutritive components, including essential metal ions and vitamins, might play a critical role in the development of FM. Muscle pain has been associated with deficiencies in amino acids, magnesium, selenium, vitamins B and D, as well as with the harmful effects of heavy metals, such as mercury, cadmium, and lead. Research indicates that patients deficient in certain essential nutrients may develop dysfunction of pain inhibitory mechanisms together with fatigue and other FM symptoms. Additionally, mercury and other toxic elements may interfere with the bioavailability of essential nutrients. This review examines the many effects of metals and vitamins in pain evaluation of FM patients. Dietary guidance is therefore critical for FM patients to help them in correcting a suboptimal or deficient intake of essential nutrients. When optimal levels of nutrition are achieved, pain levels are usually lowered. Additional research is recommended in the field of FM and nutrition to disclose further possible relationships.
Adherence to nutrition‐based cancer prevention guidelines and breast, prostate and colorectal cancer risk in the MCC‐Spain case–control study
AbstractProstate, breast and colorectal cancer are the most common tumours in Spain. The aim of the present study was to evaluate the association between adherence to nutrition‐based guidelines for cancer prevention and prostate, breast and colorectal cancer, in the MCC‐Spain case–control study. A total of 1,718 colorectal, 1,343 breast and 864 prostate cancer cases and 3,431 population‐based controls recruited between 2007 and 2012, were included in the present study. The World Cancer Research Fund/American Institute for Cancer Research (WCRC/AICR) score based on six recommendations for cancer prevention (on body fatness, physical activity, foods and drinks that promote weight gain, plant foods, animal foods and alcoholic drinks; score range 0–6) was constructed. We used unconditional logistic regression analysis adjusting for potential confounders. One‐point increment in the WCRF/AICR score was associated with 25% (95% CI 19–30%) lower risk of colorectal, and 15% (95% CI 7–22%) lower risk of breast cancer; no association with prostate cancer was detected, except for cases with a Gleason score ≥7 (poorly differentiated/undifferentiated tumours) (OR 0.87, 95% CI 0.76–0.99). These results add to the wealth of evidence indicating that a great proportion of common cancer cases could be avoided by adopting healthy lifestyle habits.
Low fermentable, oligo-, di-, mono-saccharides and polyol diet in the treatment of irritable bowel syndrome: A systematic review and meta-analysis
Abstract
Objectives: The aim of this review was to systematically assess and meta-analyze the effects of a low fermentable, oligo-, di-, mono-saccharides and polyol (FODMAP) diet (LFD) on the severity of symptoms, quality of life, and safety in patients with irritable bowel syndrome (IBS).
Methods: The MEDLINE/PubMed, Scopus, and Cochrane Library databases were screened through January 19, 2016. Randomized controlled trials (RCTs) that compared LFD to other diets were included if they assessed symptoms of IBS or abdominal pain in patients with IBS. Safety, quality of life, anxiety, depression, and effect on gut microbiota were defined as secondary outcomes. Standardized mean difference (SMD) and 95% confidence interval (CI) were calculated.
Results: Nine RCTs with a total of 596 subjects were included. Three RCTs compared LFD with a habitual diet, two RCTs provided all meals and compared LFD with a western diet, one RCT each compared LFD with a diet high in FODMAPs or a sham diet, and two RCTs compared with other diet recommendations for IBS. A meta-analysis revealed significant group differences for LFD compared with other diets with regard to gastrointestinal symptoms (SMD = -0.62; 95% CI = -0.93 to -0.31; P = 0.0001), abdominal pain (SMD = -0.50; 95% CI = -0.77 to -0.22; P = 0.008), and health-related quality of life (SMD = 0.36; 95% CI = 0.10-0.62; P = 0.007). Three studies reported a significant reduction in luminal bifidobacteria after LFD. Adverse events were assessed in three RCTs only and no intervention-related adverse events were reported.
Conclusions: This meta-analysis found evidence of the short-term efficacy and safety of LFD in patients with IBS. However, only a preliminary recommendation for LFD can be made until long-term effects are investigated.
Chronic Abdominal Pain In Children: A Technical Report of the American Academy of Pediatrics and the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition: AAP Subcommittee and NASPGHAN Committee on Chronic Abdominal Pain
Abstract
Chronic abdominal pain, defined as long-lasting intermittent or constant abdominal pain, is a common pediatric problem encountered by primary care physicians, medical subspecialists and surgical specialists. Chronic abdominal pain in children is usually functional-that is, without objective evidence of an underlying organic disorder. The Subcommittee on Chronic Abdominal Pain of the American Academy of Pediatrics and the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition has prepared this report based on a comprehensive, systematic review and rating of the medical literature. This report accompanies a clinical report based on the literature review and expert opinion.
The subcommittee examined the diagnostic and therapeutic value of a medical and psychologic history, diagnostic tests, and pharmacological and behavioral therapy. The presence of alarm symptoms or signs (such as weight loss, gastrointestinal bleeding, persistent fever, chronic severe diarrhea and significant vomiting) is associated with a higher prevalence of organic disease. There was insufficient evidence to state that the nature of the abdominal pain or the presence of associated symptoms (such as anorexia, nausea, headache and joint pain) can discriminate between functional and organic disorders. Although children with chronic abdominal pain and their parents are more often anxious or depressed, the presence of anxiety, depression, behavior problems or recent negative life events does not distinguish between functional and organic abdominal pain. Most children who are brought to the primary care physician's office for chronic abdominal pain are unlikely to require diagnostic testing. Pediatric studies of therapeutic interventions were examined and found to be limited or inconclusive.
Lactobacillus reuteri DSM 17938 in the Treatment of Functional Abdominal Pain in Children: RCT Study
Abstract
Objectives:
Beneficial therapeutic effect of probiotics has been reported in children with the irritable bowel syndrome (IBS) but not consistently in other functional abdominal pain-related disorders. The aim of the present study was to investigate the effect of Lactobacillus reuteri DSM 17938 in the treatment of functional abdominal pain (FAP) and IBS in children.
Methods:
Children (age 4–18 years) referred to pediatric gastroenterologist at Children's Hospital Zagreb from May 2012 to December 2014, diagnosed as FAP or IBS, were randomized to receive L reuteri DSM 17938 108 CFU daily or placebo. The study was a prospective, randomized, double-blind, placebo-controlled parallel study. Symptoms were evaluated using Wong-Baker FACES pain rating scale for pain and Bristol scale for stool shape and consistence.
Results:
Data were analyzed for 55 children (26 in the intervention group and 29 in the placebo group). Children in the intervention group had significantly more days without pain (median 89.5 vs 51 days, P = 0.029). Abdominal pain was less severe in children taking probiotics during the second month (P < 0.05) and fourth month (P < 0.01). The 2 groups did not differ in the duration of abdominal pain, stool type, or absence from school. Both groups experienced significant reduction in the severity of abdominal pain from first to fourth month, with the reduction more prominent in the intervention group (P < 0.001 vs P = 0.004).
Conclusions:
Administration of L reuteri DSM 17938 was associated with a possible reduction of the intensity of pain and significantly more days without pain in children with FAP and IBS.
Long-term quality of life improvement for chronic intractable back and leg pain patients using spinal cord stimulation: 12-month results from the SENZA-RCT
Abstract
Purpose
Chronic axial low-back pain is a debilitating disorder that impacts all aspects of an afflicted individual’s life. Effective, durable treatments have historically been elusive. Interventional therapies, such as spinal cord stimulation (SCS), have shown limited efficacy at best. Recently, a novel treatment, 10 kHz SCS, has demonstrated superior pain relief compared with traditional SCS in a randomized controlled trial (RCT). In this manuscript, we report on the long-term improvements in quality of life (QoL) outcomes for subjects enrolled in this study.
Methods
A prospective, multicenter, randomized controlled trial (SENZA-RCT) was conducted. Patients with both chronic back and leg pain were enrolled and randomized (1:1) into 10 kHz SCS or traditional SCS treatment groups. A total of 171 subjects received a permanent SCS device implant. QoL and functionality measures were collected up to 12 months. The device remote control utilization, which is an indication of patient interaction with the device for adjustments, was collected at 24-month post-implantation.
Results
At 12 months, a higher proportion of 10 kHz SCS subjects had marked improvement of their disability (Oswestry Disability Index) to a “moderate” or “minimal” impact on their daily function versus the control group. The subjects also reported better improvement in the Global Assessment of Functioning, Clinician Global Impression of Change, Pittsburgh Sleep Quality Index, and short-form McGill Pain Questionnaire, compared to traditional SCS subjects. The 10 kHz SCS subjects also reported far higher rates of both driving and sleeping with their device turned on, as well as reduced reliance on their programmers to adjust therapy settings.
Conclusions
In addition to superior pain relief, 10 kHz SCS provides long-term improvements in quality of life and functionality for subjects with chronic low-back and leg pain. Trial registration: ClinicalTrials.gov (NCT01609972).
Oro‐facial pain and nutrition: a forgotten relationship?
Summary
Oro‐facial pain (OFP) is known to exert profound impacts on quality of life including functionally and psychosocially mediated changes in dietary intake and thereby nutrition. This commentary explores the evidence base available on chronic oro‐facial pain, diet and nutrition and discusses current dietary guidance for individuals with chronic OFP; potential impact of chronic OFP on eating and nutritional status; impact of nutritional status on pathophysiology of chronic OFP; and potential role of nutrition in the management of chronic OFP.
A systematic review and meta‐analysis of nutrition interventions for chronic noncancer pain
AbstractBackground
This systematic review aimed to evaluate the impact of nutrition interventions on participant reported pain severity and intensity in populations with chronic pain.
Methods
Eight databases were systematically searched for studies that included adult populations with a chronic pain condition, a nutrition intervention and a measure of pain. Where possible, data were pooled using meta‐analysis. Seventy‐one studies were included, with 23 being eligible for meta‐analysis.
Results
Studies were categorised into four groups: (i) altered overall diet with 12 of 16 studies finding a significant reduction in participant reported pain; (ii) altered specific nutrients with two of five studies reporting a significant reduction in participant reported pain; (iii) supplement‐based interventions with 11 of 46 studies showing a significant reduction in pain; and (iv) fasting therapy with one of four studies reporting a significant reduction in pain. The meta‐analysis found that, overall, nutrition interventions had a significant effect on pain reduction with studies testing an altered overall diet or just one nutrient having the greatest effect.
Conclusions
This review highlights the importance and effectiveness of nutrition interventions for people who experience chronic pain.
Symptom management, nutrition and hydration at end-of-life: a qualitative exploration of patients’, carers’ and health professionals’ experiences and further research questions
Abstract
Background
Symptom management is an essential aspect of palliative and end-of-life care, but evidence suggests that patients’ symptoms may not always be relieved, causing significant harm to patients and magnifying their relatives’ distress. A growing body of evidence focuses on symptom management at the end-of-life, but research funding for palliative care remains disproportionately low. It is therefore crucial that research funding is targeted at areas of importance to patients and relatives. The Palliative and end-of-life care Priority Setting Partnership (PeolcPSP) undertook a UK-wide free-text survey to establish research priorities within palliative and end-of-life care and disseminated its results in 2015. Much of the data were related more broadly to personal perceptions and experiences rather than specific research questions. The aim of this article is to report on a supplementary analysis exploring the experiences and questions of PeolcPSP survey respondents regarding symptoms, hydration and nutrition.
Methods
The PeolcPSP data (n = 1403) were coded by a team of qualitative researchers in a supplementary analysis. There were 190 responses that related to symptoms, nutrition and hydration. The data were analysed thematically using Braun and Clarke’s approach.
Results
Five themes were identified: pain, breathlessness, agitation, nutrition and hydration. The majority of responses related to symptoms that were sub-optimally managed, in particular pain. Nutrition and hydration were of significant concern, particularly for carers. Overall, respondents consistently asked about the most effective, evidence-based methods for managing symptoms and suggested areas where further research is necessary.
Conclusions
This study highlights the perceptions and experiences of patients, families and professionals within palliative care, highlighting the need for improved care, communication and further research to establish which treatments are most effective within a palliative care population. This is essential to reduce harm and distress for patients and families.
Oral nutritional supplements containing n-3 polyunsaturated fatty acids affect quality of life and functional status in lung cancer patients during multimodality treatment: an RCT
Abstract
Background/Objectives:
Our objective was to investigate effects of an oral nutritional supplement containing n-3 polyunsaturated fatty acids (FAs) on quality of life, performance status, handgrip strength and physical activity in patients with non-small cell lung cancer (NSCLC) undergoing multimodality treatment.
Subjects/Methods:
In a double-blind experiment, 40 patients with stage III NSCLC were randomised to receive 2 cans/day of a protein- and energy-dense oral nutritional supplement containing n-3 polyunsaturated FAs (2.02 g eicosapentaenoic acid+0.92 g docosahexaenoic acid/day) or an isocaloric control supplement, during multimodality treatment. Quality of life, Karnofsky Performance Status, handgrip strength and physical activity (by wearing an accelerometer) were assessed. Effects of intervention were analysed by generalised estimating equations. P-values <0.05 were regarded as statistically significant.
Results:
The intervention group reported significantly higher on the quality of life parameters, physical and cognitive function (B=11.6 and B=20.7, P<0.01), global health status (B=12.2, P=0.04) and social function (B=22.1, P=0.04) than the control group after 5 weeks. The intervention group showed a higher Karnofsky Performance Status (B=5.3, P=0.04) than the control group after 3 weeks. Handgrip strength did not significantly differ between groups over time. The intervention group tended to have a higher physical activity than the control group after 3 and 5 weeks (B=6.6, P=0.04 and B=2.5, P=0.05).
Conclusion:
n-3 Polyunsaturated FAs may beneficially affect quality of life, performance status and physical activity in patients with NSCLC undergoing multimodality treatment.
Enteral nutritional support in prevention and treatment of pressure ulcers: A systematic review and meta-analysis
Abstract
Background:
There have been few systematic reviews and no meta-analyses of the clinical benefits of nutritional support in patients with, or at risk of developing, pressure ulcers. Therefore, this systematic review and meta-analysis was undertaken to address the impact of enteral nutritional support on pressure ulcer incidence and healing and a range of other clinically relevant outcome measures in this group.
Methods:
Fifteen studies (including eight randomised controlled trials (RCTs)) of oral nutritional supplements (ONS) or enteral
tube feeding
(ETF), identified using electronic databases (including Pub Med and Cochrane) and bibliography searches, were included in the systematic review. Outcomes including pressure ulcer incidence, pressure ulcer healing, quality of life, complications, mortality, anthropometry and dietary intake were recorded, with the aim of comparing nutritional support versus routine care (e.g. usual diet and pressure ulcer care) and nutritional formulas of different composition. Of these 15 studies, 5 RCTs comparing ONS (4 RCTs) and ETF (1 RCT) with routine care could be included in a meta-analysis of pressure ulcer incidence.
Results:
Meta-analysis showed that ONS (250–500 kcal, 2–26 weeks) were associated with a significantly lower incidence of pressure ulcer development in at-risk patients compared to routine care (odds ratio 0.75, 95% CI 0.62–0.89, 4 RCTs, n = 1224, elderly, post-surgical, chronically hospitalised patients). Similar results were obtained when a combined meta-analysis of ONS (4 RCT) and ETF (1 RCT) trials was performed (OR 0.74, 95% CI 0.62–0.88, 5 RCTs, n = 1325). Individual studies showed a trend towards improved healing of existing pressure ulcers with disease-specific (including high protein) versus standard formulas, although robust RCTs are required to confirm this. Although some studies indicate that total nutritional intake is improved, data on other outcome measures (quality of life) are lacking.
Conclusions:
This systematic review shows enteral nutritional support, particularly high protein ONS, can significantly reduce the risk of developing pressure ulcers (by 25%). Although studies suggest ONS and ETF may improve healing of PU, further research to confirm this trend is required.
Combining pain therapy with lifestyle: the role of personalized nutrition and nutritional supplements according to the SIMPAR Feed Your Destiny approach
Abstract
Recently, attention to the lifestyle of patients has been rapidly increasing in the field of pain therapy, particularly with regard to the role of nutrition in pain development and its management. In this review, we summarize the latest findings on the role of nutrition and nutraceuticals, microbiome, obesity, soy, omega-3 fatty acids, and curcumin supplementation as key elements in modulating the efficacy of analgesic treatments, including opioids. These main topics were addressed during the first edition of the Study In Multidisciplinary Pain Research workshop: “FYD (Feed Your Destiny): Fighting Pain”, held on April 7, 2016, in Rome, Italy, which was sponsored by a grant from the Italian Ministry of Instruction on “Nutraceuticals and Innovative Pharmacology”. The take-home message of this workshop was the recognition that patients with chronic pain should undergo nutritional assessment and counseling, which should be initiated at the onset of treatment. Some foods and supplements used in personalized treatment will likely improve clinical outcomes of analgesic therapy and result in considerable improvement of patient compliance and quality of life. From our current perspective, the potential benefit of including nutrition in personalizing pain medicine is formidable and highly promising.
Keywords: pain, personalized nutrition, nutritional supplements
Stroke
Effect of an Oral Health Programme on Oral Health, Oral Intake, and Nutrition in Patients with Stroke and Dysphagia in Taiwan: A Randomised Controlled Trial
Abstract
No previous studies have evaluated an oral health programme, before swallowing therapy, in patients with stroke and dysphagia in Taiwan. This randomised controlled trial evaluated the effect of an oral health programme (i.e., sputum assessment, Bass method-based tooth brushing, and tooth coating with fluoride toothpaste) before swallowing therapy. Sixty-six patients with stroke (23 female, 43 male) in our rehabilitation ward, who underwent nasogastric tube insertion, were assigned randomly to an oral care group (n = 33) and a control group (n = 33). Demographic data, oral health assessment, Functional Oral Intake Scale (FOIS) scores, Mini-Nutritional Assessment-Short Form (MNA-SF) scores, and nasogastric tube removal rates were compared between groups. We evaluated outcomes using generalised estimating equation analysis. Three weeks post-implementation, the oral care group had significant oral health improvements relative to the control group (95% CI =-2.69 to -1.25, Wald χ2 = 29.02, p < 0.001). There was no difference in the FOIS (95% CI = -0.16 to 0.89, Wald χ2 = 1.86, p > 0.05), MNA-SF (95% CI = -0.35 to 0.53, Wald χ2 =-0.17, p > 0.05), and nasogastric tube removal (p > 0.05) between groups. The oral care group had a higher, but non-significant FOIS score (3.94 vs 3.52) (p > 0.05). Routine oral health programmes implemented during stroke rehabilitation in patients with dysphagia may promote oral health and maintain oral intake.
Nutrition program selection in acute ischemic stroke patients with GI hemorrhage
Abstract
Background and objectives: The severity of neurologic impairment is significantly associated with gastrointestinal (GI) hemorrhage. Therefore, the aim of this study was to compare the effect of two nutritional interventions in acute ischemic stroke patients with GI hemorrhage.
Methods and study design: We retrospectively studied consecutive ischemic stroke patients with GI hemorrhage from January 2014 to December 2018. They were stratified into two programs of nutritional therapy after GI hemorrhage: moderate feeding (more than 70% optimal caloric uptake, 50-100 mL/h) and trophic feeding (16-25% of the target energy expenditure, 25 kcal/kg per day, 10- 30 mL/h) with supplemental parenteral nutrition.
Results: The group receiving moderate feeding included 30 patients, and the group receiving trophic feeding and supplemental parenteral nutrition included 32 patients. There was no statistically significant difference between the two groups in the baseline characteristics of the patients. Mortality, Glasgow Coma Scale (GCS) score at discharge, and Glasgow Outcome Scale (GOS) score 3 months after discharge were compared between the two groups. In the moderate feeding group, the overall mortality was significantly lower than in the trophic feeding and supplemental parenteral nutrition group (p<0.05). Conscious state and neurological severity were assessed by the GCS score before discharge, and the score was higher in the moderate feeding group than in the other group (p<0.05). The GOS score 3 months after discharge was higher in the moderate feeding group than in the trophic feeding and supplemental parenteral nutrition group (p<0.05). These three items showed that moderate feeding led to a better prognosis: lower occurrence of mortality, higher GCS score at discharge, and higher GOS score 3 months after discharge.
Conclusions: This study showed that moderate feeding had a much more profound effect on the outcomes than trophic feeding and supplemental parenteral nutrition, as it was associated with lower mortality, higher GCS score at discharge, and higher GOS score 3 months after discharge.
Meta-Analysis of Potassium Intake and the Risk of Stroke
Abstract
Background: The possibility that lifestyle factors such as diet, specifically potassium intake, may modify the risk of stroke has been suggested by several observational cohort studies, including some recent reports. We performed a systematic review and meta-analysis of existing studies and assessed the dose-response relation between potassium intake and stroke risk.
Methods and results: We reviewed the observational cohort studies addressing the relation between potassium intake, and incidence or mortality of total stroke or stroke subtypes published through August 6, 2016. We carried out a meta-analysis of 16 cohort studies based on the relative risk (RR) of stroke comparing the highest versus lowest intake categories. We also plotted a pooled dose-response curve of RR of stroke according to potassium intake. Analyses were performed with and without adjustment for blood pressure. Relative to the lowest category of potassium intake, the highest category of potassium intake was associated with a 13% reduced risk of stroke (RR=0.87, 95% CI 0.80-0.94) in the blood pressure-adjusted analysis. Summary RRs tended to decrease when original estimates were unadjusted for blood pressure. Analysis for stroke subtypes yielded comparable results. In the spline analysis, the pooled RR was lowest at 90 mmol of potassium daily intake (RRs=0.78, 95% CI 0.70-0.86) in blood pressure-adjusted analysis, and 0.67 (95% CI 0.57-0.78) in unadjusted analysis.
Conclusions: Overall, this dose-response meta-analysis confirms the inverse association between potassium intake and stroke risk, with potassium intake of 90 mmol (≈3500 mg)/day associated with the lowest risk of stroke.
Optimizing early enteral nutrition in severe stroke (OPENS): protocol for a multicentre randomized controlled trial
Abstract
Background: Malnutrition is one of the crucial factors associated with poor prognosis in critical ill patients, yet a significant evidence gap surrounds the management of initial enteral feeding in severe stroke. The Optimizing Early Enteral Nutrition in Severe Stroke (OPENS) trial will compare a strategy of modified full enteral nutrition (EN) (standard full EN in conjunction with prokinetic drug) and a strategy of permissive underfeeding (40 to 60% of estimated caloric requirements) with standard full EN (advancement to target nutrition goals) in patients with severe stroke.
Methods: The OPENS trial is a multicenter randomized controlled study. A total of 600 adult patients with severe stroke will be enrolled in 12 study sites in China, and randomized to standard full EN, modified full EN, or permissive underfeeding. The primary outcome measurement is the proportion of participants with a poor outcome (modified Rankin Scale ≥3) at day 90 of enrollment. Secondary outcomes include incidence rates of complications during hospitalization, disability at hospital discharge, and the ability of activities of daily living at day 90 of enrollment. The relationship between intervention and the primary outcome will be analyzed using multivariate logistic regression adjusted for study site, demographics, and baseline characteristics.
Discussion: The OPENS trial will explore the optimum initial feeding strategy for acute severe stroke. This trial is, therefore, an important step in bridging the evidence gap surrounding the enteral feeding for patients with severe stroke during the first week of hospitalization.
[How is the patient’s nutrition after a stroke?]
Abstract
Neurological conditions usually cause altered levels of consciousness or swallowing mechanisms which make artificial nutritional support necessary. International guidelines recommend nutritional screening to detect malnutrition in patients with neurological diseases. Dysphagia is a common problem after a stroke, however, it is a treatable pathology, and swallowing rehabilitation allows for improving patients’ nutritional status. Awareness of this problem is required among healthcare professionals both for its diagnosis and for the implementation of nutritional intervention measures. Patients should be tested for dysphagia within the first 24 hours of the stroke onset; this swallowing assessment as well as malnutrition screening should never be delayed by more than 72 hours. The present study addresses diagnostic and therapeutic approaches, the indications of the different nutritional treatments available and the transition to oral feeding in patients who have had a stroke episode.
The Use of Enteral Nutrition in the Management of Stroke
Abstract
This article discusses the use of enteral nutrition in the management of stroke. Stroke is a major source of disability, including dysphagia. The clinical manifestation of swallowing difficulties in stroke patients may lead to malnutrition which has implications for health status and clinical outcomes including morbidity, mortality and cost to the health service. The prevalence of malnutrition following an acute stroke could range from 8% to 34%. Therefore, the need to develop and implement the use of enteral nutrition support in stroke patients becomes pertinent. A range of enteral feeding tubes and feeding methods may be used to support stroke patients who are unable to meet their nutritional requirements through oral intake alone, although each of these approaches has its merits and limitations. Based on this review, there is evidence that enteral nutrition support is a useful method of providing nutrition for patients with dysphagia following a stroke in order to enhance their nutritional status and promote their health. However, there are challenges in the use of enteral tube feeding in these patients.
Reliability and Validity of Simple Stroke Food Frequency Questionnaire (SS-FFQ) for Nutrition Monitoring in Patients with Acute Ischemic Stroke
Abstract
Objectives Standard dietary questionnaires may have some limitations in cases with stroke, particularly in those suffering from language and communication difficulties. The present study aimed to develop a dietary questionnaire appropriate for patients with acute ischemic stroke (AIS).
Materials and Methods Major food groups (n = 19) were first identified using the dietary questionnaire of the INTERHEART study. Using the Food Frequency Questionnaire (FFQ), an expert dietitian and a vascular neurologist then selected a total number of 68 corresponding food items from 168 available FFQ items. In the next phase, a panel of expert dietitians (n = 10) assessed the face validity and the content validity of these 68 items and approved a total number of 62 items for the final questionnaire, namely, the Simple Stroke FFQ (SS-FFQ). Employing test-retest method, the intraclass correlation (ICC) of the SS-FFQ was subsequently calculated in 30 randomly selected cases affected with AIS. Ultimately, principal component analysis (PCA) was utilized for 153 cases with AIS to assess the construct validity of the questionnaire concerned. The SPSS Statistics software (version 18: SPSS Inc., Chicago, Illinois, United States) as well as descriptive tests including mean and percentage were additionally used to account for the baseline characteristics of the study participants.
Results The results revealed that the reliability of the newly developed form of the SS-FFQ was perfect (ICC = 0.86). Dietary conditions were further assessed administering the SS-FFQ on 153 cases of AIS with the mean age of 63.76 ± 15.93 years. The PCA results also showed that 15 extracted items of the given questionnaire could explain 73.10% of total item variance.
Conclusions It was concluded that the SS-FFQ was a valid and reliable questionnaire to assess nutrient intakes among patients with AIS.
Risk Factors Influencing Stroke : using data from the 7th(2016-2018) Korea National Health and Nutrition Examination Survey
Abstract
The purpose of this study was to identify the risk factors influencing stroke. The research method was used two-stage stratified cluster sampling using data from the National Health and Nutrition Survey (2016-2018). This study subjects performed a complex sample logistic regression analysis on adults aged 19 or older. Risk factors affecting stroke were shown as follows: in age groups, odds ratio were conformed when people are in their 70s, the rate is 8.861 times higher; when they are in their subjective health conditions, the odds ratio are 4.501 times higher in the bad groups; odds ratio was 3.158 times higher in the group diagnosed with hypertension and 1.598 times higher in the group diagnosed with diabetes. The result of this study found that chronic diseases such as high blood pressure and diabetes and the management of senior citizens are important because stroke is dangerous and can be managed through prevention.
Health-related quality of life and related factors in stroke survivors: Data from Korea National Health and Nutrition Examination Survey (KNHANES) 2008 to 2014
Abstract
As persons with stroke are surviving longer, monitoring and managing their quality of life is becoming important. We reviewed the Korea National Health and Nutrition Examination Survey (KNHANES) in order to evaluate the health-related quality of life (HRQoL) in stroke survivors as measured by the Euro Quality of Life-5D (EQ-5D), and to find out influencing factors. A total of 42,500 subjects were enrolled in the KNHANES, and 575 of them were persons with stroke. The EQ-5D index was lower in persons with stroke than those without stroke, when adjusted for age and sex (with stroke: 0.757±0.012, without stroke: 0.948±0.001, p < .0001). Dimension-specific influencing factors of HRQoL were observed in persons with stroke; mobility problems increased with old age; self-care problems increased with old age and depression; usual activity problems increased with old age, low income, absence of economic activity, and depression; pain/discomfort problems increased with low income. The EQ-5D index was lower in stroke survivors with older age, hypertension, diabetes mellitus, and lack of regular exercise. This is the first study to utilize nationally representative data of the Korean population to investigate the effect of stroke on HRQoL and explore the dimension-specific influencing factors. Further development of rehabilitative interventions for post-stroke depression, vocational rehabilitation, and tailored programs for encouraging physical activity may be needed to improve the HRQoL in Korean stroke survivors.
Diet and primary prevention of stroke: Systematic review and dietary recommendations by the ad hoc Working Group of the Italian Society of Human Nutrition
Abstract
Background and aims
To systematically review the latest evidence on established and emerging nutrition-related risk factors for incidence of and mortality from total,
ischemic and haemorrhagic strokes
.
The present review was conducted in the framework of the work carried out through 2015 and 2016 for the preparation of the Italian Guidelines for the Prevention and Treatment of Stroke, 8th Edition, by ISO-SPREAD (Italian Stroke Organization and the Stroke Prevention and Educational Awareness Diffusion).
Methods and results
Systematic review of articles focused on primary prevention of stroke published between January 2013 to May 2016 through an extensive search of the literature using MEDLINE/PUBMED, EMBASE and the Cochrane Library. Articles were ranked according to the SIGN methodology while the GRADE system was used to establish the strength of recommendations.
As a result of our literature search, we examined 87 meta-analyses overall (mainly of prospective studies), a few isolated more recent prospective studies not included in the meta-analyses, and a smaller number of available randomized controlled trials and case–control studies. Based on the analysis of the above articles, 36 Syntheses of the available evidence and 36 Recommendations were eventually prepared.
The present document was developed by organizing the available evidence into three individual areas (nutrients, food groups and dietary patterns) to provide a systematic and user-friendly overview of the available evidence on the relationship between
nutrition
and primary prevention of stroke. Yet analysis of foods and food patterns allowed translating the information about nutrients in a tool more amenable to use in daily life also in the light of the argument that people eat foods rather than nutrients.
Conclusions
The present literature review and dietary recommendations provide healthcare professionals and all interested readers with a useful overview for the reduction of the risk of total, ischemic and haemorrhagic stroke through dietary modifications.
Malnutrition risk predicts recovery of full oral intake among older adult stroke patients undergoing enteral nutrition: Secondary analysis of a multicentre survey (the APPLE study)
Summary
Background & aims
Whether
malnutrition
risk correlates with recovery of swallowing function of convalescent stroke patients is unknown. This study was conducted to clarify whether malnutrition risks predict achievement of full oral intake in convalescent stroke patients undergoing
enteral nutrition
.
Methods
We conducted a secondary analysis of 466 convalescent stroke patients, aged 65 years or over, who were undergoing enteral nutrition. Patients were extracted from the “Algorithm for Post-stroke Patients to improve oral intake Level; APPLE” study database compiled at the Kaifukuki (convalescent) rehabilitation wards. Malnutrition risk was determined by the Geriatric Nutritional Risk Index as follows: severe (<82), moderate (82 to <92), mild (92 to <98), and no malnutrition risks (≥98). Swallowing function was assessed by Fujishima's swallowing grade (FSG) on admission and discharge. The primary outcome was achievement of full oral intake, indicated by FSG ≥ 7. Binary
logistic regression analysis
was performed to identify
predictive factors
, including malnutrition risk, for achieving full oral intake. Estimated hazard risk was computed by Cox's hazard model.
Results
Of the 466 individuals, 264 were ultimately included in this study. Participants with severe malnutrition risk showed a significantly lower proportion of achievement of full oral intake than lower severity groups (P = 0.001). After adjusting for potential confounders, binary logistic regression analysis showed that patients with severe malnutrition risk were less likely to achieve full oral intake (adjusted odds ratio: 0.232, 95% confidence interval [95% CI]: 0.047–1.141). Cox's
proportional hazard model
revealed that severe malnutrition risk was an independent predictor of full oral intake (adjusted hazard ratio: 0.374, 95% CI: 0.166–0.842). Compared to patients who did not achieve full oral intake, patients who achieved full oral intake had significantly higher
energy intake
, but there was no difference in
protein intake
and
weight change
.
Conclusion
Severe malnutrition risk independently predicts the achievement of full oral intake in convalescent stroke patients undergoing enteral nutrition.
Selenium Drives a Transcriptional Adaptive Program to Block Ferroptosis and Treat Stroke
Abstract
Ferroptosis, a non-apoptotic form of programmed cell death, is triggered by oxidative stress in cancer, heat stress in plants, and hemorrhagic stroke. A homeostatic transcriptional response to ferroptotic stimuli is unknown. We show that neurons respond to ferroptotic stimuli by induction of selenoproteins, including antioxidant glutathione peroxidase 4 (GPX4). Pharmacological selenium (Se) augments GPX4 and other genes in this transcriptional program, the selenome, via coordinated activation of the transcription factors TFAP2c and Sp1 to protect neurons. Remarkably, a single dose of Se delivered into the brain drives antioxidant GPX4 expression, protects neurons, and improves behavior in a hemorrhagic stroke model. Altogether, we show that pharmacological Se supplementation effectively inhibits GPX4-dependent ferroptotic death as well as cell death induced by excitotoxicity or ER stress, which are GPX4 independent. Systemic administration of a brain-penetrant selenopeptide activates homeostatic transcription to inhibit cell death and improves function when delivered after hemorrhagic or ischemic stroke.
Keywords: GPX4; adaptation; cell death; ferroptosis; intracerebral hemorrhage; selenium; selenoprotein; stroke; therapeutic peptides; transcription.
Dietary and blood selenium are inversely associated with the prevalence of stroke among Inuit in Canada
Abstract
Inuit in Canada have high selenium intake from the consumption of country food such as fish and marine mammals. The health consequence is not known. This study examines the association between blood selenium concentration and prevalence of stroke among Canadian Inuit. The International Polar Year Inuit Health Survey was conducted in 2007-2008. Among the 2077 adults participants (≥18years old) who completed a questionnaire and gave blood samples, 49 stroke cases were reported, 31 of which were from women. The crude prevalence of stroke was 2.4% in the participants. Participants with stroke had lower blood selenium (geometric mean: 260μg/L vs. 319μg/L) and dietary selenium (144μg/day vs. 190μg/day) compared to individuals without stroke. Participants with high blood/dietary selenium exposure (quartiles 3 and 4) had a lower prevalence of stroke compared to those with low selenium exposure (quartile 1). The adjusted odds ratio ranged from 0.09 to 0.25 among subgroups (e.g. age, sex, and blood mercury). An L-shaped relationship between prevalence of stroke with blood and dietary selenium was observed, based on the cubic restricted spline and segmented regression analyses. The estimated turning points of the L-shaped curve for blood selenium and dietary selenium were 450μg/L and 350μg/day, respectively. Below the turning points, it was estimated that each 50-μg/L increase in blood selenium was associated with a 38% reduction in the prevalence of stroke, and each 50-μg/day increase in dietary selenium was associated with a 30% reduction in the prevalence of stroke. In conclusion, blood and dietary selenium are reversely associated with the prevalence of stroke in Inuit, which follows an L-shaped relationship. Whether this relationship applies to other population needs further investigation.
Keywords: Cross-sectional study; Daily selenium intake; Inuit; Stroke; Whole blood selenium.
Can dietary saturated fat be beneficial in prevention of stroke risk? A meta-analysis
Abstract
We conducted a meta-analysis to summarize available evidence regarding the relation between saturated fatty acid (SFA) intake and stroke risk. We searched multiple electronic databases through February 2016. Log relative risks (RRs) with 95 % confidence intervals (CIs) of the highest versus the lowest for cohort studies were weighed by the inverse variance method to obtain combined RRs. 15 prospective studies including 476,569 individuals and 11,074 strokes were included. Higher SFA intake was associated with reduced overall stroke risk [RR = 0.89 (95 % CI 0.82-0.96)] and fatal stroke risk [RR = 0.75 (95 % CI 0.59-0.94)]. Subgroup analysis indicated that higher SFA intake was associated with reduced stroke risks for East-Asians [RR = 0.79 (95 % CI 0.69-0.90)], for dose <25 g/day [RR = 0.81 (95 % CI 0.71-0.92)], for males [RR = 0.85 (95 % CI 0.75-0.96)], and for individuals with body mass index (BMI) <24 [RR = 0.75 (95 % CI 0.65-0.87)], but not for non East-Asians, females, and individuals with dose ≥25 g/day and BMI ≥24. This meta-analysis reveals that higher SFA intake is inversely associated with risk of stroke morbidity and mortality with race, sex, and BMI as key factors influencing this risk. There seems to be a threshold of SFA intake for inverse relation of SFA intake with stroke. However, the stroke-reducing or -increasing effects for specific subtypes and specific food sources of SFA can be concealed. Functions of specific subtypes of SFA (e.g. lignoceric acid) and specific food sources of SFA (i.e. plant vs. animal) in relation to stroke need to be clarified in further studies.
Keywords: Dietary; Prevention; Risk; Saturated fatty acids; Stroke.
Saturated Fat Consumption and Risk of Coronary Heart Disease and Ischemic Stroke: A Science Update
Abstract
At a workshop to update the science linking saturated fatty acid (SAFA) consumption with the risk of coronary heart disease (CHD) and ischemic stroke, invited participants presented data on the consumption and bioavailability of SAFA and their functions in the body and food technology. Epidemiological methods and outcomes were related to the association between SAFA consumption and disease events and mortality. Participants reviewed the effects of SAFA on CHD, causal risk factors, and surrogate risk markers. Higher intakes of SAFA were not associated with higher risks of CHD or stroke apparently, but studies did not take macronutrient replacement into account. Replacing SAFA by cis-polyunsaturated fatty acids was associated with significant CHD risk reduction, which was confirmed by randomized controlled trials. SAFA reduction had little direct effect on stroke risk. Cohort studies suggest that the food matrix and source of SAFA have important health effects.
Association between omega-3 fatty acid supplementation and risk of major cardiovascular disease events: a systematic review and meta-analysis
Abstract
Context: Considerable controversy exists regarding the association of omega-3 polyunsaturated fatty acids (PUFAs) and major cardiovascular end points.
Objective: To assess the role of omega-3 supplementation on major cardiovascular outcomes.
Data sources: MEDLINE, EMBASE, and the Cochrane Central Register of Controlled Trials through August 2012.
Study selection: Randomized clinical trials evaluating the effect of omega-3 on all-cause mortality, cardiac death, sudden death, myocardial infarction, and stroke.
Data extraction: Descriptive and quantitative information was extracted; absolute and relative risk (RR) estimates were synthesized under a random-effects model. Heterogeneity was assessed using the Q statistic and I2. Subgroup analyses were performed for the presence of blinding, the prevention settings, and patients with implantable cardioverter-defibrillators, and meta-regression analyses were performed for the omega-3 dose. A statistical significance threshold of .0063 was assumed after adjustment for multiple comparisons.
Data synthesis: Of the 3635 citations retrieved, 20 studies of 68,680 patients were included, reporting 7044 deaths, 3993 cardiac deaths, 1150 sudden deaths, 1837 myocardial infarctions, and 1490 strokes. No statistically significant association was observed with all-cause mortality (RR, 0.96; 95% CI, 0.91 to 1.02; risk reduction [RD] -0.004, 95% CI, -0.01 to 0.02), cardiac death (RR, 0.91; 95% CI, 0.85 to 0.98; RD, -0.01; 95% CI, -0.02 to 0.00), sudden death (RR, 0.87; 95% CI, 0.75 to 1.01; RD, -0.003; 95% CI, -0.012 to 0.006), myocardial infarction (RR, 0.89; 95% CI, 0.76 to 1.04; RD, -0.002; 95% CI, -0.007 to 0.002), and stroke (RR, 1.05; 95% CI, 0.93 to 1.18; RD, 0.001; 95% CI, -0.002 to 0.004) when all supplement studies were considered.
Conclusion: Overall, omega-3 PUFA supplementation was not associated with a lower risk of all-cause mortality, cardiac death, sudden death, myocardial infarction, or stroke based on relative and absolute measures of association.
Fatty acid transporting proteins: Roles in brain development, aging, and stroke
Abstract
Polyunsaturated fatty acids are required for the brain development and significantly impact aging and stroke. Due to the hydrophobicity of fatty acids, fatty acids transportation related proteins that include fatty acid binding proteins (FABPs), long chain acyl-coA synthase (ACS), fatty acid transportation proteins (FATPs), fatty acid translocase (FAT/CD36) and newly reported major facilitator superfamily domain-containing protein (Mfsd2a) play critical roles in the uptake of various fatty acids, especially polyunsaturated fatty acids. They are not only involved in neurodevelopment, but also have great impact on neurological disease, such as aging related dementia and stroke.
Mediterranean diet: The role of long-chain ω-3 fatty acids in fish; polyphenols in fruits, vegetables, cereals, coffee, tea, cacao and wine; probiotics and vitamins in prevention of stroke, age-related cognitive decline, and Alzheimer disease
Abstract
The mechanisms of action of the dietary components of the Mediterranean diet are reviewed in prevention of cardiovascular disease, stroke, age-associated cognitive decline and Alzheimer disease. A companion article provides a comprehensive review of extra-virgin olive oil. The benefits of consumption of long-chain ω-3 fatty acids are described. Fresh fish provides eicosapentaenoic acid while α-linolenic acid is found in canola and soybean oils, purslane and nuts. These ω-3 fatty acids interact metabolically with ω-6 fatty acids mainly linoleic acid from corn oil, sunflower oil and peanut oil. Diets rich in ω-6 fatty acids inhibit the formation of healthier ω-3 fatty acids. The deleterious effects on lipid metabolism of excessive intake of carbohydrates, in particular high-fructose corn syrup and artificial sweeteners, are explained. The critical role of the ω-3 fatty acid docosahexaenoic acid in the developing and aging brain and in Alzheimer disease is addressed. Nutritional epidemiology studies, prospective population-based surveys, and clinical trials confirm the salutary effects of fish consumption on prevention of coronary artery disease, stroke and dementia. Recent recommendations on fish consumption by pregnant women and potential mercury toxicity are reviewed. The polyphenols and flavonoids of plant origin play a critical role in the Mediterranean diet, because of their antioxidant and anti-inflammatory properties of benefit in type-2 diabetes mellitus, cardiovascular disease, stroke and cancer prevention. Polyphenols from fruits and vegetables modulate tau hyperphosphorylation and beta amyloid aggregation in animal models of Alzheimer disease. From the public health viewpoint worldwide the daily consumption of fruits and vegetables has become the main tool for prevention of cardiovascular disease and stroke. We review the important dietary role of cereal grains in prevention of coronary disease and stroke. Polyphenols from grapes, wine and alcoholic beverages are discussed, in particular their effects on coagulation. The mechanisms of action of probiotics and vitamins are also included.
Keywords: Alzheimer disease; B-vitamins; Cacao; Cardiovascular disease; Cereals; Cerebrovascular disease; Cobalamin; Coffee; DASH diet; Fish consumption; Fruits; Legumes; Mediterranean diet; Omega-3 fatty acids; Polyphenols; Prevention; Probiotics; Stroke; Tea; Vascular cognitive impairment; Vascular dementia; Vegetables; Wine; Yogurt.
B-vitamin and choline supplementation increases neuroplasticity and recovery after stroke
Abstract
Folates are B-vitamins that play an important role in brain function. Dietary and genetic deficiencies in folate metabolism result in elevated levels of homocysteine which have been linked to increased risk of developing a stroke. Reducing levels of homocysteine before or after a stroke through B-vitamin supplementation has been a focus of many clinical studies, however, the results remain inconsistent. Animal model systems provide a powerful mechanism to study and understand functional impact and mechanisms through which supplementation affects stroke recovery. The aim of this study was to understand the role of B-vitamins in stroke pathology using in vivo and in vitro mouse models. The first objective assessed the impact of folate deficiency prior to ischemic damage followed by B-vitamins and choline supplementation. Ischemic damage targeted the sensorimotor cortex. C57Bl/6 wild-type mice were maintained on a folic acid deficient diet for 4weeks prior to ischemic damage to increased levels of plasma homocysteine, a risk factor for stroke. Post-operatively mice were placed on a B-vitamin and choline supplemented diet for a period of four weeks, after which motor function was assessed in mice using the rotarod, ladder beam and forepaw asymmetry tasks. The second objective was to determine how a genetic deficiency in methylenetetrahydrofolate reductase (MTHFR), an enzyme involved in folate metabolism, increases vulnerability to stroke. Primary cortical neurons were isolated from Mthfr+/+, Mthfr+/- and Mthfr-/- embryos and were exposed to in vitro models of stroke which include hypoxia or oxygen glucose deprivation. Cell viability was measured 24-h after exposure stroke like conditions in vitro. In supplemented diet mice, we report improved motor function after ischemic damage compared to mice fed a control diet after ischemic damage. Within the perilesional cortex, we show enhanced proliferation, neuroplasticity and anti-oxidant activity in mice fed the supplemented diet. A genetic MTHFR deficiency resulted in neurodegeneration after exposure to in vitro models of stroke, by activating apoptosis promoting p53-dependent mechanisms. These results suggest that one-carbon metabolism plays a significant role in recovery after stroke and MTHFR deficiency contributes to poor recovery from stroke.
Keywords: Cerebral ischemia; Cortical plasticity; Folate; Homocysteine; Methylenetetrahydrfolate reductase.
Vitamin D and cardiovascular disease: From atherosclerosis to myocardial infarction and stroke
Abstract
There continues to be interest in understanding the role of vitamin D in the pathogenesis, epidemiology and prevention of cardiovascular disease (CVD). In fact vitamin D deficiency has been associated to an increased risk of developing CVD given to the relationship between low vitamin D levels and obesity, diabetes mellitus, dyslipidaemia, endothelial dysfunction and hypertension. However, although vitamin D has been identified as a potentially important marker of CVD, the mechanisms through which vitamin D deficiency leads from endothelial dysfunction to myocardial infarction and stroke are not fully understood. Thus, the goal of this review is to provide an updated review of the literature on the basic science of how vitamin D may affect the cardiovascular system and in particular to analyze the role that vitamin D may have in the whole dynamic process from the initiation of endothelial dysfunction to the development of myocardial infarction and stroke.
Keywords: Atherosclerosis; Environment; Lifestyle; Myocardial infarction; Stroke; Vitamin D.
Metabolic vitamin B12 deficiency: a missed opportunity to prevent dementia and stroke
Abstract
The purpose of this narrative review is to highlight insights into the importance and frequency of metabolic vitamin B12 (B12) deficiency, reasons why it is commonly missed, and reasons for the widespread but mistaken belief that treatment of B12 deficiency does not prevent stroke or improve cognitive function. Metabolic B12 deficiency is common, being present in 10%-40% of the population; is frequently missed; is easily treated; and contributes importantly to cognitive decline and stroke in older people. Measuring serum B12 alone is not sufficient for diagnosis; it is necessary to measure holotranscobalamin or functional markers of B12 adequacy such as methylmalonic acid or plasma total homocysteine. B-vitamin therapy with cyanocobalamin reduces the risk of stroke in patients with normal renal function but is harmful (perhaps because of thiocyanate accumulation from cyanide in cyanocobalamin) in patients with renal impairment. Methylcobalamin may be preferable in renal impairment. B12 therapy slowed gray matter atrophy and cognitive decline in the Homocysteine and B Vitamins in Cognitive Impairment Trial. Undiagnosed metabolic B12 deficiency may be an important missed opportunity for prevention of dementia and stroke; in patients with metabolic B12 deficiency, it would be prudent to offer inexpensive and nontoxic supplements of oral B12, preferably methylcobalamin or hydroxycobalamin. Future research is needed to distinguish the effects of thiocyanate from cyanocobalamin on hydrogen sulfide, and effects of treatment with methylcobalamin on cognitive function and stroke, particularly in patients with renal failure.
Keywords: Cobalamin; Cognitive function; Cyanide; Homocysteine; Renal impairment; Stroke; Vitamin B12.
Is Ischemic Stroke Risk Related to Folate Status or Other Nutrients Correlated With Folate Intake?
Abstract
Background and Purpose— Folate status was inversely associated with plasma homocysteine concentration, a potential risk factor of cardiovascular disease. However, it is uncertain whether folate is causally associated with risk of ischemic stroke (IS). We aimed to examine the association between IS incidence and folate intake, biochemical folate status, and folate associated nutrients.
Methods— Information on baseline characteristics and food frequency questionnaire was collected in 1990 to 1993 and included for analyses data from 1772 adults over 40 years, who were free of stroke and cancer at baseline from the CardioVascular Disease risk FACtor Two-township Study. Multivariate Cox proportional hazard model was used to relate baseline nutrient status with IS event.
Results— Over an average of 10.6 years of follow-up, 132 incident IS events were documented. Low folate intake (1st and 2nd quartiles) was significantly and independently associated with increased IS risk (HR=1.61; 95% CI: 1.04 to 2.48 and HR=1.82; 95% CI: 1.20 to 2.76) compared with those in the 3rd and 4th quartile combined, whereas no association was observed for plasma folate concentration. On the other hand, several nutrients correlated with dietary folate: vitamin B2, potassium, iron, vitamin A of plant origin, calcium were also associated with IS risk in an inverse linear manner with HR ranging from 1.5 to 1.9 for the first quartile.
Conclusions— The protective association of dietary folate on IS risk may be in part through that of other correlated nutrients or other dietary components.
Consumption of nuts and legumes and risk of incident ischemic heart disease, stroke, and diabetes: a systematic review and meta-analysis
ABSTRACT
Background: Relations between the consumption of nuts and legumes and risk of ischemic heart disease (IHD), stroke, and diabetes have not been well established.
Objective: We systematically investigated and quantified associations of nut and legume consumption with incident IHD, stroke, and diabetes.
Design: We systematically searched multiple databases to identify randomized controlled trials or observational studies that examined the relations. Studies were excluded if they reported only intermediate physiologic measures, soft cardiovascular outcomes, or crude risk estimates. Data were extracted independently and in duplicate. We assessed pooled dose-response relations by using a generalized least-squares trend estimation, and prespecified sources of heterogeneity were assessed by using metaregression. The potential for publication bias was explored by using funnel plots, Begg’s and Egger’s tests, and Duval and Tweedie trim-and-fill methods.
Results: Of 3851 abstracts, 25 observational studies (23 prospective and 2 retrospective studies) and 2 trial reports met inclusion criteria and comprised 501,791 unique individuals and 11,869 IHD, 8244 stroke, and 14,449 diabetes events. The consumption of nuts was inversely associated with fatal IHD (6 studies; 6749 events; RR per 4 weekly 28.4-g servings: 0.76; 95% CI: 0.69, 0.84; I2 = 28%), nonfatal IHD (4 studies; 2101 events; RR: 0.78; 0.67, 0.92; I2 = 0%), and diabetes (6 studies; 13,308 events; RR: 0.87; 0.81,0.94; I2 = 22%) but not stroke (4 studies; 5544 events). Legume consumption was inversely associated with total IHD (5 studies; 6514 events; RR per 4 weekly 100-g servings: 0.86; 0.78, 0.94; I2 = 0%) but not significantly associated with stroke (6 studies; 6690 events) or diabetes (2 studies; 2746 events). A meta-regression did not identify the effect modification by age, duration of follow-up, study location, or study quality. Mixed evidence was seen for publication bias, but analyses by using the Duval and Tweedie trim-and-fill method did not appreciably alter results.
Conclusion: This systematic review supports inverse associations between eating nuts and incident IHD and diabetes and eating legumes and incident IHD.
Inhibition of circulating immune cell activation: a molecular antiinflammatory effect of the Mediterranean diet
Abstract
Background: Adherence to the Mediterranean diet (Med-Diet) is associated with a reduced risk of cardiovascular disease (CVD). However, the molecular mechanisms involved are not fully understood.
Objective: The objective was to compare the effects of 2 Med-Diets with those of a low-fat diet on immune cell activation and soluble inflammatory biomarkers related to atherogenesis in subjects at high risk of CVD.
Design: In a controlled study, we randomly assigned 112 older subjects with diabetes or > or =3 CVD risk factors to 3 dietary intervention groups: Med-Diet with supplemental virgin olive oil (VOO), Med-Diet with supplemental nuts, and low-fat diet. Changes from baseline in cellular and serum inflammatory biomarkers were assessed at 3 mo.
Results: One hundred six participants (43% women; average age: 68 y) completed the study. At 3 mo, monocyte expression of CD49d, an adhesion molecule crucial for leukocyte homing, and of CD40, a proinflammatory ligand, decreased (P < 0.05) after both Med-Diets but not after the low-fat diet. Serum interleukin-6 and soluble intercellular adhesion molecule-1, inflammatory mediators crucial in firm adhesion of leukocytes to endothelial surfaces, decreased (P < 0.05) in both Med-Diet groups. Soluble vascular cellular adhesion molecule-1 and C-reactive protein decreased only after the Med-Diet with VOO (P < 0.05), whereas interleukin-6, soluble vascular cellular adhesion molecule-1, and soluble intercellular adhesion molecule-1 increased (P < 0.05) after the low-fat diet.
Conclusions: Med-Diets supplemented with VOO or nuts down-regulate cellular and circulating inflammatory biomarkers related to atherogenesis in subjects at high risk of CVD. The results support the recommendation of the Med-Diet as a useful tool against CVD.
Dietary fats and other nutrients on stroke
Abstract
Purpose of review
This review summarizes current epidemiologic evidence regarding the associations of dietary fat and other nutrients with risk of stroke.
Recent findings
Recent epidemiologic studies show no association of total fat intake or absolute intakes of saturated, monounsaturated, or polyunsaturated fat with risk of stroke. Data on long-chain omega-3 polyunsaturated fatty acids in relation to stroke risk are inconclusive but may favor fewer strokes in women. Insufficient evidence exists for trans fatty acids, other fatty acids, and dietary cholesterol intake. Present evidence indicates that high dietary magnesium and potassium intakes may lower the risk of stroke, whereas a high sodium (salt) intake and a low dietary vitamin D intake likely increase stroke risk. Calcium does not prevent stroke in populations with moderate-to-high calcium intakes but might play a role in populations with low calcium intakes. Supplementation with single vitamins likely has no protective effect on stroke in well nourished populations.
Summary
Available epidemiologic evidence indicates that diets high in magnesium and potassium may play a role in the prevention of stroke, whereas a high sodium intake is a risk factor. It remains unclear whether specific fatty acids, dietary cholesterol, and combinations of vitamins affect the risk of stroke.
Nutrition and the risk of stroke
Summary
Poor nutrition
in the first year of a mother's life and undernutrition in utero, infancy, childhood, and adulthood predispose individuals to stroke in later life, but the mechanism of increased stroke risk is unclear. Overnutrition also increases the risk of stroke, probably by accelerating the development of obesity, hypertension,
hyperlipidaemia
, and
diabetes
. Reliable evidence suggests that
dietary supplementation
with
antioxidant
vitamins, B
vitamins, and calcium does not reduce the risk of stroke. Less reliable evidence suggests that stroke can be prevented by diets that are prudent, aligned to the Mediterranean or DASH (Dietary Approaches to Stop Hypertension) diets, low in salt and added sugars, high in
potassium
, and meet, but do not exceed, energy requirements. Trials in progress are examining the effects of
vitamin D
and marine
omega-3 fatty acid
supplementation on incidence of stroke. Future challenges include the need to improve the quality of evidence linking many nutrients, foods, and
dietary patterns
to the risk of stroke.
The Role of Nutrition in the Risk and Burden of Stroke
The Role of Nutrition in the Risk of Stroke
Case–Control Studies
Diet quality was 1 of 10 potentially modifiable risk factors for stroke in the prospective INTERSTROKE study of 13 447 cases of acute first stroke and 13 472 age- and sex-matched controls with no history of stroke in 32 countries.
2
Diet quality was derived from the modified Alternative Healthy Eating Index, which was based on daily servings of fruits, vegetables, nuts and soy protein, fish, meat, eggs, whole grain, and fried foods. Higher modified Alternative Healthy Eating Index scores have been associated with lower risk of cardiovascular disease in previous studies.
3
In INTERSTROKE, individuals in the highest tertile for the modified Alternative Healthy Eating Index had a 40% lower odds of stroke (odds ratio, 0.60; 99% confidence interval [CI], 0.53–0.67), and individuals in the second tertile had a 23% lower odds of stroke (odds ratio, 0.77; 99% CI, 0.69–0.86), compared with those in the lowest tertile.
2
Individuals in the lowest 2 tertiles contributed substantially to the population attributable risk of stroke (population attributable risk, 23.2%; CI, 18.2–28.9) compared with the highest tertile of modified Alternative Healthy Eating Index.
2
Diet had a stronger association with stroke in individuals older than 55 years than younger.
2
There was also a qualitative difference in the direction of association between diet score and risk of stroke in south Asia compared with other regions. The lack of a reduction in risk of stroke associated with daily fruit and vegetable intake in south Asia might relate to qualitative differences in the type of fruit and vegetables consumed and methods of their preparation and quantitative differences in the volume (lower) intake of combined fruit and vegetables in south Asia compared with other regions.
2
Vitamin C intake, circulating vitamin C and risk of stroke: a meta-analysis of prospective studies
Abstract
Background: Though vitamin C supplementation has shown no observed effects on stroke prevention in several clinical trials, uncertainty remains as to whether long-term, low-dose intake influences the development of stroke among general populations. Furthermore, the association between circulating vitamin C and the risk of stroke is also unclear. For further clarification of these issues, we conducted a meta-analysis of prospective studies.
Methods and results: PubMed and EMBASE databases were searched, and the bibliographies of the retrieved articles were also reviewed to identify eligible studies. Summary relative risk (RRs) with corresponding 95% confidence intervals (CIs) were computed with a random-effects model. The summary RR for the high-versus-low categories was 0.81 (95% CI: 0.74 to 0.90) for dietary vitamin C intake (11 studies), and 0.62 (95% CI: 0.49 to 0.79) for circulating vitamin C (6 studies). The summary RR for each 100 mg/day increment in dietary vitamin C was 0.83 (95% CI: 0.75 to 0.93) (10 studies), and for each 20 μmol/L increment in circulating vitamin C was 0.81 (95% CI: 0.75 to 0.88) (5 studies). Few studies reported results for vitamin C supplements (RR for high-versus-low intake=0.83, 95% CI: 0.62 to 1.10, 3 studies).
Conclusions: This meta-analysis suggests significant inverse relationships between dietary vitamin C intake, circulating vitamin C, and risk of stroke.
Keywords: antioxidants; diet; meta‐analysis; prevention; stroke.
Sugar- and Artificially Sweetened Beverages and the Risks of Incident Stroke and Dementia
Abstract
Background and Purpose—
Sugar- and artificially-sweetened beverage intake have been linked to cardiometabolic risk factors, which increase the risk of cerebrovascular disease and dementia. We examined whether sugar- or artificially sweetened beverage consumption was associated with the prospective risks of incident stroke or dementia in the community-based Framingham Heart Study Offspring cohort.
Methods—
We studied 2888 participants aged >45 years for incident stroke (mean age 62 [SD, 9] years; 45% men) and 1484 participants aged >60 years for incident dementia (mean age 69 [SD, 6] years; 46% men). Beverage intake was quantified using a food-frequency questionnaire at cohort examinations 5 (1991–1995), 6 (1995–1998), and 7 (1998–2001). We quantified recent consumption at examination 7 and cumulative consumption by averaging across examinations. Surveillance for incident events commenced at examination 7 and continued for 10 years. We observed 97 cases of incident stroke (82 ischemic) and 81 cases of incident dementia (63 consistent with Alzheimer’s disease).
Results—
After adjustments for age, sex, education (for analysis of dementia), caloric intake, diet quality, physical activity, and smoking, higher recent and higher cumulative intake of artificially sweetened soft drinks were associated with an increased risk of ischemic stroke, all-cause dementia, and Alzheimer’s disease dementia. When comparing daily cumulative intake to 0 per week (reference), the hazard ratios were 2.96 (95% confidence interval, 1.26–6.97) for ischemic stroke and 2.89 (95% confidence interval, 1.18–7.07) for Alzheimer’s disease. Sugar-sweetened beverages were not associated with stroke or dementia.
Conclusions—
Artificially sweetened soft drink consumption was associated with a higher risk of stroke and dementia.
Hypertension
Non-pharmacological management of hypertension: in the light of current research
Abstract
Hypertension is a major risk factor for a number of cardiovascular diseases. Proper management of hypertension may require both pharmacological and non-pharmacological interventions. Non-pharmacological interventions help reduce the daily dose of antihypertensive medication and delay the progression from prehypertension to hypertension stage. Non-pharmacological interventions include lifestyle modifications like dietary modifications, exercise, avoiding stress, and minimizing alcohol consumption. Nutritional requirements of hypertensive individuals can be addressed through adopting either the DASH diet or through traditional Mediterranean diet. These dietary guidelines promote the consumption of fruits, vegetables, grains, dairy products, and food rich in K+, Mg+2, Ca+2, and phosphorus. Restriction of Na+ intake has the greatest role in lowering the blood pressure. The DASH diet alone has the effect equal to that of a single drug therapy. After dietary modifications, exercise and weight loss are the second major intervention for hypertension management. Avoiding stressful lifestyle, depression, and anxiety also help to reduce elevated blood pressure. Minimizing alcohol intake also favors the blood pressure reduction. However, lifestyle modification is a dynamic process and requires continuous adherence. It is a multi-factorial approach targeting more than one intervention. However, 6-12-month lifestyle modifications can be attempted in stage-1 hypertensive patients without any cardiovascular complication, in the hope that they may be sufficiently effective to make it unnecessary to use medicines.
Protein Nutrition and Malnutrition in CKD and ESRD
Abstract
Elevated protein catabolism and protein malnutrition are common in patients with chronic kidney disease (CKD) and end-stage renal disease (ESRD). The underlying etiology includes, but is not limited to, metabolic acidosis intestinal dysbiosis; systemic inflammation with activation of complements, endothelin-1 and renin-angiotensin-aldosterone (RAAS) axis; anabolic hormone resistance; energy expenditure elevation; and uremic toxin accumulation. All of these derangements can further worsen kidney function, leading to poor patient outcomes. Many of these CKD-related derangements can be prevented and substantially reversed, representing an area of great potential to improve CKD and ESRD care. This review integrates known information and recent advances in the area of protein nutrition and malnutrition in CKD and ESRD. Management recommendations are summarized. Thorough understanding the pathogenesis and etiology of protein malnutrition in CKD and ESRD patients will undoubtedly facilitate the design and development of more effective strategies to optimize protein nutrition and improve outcomes.
Impact of Salt Intake on the Pathogenesis and Treatment of Hypertension
Abstract
Excessive dietary salt (sodium chloride) intake is associated with an increased risk for hypertension, which in turn is especially a major risk factor for stroke and other cardiovascular pathologies, but also kidney diseases. Besides, high salt intake or preference for salty food is discussed to be positive associated with stomach cancer, and according to recent studies probably also obesity risk. On the other hand a reduction of dietary salt intake leads to a considerable reduction in blood pressure, especially in hypertensive patients but to a lesser extent also in normotensives as several meta-analyses of interventional studies have shown. Various mechanisms for salt-dependent hypertension have been put forward including volume expansion, modified renal functions and disorders in sodium balance, impaired reaction of the renin-angiotensin-aldosterone-system and the associated receptors, central stimulation of the activity of the sympathetic nervous system, and possibly also inflammatory processes.Not every person reacts to changes in dietary salt intake with alterations in blood pressure, dividing people in salt sensitive and insensitive groups. It is estimated that about 50-60 % of hypertensives are salt sensitive. In addition to genetic polymorphisms, salt sensitivity is increased in aging, in black people, and in persons with metabolic syndrome or obesity. However, although mechanisms of salt-dependent hypertensive effects are increasingly known, more research on measurement, storage and kinetics of sodium, on physiological properties, and genetic determinants of salt sensitivity are necessary to harden the basis for salt reduction recommendations.Currently estimated dietary intake of salt is about 9-12 g per day in most countries of the world. These amounts are significantly above the WHO recommended level of less than 5 g salt per day. According to recent research results a moderate reduction of daily salt intake from current intakes to 5-6 g can reduce morbidity rates. Potential risks of salt reduction, like suboptimal iodine supply, are limited and manageable. Concomitant to salt reduction, potassium intake by higher intake of fruits and vegetables should be optimised, since several studies have provided evidence that potassium rich diets or interventions with potassium can lower blood pressure, especially in hypertensives.In addition to dietary assessment the gold standard for measuring salt intake is the analysis of sodium excretion in the 24 h urine. Spot urine samples are appropriate alternatives for monitoring sodium intake. A weakness of dietary evaluations is that the salt content of many foods is not precisely known and information in nutrient databases are limited. A certain limitation of the urine assessment is that dietary sources contributing to salt intake cannot be identified.Salt reduction strategies include nutritional education, improving environmental conditions (by product reformulation and optimization of communal catering) up to mandatory nutrition labeling and regulated nutrition/health claims, as well as legislated changes in the form of taxation.Regarding dietary interventions for the reduction of blood pressure the Dietary Approaches to Stop Hypertension (DASH) diet can be recommended. In addition, body weight should be normalized in overweight and obese people (BMI less than 25 kg/m2), salt intake should not exceed 5 g/day according to WHO recommendations (<2 g sodium/day), no more than 1.5 g sodium/d in blacks, middle- and older-aged persons, and individuals with hypertension, diabetes, or chronic kidney disease, intake of potassium (~4.7 g/day) should be increased and alcohol consumption limited. In addition, regular physical activity (endurance, dynamic resistance, and isometric resistance training) is very important.
Low-Renin Hypertension
Abstract
Low-renin hypertension affects 30% of hypertensive patients. Primary hyperaldosteronism presents with low renin and aldosterone excess. Low-renin, low-aldosterone hypertension represents a wide spectrum of disorders that includes essential low-renin hypertension, hereditary forms of hypertension, and hypertension secondary to endogenous or exogenous factors. This review addresses the different conditions that present with low-renin hypertension, discussing an appropriate diagnostic approach and highlighting the genetic subtypes within familial forms.
Keywords: Apparent mineralocorticoid excess syndrome; CYP11B1 and CYP17 deficiency; Glucocorticoid-resistance syndrome; Gordon syndrome; Liddle syndrome; Low-renin hypertension; Mineralocorticoid receptor– activating mutation; Primary aldosteronism.
Role of Personalized Nutrition in Chronic-Degenerative Diseases
Abstract
Human nutrition is a branch of medicine based on foods biochemical interactions with the human body. The phenotypic transition from health to disease status can be attributed to changes in genes and/or protein expression. For this reason, a new discipline has been developed called "-omic science". In this review, we analyzed the role of "-omics sciences" (nutrigenetics, nutrigenomics, proteomics and metabolomics) in the health status and as possible therapeutic tool in chronic degenerative diseases. In particular, we focused on the role of nutrigenetics and the relationship between eating habits, changes in the DNA sequence and the onset of nutrition-related diseases. Moreover, we examined nutrigenomics and the effect of nutrients on gene expression. We perused the role of proteomics and metabolomics in personalized nutrition. In this scenario, we analyzed also how dysbiosis of gut microbiota can influence the onset and progression of chronic degenerative diseases. Moreover, nutrients influencing and regulating gene activity, both directly and indirectly, paves the way for personalized nutrition that plays a key role in the prevention and treatment of chronic degenerative diseases.
Impact of Nutrition on Pulmonary Arterial Hypertension
Abstract
Pulmonary arterial hypertension (PAH) is characterized by sustained vasoconstriction, vascular remodeling, inflammation, and in situ thrombosis. Although there have been important advances in the knowledge of the pathophysiology of PAH, it remains a debilitating, limiting, and rapidly progressive disease. Vitamin D and iron deficiency are worldwide health problems of pandemic proportions. Notably, these nutritional alterations are largely more prevalent in PAH patients than in the general population and there are several pieces of evidence suggesting that they may trigger or aggravate disease progression. There are also several case reports associating scurvy, due to severe vitamin C deficiency, with PAH. Flavonoids such as quercetin, isoflavonoids such as genistein, and other dietary polyphenols including resveratrol slow the progression of the disease in animal models of PAH. Finally, the role of the gut microbiota and its interplay with the diet, host immune system, and energy metabolism is emerging in multiple cardiovascular diseases. The alteration of the gut microbiota has also been reported in animal models of PAH. It is thus possible that in the near future interventions targeting the nutritional status and the gut dysbiosis will improve the outcome of these patients.
Diet behaviours and hypertension in US adults
the National Health and Nutrition Examination Survey 2013–2014
Abstract
Objective:
The present study aims to explore the association between ideal diet behaviours recommended by the American Heart Association (AHA) and hypertension in the United States (US) adults using data from the National Health and Nutrition Examination Survey (NHANES) 2013–2014.
Methods:
Whole grains, fruits and vegetables, fish, sodium and sugar-sweetened beverages at an ideal level were defined as the AHA's recommendation. Associations between number of ideal diet behaviours and hypertension were assessed through multivariate logistic regression models.
Results:
A total of 4462 US adult participants (2110 men and 2352 women) were included in the analysis, of whom 1516 (34.0%) were diagnosed with hypertension. The multivariate adjusted odds ratios and 95% confidence intervals (95% CIs) for hypertension in the groups with one, two and at least three ideal diet behaviours were 0.88 (0.71–1.10), 0.89 (0.70–1.12) and 0.67 (0.49–0.91), when the group with 0 ideal diet behaviour was used as the reference. Results also showed that women with three or more ideal diet behaviours had 43% (95% CI: 10–64%) lower odds of hypertension.
Conclusion:
The number of diet behaviours at the ideal level recommended by the AHA was inversely associated with hypertension in US adults.
Association between the Intake of Fermented Soy Products and Hypertension Risk in Postmenopausal Women and Men Aged 50 Years or Older: The Korea National Health and Nutrition Examination Survey 2013–2018
Abstract
Sodium intake is positively associated with hypertension risk; however, it is not clear whether there is an association between the intake of fermented soy products, a major source of salt, and blood pressure (BP). This study aimed to investigate the hypothesis that hypertension risk and BP were negatively associated with the intake of fermented soy products but not with the intake of sodium from fermented soy products. This cross-sectional study was performed using data from the Korea National Health and Nutrition Examination Survey (2013–2018). In total, 11,566 men and postmenopausal women aged ≥50 years were divided according to quintiles of sodium or fermented soy product intake. The intake of fermented soy products was negatively associated with hypertension risk (odds ratio: 0.81, 95% confidence interval: 0.66–0.98; p-trend = 0.023) and systolic BP (SBP; p-trend = 0.043) in postmenopausal women. Mediation analysis showed that the intake of fermented soy products had total and direct effects on SBP; however, there was no indirect effect because soy nutrients, such as protein, fiber, calcium, and potassium, had no significant effects on SBP. Among men, fermented soy product intake was not associated with hypertension risk and BP. Additionally, the intake of sodium from fermented soy products was not significantly associated with hypertension risk and BP in both postmenopausal women and men. This study suggests that hypertension risk and BP were not associated with the intake of sodium from fermented soy products; further, hypertension risk and BP were inversely associated with fermented soy product intake in postmenopausal women. Further clinical studies are needed to confirm the effect of fermented soy product intake on hypertension risk and BP.
Isolated systolic hypertension and central blood pressure: Implications from the national nutrition and health survey in Taiwan
AbstractWe aimed to investigate the association between isolated systolic hypertension (ISH) and central blood pressure (BP) in a nationally representative population, with a focus on the young and middle‐aged adults (<50 years old). A total of 2029 adults without taking antihypertensive medications, aged ≥ 19 years old, participated in the 2013–2016 National Nutrition and Health Survey in Taiwan. Central and brachial BP were simultaneously measured using a cuff‐based stand‐alone central blood pressure monitor purporting to measure invasive central BP (type II device). Central hypertension was defined by central systolic (SBP)/diastolic BP (DBP) ≥130 or 90 mm Hg, and ISH was defined by brachial SBP ≥ 140 and DBP < 90 mm Hg. Overall, the prevalence rates of ISH, isolated diastolic hypertension (IDH, brachial SBP < 140 and DBP ≥ 90 mmHg), and systolic/diastolic hypertension (SDH, brachial SBP ≥ 140 and DBP ≥ 90 mmHg) were 6.51%, 1.92%, and 4.34%, respectively. ISH subjects had significantly higher central pulse pressure (PP) (62.8 ± 9.7 mm Hg for age < 50 years and 72.4 ± 13.5 mmHg for age ≥ 50 years) than those subjects with either IDH (44.7 ± 10.7 and 44.9 ± 10.6 mmHg) or SDH (55.2 ± 14.0 and 62.6 ± 17.1 mmHg). All ISH adults had central hypertension, and a higher prevalence of central obesity than the normotensives (80.95% vs. 26.15%, for age < 50 years; and 63.96% vs. 43.37% for age ≥ 50 years). All untreated subjects with ISH, whether younger or older, had central hypertension and had significantly higher central PP than those with IDH or SDH. Central obesity was one of the major characteristics of ISH, especially in the young‐ and middle‐aged adults.
Treatment of Hypertension with Nutrition and Nutraceutical Supplements: Part 1
Introduction
Cardiovascular disease (CVD) remains the leading cause of death in the United States. Hypertension is one of the top five risk factors for coronary heart disease (CHD) and CVD and remains the most common reason for visits to primary care physicians, with antihypertensive drugs costing >U.S.$20 billion annually.1–19
There are >100 million people in the United States with hypertension based on new hypertension guidelines.19
In numerous clinical trials, pharmacotherapy will control blood pressure (BP) and reduce stroke, CHD, myocardial infarction (MI), congestive heart failure (CHF), and renal disease.16
,
17
However, some hypertensive patients either refuse to take drugs or prefer to treat with nutrition or nutritional supplements.1–20
Hypertension is a consequence of micro- and macronutrient insufficiencies, abnormal vascular biology, reduced bioavailability of nitric oxide (NO), and the three finite vascular responses to vascular injury: inflammation, oxidative stress, and vascular immune dysfunction with activation for cell-mediated immunity (see
Fig. 1
).2–5
,
11–14
These abnormalities coexist and interact with genetics, epigenetics, nutrient–gene expression, and other environmental and lifestyle factors.2–5
,
11–14
Hypertension is initially the expected and normal response to these infinite insults from the environment (including microbes, heavy metals, biochemical, biohumoral, and biomechanical issues, lipids, glucose, obesity, smoking, homocysteine, and many others) to the endothelium, but chronic dysregulation of this response associated with gene expression patterns leads to a complex series of vascular events in which the vascular system becomes an innocent bystander.2–5
,
11–14
Hypertension is one of several responses of the blood vessel to endothelial dysfunction (ED). Cardiac smooth-muscle and vascular dysfunction and abnormalities of both microvascular function and structure precede the development of hypertension by decades. This consequently leads to vascular and cardiac hypertrophy, remodeling, functional and structural network rarefaction, decreased vasodilatory reserve, altered media-to-lumen ratio, stiffness, loss of arterial elasticity, fibrosis, increased pulse pressure, elevated pulse wave velocity (PWV), and increased augmentation index (see
Fig. 2
).2–5
,
11–14
Significant functional and then structural microvascular impairment begins before elevations in BP in normotensive offspring of hypertensive parents.
Increasing quality of life in pulmonary arterial hypertension: is there a role for nutrition?
Pulmonary arterial hypertension (PAH) is a progressive disease primarily affecting the pulmonary vasculature and heart. PAH patients suffer from exercise intolerance and fatigue, negatively affecting their quality of life. This review summarizes current insights in the pathophysiological mechanisms underlying PAH. It zooms in on the potential involvement of nutritional status and micronutrient deficiencies on PAH exercise intolerance and fatigue, also summarizing the potential benefits of exercise and nutritional interventions. Pubmed/Medline, Scopus, and Web of Science were searched for publications on pathophysiological mechanisms of PAH negatively affecting physical activity potential and nutritional status, and for potential effects of interventions involving exercise or nutritional measures known to improve exercise intolerance. Pathophysiological processes that contribute to exercise intolerance and impaired quality of life of PAH patients include right ventricular dysfunction, inflammation, skeletal muscle alterations, and dysfunctional energy metabolism. PAH-related nutritional deficiencies and metabolic alterations have been linked to fatigue, exercise intolerance, and endothelial dysfunction. Available evidence suggests that exercise interventions can be effective in PAH patients to improve exercise tolerance and decrease fatigue. By contrast, knowledge on the prevalence of micronutrient deficiencies and the possible effects of nutritional interventions in PAH patients is limited. Although data on nutritional status and micronutrient deficiencies in PAH are scarce, the available knowledge, including that from adjacent fields, suggests that nutritional intervention to correct deficiencies and metabolic alterations may contribute to a reduction of disease burden.
Presence of Hypertension Is Reduced by Mediterranean Diet Adherence in All Individuals with a More Pronounced Effect in the Obese: The Hellenic National Nutrition and Health Survey (HNNHS)
Abstract
Hypertension is a major risk of cardiovascular diseases. This study’s aim was to examine associations between hypertension and a priori known lifestyle risk factors, including weight status and Mediterranean diet adherence. The study included a representative sample of the adult population (N = 3775 (40.8% males)), from the Hellenic National Nutrition and Health Survey (HNNHS), which took place from September 2013 to May 2015. Demographic and anthropometric data were collected using validated questionnaires, and blood pressure (BP) measurements were performed for the two main metropolitan areas (N = 1040; 41.1%). Hypertension diagnosis was according to the International Classification of Diseases (ICD-10) guidelines. Weighted proportions, extended Mantel–Haenszel (M–H) analyses, and multiple logistic regressions (for the survey data) were performed. Mean systolic BP (SBP) and diastolic BP (DBP) were 118.6 mmHg and 72.2 mmHg respectively, with both values being higher in males compared to females in all age groups (p < 0.001). Study participants with hyperlipidemia or diabetes, and those overweight, were almost twice as likely to be hypertensives, with the odds increasing to 4 for those obese (p for all, < 0.05). Stricter Mediterranean diet adherence significantly decreased the likelihood of hypertension by 36% (OR: 0.64; 95% CI: 0.439, 0.943), and a significant interaction was found between Mediterranean diet adherence and weight status on hypertension. The presence of hypertension is clustered with comorbidities, but is significantly associated with modifiable risk factors, including Mediterranean diet and weight status, underlining the need for personalized medical nutritional treatment.
Dietary Approaches to Stop Hypertension Diet, Weight Status, and Blood Pressure among Children and Adolescents: National Health and Nutrition Examination Surveys 2003-2012
Abstract
Background
The Dietary Approaches to Stop Hypertension (DASH) diet is associated with lower blood pressure and reduced risk of
cardiovascular disease
among adults, but little is known about accordance with this
dietary pattern
or health benefits among children and adolescents.
Objective
The objectives were to evaluate accordance with the
DASH diet
, differences over time, and the association with health attributes among a nationally representative sample of US children and adolescents.
Design
Cross-sectional data from the 2003-2012 National Health and
Nutrition
Examination Surveys (NHANES) were analyzed.
Participants/setting
Data from 9,793 individuals aged 8 to 18 years were examined.
Main outcome measures
DASH accordance was estimated based on nine nutrient targets: total fat,
saturated fat
, protein, cholesterol, fiber, calcium,
magnesium
,
potassium
, and sodium; possible score range is 0 to 9.
Statistical analyses performed
Accordance with the DASH diet across time was examined comparing the 2011-2012 to 2003-2004 NHANES surveys. The association between
DASH score
and weight status was examined using multinomial
logistic regression
, and the associations with
waist circumference
,
systolic blood pressure
, and
diastolic blood pressure
were examined using multivariable
linear regression
.
Results
Accordance with the DASH diet was low across the age groups, with a range of mean DASH scores from 1.48 to 2.14. There were no significant changes across time. DASH score was inversely associated with systolic blood pressure (mm Hg) among 14- to 18-year-olds (β=−.46; 95% CI −.83 to −.09) among the larger sample of participants who completed at least one dietary recall, but no significant differences were seen in other age categories. In the subsample of participants with both dietary recalls, a significant inverse association was seen between DASH score and systolic blood pressure for 11- to 13-year-olds (β=−.57; 95% CI −1.02 to −.12). There were no significant associations between this dietary pattern and weight status, waist circumference, or diastolic blood pressure.
Conclusions
Few US children and adolescents have diets that are in alignment with the DASH diet. Future research should explore strategies to encourage fruit, vegetable, and
whole-grain
consumption, as well as sodium reductions to help meet DASH nutrient targets in children and adolescents, as well as examine the potential benefits of this eating pattern on health in this population group.
Critical review of nutrition, blood pressure and risk of hypertension through the lifecycle: do B vitamins play a role?
Abstract
Hypertension is the leading cause of preventable mortality worldwide, contributing to over 9 million deaths per annum, predominantly owing to cardiovascular disease. The association of obesity, physical inactivity and alcohol with elevated blood pressure (BP) is firmly established. Weight loss or other dietary strategies, such as the Dietary Approaches to Stop Hypertension (DASH) diet, have been shown to be effective in lowering BP. Additionally, specific nutrients are recognised to contribute to BP, with higher sodium intake linked with an increased risk of hypertension, while potassium is associated with a reduced risk of hypertension. Of note, emerging evidence has identified a novel role for one-carbon metabolism and the related B vitamins, particularly riboflavin, in BP. Specifically in adults genetically at risk of developing hypertension, owing to the common C677T polymorphism in MTHFR, supplemental riboflavin (co-factor for MTHFR) was shown in randomised trials to lower systolic BP by up to 13 mmHg. A BP response to intervention of this magnitude could have important clinical impacts, given that a reduction in systolic BP of 10 mmHg is estimated to decrease stroke risk by 40%. This review aims to explore the factors contributing to hypertension across the lifecycle and to critically evaluate the evidence supporting a role for nutrition, particularly folate-related B vitamins, in BP and risk of hypertension. In addition, gaps in our current knowledge that warrant future research in this area, will be identified.
Fish and omega-3 fatty acid consumption and risk of hypertension
Abstract
Background:
Experimental studies suggest that omega-3 fatty acid have favorable effects on blood pressure (BP). However, data on the association of long-term dietary intake of omega-3 fatty acid or fish with risk of hypertension in healthy subjects are sparse. We examined whether fish or omega-3 fatty acid consumption was associated with incident hypertension in the Physicians’ Health Study (PHS).
Methods:
In a prospective cohort study, we analyzed data on 12 279 PHS participants (mean age: 53.0 ± 8.7 years) free of hypertension at baseline. Fish and omega-3 fatty acid consumption were assessed from a baseline semiquantitative food-frequency questionnaire. Incident hypertension was ascertained via self-reports on annual follow-up questionnaires.
Results:
During a mean follow-up of 15.8 years, 6299 men (51.3%) developed hypertension. In a multivariable model controlling for established risk factors for hypertension, fish and omega-3 fatty acid consumption was not significantly associated with incident hypertension. The hazard ratio (95% CI) of hypertension was 1.10 (0.93–1.30) for men who consumed at least five servings per week of fish compared with those who did not consume any fish (P for trend = 0.29). For the highest versus lowest quintile of omega-3 fatty acid intake, the hazard ratio of hypertension was 1.02 (0.94–1.11) (P for trend = 0.34). The associations did not vary by type of fish. There was also no evidence of effect modification by baseline BP, BMI, or history of hypercholesterolemia.
Conclusion:
Overall, long-term dietary intake of fish and omega-3 fatty acid was not associated with incident hypertension in a cohort of middle-aged and older US men.
Soy Protein Alleviates Hypertension and Fish Oil Improves Diastolic Heart Function in the Han:SPRD-Cy Rat Model of Cystic Kidney Disease
Abstract
Abnormalities in cardiac structure and function are very common among people with chronic kidney disease, in whom cardiovascular disease is the major cause of death. Dietary soy protein and fish oil reduce kidney disease progression in the Han:SPRD-Cy model of cystic renal disease. However, the effects of these dietary interventions in preventing alterations in cardiac structure and function due to kidney disease (reno-cardiac syndrome) in a cystic kidney disease model are not known. Therefore, weanling Han:SPRD-Cy diseased (Cy/+) and normal (+/+) rats were given diets containing either casein or soy protein, and either soy or fish oil in a three-way design for 8 weeks. Diseased rats had larger hearts, augmented left ventricular mass, and higher systolic and mean arterial blood pressure compared to the normal rats. Assessment of cardiac function using two-dimensional guided M-mode and pulse-wave Doppler echocardiography revealed that isovolumic relaxation time was prolonged in the diseased compared to normal rats, reflecting a diastolic heart dysfunction, and fish oil prevented this elevation. Soy protein resulted in a small improvement in systolic and mean arterial pressure but did not improve diastolic heart function, while fish oil prevented diastolic heart dysfunction in this model of cystic kidney disease.
Role of Magnesium Deficiency in Promoting Atherosclerosis, Endothelial Dysfunction, and Arterial Stiffening as Risk Factors for Hypertension
Abstract
Arterial hypertension is a disease with a complex pathogenesis. Despite considerable knowledge about this socially significant disease, the role of magnesium deficiency (MgD) as a risk factor is not fully understood. Magnesium is a natural calcium antagonist. It potentiates the production of local vasodilator mediators (prostacyclin and nitric oxide) and alters vascular responses to a variety of vasoactive substances (endothelin-1, angiotensin II, and catecholamines). MgD stimulates the production of aldosterone and potentiates vascular inflammatory response, while expression/activity of various antioxidant enzymes (glutathione peroxidase, superoxide dismutase, and catalase) and the levels of important antioxidants (vitamin C, vitamin E, and selenium) are decreased. Magnesium balances the effects of catecholamines in acute and chronic stress. MgD may be associated with the development of insulin resistance, hyperglycemia, and changes in lipid metabolism, which enhance atherosclerotic changes and arterial stiffness. Magnesium regulates collagen and elastin turnover in the vascular wall and matrix metalloproteinase activity. Magnesium helps to protect the elastic fibers from calcium deposition and maintains the elasticity of the vessels. Considering the numerous positive effects on a number of mechanisms related to arterial hypertension, consuming a healthy diet that provides the recommended amount of magnesium can be an appropriate strategy for helping control blood pressure.
Anti-inflammatory nutrition with high protein attenuates cardiac and skeletal muscle alterations in a pulmonary arterial hypertension model
Abstract
Pulmonary arterial hypertension (PAH) is characterized by remodelling of the pulmonary arteries and right ventricle (RV), which leads to functional decline of cardiac and skeletal muscle. This study investigated the effects of a multi-targeted nutritional intervention with extra protein, leucine, fish oil and oligosaccharides on cardiac and skeletal muscle in PAH. PAH was induced in female C57BL/6 mice by weekly injections of monocrotaline (MCT) for 8 weeks. Control diet (sham and MCT group) and isocaloric nutritional intervention (MCT + NI) were administered. Compared to sham, MCT mice increased heart weight by 7%, RV thickness by 13% and fibrosis by 60% (all p < 0.05) and these were attenuated in MCT + NI mice. Microarray and qRT-PCR analysis of RV confirmed effects on fibrotic pathways. Skeletal muscle fiber atrophy was induced (P < 0.05) by 22% in MCT compared to sham mice, but prevented in MCT + NI group. Our findings show that a multi-targeted nutritional intervention attenuated detrimental alterations to both cardiac and skeletal muscle in a mouse model of PAH, which provides directions for future therapeutic strategies targeting functional decline of both tissues.
Factors Associated With Hypertension Control in US Adults Using 2017 ACC/AHA Guidelines: National Health and Nutrition Examination Survey 1999–2016
Abstract
BACKGROUND
Factors and trends associated with hypertension control (BP < 130/80 mm Hg) and mean blood pressure (BP) among hypertensive adults (BP ≥1 30/80 mm Hg or medicated for hypertension).
METHOD
Data on 22,911 hypertensive US adults from the 1999–2016 National Health and Nutrition Examination Survey.
RESULTS
For men, hypertension control prevalence increased from 8.6% in 1999–2000 to 16.2% in 2003–2004 (P < 0.001), and continued the increasing trend afterwards to 23.2% in 2011–2012 (P < 0.001) and then plateaued. For women, hypertension control prevalence increased from 1999–2000 to 2009–2010 (10.8–26.3%, P < 0.001) and then plateaued. For men with hypertension, systolic BP decreased from 1999–2000 to 2011–2012 (135.7–132.8 mm Hg, P < 0.001) and then increased to 135.3 mm Hg in 2015–2016 (P < 0.001). For women with hypertension, systolic BP decreased from 1999–2000 to 2009–2010 (139.7–131.9 mm Hg; P < 0.001) and then increased to 134.4 mm Hg in 2015–2016 (P = 0.003). Diastolic BP decreased from 1999–2000 to 2015–2016 (men: 79.1–75.5 mm Hg and women: 76.4–73.7 mm Hg, P < 0.001 for both). In 2011–2016, hypertension control was 22.0% for men and 25.2% for women. The adjusted prevalence ratio (PR) of hypertension control were lower for non-Hispanic black men and women (PR = 0.72, 95% confidence interval (CI) = 0.61–0.86; PR = 0.83, 95% CI = 0.70–0.99, respectively; non-Hispanic white (NHW) as reference), Hispanic and non-Hispanic Asian men (PR = 0.70, 95% CI = 0.54–0.92; PR = 0.59, 95% CI = 0.39–0.86; respectively; NHW as reference).
CONCLUSION
Hypertension control significantly increased from 1999–2000 to 2011–2012 (men) and 2009–2010 (women) and then plateaued. About a quarter of US adults with hypertension were controlled in 2011–2016.
An overview of the nutrition transition in West Africa: implications for non-communicable diseases
Abstract
The nutrition landscape in West Africa has been dominated by the programmes to address undernutrition. However, with increasing urbanisation, technological developments and associated change in dietary patterns and physical activity, childhood and adult overweight, and obesity are becoming more prevalent. There is an evidence of increasing intake of dietary energy, fat, sugars and protein. There is low consumption of fruit and vegetables universally in West Africa. Overall, the foods consumed are predominantly traditional with the component major food groups within recommended levels. Most of the West African countries are at the early stages of nutrition transition but countries such as Cape Verde, Ghana and Senegal are at the latter stages. In the major cities of the region, children consume energy-dense foods such as candies, ice cream and sweetened beverages up to seven times as frequently as fruit and vegetables. Adult obesity rates have increased by 115 % in 15 years since 2004. In Ghana, the prevalence of overweight/obesity in women has increased from 12·8 % in 1993 to 29·9 % in 2008. In Accra, overweight/obesity in women has increased from 62·2 % in 2003 to 64·9 % in 2009. The age-standardised proportion of adults who engage in adequate levels of physical activity ranges from 46·8 % in Mali to 94·7 % in Benin. The lingering stunting in children and the rising overweight in adults have resulted to a dual burden of malnutrition affecting 16·2 % of mother-child pairs in Cotonou. The prevalence of hypertension has been increased and ranges from 17·6 % in Burkina Faso to 38·7 % in Cape Verde. The prevalence is higher in the cities: 40·2 % in Ougadougou, 46·0 % in St Louis and 54·6 % in Accra. The prevalence of diabetes ranges from 2·5 to 7·9 % but could be as high as 17·9 % in Dakar, Senegal. The consequences of nutrition transition are not only being felt by the persons in the high socioeconomic class, but also in cities such as Accra and Ouagadougou, where at least 19 % of adults from the poorest households are overweight and 19-28 % have hypertension. Concerted national action involving governments, partners, private sector and civil society is needed to re-orient health systems and build capacity to address the dual burden of malnutrition, to regulate the food and beverage industry and to encourage healthy eating throughout the life course.
Association between dietary carbohydrate quality and the prevalence of obesity and hypertension
AbstractBackground
Dietary carbohydrate quality may play an important role in disease development. We evaluated the association between carbohydrate quality index (CQI) and the prevalence of obesity and metabolic disorders among adults in South Korea.
Methods
We analysed 12 027 adults aged 19–64 years from the fifth Korea National Health and Nutrition Examination Survey (KNHANES). CQI was based on four criteria: crude fibre intake, dietary glycaemic index (DGI), whole grains/total grains ratio and solid carbohydrates/total carbohydrates ratio.
Results
Participants with a lower CQI were younger, had a lower income and were more likely to be smokers and to drink alcohol. The highest quintile CQI group showed the lowest DGI and the lowest consumption of liquid carbohydrates and refined grains, as well as the highest consumption of solid carbohydrates, crude fibre and whole grains (P < 0.05). A higher CQI was negatively associated with the prevalence of obesity (odds ratio = 0.83; 95% confidence interval = 0.69–0.99) and hypertension (odds ratio = 0.78; 95% confidence interval = 0.61–0.99) but was not associated with other metabolic disorders.
Conclusions
These results suggest that the quality of carbohydrates consumed is associated with the risk of obesity and hypertension. However, the cross‐sectional design does not preclude reverse causality.
Association between dietary acid load and the risk of hypertension among adults from South China: result from nutrition and health survey (2015-2017)
Abstract
Background: Higher dietary acid load (DAL) was considered to be associated with an elevated risk of hypertension, while related data from mainland China remains scarce and incomplete. We aim to evaluate the association between DAL and the risk of hypertension among adults from South China.
Methods: We conducted a nutrition and health survey in Guangdong Province located in southern China from 2015 to 2017. A four-stage probability sampling method was utilized to select representative samples of citizens aged ≥18 years old. DAL was assessed by potential renal acid load (PRAL) and net endogenous acid production (NEAP). Participants were divided to 4 groups (Q1-Q4) according to the quartile points of PRAL or NEAP distributions. Generalized linear mixed effects models were applied to evaluate the association between DAL and the risk of hypertension.
Results: A total of 3501 individuals were eligible for this study and 45.9% was male participants. Hypertension rate was 30.7%. A higher PRAL was associated with higher prevalence rate of hypertension among the male (P-trend = 0.03). OR for Q2 was 1.34 (95%CI, 0.94-1.91), Q3 was 1.53 (95%CI = 1.08, 2.16) and Q4 was 1.51 (95%CI, 1.08-2.16) among the male. However, as for total participants, the female, the participants with ≤55 years or participants with > 55 years, the associations were lack of significance. With respect to association between NEAP and hypertension, non-significant results were identified.
Conclusions: The current study indicated male hypertension was associated with higher PRAL, while given to this study was cross-sectional design, further studies are warranted to verify the association.
Malnutrition in pulmonary arterial hypertension: a possible role for dietary intervention
Abstract
Purpose of review: The last decade's progress has been made in the pharmacological treatment of pulmonary arterial hypertension (PAH). The role of nutrition in relation to quality of life in this group of patients is not investigated yet. In addition to avoiding salt and high-fluid intake based on left heart failure diet, there is no evidence-based diet recommendation for PAH.
Recent findings: It was recently demonstrated that patients with PAH suffer from malnutrition resulting in iron and vitamin D deficiency and glucose/insulin resistance. Recent experimental studies suggest that besides reduced malabsorption of important nutrients, the microbiome of the gut is also less diverse in PAH. In this review, we summarize the current knowledge on malnutrition and dietary intake in PAH. We discuss the possible underlying mechanisms and discuss novel therapeutic interventions validated in patients with left heart failure.
Summary: Large-scaled studies on dietary interventions are needed in PAH.
A systematic review of nutrition-based practices in prevention of hypertension among healthy youth
Abstract
The aim of this systematic review was to analyze the results of observational and interventional research/studies on nutrition-based practices in the prevention of hypertension among healthy youth. The MEDLINE/PubMed database was searched using the key words, "hypertension," "nutrition/diet," "prevention" and "youth." Inclusion criteria were: 1) sample with a majority of adolescents, defined as 10-24 years of age, or findings for adolescents reported separately from other age groups; 2) primary research reports; 3) studies with normotensive participants; and 4) studies that focused on preventing hypertension/lowering blood pressure through at least one nutritional practice. Results of the analysis indicated that increased consumption of unsaturated fats, fruits, vegetables and low-fat dietary products, decreased consumption of dietary sodium and beverages containing caffeine, and breastfeeding were found to have preventive effects against high blood pressure in later years of life. The effects of training given during youth to encourage a healthy lifestyle and behavior changes based on diet and physical activity were also noted.
Hypertension and the fat-soluble vitamins A, D and E
Abstract
Hypertension affects populations globally and is thus a public health and socio-economic problem. Macronutrient and micronutrient deficiencies are common in the general population, and may be even more prevalent in hypertensive patients. This study aimed to determine a possible association between hypertension and intake of fat-soluble vitamins A, D and E. Participants were from the cross-sectional Hortega nutrition study conducted with a random sample of 1514 people (50.3% women, 49.7% men) and two groups: nonhypertensive controls≥40 years old (n=429; 28.3%); unknown untreated hypertension cases≥40 years old (n=246; 16.2%). Biochemical and anthropometric measurements were taken. Data on dietary intakes, education, socio-economic status, place of residence, health habits, comorbidities, alcohol consumption and smoking were collected and assessed. A descriptive data study was done and compared by ANOVA and Chi-Square. No p value higher than 0.05 was considered significant. The results showed that vitamin A intake was higher in the hypertensive subpopulation (1732.77±962.27 µg vs. 1655.89±902.81 µg), and vitamin D and E intakes were lower (8.13±9.71 µg vs. 8.25±9.52 µg and 18.79±7.84 mg vs. 18.60±8.20 mg, respectively). No statistically significant differences were found in any adjusted model. This study did not significantly associate intake of vitamins A, D and E with hypertension in people aged over 40. Future studies on this topic and a larger sample are necessary.
Nutrition and physical activity on hypertension: implication of current evidence and guidelines
Abstract
Hypertension (HTN) is the leading cause of worldwide mortality and is responsible for approximately 40% of deaths from cardiovascular disease, chronicle kidney disease (CKD) and type 2 diabetes mellitus (T2DM) according to the World Health Organization (WHO). It is known that about 80% of all mortality from cardiovascular disorders could be prevented if a healthy diet and higher levels of physical activity were included among general population's lifestyle. Besides, guidelines for the treatment and control of HTN were recently modified for adequate nutritional and physical activity recommendations highlighted in meta-analysis and strong evidences such as randomized clinical trials. Therefore, to discuss nutrition and physical activity in the context of HTN seems to be crucial.
Nutrition and nutraceutical supplements in the treatment of hypertension
Abstract
Macronutrient and micronutrient deficiencies are very common in the general population, and may be even more common in patients with hypertension and cardiovascular disease due to genetic and environmental causes, and prescription drug use. Vascular biology assumes a pivotal role in the initiation and perpetuation of hypertension and target organ damage sequelae. Endothelial activation, oxidative stress and vascular smooth muscle dysfunction (hypertrophy, hyperplasia and remodeling) are initial events that initiate hypertension. Nutrient-gene interactions determine a broad array of phenotypic consequences such as vascular problems and hypertension. Optimal nutrition, nutraceuticals, vitamins, antioxidants, minerals, weight loss, exercise, smoking cessation, and moderate restriction of alcohol and caffeine, in addition to other lifestyle modifications, can prevent, delay the onset, reduce the severity, treat and control hypertension in many patients. An integrative approach combining these lifestyle suggestions with the correct pharmacologic treatment will best achieve new goal blood pressure levels, reduce cardiovascular risk factors, improve vascular health, reduce target organ damage, including coronary heart disease, stroke, congestive heart failure and renal disease, and reduce healthcare expenditure. The expanded scientific roles for nutraceutical supplements will be discussed in relation to the prevention and treatment of essential hypertension and cardiovascular diseases.
Inhibitory Effect of Garlic, Purple Onion, and White Onion on Key Enzymes Linked with Type 2 Diabetes and Hypertension
ABSTRACT
Spices are used in soup preparation in many homes and serve as ingredients in the preparation of several traditional delicacies endowed with natural antioxidants such as polyphenols. The aim of this study is to evaluate the effect of aqueous extract of garlic, white onion, and purple onion on angiotensin-converting enzyme, α-amylase, and α-glucosidase activity in vitro and determine their antioxidant properties via various antioxidant assays such as OH*, Fe2+ chelation, and 2, 2′-azino-bis 3-ethylbenzothiazoline-6-sulphonic acid (ABTS) radical-scavenging assays. The results reveal that aqueous extract of garlic, purple onion, and white onion inhibited angiotensin-converting enzyme, α-amylase, and α-glucosidase in a concentration-dependent manner (0–4 mg/ml). However, purple onion (IC50 = 0.59 mg/ml) had higher inhibitory effect on angiotensin-converting enzyme than white onion (IC50 = 0.66 mg/ml) and purple onion (IC50 = 0.96 mg/ml). Furthermore, white onion had significantly (p < .05) stronger inhibitory effect on α-amylase (IC50 = 3.93 mg/mL) than garlic (IC50 = 8.19 mg/ml) and purple onion (IC50 = 8.27 mg/ml). Conversely, garlic (IC50 = 4.50 mg/ml) had no significantly higher inhibitory effect on α-glucosidase activity than white onion and purple onion. In addition, the aqueous extracts were able to scavenge 2,2- diphenyl-1-picrylhydrazyl (DPPH*) free radical and reduce Fe3+ to Fe2+ in a dose-dependent manner. Therefore, a possible mechanism by which garlic, white onion, and purple onion exert antidiabetes and antihypertensive properties could be through the inhibitory effect on ACE, α-amylase, and α-glucosidase coupled with their ability to prevent lipid peroxidation in the pancreas and heart, which justify their strong antioxidant properties.
Topical Coenzyme Q10 demonstrates mitochondrial-mediated neuroprotection in a rodent model of ocular hypertension
Abstract
Coenzyme Q10
(CoQ10) is a mitochondrial-targeted antioxidant with known neuroprotective activity. Its ocular effects when co-solubilised with
α–tocopherol
polyethylene glycol succinate (TPGS) were evaluated. In vitro studies confirmed that CoQ10 was significantly protective in different
retinal ganglion cell
(RGC) models. In vivo studies in Adult Dark
Agouti
(DA) rats with unilateral surgically-induced ocular hypertension (OHT) treated with either CoQ10/TPGS
micelles
or TPGS vehicle twice daily for three weeks were performed, following which retinal cell health was assessed in vivo using DARC (Detection of Apoptotic Retinal Cells) and post-mortem with Brn3a histological assessment on whole retinal mounts. CoQ10/TPGS showed a significant neuroprotective effect compared to control with DARC (p < 0.05) and Brn3 (p < 0.01). Topical CoQ10 appears an effective therapy preventing RGC apoptosis and loss in glaucoma-related models.
Blood pressure lowering efficacy of coenzyme Q10 for primary hypertension
Collapse all Expand all
AbstractAvailable in
English
Español
Background
Blood pressure is a commonly measured risk factor for non‐fatal and fatal cardiovascular adverse events such as heart attacks and strokes. Clinical trials have suggested that coenzyme Q10, a non‐prescription nutritional supplement, can effectively lower blood pressure (BP). When this review was completed and published in October 2009, it concluded that "due to the possible unreliability of the 3 included studies, it is uncertain whether or not coenzyme Q10 reduces blood pressure in the long‐term management of primary hypertension."
Objectives
To determine the blood pressure lowering effect of coenzyme Q10 in primary hypertension.
Search methods
We searched the Hypertension Group Specialised Register (1946 to November 2015), The Cochrane Central Register of Controlled Trials (The Cochrane Library 2015, Issue 10), MEDLINE (1946 to November 2015), MEDLINE In‐Process (accessed 10 November 2015), EMBASE (1974 to November 2015), Web of Science (1899 to November 2015), CINAHL (1970 to November 2015), and ClinicalTrials.gov (accessed 10 November 2015). We also searched reference lists of articles for relevant clinical trials in any language.
Selection criteria
Double blind, randomized, placebo‐controlled parallel or cross‐over trials evaluating the blood pressure (BP) lowering efficacy of coenzyme Q10 for a duration of at least three weeks, in patients with primary hypertension.
Data collection and analysis
The primary author determined trial inclusion, extracted the data and assessed the risk of bias. The second author independently verified trial inclusion and data extraction.
Main results
In this update of the review, one new randomized, controlled cross‐over trial with a total of 30 participants was added, and one trial included in the initial review was excluded. Only two of the three included trials were pooled in the meta‐analysis, as one trial was judged to have an unacceptably high risk of bias. In the meta‐analysis of two RCTs (50 participants), coenzyme Q10 did not significantly change systolic BP: ‐3.68 mm Hg (95% confidence interval (CI) ‐8.86 to 1.49), or diastolic BP: ‐2.03 mm Hg (95% CI ‐4.86 to 0.81] ), based on clinic data.
Authors' conclusions
This review provides moderate‐quality evidence that coenzyme Q10 does not have a clinically significant effect on blood pressure. In one of three trials reporting adverse effects, coenzyme Q10 was well tolerated. Due to the small number of individuals and studies available for analysis, more well‐conducted trials are needed.
Fish oil intakes providing dietary attainable levels of EPA and DHA reduces blood pressure in adults with systolic hypertension in a retrospective analysis
Abstract/Summary
Background: Although a large number of randomized controlled trials (RCTs) have examined the impact of the n-3 (ω-3) fatty acids EPA (20:5n-3) and DHA (22:6n-3) on blood pressure and vascular function, the majority have used doses of EPA+DHA of > 3 g per d,which are unlikely to be achieved by diet manipulation. Objective: The objective was to examine, using a retrospective analysis from a multi-center RCT, the impact of recommended, dietary achievable EPA+DHA intakes on systolic and diastolic blood pressure and microvascular function in UK adults. Design: Healthy men and women (n = 312) completed a double-blind, placebo-controlled RCT consuming control oil, or fish oil providing 0.7 g or 1.8 g EPA+DHA per d in random order each for 8 wk. Fasting blood pressure and microvascular function (using Laser Doppler Iontophoresis) were assessed and plasma collected for the quantification of markers of vascular function. Participants were retrospectively genotyped for the eNOS rs1799983 variant. Results: No impact of n-3 fatty acid treatment or any treatment * eNOS genotype interactions were evident in the group as a whole for any of the clinical or biochemical outcomes. Assessment of response according to hypertension status at baseline indicated a significant (P=0.046) fish oil-induced reduction (mean 5 mmHg) in systolic blood pressure specifically in those with isolated systolic hypertension (n=31). No dose response was observed. Conclusions: These findings indicate that, in those with isolated systolic hypertension, daily doses of EPA+DHA as low as 0.7 g bring about clinically meaningful blood pressure reductions which, at a population level, would be associated with lower cardiovascular disease risk. Confirmation of findings in an RCT where participants are prospectively recruited on the basis of blood pressure status is required to draw definite conclusions.
Cardiovascular Disease
Vitamin and mineral supplements in the primary prevention of cardiovascular disease and cancer: An updated systematic evidence review for the U.S. Preventive Services Task Force
Abstract
Background: Vitamin and mineral supplements are commonly used to prevent chronic diseases.
Purpose: To systematically review evidence for the benefit and harms of vitamin and mineral supplements in community-dwelling, nutrient-sufficient adults for the primary prevention of cardiovascular disease (CVD) and cancer.
Data sources: MEDLINE, Embase, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, and Database of Abstracts of Reviews of Effects were searched from January 2005 to 29 January 2013, with manual searches of reference lists and gray literature.
Study selection: Two investigators independently selected and reviewed fair- and good-quality trials for benefit and fair- and good-quality trials and observational studies for harms.
Data extraction: Dual quality assessments and data abstraction.
Data synthesis: Two large trials (n = 27 658) reported lower cancer incidence in men taking a multivitamin for more than 10 years (pooled unadjusted relative risk, 0.93 [95% CI, 0.87 to 0.99]). The study that included women showed no effect in that group. High-quality studies (k = 24; n = 324 653) of single and paired nutrients (such as vitamins A, C, or D; folic acid; selenium; or calcium) were scant and heterogeneous and showed no clear evidence of benefit or harm. Neither vitamin E nor β-carotene prevented CVD or cancer, and β-carotene increased lung cancer risk in smokers.
Limitations: The analysis included only primary prevention studies in adults without known nutritional deficiencies. Studies were conducted in older individuals and included various supplements and doses under the set upper tolerable limits. Duration of most studies was less than 10 years.
Conclusion: Limited evidence supports any benefit from vitamin and mineral supplementation for the prevention of cancer or CVD. Two trials found a small, borderline-significant benefit from multivitamin supplements on cancer in men only and no effect on CVD.
Supplemental Vitamins and Minerals for Cardiovascular Disease Prevention and Treatment
Abstract
Purpose of review: The objective of this study is to explore the current literature supporting the use oral multivitamins and multi/minerals (OMVMs) for cardiovascular diseases (CVD) treatment and prevention.
Recent findings: Data on multivitamins, vitamin C and D, coenzyme Q, calcium, and selenium, has showed no consistent benefit for the prevention of CVD, myocardial infarction, or stroke, nor was there a benefit for all-cause mortality to support their routine supplementation. Folic acid alone and B vitamins with folic acid, B6 and B12, reduce stroke, whereas niacin and antioxidants are associated with an increased risk of all-cause mortality. Iron deficiency should be avoided and treated if found, but routine supplementation to those without deficiency is not evidence based. Despite the high supplement use by the general public, there is no evidence to support the routine supplementation of oral multivitamins and multi/minerals (OVMN) for CVD prevention or treatment.
Keywords: Cardiovascular disease; Supplements; Vitamins.
Relation of Total Sugars, Sucrose, Fructose, and Added Sugars With the Risk of Cardiovascular Disease: A Systematic Review and Dose-Response Meta-analysis of Prospective Cohort Studies
Abstract
Objective: To determine the association of total and added fructose-containing sugars on cardiovascular (CVD) incidence and mortality.
Methods: MEDLINE, EMBASE and Cochrane Library were searched from January 1, 1980, to July 31, 2018. Prospective cohort studies assessing the association of reported intakes of total, sucrose, fructose and added sugars with CVD incidence and mortality in individuals free from disease at baseline were included. Risk estimates were pooled using the inverse variance method, and dose-response analysis was modeled.
Results: Eligibility criteria were met by 24 prospective cohort comparisons (624,128 unique individuals; 11,856 CVD incidence cases and 12,224 CVD mortality cases). Total sugars, sucrose, and fructose were not associated with CVD incidence. Total sugars (risk ratio, 1.09 [95% confidence interval, 1.02 to 1.17]) and fructose (1.08 [1.01 to 1.15]) showed a harmful association for CVD mortality, there was no association for added sugars and a beneficial association for sucrose (0.94 [0.89 to 0.99]). Dose-response analyses showed a beneficial linear dose-response gradient for sucrose and nonlinear dose-response thresholds for harm for total sugars (133 grams, 26% energy), fructose (58 grams, 11% energy) and added sugars (65 grams, 13% energy) in relation to CVD mortality (P<.05). The certainty of the evidence using GRADE was very low for CVD incidence and low for CVD mortality for all sugar types.
Conclusion: Current evidence supports a threshold of harm for intakes of total sugars, added sugars, and fructose at higher exposures and lack of harm for sucrose independent of food form for CVD mortality. Further research of different food sources of sugars is needed to define better the relationship between sugars and CVD. REGISTRATION: clinicaltrials.gov,
NCT01608620
Water intake from foods and beverages and risk of mortality from CVD: the Japan Collaborative Cohort (JACC) Study
Abstract
Objective: To examine the association of water intake with risk of mortality from CVD.
Design: Prospective cohort study.Setting/SubjectsA total of 22 939 men and 35 362 women aged 40-79 years enrolled in the Japan Collaborative Cohort (JACC) Study with available data regarding water intake from foods and beverages. The underlying causes of death were determined based on the International Classification of Diseases.
Results: During the median 19·1 years of follow-up, 1637 men and 1707 women died from CVD. There was an inverse trend between high water intake and risk of CVD in both sexes. Compared with participants in the lowest quintile of water intake, the multivariable-adjusted hazard ratios (95 % CI) for mortality from total CVD in the highest quintile of water intake were 0·88 (0·72, 1·07; P for trend=0·03) in men and 0·79 (0·66, 0·95; P for trend=0·10) in women. Those for CHD were 0·81 (0·54, 1·21; P for trend=0·06) in men and 0·60 (0·39, 0·93; P for trend=0·20) in women. Reduced risk of mortality from ischaemic stroke was also observed among women in the highest water intake quintile: 0·70 (0·47, 0·99; P for trend=0·19). There was no association between water intake and mortality from haemorrhagic stroke in either sex.
Conclusions: Higher intake of fluids from foods and beverages was associated with reduced risk of cardiovascular mortality in both sexes and reduced risk of ischaemic stroke in women in Japan.
Keywords: CHD; Cardiovascular mortality; Japanese; Moisture in foods and beverages; Stroke; Water.
[Optimal cholesterol levels in patients in real-life. A systematic review]
Abstract
Dyslipidaemia is one of the main risk factors for the development of atherosclerosis. Different studies have demonstrated that the lower the LDL cholesterol, the better. Current evidence shows that the LDL cholesterol targets recommended by the clinical practice guidelines are beneficial and safe. However, consistent data show that higher reductions might provide additional cardiovascular beneficial effects, without an increase in side effects. Unfortunately, the current control of dyslipidaemia is very poor. Although statins are the treatment of choice in the majority of patients with dyslipidaemia, the current therapeutic armamentarium has different alternatives that effectively reduce LDL cholesterol levels, and that alone, or in combination, help to achieve LDL cholesterol targets in the majority of patients.
Keywords: Cholesterol; Colesterol; Estatina; Ezetimiba; Ezetimibe; Inhibidores PCSK9; PCSK9 inhibitors; Statin.
[LDL-cholesterol and cardiovascular events: the lower the better?]
Abstract
For over 30 years, intensive research efforts investigated the role of LDL cholesterol in the pathogenesis of cardiovascular disease. In various settings, large statin trials showed an association between LDL cholesterol levels and cardiovascular event rates. This association is often referred to as the 'LDL cholesterol hypothesis'. More recent trials on agents with totally different modes of action confirmed this association and indicated a causal relationship between lower LDL cholesterol levels and improved cardiovascular outcomes. It has been proposed to term this causal relationship the 'LDL cholesterol principle'. It is to be expected that currently ongoing outcomes trials will further support the assumption of a causal relationship and will finally offer an armamentarium to therapists that will enable individualized treatment of dyslipidemias and their sequelae.
Unravelling HDL-Looking beyond the Cholesterol Surface to the Quality Within
Abstract
High-density lipoprotein (HDL) particles have experienced a turbulent decade of falling from grace with widespread demotion from the most-sought-after therapeutic target to reverse cardiovascular disease (CVD), to mere biomarker status. HDL is slowly emerging from these dark times due to the HDL flux hypothesis wherein measures of HDL cholesterol efflux capacity (CEC) are better predictors of reduced CVD risk than static HDL-cholesterol (HDL-C) levels. HDL particles are emulsions of metabolites, lipids, protein, and microRNA (miR) built on the backbone of Apolipoprotein A1 (ApoA1) that are growing in their complexity due to the higher sensitivity of the respective “omic” technologies. Our understanding of particle composition has increased dramatically within this era and has exposed how our understanding of these particles to date has been oversimplified. Elucidation of the HDL proteome coupled with the identification of specific miRs on HDL have highlighted the “hormonal” characteristics of HDL in that it carries and delivers messages systemically. HDL can dock to most peripheral cells via its receptors, including SR-B1, ABCA1, and ABCG1, which may be a critical step for facilitating HDL-to-cell communication. The composition of HDL particles is, in turn, altered in numerous disease states including diabetes, auto-immune disease, and CVD. The consequence of changes in composition, however, on subsequent biological activities of HDL is currently poorly understood and this is an important avenue for the field to explore in the future. Improving HDL particle quality as opposed to HDL quantity may, in turn, prove a more beneficial investment to reduce CVD risk.
Keywords: HDL; HDL functions; HDL lipidome; HDL microRNA; HDL proteome; cardiovascular disease; cholesterol efflux capacity; inflammation.
The effect of oat β-glucan on LDL-cholesterol, non-HDL-cholesterol and apoB for CVD risk reduction: a systematic review and meta-analysis of randomised-controlled trials
Abstract
Oats are a rich source of β-glucan, a viscous, soluble fibre recognised for its cholesterol-lowering properties, and are associated with reduced risk of CVD. Our objective was to conduct a systematic review and meta-analysis of randomised-controlled trials (RCT) investigating the cholesterol-lowering potential of oat β-glucan on LDL-cholesterol, non-HDL-cholesterol and apoB for the risk reduction of CVD. MEDLINE, Embase, CINAHL and Cochrane CENTRAL were searched. We included RCT of ≥3 weeks of follow-up, assessing the effect of diets enriched with oat β-glucan compared with controlled diets on LDL-cholesterol, non-HDL-cholesterol or apoB. Two independent reviewers extracted data and assessed study quality and risk of bias. Data were pooled using the generic inverse-variance method with random effects models and expressed as mean differences with 95 % CI. Heterogeneity was assessed by the Cochran's Q statistic and quantified by the I 2-statistic. In total, fifty-eight trials (n 3974) were included. A median dose of 3·5 g/d of oat β-glucan significantly lowered LDL-cholesterol (-0·19; 95 % CI -0·23, -0·14 mmol/l, P<0·00001), non-HDL-cholesterol (-0·20; 95 % CI -0·26, -0·15 mmol/l, P<0·00001) and apoB (-0·03; 95 % CI -0·05, -0·02 g/l, P<0·0001) compared with control interventions. There was evidence for considerable unexplained heterogeneity in the analysis of LDL-cholesterol (I 2=79 %) and non-HDL-cholesterol (I 2=99 %). Pooled analyses showed that oat β-glucan has a lowering effect on LDL-cholesterol, non-HDL-cholesterol and apoB. Inclusion of oat-containing foods may be a strategy for achieving targets in CVD reduction.
The Role of Omega-3 Fatty Acids in the Setting of Coronary Artery Disease and COPD: A Review
Abstract
Chronic obstructive pulmonary disease (COPD) is a growing healthcare concern and will represent the third leading cause of death worldwide within the next decade. COPD is the result of a complex interaction between environmental factors, especially cigarette smoking, air pollution, and genetic preconditions, which result in persistent inflammation of the airways. There is growing evidence that the chronic inflammatory state, measurable by increased levels of circulating cytokines, chemokines, and acute phase proteins, may not be confined to the lungs. Cardiovascular disease (CVD) and especially coronary artery disease (CAD) are common comorbidities of COPD, and low-grade systemic inflammation plays a decisive role in its pathogenesis. Omega-3 polyunsaturated fatty acids (n-3 PUFAs) exert multiple functions in humans and are crucially involved in limiting and resolving inflammatory processes. n-3 PUFAs have been intensively studied for their ability to improve morbidity and mortality in patients with CVD and CAD. This review aims to summarize the current knowledge on the effects of n-3 PUFA on inflammation and its impact on CAD in COPD from a clinical perspective.
Omega-3 Fatty Acids and Cardiovascular Disease: Summary of the 2016 Agency of Healthcare Research and Quality Evidence Review
Abstract
We summarize the 2016 update of the 2004 Agency of Healthcare Research and Quality's evidence review of omega-3 fatty acids and cardiovascular disease (CVD). The overall findings for the effects of marine oil supplements on intermediate CVD outcomes remain largely unchanged. There is high strength of evidence, based on numerous trials, of no significant effects of marine oils on systolic or diastolic blood pressures, but there are small, yet statistically significant increases in high density lipoprotein and low density lipoprotein cholesterol concentrations. The clinical significance of these small changes, particularly in combination, is unclear. The strongest effect of marine oils is on triglyceride concentrations. Across studies, this effect was dose-dependent and related to studies' mean baseline triglyceride concentration. In observational studies, there is low strength of evidence that increased marine oil intake lowers ischemic stroke risk. Among randomized controlled trials and observational studies, there is evidence of variable strength of no association with increased marine oil intake and lower CVD event risk. Evidence regarding alpha-linolenic acid intake is sparser. There is moderate strength of evidence of no effect on blood pressure or lipoprotein concentrations and low strength of evidence of no association with coronary heart disease, atrial fibrillation and congestive heart failure.
Omega-3 fatty acids for the primary and secondary prevention of cardiovascular disease
Abstract
Background: Researchers have suggested that omega-3 polyunsaturated fatty acids from oily fish (long-chain omega-3 (LCn3), including eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA)), as well as from plants (alpha-linolenic acid (ALA)) benefit cardiovascular health. Guidelines recommend increasing omega-3-rich foods, and sometimes supplementation, but recent trials have not confirmed this.
Objectives: To assess effects of increased intake of fish- and plant-based omega-3 for all-cause mortality, cardiovascular (CVD) events, adiposity and lipids.
Search methods: We searched CENTRAL, MEDLINE and Embase to April 2017, plus ClinicalTrials.gov and World Health Organization International Clinical Trials Registry to September 2016, with no language restrictions. We handsearched systematic review references and bibliographies and contacted authors.
Selection criteria: We included randomised controlled trials (RCTs) that lasted at least 12 months and compared supplementation and/or advice to increase LCn3 or ALA intake versus usual or lower intake.
Data collection and analysis: Two review authors independently assessed studies for inclusion, extracted data and assessed validity. We performed separate random-effects meta-analysis for ALA and LCn3 interventions, and assessed dose-response relationships through meta-regression.
Main results: We included 79 RCTs (112,059 participants) in this review update and found that 25 were at low summary risk of bias. Trials were of 12 to 72 months' duration and included adults at varying cardiovascular risk, mainly in high-income countries. Most studies assessed LCn3 supplementation with capsules, but some used LCn3- or ALA-rich or enriched foods or dietary advice compared to placebo or usual diet. LCn3 doses ranged from 0.5g/d LCn3 to > 5 g/d (16 RCTs gave at least 3g/d LCn3).Meta-analysis and sensitivity analyses suggested little or no effect of increasing LCn3 on all-cause mortality (RR 0.98, 95% CI 0.90 to 1.03, 92,653 participants; 8189 deaths in 39 trials, high-quality evidence), cardiovascular mortality (RR 0.95, 95% CI 0.87 to 1.03, 67,772 participants; 4544 CVD deaths in 25 RCTs), cardiovascular events (RR 0.99, 95% CI 0.94 to 1.04, 90,378 participants; 14,737 people experienced events in 38 trials, high-quality evidence), coronary heart disease (CHD) mortality (RR 0.93, 95% CI 0.79 to 1.09, 73,491 participants; 1596 CHD deaths in 21 RCTs), stroke (RR 1.06, 95% CI 0.96 to 1.16, 89,358 participants; 1822 strokes in 28 trials) or arrhythmia (RR 0.97, 95% CI 0.90 to 1.05, 53,796 participants; 3788 people experienced arrhythmia in 28 RCTs). There was a suggestion that LCn3 reduced CHD events (RR 0.93, 95% CI 0.88 to 0.97, 84,301 participants; 5469 people experienced CHD events in 28 RCTs); however, this was not maintained in sensitivity analyses - LCn3 probably makes little or no difference to CHD event risk. All evidence was of moderate GRADE quality, except as noted.Increasing ALA intake probably makes little or no difference to all-cause mortality (RR 1.01, 95% CI 0.84 to 1.20, 19,327 participants; 459 deaths, 5 RCTs),cardiovascular mortality (RR 0.96, 95% CI 0.74 to 1.25, 18,619 participants; 219 cardiovascular deaths, 4 RCTs), and CHD mortality (1.1% to 1.0%, RR 0.95, 95% CI 0.72 to 1.26, 18,353 participants; 193 CHD deaths, 3 RCTs) and ALA may make little or no difference to CHD events (RR 1.00, 95% CI 0.80 to 1.22, 19,061 participants, 397 CHD events, 4 RCTs, low-quality evidence). However, increased ALA may slightly reduce risk of cardiovascular events (from 4.8% to 4.7%, RR 0.95, 95% CI 0.83 to 1.07, 19,327 participants; 884 CVD events, 5 RCTs, low-quality evidence with greater effects in trials at low summary risk of bias), and probably reduces risk of arrhythmia (3.3% to 2.6%, RR 0.79, 95% CI 0.57 to 1.10, 4,837 participants; 141 events, 1 RCT). Effects on stroke are unclear.Sensitivity analysis retaining only trials at low summary risk of bias moved effect sizes towards the null (RR 1.0) for all LCn3 primary outcomes except arrhythmias, but for most ALA outcomes, effect sizes moved to suggest protection. LCn3 funnel plots suggested that adding in missing studies/results would move effect sizes towards null for most primary outcomes. There were no dose or duration effects in subgrouping or meta-regression.There was no evidence that increasing LCn3 or ALA altered serious adverse events, adiposity or lipids, except LCn3 reduced triglycerides by ˜15% in a dose-dependant way (high-quality evidence).
Authors' conclusions: This is the most extensive systematic assessment of effects of omega-3 fats on cardiovascular health to date. Moderate- and high-quality evidence suggests that increasing EPA and DHA has little or no effect on mortality or cardiovascular health (evidence mainly from supplement trials). Previous suggestions of benefits from EPA and DHA supplements appear to spring from trials with higher risk of bias. Low-quality evidence suggests ALA may slightly reduce CVD event and arrhythmia risk.
Vitamin D and Cardiovascular Disease: An Update
Abstract
In the clinical setting, administration of high daily or bolus doses of vitamin D is often solely based on 25-hydroxyvitamin D [25(OH)D] testing. This review summarizes the evidence of the effect of vitamin D on cardiovascular disease (CVD). Meta-analyses of randomized controlled trials (RCTs) have demonstrated that CVD risk markers, such as lipid parameters, inflammation markers, blood pressure, and arterial stiffness, are largely unaffected by vitamin D supplementation. Similar results have been obtained regarding CVD events and mortality from (meta)-analyses of RCTs, even in subgroups with 25(OH)D concentrations <50 nmol/l. Likewise, Mendelian randomization studies have indicated that the genetic reduction of the 25(OH)D concentration does not increase CVD risk. Some studies do not exclude the possibility of adverse vitamin D effects, such as elevated plasma calcium concentration and an increased CVD risk at a 25(OH)D concentration >125 nmol/l. Based on a conservative benefit-risk management approach, vitamin D doses beyond the nutritionally recommended amounts of 600 to 800 IE daily currently cannot be advised for the prevention of CVD events.
Exercise benefits in cardiovascular disease: beyond attenuation of traditional risk factors
Abstract
Despite strong scientific evidence supporting the benefits of regular exercise for the prevention and management of cardiovascular disease (CVD), physical inactivity is highly prevalent worldwide. In addition to merely changing well-known risk factors for systemic CVD, regular exercise can also improve cardiovascular health through non-traditional mechanisms. Understanding the pathways through which exercise influences different physiological systems is important and might yield new therapeutic strategies to target pathophysiological mechanisms in CVD. This Review includes a critical discussion of how regular exercise can have antiatherogenic effects in the vasculature, improve autonomic balance (thereby reducing the risk of malignant arrhythmias), and induce cardioprotection against ischaemia-reperfusion injury, independent of effects on traditional CVD risk factors. This Review also describes how exercise promotes a healthy anti-inflammatory milieu (largely through the release of muscle-derived myokines), stimulates myocardial regeneration, and ameliorates age-related loss of muscle mass and strength, a frequently overlooked non-traditional CVD risk factor. Finally, we discuss how the benefits of exercise might also occur via promotion of a healthy gut microbiota. We argue, therefore, that a holistic view of all body systems is necessary and useful when analysing the role of exercise in cardiovascular health.
Nutritional management of hyperapoB
Abstract
Plasma apoB is a more accurate marker of the risk of CVD and type 2 diabetes (T2D) than LDL-cholesterol; however, nutritional reviews targeting apoB are scarce. Here we reviewed eighty-seven nutritional studies and present conclusions in order of strength of evidence. Plasma apoB was reduced in all studies that induced weight loss of 6-12 % using hypoenergetic diets (seven studies; 5440-7110 kJ/d; 1300-1700 kcal/d; 34-50 % carbohydrates; 27-39 % fat; 18-24 % protein). When macronutrients were compared in isoenergetic diets (eleven studies including eight randomised controlled trials (RCT); n 1189), the diets that reduced plasma apoB were composed of 26-51 % carbohydrates, 26-46 % fat, 11-32 % protein, 10-27 % MUFA, 5-14 % PUFA and 7-13 % SFA. Replacement of carbohydrate by MUFA, not SFA, decreased plasma apoB. Moreover, dietary enriching with n-3 fatty acids (FA) (from fish: 1·1-1·7 g/d or supplementation: 3·2-3·4 g/d EPA/DHA or 4 g/d EPA), psyllium (about 8-20 g/d), phytosterols (about 2-4 g/d) or nuts (30-75 g/d) also decreased plasma apoB, mostly in hyperlipidaemic subjects. While high intake of trans-FA (4·3-9·1 %) increased plasma apoB, it is unlikely that these amounts represent usual consumption. Inconsistent data existed on the effect of soya proteins (25-30 g/d), while the positive association of alcohol consumption with low plasma apoB was reported in cross-sectional studies only. Five isoenergetic studies using Mediterranean diets (including two RCT; 823 subjects) reported a decrease of plasma apoB, while weaker evidence existed for Dietary Approaches to Stop Hypertension (DASH), vegetarian, Nordic and Palaeolithic diets. We recommend using a Mediterranean dietary pattern, which also encompasses the dietary components reported to reduce plasma apoB, to target hyperapoB and reduce the risks of CVD and T2D.
Vitamin C and Heart Health: A Review Based on Findings from Epidemiologic Studies
Abstract
Vitamin C is a powerful dietary antioxidant that has received considerable attention in the literature related to its possible role in heart health. Although classical vitamin C deficiency, marked by scurvy, is rare in most parts of the world, some research has shown variable heart disease risks depending on plasma vitamin C concentration, even within the normal range. Furthermore, other studies have suggested possible heart-related benefits to vitamin C taken in doses beyond the minimal amounts required to prevent classically defined deficiency. The objective of this review is to systematically review the findings of existing epidemiologic research on vitamin C and its potential role in cardiovascular disease (CVD). It is well established that vitamin C inhibits oxidation of LDL-protein, thereby reducing atherosclerosis, but the cardiovascular outcomes related to this action and other actions of vitamin C are not fully understood. Randomized controlled trials as well as observational cohort studies have investigated this topic with varying results. Vitamin C has been linked in some work to improvements in lipid profiles, arterial stiffness, and endothelial function. However, other studies have failed to confirm these results, and observational cohort studies are varied in their findings on the vitamin's effect on CVD risk and mortality. Overall, current research suggests that vitamin C deficiency is associated with a higher risk of mortality from CVD and that vitamin C may slightly improve endothelial function and lipid profiles in some groups, especially those with low plasma vitamin C levels. However, the current literature provides little support for the widespread use of vitamin C supplementation to reduce CVD risk or mortality.
Combined effect of low-risk dietary and lifestyle behaviors in primary prevention of myocardial infarction in women
Abstract
Background: Limited data are available on the benefit of combining healthy dietary and lifestyle behaviors in the prevention of myocardial infarction (MI) in women.
Methods: We used factor analysis to identify a low-risk behavior-based dietary pattern in 24 444 postmenopausal women from the population-based prospective Swedish Mammography Cohort who were free of diagnosed cancer, cardiovascular disease, and diabetes mellitus at baseline (September 15, 1997). We also defined 3 low-risk lifestyle factors: nonsmoking, waist-hip ratio less than the 75th percentile (< 0.85), and being physically active (at least 40 minutes of daily walking or bicycling and 1 hour of weekly exercise).
Results: During 6.2 years (151 434 person-years) of follow-up, we ascertained 308 cases of primary MI. Two major identified dietary patterns, "healthy" and "alcohol," were significantly associated with decreased risk of MI. The low-risk diet (high scores for the healthy dietary pattern) characterized by a high intake of vegetables, fruit, whole grains, fish, and legumes, in combination with moderate alcohol consumption (>/= 5 g of alcohol per day), along with the 3 low-risk lifestyle behaviors, was associated with 92% decreased risk (95% confidence interval, 72%-98%) compared with findings in women without any low-risk diet and lifestyle factors. This combination of healthy behaviors, present in 5%, may prevent 77% of MIs in the study population.
Conclusion: Most MIs in women may be preventable by consuming a healthy diet and moderate amounts of alcohol, being physically active, not smoking, and maintaining a healthy weight.
Low-risk diet and lifestyle habits in the primary prevention of myocardial infarction in men: a population-based prospective cohort study
Abstract
Background: Adherence to a combination of healthy dietary and lifestyle practices may have an impressive impact on the primary prevention of myocardial infarction (MI).
Objectives: The aim of this study was to examine the benefit of combined low-risk diet and healthy lifestyle practices on the incidence of MI in men.
Methods: The population-based, prospective cohort of Swedish men comprised 45- to 79-year-old men who completed a detailed questionnaire on diet and lifestyle at baseline in 1997. In total, 20,721 men with no history of cancer, cardiovascular disease, diabetes, hypertension, or high cholesterol levels were followed through 2009. Low-risk behavior included 5 factors: a healthy diet (top quintile of Recommended Food Score), moderate alcohol consumption (10 to 30 g/day), no smoking, being physically active (walking/bicycling ≥40 min/day and exercising ≥1 h/week), and having no abdominal adiposity (waist circumference <95 cm).
Results: During 11 years of follow-up, we ascertained 1,361 incident cases of MI. The low-risk dietary choice together with moderate alcohol consumption was associated with a relative risk of 0.65 (95% confidence interval [CI]: 0.48 to 0.87) compared with men having 0 of 5 low-risk factors. Men having all 5 low-risk factors compared with those with 0 low-risk factors had a relative risk of 0.14 (95% CI: 0.04 to 0.43). This combination of healthy behaviors, present in 1% of the men, could prevent 79% (95% CI: 34% to 93%) of the MI events on the basis of the study population.
Conclusions: Almost 4 of 5 MIs in men may be preventable with a combined low-risk behavior.
High levels of lipoprotein (a) and premature acute coronary syndrome
Abstract
Background and aims
High levels of lipoprotein(a) [Lp(a)] are associated with increased risk of acute coronary syndrome (ACS). We explored whether Lp(a) exhibits a stronger association with premature ACS.
Methods
A case-control study was conducted; 1457 patients with a history of ACS (54.8 ± 13 years, 86% males) and 2090 age-sex matched adults free of cardiovascular disease were enrolled. Bio-clinical characteristics [risk factors, low-density lipoprotein-cholesterol, Lp(a)] were derived through standard procedures.
Results
A 10 mg/dL increase in Lp(a) was associated with 4% (95% CI, 1.01 to 1.02) higher likelihood of having ACS in younger (<45 years) and 2% (95% CI, 1.01 to 1.02) higher likelihood in middle-aged (45-60 years) individuals. Adjusting for common risk factors, elevated Lp(a), i.e. >50 mg/dL, was still associated with increased likelihood of ACS in younger adults (<45 years) (OR = 2.88, 95% CI, 1.7 to 4.6) and in middle aged ones (45 and 60 years) (OR = 2.06, 95% CI, 1.4 to 3.2), but not in older participants (>60 years) (OR = 1.31, 95% CI, 0.8 to 2.4).
Conclusions
Lp(a) seems to be an independent risk factor for ACS in individuals <45 years, and high Lp(a) levels increase by ∼3folds the risk for ACS. The association is preserved but is less in middle-aged individuals (45-60 years) and is abolished >60 years.
Sugar-Sweetened Beverage Intake Is Positively Associated with Baseline Triglyceride Concentrations, and Changes in Intake Are Inversely Associated with Changes in HDL Cholesterol over 12 Months in a Multi-Ethnic Sample of Children
Abstract
Background: Intake of sugar-sweetened beverages (SSBs) is linked to greater cardiometabolic risk in adults. Although longitudinal evidence is sparse among children, SSB intake reduction is targeted to reduce cardiometabolic risk factors in this group.
Objective: We investigated characteristics associated with consumption of SSBs in a multi-ethnic sample of children/adolescents and measured cross-sectional and longitudinal associations between SSB intake and plasma HDL cholesterol and triglycerides (TGs) over 12 mo.
Methods: In a diverse cohort of children aged 8–15 y, cross-sectional associations (n = 613) between baseline SSB intake and blood lipid concentrations and longitudinal associations (n = 380) between mean SSB intake, changes in SSB intake, and lipid changes over 12 mo were assessed with multivariable linear regression.
Results: Greater SSB intake was associated with lower socioeconomic status, higher total energy intake, lower fruit/vegetable intake, and more sedentary time. In cross-sectional analysis, greater SSB intake was associated with higher plasma TG concentrations among consumers (62.4, 65.3, and 71.6 mg/dL in children who consumed >0 but <2, ≥2 but <7, and ≥7 servings/wk, respectively; P-trend: 0.03); plasma HDL cholesterol showed no cross-sectional association. In the longitudinal analysis, mean SSB intake over 12 mo was not associated with lipid changes; however, the 12-mo increase in plasma HDL-cholesterol concentration was greater among children who decreased their intake by ≥1 serving/wk (4.6 ± 0.8 mg/dL) compared with children whose intake stayed the same (2.0 ± 0.8 mg/dL) or increased (1.5 ± 0.8 mg/dL; P = 0.02).
Conclusions: In a multi-ethnic sample of children, intake of SSBs was positively associated with TG concentrations among consumers, and changes in SSB intake were inversely associated with HDL cholesterol concentration changes over 12 mo. Further research in large diverse samples of children is needed to study the public health implications of reducing SSB intake among children of different racial/ethnic groups. The Daily D Health Study was registered at
clinicaltrials.gov
as NCT01537809.
Egg consumption and coronary artery calcification in asymptomatic men and women
Abstract
Objective
The association of egg consumption with subclinical coronary atherosclerosis remains unknown. Our aim was to examine the association between egg consumption and prevalence of coronary artery calcium (CAC).
Methods
Cross-sectional study of 23,417 asymptomatic adult men and women without a history of cardiovascular disease (CVD) or hypercholesterolemia, who underwent a health screening examination including cardiac computed tomography for CAC scoring and completed a validated food frequency questionnaire at the Kangbuk Samsung Hospital Total Healthcare Centers, South Korea (March 2011–April 2013).
Results
The prevalence of detectable CAC (CAC score > 0) was 11.2%. In multivariable-adjusted models, CAC score ratio (95% confidence interval [CI]) comparing participants eating ≥ 7 eggs/wk to those eating < 1 egg/wk was 1.80 (1.14–2.83; P for trend = 0.003). The multivariable CAC score ratio (95% CI) associated with an increase in consumption of 1 egg/day was 1.54 (1.11–2.14). The positive association seemed to be more pronounced among participants with low vegetable intake ( P for interaction = 0.02) and those with high BMI ( P for interaction = 0.05). The association was attenuated and no longer significant after further adjustment for dietary cholesterol.
Conclusion
Egg consumption was associated with an increased prevalence of subclinical coronary atherosclerosis and with a greater degree of coronary calcification in asymptomatic Korean adults, which may be mediated by dietary cholesterol. The association was particularly pronounced among individuals with low vegetable intake and those with high BMI.
Nut Consumption and Risk of Cardiovascular Disease
Abstract
Background The associations between specific types of nuts, specifically peanuts and walnuts, and cardiovascular disease remain unclear.
Objectives The authors sought to analyze the associations between the intake of total and specific types of nuts and cardiovascular disease, coronary heart disease, and stroke risk.
Methods The authors included 76,364 women from the Nurses’ Health Study (1980 to 2012), 92,946 women from the Nurses’ Health Study II (1991 to 2013), and 41,526 men from the Health Professionals Follow-Up Study (1986 to 2012) who were free of cancer, heart disease, and stroke at baseline. Nut consumption was assessed using food frequency questionnaires at baseline and was updated every 4 years.
Results During 5,063,439 person-years of follow-up, the authors documented 14,136 incident cardiovascular disease cases, including 8,390 coronary heart disease cases and 5,910 stroke cases. Total nut consumption was inversely associated with total cardiovascular disease and coronary heart disease after adjustment for cardiovascular risk factors. The pooled multivariable hazard ratios for cardiovascular disease and coronary heart disease among participants who consumed 1 serving of nuts (28 g) 5 or more times per week, compared with the reference category (never or almost never), were 0.86 (95% confidence interval: 0.79 to 0.93; p for trend = 0.0002) and 0.80 (95% confidence interval: 0.72 to 0.89; p for trend <0.001), respectively. Consumption of peanuts and tree nuts (2 or more times/week) and walnuts (1 or more times/week) was associated with a 13% to 19% lower risk of total cardiovascular disease and 15% to 23% lower risk of coronary heart disease.
Conclusions In 3 large prospective cohort studies, higher consumption of total and specific types of nuts was inversely associated with total cardiovascular disease and coronary heart disease.
Unhealthy diets linked to more than 400,000 cardiovascular deaths
Study Highlights:
- Eating a diet lacking in healthy foods and/or high in unhealthy foods was estimated to contribute to more than 400,000 deaths from heart and blood vessel diseases in the United States in 2015.
- Eating more nuts, vegetables, and whole grains, and less salt and trans fats, could save tens of thousands of lives in the U.S. each year.
Denmark's Policy on Artificial Trans Fat and Cardiovascular Disease
Abstract
Introduction: The consumption of trans fat is associated with cardiovascular disease (CVD). In January 2004, Denmark became the first country in the world to regulate the content of artificial trans fat in certain ingredients in food products, which nearly eliminated artificial trans fat from the Danish food supply. The goal of this study was to assess whether Denmark's trans fat policy reduced deaths caused by CVD.
Methods: Annual mortality rates in Organisation for Economic Co-operation and Development (OECD) countries from 1990 to 2012 were used to estimate the effect of Denmark's food policy on CVD mortality rates. Synthetic control methods were employed to simulate the CVD mortality trajectory that Denmark would have witnessed in the absence of the policy and to measure the policy's impact on CVD mortality rates. Analyses were conducted in 2015.
Results: Before the trans fat policy was implemented, CVD mortality rates in Denmark closely tracked those of a weighted average of other OECD countries (i.e., the synthetic control group). In the years before the policy, the annual mean was 441.5 deaths per 100,000 people in Denmark and 442.7 in the synthetic control group. In the 3 years after the policy was implemented, mortality attributable to CVD decreased on average by about 14.2 deaths per 100,000 people per year in Denmark relative to the synthetic control group.
Conclusions: Denmark's food policy, which restricted the content of artificial trans fat in certain ingredients in its food supply, has been followed by a decrease in CVD mortality rates.
Hospital Admissions for Myocardial Infarction and Stroke Before and After the Trans-Fatty Acid Restrictions in New York
Abstract
Importance Trans-fatty acids (TFAs) have deleterious cardiovascular effects. Restrictions on their use were initiated in 11 New York State (NYS) counties between 2007 and 2011. The US Food and Drug Administration plans a nationwide restriction in 2018. Public health implications of TFA restrictions are not well understood.
Objective To determine whether TFA restrictions in NYS counties were associated with fewer hospital admissions for myocardial infarction (MI) and stroke compared with NYS counties without restrictions.
Design, Setting, and Participants We conducted a retrospective observational pre-post study of residents in counties with TFA restrictions vs counties without restrictions from 2002 to 2013 using NYS Department of Health’s Statewide Planning and Research Cooperative System and census population estimates. In this natural experiment, we included those residents who were hospitalized for MI or stroke. The data analysis was conducted from December 2014 through July 2016.
Exposure Residing in a county where TFAs were restricted.
Main Outcomes and Measures The primary outcome was a composite of MI and stroke events based on primary discharge diagnostic codes from hospital admissions in NYS. Admission rates were calculated by year, age, sex, and county of residence. A difference-in-differences regression design was used to compare admission rates in populations with and without TFA restrictions. Restrictions were only implemented in highly urban counties, based on US Department of Agriculture Economic Research Service Urban Influence Codes. Nonrestriction counties of similar urbanicity were chosen to make a comparison population. Temporal trends and county characteristics were accounted for using fixed effects by county and year, as well as linear time trends by county. We adjusted for age, sex, and commuting between restriction and nonrestriction counties.
Results In 2006, the year before the first restrictions were implemented, there were 8.4 million adults (53.6% female) in highly urban counties with TFA restrictions and 3.3 million adults (52.3% female) in highly urban counties without restrictions. Twenty-five counties were included in the nonrestriction population and 11 in the restriction population. Three or more years after restriction implementation, the population with TFA restrictions experienced significant additional decline beyond temporal trends in MI and stroke events combined (−6.2%; 95% CI, −9.2% to −3.2%; P < .001) and MI (−7.8%; 95% CI, −12.7% to −2.8%; P = .002) and a nonsignificant decline in stroke (−3.6%; 95% CI, −7.6% to 0.4%; P = .08) compared with the nonrestriction populations.
Conclusions and Relevance The NYS populations with TFA restrictions experienced fewer cardiovascular events, beyond temporal trends, compared with those without restrictions.
Trans fat and cardiovascular disease mortality: Evidence from bans in restaurants in New York
Abstract
This paper analyzes the impact of trans fat bans on cardiovascular disease (CVD) mortality rates. Several New York State jurisdictions have restricted the use of ingredients containing artificial trans fat in food service establishments. The resulting within-county variation over time and the differential timing of the policy's rollout is used in estimation. The results indicate that the policy caused a 4.5% reduction in CVD mortality rates, or 13 fewer CVD deaths per 100,000 persons per year. The averted deaths can be valued at about $3.9 million per 100,000 persons annually.
Trans Fatty Acids and Cardiovascular Disease
The intake of trans fat has been associated with coronary heart disease, sudden death from cardiac causes, and diabetes. This article reviews the evidence for physiological and cellular effects of trans fatty acids, unsaturated fatty acids with at least one double bond in the trans configuration. The authors consider the feasibility and potential implications of reducing or eliminating the consumption of trans fatty acids from partially hydrogenated vegetable oils in the United States.
Greater Frequency of Fruit and Vegetable Consumption Is Associated With Lower Prevalence of Peripheral Artery Disease
Abstract
Objective—
Although fruit and vegetable (F&V) consumption is associated with lower risk of coronary heart disease and stroke, its association with peripheral artery disease (PAD) is less certain. We, thus, sought to characterize F&V intake and investigate the association between F&V consumption and presence of PAD in a large community sample.
Approach and Results—
Self-referred participants at >20 000 US sites who completed medical and lifestyle questionnaires were evaluated by screening ankle brachial indices for PAD (ankle brachial index ≤0.9). Among 3 696 778 individuals, mean age was 64.1±10.2 years and 64.1% were female. Daily consumption of ≥3 servings of F&V was reported by 29.2%. Increasing age, female sex, white race, never smoking, being currently married, physical activity, increasing income, and frequent consumption of fish, nuts, and red meat were positively associated with daily consumption of F&V. After multivariable adjustment, there was a stepwise inverse association between F&V intake and PAD. Participants reporting daily intake of ≥3 servings of F&V had 18% lower odds of PAD than those reporting less than monthly consumption. In unadjusted and multivariable-adjusted models, the inverse association with F&V became stronger as ankle brachial index decreased. When stratified by smoking status, the association was present only among those subjects who currently or formerly smoked tobacco.
Conclusions—
Our study demonstrates an inverse association of F&V consumption with prevalent PAD and overall low F&V consumption. These observations suggest the need to further efforts to increase F&V consumption and for more rigorous evaluation of the role of F&V in PAD prevention.
Mediterranean versus vegetarian diet for cardiovascular disease prevention (the CARDIVEG study): study protocol for a randomized controlled trial
Abstract
Background
Nutrition is able to alter the cardiovascular health of the general population. However, the optimal dietary strategy for cardiovascular disease prevention is still far from being defined. Mediterranean and vegetarian diets are those reporting the greatest grade of evidence in the literature, but no experimental studies comparing these two dietary patterns are available.
Methods/design
This is an open randomized crossover clinical trial including healthy subjects with a low-to-medium cardiovascular risk profile, characterized by being overweight and by the presence of at least an additional metabolic risk factor (abdominal obesity, high total cholesterol, high LDL cholesterol, high triglycerides, impaired glucose fasting levels) but free from medications. A total of 100 subjects will be included and randomly assigned to two groups: Mediterranean calorie-restricted diet (n = 50) and vegetarian calorie-restricted diet (n = 50). The intervention phases will last 3 months each, and at the end of intervention phase I the groups will be crossed over. The two diets will be isocaloric and of three different sizes (1400 – 1600 – 1800 kcal/day), according to specific energy requirements. Adherence to the dietary intervention will be established through questionnaires and 24-h dietary recall. Anthropometric measurements, body composition, blood samples and stool samples will be obtained from each participant at the beginning and at the end of each intervention phase. The primary outcome measure will be change in weight from baseline. The secondary outcome measures will be variations of anthropometric and bioelectrical impedance variables as well as traditional and innovative cardiovascular biomarkers.
Discussion
Despite all the data supporting the efficacy of Mediterranean and vegetarian diets on the prevention of cardiovascular diseases, no studies have directly compared these two dietary profiles. The trial will test whether there are statistically significant differences between these dietary profiles in reducing the cardiovascular risk burden for the general population.
Saturated Fat as Compared With Unsaturated Fats and Sources of Carbohydrates in Relation to Risk of Coronary Heart Disease: A Prospective Cohort Study
Abstract
Background
The associations between dietary saturated fat and risk of coronary heart disease (CHD) remain controversial, but few studies have compared saturated with unsaturated fats and sources of carbohydrates in relation to CHD risk.
Objective
This study sought to investigate associations of saturated fats as compared with unsaturated fats and different sources of carbohydrates in relation to CHD risk.
Methods
We followed 84,628 women (Nurses’ Health Study, 1980 to 2010), and 42,908 men (Health Professionals Follow-up Study, 1986 to 2010) who were free of diabetes, cardiovascular disease, and cancer at baseline. Diet was assessed by semiquantitative food frequency questionnaire every 4 years.
Results
During 24 to 30 years of follow-up, we documented 7,667 incident cases of CHD. Higher intakes of polyunsaturated fatty acids (PUFAs) and carbohydrates from whole grains were significantly associated with lower risk of CHD (hazard ratios [HR] (95% confidence intervals [CI]) comparing the highest to the lowest quintile for PUFA: 0.80 [0.73 to 0.88], p trend <0.0001; and for carbohydrates from whole grains: 0.90 [0.83 to 0.98], p trend = 0.003). In contrast, carbohydrates from refined starches/added sugars were positively associated with risk of CHD (1.10 [1.00 to 1.21], p trend = 0.04). Replacing 5% of energy intake from saturated fats with equivalent energy intake from either PUFAs, monounsaturated fats (MUFAs), or carbohydrates from whole grains was associated with 25%, 15%, and 9% lower risk of CHD, respectively (PUFAs: 0.75 [0.67 to 0.84]; p < 0.0001; MUFAs: 0.85 [0.74 to 0.97]; p = 0.02; carbohydrates from whole grains (0.91 [0.85 to 0.98]; p = 0.01). Replacing saturated fat with carbohydrates from refined starches/added sugars was not significantly associated with CHD risk (p > 0.10).
Conclusions
Our findings indicate that unsaturated fats, especially PUFAs, and/or high-quality carbohydrates should replace dietary saturated fats to reduce CHD risk.
Keywords: diet, follow-up studies, glycemic index
The portfolio diet for cardiovascular risk reduction
Abstract
Prompted by current dietary recommendations for the control of serum cholesterol to new targets to reduce the risk of coronary heart disease (CHD), and by the CHD risk reduction claims made for certain foods or food components, studies are now being undertaken using combinations of cholesterol-lowering foods in one diet (eg, a dietary portfolio) rather than single foods to achieve more effective dietary control of serum cholesterol. This approach has increased the potential relevance of dietary therapy and may yield nutrition strategies that bridge the gap between what is regarded as a good diet and drug therapy.
Effect of a Dietary Portfolio of Cholesterol-Lowering Foods Given at 2 Levels of Intensity of Dietary Advice on Serum Lipids in Hyperlipidemia
Abstract
Context Combining foods with recognized cholesterol-lowering properties (dietary portfolio) has proven highly effective in lowering serum cholesterol under metabolically controlled conditions.
Objective To assess the effect of a dietary portfolio administered at 2 levels of intensity on percentage change in low-density lipoprotein cholesterol (LDL-C) among participants following self-selected diets.
Design, Setting, and Participants A parallel-design study of 351 participants with hyperlipidemia from 4 participating academic centers across Canada (Quebec City, Toronto, Winnipeg, and Vancouver) randomized between June 25, 2007, and February 19, 2009, to 1 of 3 treatments lasting 6 months.
Intervention Participants received dietary advice for 6 months on either a low− saturated fat therapeutic diet (control) or a dietary portfolio, for which counseling was delivered at different frequencies, that emphasized dietary incorporation of plant sterols, soy protein, viscous fibers, and nuts. Routine dietary portfolio involved 2 clinic visits over 6 months and intensive dietary portfolio involved 7 clinic visits over 6 months.
Main Outcome Measures Percentage change in serum LDL-C.
Results In the modified intention-to-treat analysis of 345 participants, the overall attrition rate was not significantly different between treatments (18% for intensive dietary portfolio, 23% for routine dietary portfolio, and 26% for control; Fisher exact test, P = .33). The LDL-C reductions from an overall mean of 171 mg/dL (95% confidence interval [CI], 168-174 mg/dL) were −13.8% (95% CI, −17.2% to −10.3%; P < .001) or −26 mg/dL (95% CI, −31 to −21 mg/dL; P < .001) for the intensive dietary portfolio; −13.1% (95% CI, −16.7% to −9.5%; P < .001) or –24 mg/dL (95% CI, −30 to −19 mg/dL; P < .001) for the routine dietary portfolio; and −3.0% (95% CI, −6.1% to 0.1%; P = .06) or −8 mg/dL (95% CI, −13 to −3 mg/dL; P = .002) for the control diet. Percentage LDL-C reductions for each dietary portfolio were significantly more than the control diet (P < .001, respectively). The 2 dietary portfolio interventions did not differ significantly (P = .66). Among participants randomized to one of the dietary portfolio interventions, percentage reduction in LDL-C on the dietary portfolio was associated with dietary adherence (r = −0.34, n = 157, P < .001).
Conclusion Use of a dietary portfolio compared with the low−saturated fat dietary advice resulted in greater LDL-C lowering during 6 months of follow-up.
Trending Cardiovascular Nutrition Controversies
Abstract
The potential cardiovascular benefits of several trending foods and dietary patterns are still incompletely understood, and nutritional science continues to evolve. However, in the meantime, a number of controversial dietary patterns, foods, and nutrients have received significant media exposure and are mired by hype. This review addresses some of the more popular foods and dietary patterns that are promoted for cardiovascular health to provide clinicians with accurate information for patient discussions in the clinical setting.
Primary Prevention of Cardiovascular Disease with a Mediterranean Diet
Abstract
BACKGROUND
Observational cohort studies and a secondary prevention trial have shown an inverse association between adherence to the Mediterranean diet and cardiovascular risk. We conducted a randomized trial of this diet pattern for the primary prevention of cardiovascular events.
METHODS
In a multicenter trial in Spain, we randomly assigned participants who were at high cardiovascular risk, but with no cardiovascular disease at enrollment, to one of three diets: a Mediterranean diet supplemented with extra-virgin olive oil, a Mediterranean diet supplemented with mixed nuts, or a control diet (advice to reduce dietary fat). Participants received quarterly individual and group educational sessions and, depending on group assignment, free provision of extra-virgin olive oil, mixed nuts, or small nonfood gifts. The primary end point was the rate of major cardiovascular events (myocardial infarction, stroke, or death from cardiovascular causes). On the basis of the results of an interim analysis, the trial was stopped after a median follow-up of 4.8 years.
RESULTS
A total of 7447 persons were enrolled (age range, 55 to 80 years); 57% were women. The two Mediterranean-diet groups had good adherence to the intervention, according to self-reported intake and biomarker analyses. A primary end-point event occurred in 288 participants. The multivariable-adjusted hazard ratios were 0.70 (95% confidence interval [CI], 0.54 to 0.92) and 0.72 (95% CI, 0.54 to 0.96) for the group assigned to a Mediterranean diet with extra-virgin olive oil (96 events) and the group assigned to a Mediterranean diet with nuts (83 events), respectively, versus the control group (109 events). No diet-related adverse effects were reported.
CONCLUSIONS
Among persons at high cardiovascular risk, a Mediterranean diet supplemented with extra-virgin olive oil or nuts reduced the incidence of major cardiovascular events. (Funded by the Spanish government's Instituto de Salud Carlos III and others; Controlled-Trials.com number,
ISRCTN35739639
. opens in new tab
.)
Effect of a mediterranean type of diet on the rate of cardiovascular complications in patients with coronary artery disease insights into the cardioprotective effect of certain nutriments
Objectives.
We sought to describe the various cardiovascular complications that occurred in the Lyon Diet Heart Study (a secondary prevention trial testing the protective effects of a Mediterranean type of diet), to analyze their relations with the associated drug treatments and to gain insights into the possible mechanisms underlying the beneficial effects of certain nutriments.
Background.
Dietary habits are implicated in coronary heart disease, and the traditional Mediterranean diet is thought to be cardioprotective. However, the exact mechanisms of this protection are unknown.
Methods.
A total of 605 patients (303 control subjects and 302 study patients) were studied over a mean period of 27 months. Major primary end points (cardiovascular death and nonfatal acute myocardial infarction), secondary end points (including unstable angina, stroke, heart failure and embolisms) and minor end points (stable angina, need for myocardial revascularization, postangioplasty restenosis and thrombophlebitis) were analyzed separately and in combination.
Results.
When major primary and secondary end points were combined, there were 59 events in control subjects and 14 events in the study patients, showing a risk reduction of 76% (p < 0.0001). When these end points were combined with the minor end points, there were 104 events in control subjects and 68 events in the study patients, giving a risk reduction of 37% (p < 0.005). By observational analysis, only aspirin among the medications appeared to be significantly protective (risk ratio after adjustment for prognosis factors 0.45; 95% confidence interval 0.25 to 0.80).
Conclusions.
These data show a protective effect of the Mediterranean diet. However, the risk reduction varied depending on the type of end point considered. Our hypothesis is that different pathogenetic mechanisms were responsible for the development of the various complications. It is likely that certain nutriments characteristic of the Mediterranean diet (omega-3 fatty acids, oleic acid, antioxidant vitamins) have specific cardioprotective effects.
Comparison of the Atkins, Ornish, Weight Watchers, and Zone Diets for Weight Loss and Heart Disease Risk Reduction
Abstract
Context The scarcity of data addressing the health effects of popular diets is an important public health concern, especially since patients and physicians are interested in using popular diets as individualized eating strategies for disease prevention.
Objective To assess adherence rates and the effectiveness of 4 popular diets (Atkins, Zone, Weight Watchers, and Ornish) for weight loss and cardiac risk factor reduction.
Design, Setting, and Participants A single-center randomized trial at an academic medical center in Boston, Mass, of overweight or obese (body mass index: mean, 35; range, 27-42) adults aged 22 to 72 years with known hypertension, dyslipidemia, or fasting hyperglycemia. Participants were enrolled starting July 18, 2000, and randomized to 4 popular diet groups until January 24, 2002.
Intervention A total of 160 participants were randomly assigned to either Atkins (carbohydrate restriction, n=40), Zone (macronutrient balance, n=40), Weight Watchers (calorie restriction, n=40), or Ornish (fat restriction, n=40) diet groups. After 2 months of maximum effort, participants selected their own levels of dietary adherence.
Main Outcome Measures One-year changes in baseline weight and cardiac risk factors, and self-selected dietary adherence rates per self-report.
Results Assuming no change from baseline for participants who discontinued the study, mean (SD) weight loss at 1 year was 2.1 (4.8) kg for Atkins (21 [53%] of 40 participants completed, P = .009), 3.2 (6.0) kg for Zone (26 [65%] of 40 completed, P = .002), 3.0 (4.9) kg for Weight Watchers (26 [65%] of 40 completed, P < .001), and 3.3 (7.3) kg for Ornish (20 [50%] of 40 completed, P = .007). Greater effects were observed in study completers. Each diet significantly reduced the low-density lipoprotein/high-density lipoprotein (HDL) cholesterol ratio by approximately 10% (all P<.05), with no significant effects on blood pressure or glucose at 1 year. Amount of weight loss was associated with self-reported dietary adherence level (r = 0.60; P<.001) but not with diet type (r = 0.07; P = .40). For each diet, decreasing levels of total/HDL cholesterol, C-reactive protein, and insulin were significantly associated with weight loss (mean r = 0.36, 0.37, and 0.39, respectively) with no significant difference between diets (P = .48, P = .57, P = .31, respectively).
Conclusions Each popular diet modestly reduced body weight and several cardiac risk factors at 1 year. Overall dietary adherence rates were low, although increased adherence was associated with greater weight loss and cardiac risk factor reductions for each diet group.
Popular diets have become increasingly prevalent and controversial.
1
More than 1000 diet books are now available,
2
with many popular ones departing substantially from mainstream medical advice.
3
Cover stories for major news magazines, televised debates, and cautionary statements by prominent medical authorities
4
,
5
have fueled public interest and concern regarding the effectiveness and safety of such diets.
6
-
8
Although some popular diets are based on long-standing medical advice and recommend restriction of portion sizes and calories (eg, Weight Watchers),
9
a broad spectrum of alternatives has evolved. Some plans minimize carbohydrate intake without fat restriction (eg, Atkins diet),
10
many modulate macronutrient balance and glycemic load (eg, Zone diet),
11
and others restrict fat (eg, Ornish diet).
12
Given the growing obesity epidemic,
13
many patients and clinicians are interested in using popular diets as individualized eating strategies for disease prevention.
14
Unfortunately, data regarding the relative benefits, risks, effectiveness, and sustainability of popular diets have been limited.
15
-
25
We conducted a 1-year randomized trial of the dietary component of the Atkins, Zone, Weight Watchers, and Ornish plans, aiming to determine their realistic clinical effectiveness and sustainability for weight loss and cardiac risk factor reduction. Of note, this study only evaluated the dietary components and did not include other specific components that may be unique to each individual dietary program.
Effects of a Dietary Portfolio of Cholesterol-Lowering Foods vs Lovastatin on Serum Lipids and C-Reactive Protein
Abstract
Context To enhance the effectiveness of diet in lowering cholesterol, recommendations of the Adult Treatment Panel III of the National Cholesterol Education Program emphasize diets low in saturated fat together with plant sterols and viscous fibers, and the American Heart Association supports the use of soy protein and nuts.
Objective To determine whether a diet containing all of these recommended food components leads to cholesterol reduction comparable with that of 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors (statins).
Design Randomized controlled trial conducted between October and December 2002.
Setting and Participants Forty-six healthy, hyperlipidemic adults (25 men and 21 postmenopausal women) with a mean (SE) age of 59 (1) years and body mass index of 27.6 (0.5), recruited from a Canadian hospital-affiliated nutrition research center and the community.
Interventions Participants were randomly assigned to undergo 1 of 3 interventions on an outpatient basis for 1 month: a diet very low in saturated fat, based on milled whole-wheat cereals and low-fat dairy foods (n = 16; control); the same diet plus lovastatin, 20 mg/d (n = 14); or a diet high in plant sterols (1.0 g/1000 kcal), soy protein (21.4 g/1000 kcal), viscous fibers (9.8 g/1000 kcal), and almonds (14 g/1000 kcal) (n = 16; dietary portfolio).
Main Outcome Measures Lipid and C-reactive protein levels, obtained from fasting blood samples; blood pressure; and body weight; measured at weeks 0, 2, and 4 and compared among the 3 treatment groups.
Results The control, statin, and dietary portfolio groups had mean (SE) decreases in low-density lipoprotein cholesterol of 8.0% (2.1%) (P = .002), 30.9% (3.6%) (P<.001), and 28.6% (3.2%) (P<.001), respectively. Respective reductions in C-reactive protein were 10.0% (8.6%) (P = .27), 33.3% (8.3%) (P = .002), and 28.2% (10.8%) (P = .02). The significant reductions in the statin and dietary portfolio groups were all significantly different from changes in the control group. There were no significant differences in efficacy between the statin and dietary portfolio treatments.
Conclusion In this study, diversifying cholesterol-lowering components in the same dietary portfolio increased the effectiveness of diet as a treatment of hypercholesterolemia.
Most dietary manipulations result in modest cholesterol reductions of 4% to 13%,
1
-
10
and diet has been considered by some as a relatively ineffective therapy.
11
In contrast, 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors (statins) repeatedly have been shown to reduce mean serum low-density lipoprotein cholesterol (LDL-C) concentrations by 28% to 35% in long-term trials,
12
-
14
with corresponding reductions in cardiovascular death of 23% to 32% in both primary and secondary prevention trials.
13
,
14
Recently, to boost effectiveness of diet for primary prevention of cardiovascular disease, the Adult Treatment Panel (ATP III) of the National Cholesterol Education Program has recommended addition of plant sterols (2 g/d) and viscous fibers (10-25 g/d) to the diet.
15
The American Heart Association has also drawn attention to the possible benefits of soy proteins and the potential value of nuts.
In turn, the US Food and Drug Administration now permits health claims for coronary heart disease (CHD) risk reduction, based on cholesterol lowering, for foods delivering adequate amounts of plant sterols,viscous fibers (oat β-glucan and psyllium), and soy protein, and a health claim for nuts is being considered. Despite the large potential for cholesterol reduction, this dietary combination has never been compared directly with a statin. To assess the effectiveness of this dietary portfolio approach, we therefore studied a group of hyperlipidemic adults who were randomized to 1 of 3 treatments: the combination dietary portfolio, a diet lacking the additional active dietary ingredients but with a similar very low-saturated-fat content (control), or the same low-saturated-fat diet with addition of a statin.
Effects of Vegetarian Diets on Blood Lipids: A Systematic Review and Meta‐Analysis of Randomized Controlled Trials
Abstract
Background
Vegetarian diets exclude all animal flesh and are being widely adopted by an increasing number of people; however, effects on blood lipid concentrations remain unclear. This meta‐analysis aimed to quantitatively assess the overall effects of vegetarian diets on blood lipids.
Methods and Results
We searched PubMed, Scopus, Embase, ISI Web of Knowledge, and the Cochrane Library through March 2015. Studies were included if they described the effectiveness of vegetarian diets on blood lipids (total cholesterol, low‐density lipoprotein cholesterol, high‐density lipoprotein cholesterol, and triglyceride). Weighted mean effect sizes were calculated for net changes by using a random‐effects model. We performed subgroup and univariate meta‐regression analyses to explore sources of heterogeneity. Eleven trials were included in the meta‐analysis. Vegetarian diets significantly lowered blood concentrations of total cholesterol, low‐density lipoprotein cholesterol, high‐density lipoprotein cholesterol, and non–high‐density lipoprotein cholesterol, and the pooled estimated changes were −0.36 mmol/L (95% CI −0.55 to −0.17; P<0.001), −0.34 mmol/L (95% CI −0.57 to −0.11; P<0.001), −0.10 mmol/L (95% CI −0.14 to −0.06; P<0.001), and −0.30 mmol/L (95% CI −0.50 to −0.10; P=0.04), respectively. Vegetarian diets did not significantly affect blood triglyceride concentrations, with a pooled estimated mean difference of 0.04 mmol/L (95% CI −0.05 to 0.13; P=0.40).
Conclusions
This systematic review and meta‐analysis provides evidence that vegetarian diets effectively lower blood concentrations of total cholesterol, low‐density lipoprotein cholesterol, high‐density lipoprotein cholesterol, and non–high‐density lipoprotein cholesterol. Such diets could be a useful nonpharmaceutical means of managing dyslipidemia, especially hypercholesterolemia.
Keywords: cholesterol, diet, lipoprotein lipids, triglyceride, vegetarian
Vegetarian Diets and Blood Pressure
Abstract
Importance Previous studies have suggested an association between vegetarian diets and lower blood pressure (BP), but the relationship is not well established.
Objective To conduct a systematic review and meta-analysis of controlled clinical trials and observational studies that have examined the association between vegetarian diets and BP.
Data Sources MEDLINE and Web of Science were searched for articles published in English from 1946 to October 2013 and from 1900 to November 2013, respectively.
Study Selection All studies met the inclusion criteria of the use of (1) participants older than 20 years, (2) vegetarian diets as an exposure or intervention, (3) mean difference in BP as an outcome, and (4) a controlled trial or observational study design. In addition, none met the exclusion criteria of (1) use of twin participants, (2) use of multiple interventions, (3) reporting only categorical BP data, or (4) reliance on case series or case reports.
Data Extraction and Synthesis Data collected included study design, baseline characteristics of the study population, dietary data, and outcomes. The data were pooled using a random-effects model.
Main Outcomes and Measures Net differences in systolic and diastolic BP associated with the consumption of vegetarian diets were assessed.
Results Of the 258 studies identified, 7 clinical trials and 32 observational studies met the inclusion criteria. In the 7 controlled trials (a total of 311 participants; mean age, 44.5 years), consumption of vegetarian diets was associated with a reduction in mean systolic BP (−4.8 mm Hg; 95% CI, −6.6 to −3.1; P < .001; I2 = 0; P = .45 for heterogeneity) and diastolic BP (−2.2 mm Hg; 95% CI, −3.5 to −1.0; P < .001; I2 = 0; P = .43 for heterogeneity) compared with the consumption of omnivorous diets. In the 32 observational studies (a total of 21 604 participants; mean age, 46.6 years), consumption of vegetarian diets was associated with lower mean systolic BP (−6.9 mm Hg; 95% CI, −9.1 to −4.7; P < .001; I2 = 91.4; P < .001 for heterogeneity) and diastolic BP (−4.7 mm Hg; 95% CI, −6.3 to −3.1; P < .001; I2 = 92.6; P < .001 for heterogeneity) compared with the consumption of omnivorous diets.
Conclusions and Relevance Consumption of vegetarian diets is associated with lower BP. Such diets could be a useful nonpharmacologic means for reducing BP.
The relationship between blood pressure (BP) and cardiovascular disease risk is continuous, consistent, and independent of other risk factors.
1
According to Lewington et al,
2
in individuals aged 40 to 70 years, each increment of 20 mm Hg in systolic BP or 10 mm Hg in diastolic BP is associated with more than twice the risk of cardiovascular disease across the BP range from 115/75 to 185/115 mm Hg.
A substantial body of evidence supports the role of modifiable factors, including diet, body weight, physical activity, and alcohol intake, in the risk of developing hypertension.
3
Dietary modifications have been shown
3
to be particularly effective in preventing and managing hypertension.
Vegetarian diets are defined as dietary patterns that exclude or rarely include meats; some vegetarian diets include dairy products, eggs, and fish. All vegetarian diets emphasize foods of plant origin, particularly vegetables, grains, legumes, and fruits. In observational studies,
4
,
5
consumption of vegetarian diets is associated with a lower prevalence of hypertension. Although some randomized clinical trials
6
,
7
have found that adoption of a vegetarian diet reduces BP, others
8
,
9
have not yielded similar results. To our knowledge, the available evidence regarding the association between vegetarian diets and BP has not been subjected to meta-analysis. To clarify the nature of this association and provide a valid estimate of the effect size regarding the effects of consumption of vegetarian diets on BP, both of which could prove useful in formulating dietary guidance, we performed a meta-analysis of studies that had examined associations between vegetarian diets and BP.
Dental Health
The Impact of Diet, Nutrition and Nutraceuticals on Oral and Periodontal Health
Abstract
Oral and periodontal diseases can determine severe functional, phonatory and aesthetic impairments and are the main cause of adult tooth loss. They are caused by some specific bacteria that provoke an intense local inflammatory response and affect-with particular gravity-susceptible subjects, because of reasons related to genetics and lifestyles (e.g., smoking and home oral hygiene habits). They are more frequent in the disadvantaged segments of society and, in particular, in subjects who have difficulty accessing preventive services and dental care. Some systemic diseases, such as uncontrolled diabetes, can increase their risk of development and progression. Recently, in addition to the obvious considerations of severe alterations and impairments for oral health and well-being, it has been noted that periodontitis can cause changes in the whole organism. Numerous clinical and experimental studies have highlighted the presence of a strong association between periodontitis and some systemic diseases, in particular, cardiovascular diseases, diabetes, lung diseases and complications of pregnancy. The purpose of this editorial is to provide a current and thoughtful perspective on the relationship of diet and natural agents on oral, periodontal diseases, and chewing disorder preventions which may reflect good systemic conditions and related quality of life or to analyze indirect effects through the contribution of diet and nutrition to systemic health in order to obtain a modern diagnostic-therapeutic approach.
The Association of Poor Oral Health Parameters with Malnutrition in Older Adults: A Review Considering the Potential Implications for Cognitive Impairment
Abstract
Poor dental status and chewing deficiencies have been associated with cognitive decline. Altered dietary habits and malnutrition have been suggested as linking mechanisms. The aim of the present review was thus to investigate if poor oral health, and in particular tooth loss and impaired masticatory function, may affect dietary selection and nutritional intake in older adults, and moreover, to assess if prosthodontic dental care may improve nutritional status. Extensive tooth loss may impair masticatory function. Several studies in older populations have shown that severe tooth loss and masticatory impairment are associated with limited consumption of various food types (especially fruits and vegetables), increased consumption of sugary and easy-to-chew foods, and lower dietary intake of fibre and vitamins. However, these findings are not consistently reported, due to methodological variation among studies, potential adverse causalities, and the multifactorial nature of food choices. On the other hand, a few interventional studies revealed that prosthetic rehabilitation of missing teeth, when accompanied by dietary counselling, may improve dietary habits and nutritional intake. Further research is required to improve current knowledge of these associations. Under the limitations of the current study, a functional dental arch of natural or artificial teeth is important for maintaining adequate chewing efficiency and ability, but this only partly contributes to food choices and nutritional status. The multifactorial nature of food choices necessitates the interprofessional collaboration of dental professionals, dietetics practitioners, and primary care providers to improve dietary habits and nutritional intake.
Associations between oral hygiene habits, diet, tobacco and alcohol and risk of oral cancer: A case-control study from India
Abstract
Objective: This study examines the association between the incidence of oral cancer in India and oral hygiene habits, diet, chewing and smoking tobacco, and drinking alcohol. We also assessed the effects of oral hygiene habits with oral cancer risk among chewers versus never chewers.
Methods: A hospital-based case-control study was conducted in Pune, India, based on face-to-face interviews, anthropometry, and intra-oral examinations conducted for 187 oral cancer cases and 240 controls.
Results: Poor oral hygiene score was associated with a significant risk of oral cancer (adjusted OR=6.98; 95%CI 3.72-13.05). When stratified by tobacco-chewing habit, the poor oral hygiene score was a significant risk factor only among ever tobacco chewers (adjusted OR=14.74; 95%CI 6.49-33.46) compared with never chewers (adjusted OR=0.71; 95%CI 0.14-3.63). Dental check-ups only at the time of pain by ever-chewers with poor oral hygiene was associated with an elevated risk (adjusted OR=4.22; 95%CI 2.44-7.29), while consumption of green, yellow, and cruciferous vegetables and citrus fruits was protective. A linear dose-response association was observed between oral cancer and chewing tobacco in terms of age at initiation, duration, and frequency of chewing per day (P<0.001). Smoking more than 10 bidis/cigarettes per day (adjusted OR=2.74; 95%CI 1.28-5.89) and for a duration >25 years (adjusted OR=2.31; 95%CI 1.14-4.71) elevated the risk of oral cancer.
Conclusion: Good oral hygiene habits - as characterized by healthy gums, brushing more than once daily, use of toothpaste, annual dental check-ups, and a minimal number of missing teeth - can reduce the risk of oral cancer significantly. In addition to refraining from chewing/smoking tobacco, a diet adequate in fruits and vegetables may protect against the disease.
Oral health-related quality of life in patients with disorders of nutrition
Abstract
Background: Researchers demonstrated a correlation between nutrition and health-related quality of life (HRQoL). Little is known about the correlation between disorders of nutrition (DON) and Oral HRQoL (OHRQoL).
Objectives: (a) To measure OHRQoL in DON patients compared to patients attending nutritional counselling for other reasons (eg, systemic diseases or general dietary counselling) (NCOR) and to healthy controls attending routine dental screenings. (b) To analyse associations between OHRQoL and demographics, health-related behaviours and nutritional practices. We hypothesised that OHRQoL is impaired in DON patients and correlates with poor health-related behaviours and nutritional practices METHODS: Demographic, smoking, alcohol and physical activity habits, verbal pain scale, oral health impact profile-14 (OHIP-14) and nutritional practice data were collected from 63 DON, 35 NCOR and 100 controls.
Results: Compared to controls, DON patients exhibited poorer OHIP-14 global scores and had more functional limitation, physical disability, psychological disability, social disability and handicap. OHIP-14 global score was positively associated with maternal origin, oral symptoms, eggs and eggplant consumption, avoiding seasoning, hot drinks and fibrous food and negatively associated with physical activity and fresh vegetable consumption. In the conceptual hierarchical multiple regression model, verbal pain scale, eggplant consumption and physical activity were mediators in the relationship between DON and OHIP-14. DON, physical activity and eggplant consumption also directly associated with OHRQoL.
Conclusions: Oral HRQoL was impaired in DON patients and correlated with poor health-related behaviours and nutritional practices. Routine workup of DON patients should include OHRQoL assessment.
Prospective study of fruits and vegetables and risk of oral premalignant lesions in men
Abstract
The authors prospectively evaluated fruit and vegetable consumption and the incidence of oral premalignant lesions among 42,311 US men in the Health Professionals Follow-up Study. Diet was assessed every 4 years by food frequency questionnaires. The authors confirmed 207 cases of clinically or histopathologically diagnosed oral premalignant lesions occurring between 1986 and 2002. Multivariate-adjusted relative risks were calculated from proportional hazards models. Significant inverse associations were observed with citrus fruits, citrus fruit juice, and vitamin-C-rich fruits and vegetables, indicating 30-40% lower risks with greater intakes (e.g., citrus fruit juice quintile 5 vs. quintile 1 relative risk = 0.65, 95% confidence interval: 0.42, 0.99). Inverse associations with fruits did not vary by smoking status and were stronger in analyses of baseline consumption, with a 10-year lag time to disease follow-up (quintile 5 vs. quintile 1 relative risk = 0.41, 95% confidence interval: 0.20, 0.82; p = 0.01). No associations were observed with total vegetables or with beta-carotene-rich or lycopene-rich fruits and vegetables. For current smokers, green leafy vegetables (ptrend = 0.05) and beta-carotene-rich fruits and vegetables (ptrend = 0.02) showed significant linear trends of increased risk (one additional serving/day relative risk = 1.7). The risk of oral premalignant lesions was significantly reduced with higher consumption of fruits, particularly citrus fruits and juices, while no consistent associations were apparent for vegetables.
Association between oral health status and future dietary intake and diet quality in older men: The PRIME study
Abstract
Objectives: This study investigated whether oral health status, defined as number of natural teeth and subsequent prosthodontic rehabilitation, was associated with future dietary intake and diet quality in older adults in The Prospective Epidemiological Study of Myocardial Infarction (PRIME).
Methods: PRIME was originally established to explore cardiovascular risk factors in 50-59 year old men in Northern Ireland (1991-1994). A rescreening phase assessed oral health (2001-2004), while diet was assessed in 2015. Diet quality was characterised by the Dietary Diversity Score and Mediterranean Diet Score. In the current analysis, associations between oral health status, dietary intake and quality were assessed using regression models in 1096 participants.
Results: Amongst study participants, the overall mean number of teeth was 18.5, 51.5 % had ≥21 natural teeth and 49.6 % wore dentures. Oral health status was categorised into five groups: 21-28 teeth with (n = 111) and without (n = 453) dentures, 1-20 teeth with (n = 354) and without (n = 99) dentures and edentate with dentures (n = 79). After full adjustment, men with ≥21 teeth and dentures had a higher future intake of fruit, vegetables, and nuts, and diet quality scores, compared to those with <21 teeth with dentures. Edentate men with dentures were less likely to achieve the future fruit dietary recommendation.
Conclusions: Having ≥21 natural remaining teeth positively affected the future intake of fruit, vegetables, and nuts, as well as diet quality. Dentures may be beneficial in men with ≥21 natural remaining teeth, as they were associated with an increased future intake of fruit, vegetables, and nuts and better diet quality.
Clinical significance: Oral health status is associated with dietary intake, after an average time period of 13 years, with those with a larger number of natural teeth having a better diet quality. Further research is required to investigate this relationship in larger, diverse populations with more detailed dietary assessment.
Frailty, oral health and nutrition in geriatrics inpatients: A cross-sectional study
Abstract
Background: Poor nutritional status is a risk factor for the development of frailty. Likewise, oral health is independently associated with nutrition. The potential association between oral health and frailty in hospitalised elderly adults has, however, not previously been investigated.
Objective: To investigate the relationship between oral health and frailty in hospitalised elderly adults and to identify the predictors of frailty.
Method: A cross-sectional study of 168 geriatric inpatients >65 years old was performed from August to December 2016. Patients of non-English speaking background, with impaired cognition (MMSE <24), severe hearing or visual impairment or active delirium were excluded. Oral health, nutrition and frailty were assessed using previously validated tools, namely the Geriatric Oral Health Assessment Index (GOHAI), Mini Nutrition Assessment (MNA) and Reported Edmonton Frailty Scale (REFS). Other data collected included demographics, co-morbidities, level of education and smoking/alcohol history.
Results: On univariate analysis, the REFS score decreased with better nutritional status/higher MNA (P < 0.001) and better self-reported oral health/higher GOHAI (P = 0.023). Nutritional status accounted for 17% of variability in frailty assessment. On multivariate analysis, co-morbidities (P < 0.001), MNA (P < 0.001) and living in residential care (P < 0.001) were independent predictors of frailty. After adjusting for nutrition and co-morbidities, self-reported oral health was found to have an independent negative association with frailty (P = 0.019).
Conclusion: Poor self-reported oral health was found to be independently associated with frailty. Further research should be directed at whether interventions to maintain good oral health can prevent or slow the progression of frailty.
State of dental health of children in uzhhorod and the way of their nutrition
Abstract
Objective: The aim: To study and evaluate the condition of the dental health of children of school age and the characteristics of their food.
Patients and methods: Materials and methods: Statistics on the dental health of children in Transcarpathian region for the years 2009-2018 were analyzed with the application of statistical, sociological and clinical methods and the data on dental health and way of nutrition of 163 children in Uzhgorod were determined and analyzed.
Results: Results and conclusions: Reduction of 28.9% of coverage of children with preventive dental examinations was determined with the need for mouth cavity sanation of 45.93%. Redevelopment was held for 91.7% of those who needed help. From 10% to 50% of the examined children in different age groups have caries. Up to 10% of children between 11 and 15 years old have teeth removed. It was determined that nutrition of children with caries diagnosed is not rational.
The Role of Nutrition in Periodontal Health: An Update
Abstract
Periodontal health is influenced by a number of factors such as oral hygiene, genetic and epigenetic factors, systemic health, and nutrition. Many studies have observed that a balanced diet has an essential role in maintaining periodontal health. Additionally, the influences of nutritional supplements and dietary components have been known to affect healing after periodontal surgery. Studies have attempted to find a correlation between tooth loss, periodontal health, and nutrition. Moreover, bone formation and periodontal regeneration are also affected by numerous vitamins, minerals, and trace elements. The aim of this review is to critically appraise the currently available data on diet and maintenance of periodontal health and periodontal healing. The effects of nutritional intervention studies to improve the quality of life and well-being of patients with periodontal disease have been discussed.
Prevention of dental caries by grape seed extract supplementation: A systematic review
Abstract
Background: Dental caries are the most prominent chronic disease of children and adults worldwide, and facilitating evidence-based, preventative care for their prevention is critical. Caries are traditionally and successfully prevented by regular fluoride use, but there are opportunities to halt and restore caries with alternative agents in addition to fluoride use. Grape seed extract (GSE) is a readily available plant-based supplement that, due to its concentrated levels of proanthocyanidins, has promising characteristics that may assist in dental caries prevention.
Aim: The goal of this review was to investigate whether current research supports use of grape seed extract to prevent dental caries formation.
Methods: A systematic review of articles related to grape seed extract, prevention of dental caries, inhibition of Streptococcus mutans, and remineralization was conducted. Articles were first chosen by inclusion of dental models that used grape seed extract as an intervention, and then by strength of study design.
Results: Twenty articles were reviewed. Studies overall supported three unique grape seed extract properties facilitating dental caries prevention. In the first articles reviewed, grape seed extract inhibited proliferation of bacterial biofilms on tooth surfaces. In addition, studies reviewed indicated that grape seed extract promoted dental remineralization.
Conclusions: Caries prevention by grape seed extract may be unique compared with fluoride, and is linked to grape seed extract's bacteriostatic and collagen crosslinking properties. Future research should investigate potential delivery methods, and benefits of combined grape seed extract use with known caries preventative agents, in human participants.
Effects of raw vegan diet on periodontal and dental parameters
Abstract
Objectives: Macronutrients and micronutrients present in different types of diet could influence different aspects of both inflammatory and immune responses; thereby, diets could influence oral health and the periodontal condition. The raw vegan diet is a subset of vegetarianism in which only uncooked plant-derived foods are consumed. The present study's aim was to evaluate the effect of the raw vegan diet on periodontal and dental health parameters.
Materials and methods: A total of 118 participants (59 raw vegans and 59 controls) were interviewed about their level of education and oral health habits. Samples of unstimulated whole saliva were collected for pH analysis, and dental and periodontal parameters were examined. Then, statistical analysis was performed.
Results: Raw vegans had better oral hygiene (P = 0.001). The decayed-missing-filling indices were relatively equal in both groups. The probing depth, bleeding on probing (BOP), and simplified oral hygiene index were significantly lower in raw vegans (P = 0.047, P = 0.017, and P = 0.001, respectively). Multiple regression analyses disclosed that probing depth and BOP were significantly related to debris index.
Conclusion: Based on this study's results, it can be presumed that the better periodontal condition in raw vegans is a result of their better oral care and lifestyle.
Plant-based milks: the dental perspective
Abstract
Background Consumption of plant-based milk in the UK is increasing at the expense of cow's milk. Cow's milk consumption has traditionally been advocated by the dental profession as 'good for teeth'.Aims To identify the range of plant-based milks available in the UK and compare their nutritional benefits with cow's milk. A secondary aim was to explore reasons behind the increase in popularity of plant-based milks and discuss dental relevance.Methods Branded plant-based milks available in UK supermarkets were identified and nutritional data collected. Data were obtained from product labelling and manufacturer websites. The sample was collected in December 2019.Results Eighty-two products were identified. Differences were observed between plant-based and cow's milk, in particular regarding calcium, iodine, vitamin B12 and sugar content. Sugar content varied from 0-7.6 g/100 ml.Conclusions Dairy is a key source of dietary iodine and many plant-based milks contain much lower levels. Many plant-based milks contain free sugars which are cariogenic. Dentists should be aware of this emerging market and be able to advise patients accordingly.
Oral health in a cohort of individuals on a plant-based diet: a pilot study
Abstract
Introduction: Plant-based diets are associated with a lower: (i) body mass index, (ii) rates of death from ischemic heart disease, (iii) serum cholesterol, (iv) incidence of high blood pressure, (v) type II diabetes mellitus and cancer, with an overall longer life expectancy. However, little data concerning the oral health in individuals on a plant-based diet are available.
Aim: The aim of the present study was to investigate the general and clinical oral health status in a cohort of adults who had been following a plant-based diet for a minimum of 24 months.
Material and methods: For this purpose, individuals were administered two questionnaires (a.Questionnaire investigating risk areas for oral diseases; b. Italian version of the Oral Health Impact Profile -14 (IOHIP-14)) by a dental hygienist and clinical examination of the oral cavity was carried out.
Results: Seventy-seven adult individuals were enrolled. On average, they followed a plant-based diet for the last four years, had four meals a day and brushed their teeth twice a day. Fruit was the most frequently consumed food at breakfast by 48 of the participants. Thirty-four responders did not drink beer or wine, 65 did not drink spirits, 57 avoided carbonated beverages and 62 (80.5%) did not consume any highly-sugared beverages. Different dental therapies in the previous three years were reported in 36 of the responders. Overall, answers "never and almost never" to the IOHIP-14 questionnaire were observed in 87% to 100% of the individuals. Multiple logistic regression analysis revealed that fresh fruit consumption at lunch had a protective effect against caries (p<0.05).
Conclusions: In conclusion, this study showed that individuals on a plant-based diet have good overall oral health conditions. These features are in agreement with the behavior of these subjects towards an overall healthy life style.
Arthritis
The effects of the Mediterranean diet on rheumatoid arthritis prevention and treatment: a systematic review of human prospective studies
Abstract
Rheumatoid arthritis is a progressive autoimmune disease characterised by severely swollen and painful joints. To compliment pharmacotherapy, people living with rheumatoid arthritis often turn to dietary interventions such as the Mediterranean diet. The aim of the present systematic review is to discuss the effects of the Mediterranean diet on the management and prevention of rheumatoid arthritis in human prospective studies. Four studies met the inclusion criteria, including two intervention studies reporting improvement in the pain visual analogue scale (p < 0.05) and a decrease in the health assessment questionnaire for rheumatoid arthritis score (p < 0.05) in the Mediterranean diet groups. Only one study reported a reduction in the 28 joint count disease activity score for rheumatoid arthritis for the Mediterranean diet group (p < 0.05). This review has identified beneficial effects of the Mediterranean diet in reducing pain and increasing physical function in people living with rheumatoid arthritis. However, there is currently insufficient evidence to support widespread recommendation of the Mediterranean diet for prevention of rheumatoid arthritis.
Nutrition and fasting mimicking diets in the prevention and treatment of autoimmune diseases and immunosenescence
Abstract
Complex and coordinated signals are necessary to initiate and sustain the activation, proliferation, and differentiation of lymphocytes. These signals, which are known to determine T-cell fate and function, also depend on the metabolic state of the organism. Recent studies indicate that both the type and levels of nutrients can influence the generation, survival and function of lymphocytes and therefore can affect several autoimmune diseases. Here, we review the dysregulation of lymphocytes during autoimmunity and aging, the mechanisms associated with loss of immune function, and how fasting mimicking diets and other dietary interventions affect autoimmunity and immunosenescence.
Abstract
Although turmeric and its curcumin-enriched extracts have been used for treating arthritis, no systematic review and meta-analysis of randomized clinical trials (RCTs) have been conducted to evaluate the strength of the research. We systemically evaluated all RCTs of turmeric extracts and curcumin for treating arthritis symptoms to elucidate the efficacy of curcuma for alleviating the symptoms of arthritis. Literature searches were conducted using 12 electronic databases, including PubMed, Embase, Cochrane Library, Korean databases, Chinese medical databases, and Indian scientific database. Search terms used were "turmeric," "curcuma," "curcumin," "arthritis," and "osteoarthritis." A pain visual analogue score (PVAS) and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) were used for the major outcomes of arthritis. Initial searches yielded 29 articles, of which 8 met specific selection criteria. Three among the included RCTs reported reduction of PVAS (mean difference: -2.04 [-2.85, -1.24]) with turmeric/curcumin in comparison with placebo (P < .00001), whereas meta-analysis of four studies showed a decrease of WOMAC with turmeric/curcumin treatment (mean difference: -15.36 [-26.9, -3.77]; P = .009). Furthermore, there was no significant mean difference in PVAS between turmeric/curcumin and pain medicine in meta-analysis of five studies. Eight RCTs included in the review exhibited low to moderate risk of bias. There was no publication bias in the meta-analysis. In conclusion, these RCTs provide scientific evidence that supports the efficacy of turmeric extract (about 1000 mg/day of curcumin) in the treatment of arthritis. However, the total number of RCTs included in the analysis, the total sample size, and the methodological quality of the primary studies were not sufficient to draw definitive conclusions. Thus, more rigorous and larger studies are needed to confirm the therapeutic efficacy of turmeric for arthritis.
Abstract
Accumulating research evidence suggests that individual dietary factors and dietary patterns might be implicated in the risk of development of rheumatoid arthritis (RA). This narrative review aims to present this evidence and provide nutritional recommendations for reducing RA risk in susceptible individuals. Overall, a 'Western' type diet rich in energy intake, total and saturated fat, an unbalanced ratio of n-3 to n-6 fatty acids, high in refined carbohydrates and sugar and low in fiber and antioxidants might increase the risk of RA both directly through increasing inflammation and indirectly through increasing insulin resistance and obesity, with the latter being a known risk factor for RA. On the contrary, consumption of long-chain omega-3 polyunsaturated fatty acids, derived from fish and fish oil, is associated with a reduced risk of RA probably due to their anti-inflammatory properties. The Mediterranean diet (MD), rich in plant-based foods such as wholegrains, legumes, fruit, vegetables, extra-virgin olive oil and low in red meat consumption, might have the potential to reduce the risk of RA. Based on current research evidence, it is suggested that adherence to the MD enhanced with an increased consumption of fatty fish, reduced consumption of sugar-sweetened drinks and maintenance of a normal body weight, contributes to reducing the risk of RA. Further research on RA susceptibility will allow for more specific dietary recommendations to be made.
Dietary Habits and Nutrition in Rheumatoid Arthritis: Can Diet Influence Disease Development and Clinical Manifestations?
Abstract
Rheumatoid arthritis (RA) is a systemic, autoimmune disease characterized by joint involvement, with progressive cartilage and bone destruction. Genetic and environmental factors determine RA susceptibility. In recent years, an increasing number of studies suggested that diet has a central role in disease risk and progression. Several nutrients, such as polyunsaturated fatty acids, present anti-inflammatory and antioxidant properties, featuring a protective role for RA development, while others such as red meat and salt have a harmful effect. Gut microbiota alteration and body composition modifications are indirect mechanisms of how diet influences RA onset and progression. Possible protective effects of some dietary patterns and supplements, such as the Mediterranean Diet (MD), vitamin D and probiotics, could be a possible future adjunctive therapy to standard RA treatment. Therefore, a healthy lifestyle and nutrition have to be encouraged in patients with RA.
The impact of nutrition and generally available products such as nicotine and alcohol on rheumatoid arthritis – review of the literature
Abstract
Nutrition habits and diet may influence disease development and course. There are no specific recommendations related to rheumatic diseases for a diet that would facilitate treatment. However, some research results suggest that various nutrients may affect the health of patients, especially in the case of inflammatory rheumatic disease such as rheumatoid arthritis (RA). Scientists have been trying to find a relation between inflammatory rheumatic diseases and diet but have never come up with any firm conclusions that would help in determining the model of a diet for such patients. Nevertheless, there are some consistent results that refer to the influence of nutritional behaviours on symptoms of RA. The article presents a review of the research showing that certain nutrients may be beneficial for the course of disease among some RA patients.
Don’t neglect nutrition in rheumatoid arthritis!
State of knowledge
Nutrients and immune-inflammatory response in RA
Rheumatoid arthritis (RA) is characterised by a systemic immune-inflammatory response, in genetically susceptible individuals exposed to environmental and endogenous triggers, including specific nutrients.1 The major pathways in RA are characterised by an intense inflammatory response, involving impaired immunoregulatory processes and the production of different proinflammatory mediators.2 Research on possible risk factors has traditionally focused on triggers setting off disease, such as microbial/viral agents, cigarette smoking and environmental pollution, hormonal imbalance and chronic stress, but with less focus in the past few decades on nutritional factors that can influence disease onset, progression and outcomes, possibly through epigenetic mechanisms.2
More recently, simple and daily dietary factors have been implicated in the development of RA, even directly through triggering inflammatory pathways: for example, the recent evidence that increased sodium chloride salt (figure 1), activates proinflammatory macrophages (M1), Th17 cells and decrease T-regulator cells, all crucial players in RA pathogenesis.3 In addition, sodium excretion was recently found higher in patients with early RA than in matched controls.4
Comorbidities of rheumatoid arthritis: Results from the Korean National Health and Nutrition Examination Survey
Abstract
This study aimed to evaluate the prevalence of comorbidities in patients with rheumatoid arthritis (RA) compared with the non-RA population. The 2010–2012 Korea National Health and Nutrition Examination Survey (KNHANES), which assesses the general health status of populations in South Korea using interviews and basic health assessment, was analyzed retrospectively. Weighted prevalence and odds ratio (OR) of comorbidities were analyzed in patients with RA compared with the non-RA population. The overall weighted (n = 37,453,158) prevalence of RA was 1.5%. Patients with RA were older and more female predominant than subjects without RA. The prevalence of living in an urban area, college graduation, alcohol consumption and smoking was lower in patients with RA than non-RA. Patients with RA had more comorbidities including hypertension, dyslipidemia, myocardial infarction (MI) or angina, stoke, osteoarthritis, lung cancer, colon cancer, pulmonary tuberculosis, asthma, diabetes, depression, thyroid disease and chronic kidney disease. After adjusting socioeconomic and lifestyle characteristics, RA was associated with an increased prevalence of MI or angina (OR 1.86, 95% CI 1.17–2.96, p = 0.009), pulmonary TB (OR 1.95, 95% CI 1.24–3.09, p = 0.004), asthma (OR 1.97, 95% CI 1.05–3.71, p = 0.036), thyroid disease (OR 1.71, 95% CI 1.05–2.77), depression (OR 2.38, 95% CI 1.47–3.85, p < 0.001) and hepatitis B (OR 2.34, 95% CI 1.15–4.80, p = 0.020) compared with the non-RA population. Prevalence of solid cancer was not significantly associated with RA after adjustment
Nutrition Interventions in Rheumatoid Arthritis: The Potential Use of Plant-Based Diets. A Review
Rheumatoid arthritis (RA), a chronic inflammatory autoimmune disease, affects roughly 1% of the world's population. RA pathogenesis remains unclear, but genetic factors account for 50–60% of the risk while the remainder might be linked to modifiable factors, such as infectious diseases, tobacco smoking, gut bacteria, and nutrition. Dietary triggers may play an inciting role in the autoimmune process, and a compromised intestinal barrier may allow food components or microorganisms to enter the blood stream, triggering inflammation. In addition, excessive body weight may affect pharmacotherapy response and the likelihood of disease remission, as well as the risk of disease mortality. Evidence suggests that changes in diet might play an important role in RA management and remission. Several studies have shown improvements in RA symptoms with diets excluding animal products. Studies have also shown that dietary fiber found in these plant-based foods can improve gut bacteria composition and increase bacterial diversity in RA patients, thus reducing their inflammation and joint pain. Although some of the trigger foods in RA patients are individualized, a vegan diet helps improve symptoms by eliminating many of these foods. This review examines the potential role of a plant-based diet in mediating RA symptoms. Further research is needed to test the effectiveness of plant-based diets on joint pain, inflammation, and quality of life in patients with RA.
Are we really what we eat? Nutrition and its role in the onset of rheumatoid arthritis
Abstract
Accumulating research evidence suggests that individual dietary factors and
dietary patterns
might be implicated in the risk of development of
rheumatoid arthritis
(RA). This narrative review aims to present this evidence and provide nutritional recommendations for reducing RA risk in susceptible individuals. Overall, a ‘Western’ type diet rich in
energy intake
, total and
saturated fat
, an unbalanced ratio of n-3 to
n-6 fatty acids
, high in refined carbohydrates and sugar and low in fiber and antioxidants might increase the risk of RA both directly through increasing inflammation and indirectly through increasing insulin resistance and obesity, with the latter being a known risk factor for RA. On the contrary, consumption of long-chain omega-3 polyunsaturated fatty acids, derived from fish and fish oil, is associated with a reduced risk of RA probably due to their anti-inflammatory properties. The Mediterranean diet (MD), rich in plant-based foods such as wholegrains, legumes, fruit, vegetables,
extra-virgin olive oil
and low in red meat consumption, might have the potential to reduce the risk of RA. Based on current research evidence, it is suggested that adherence to the MD enhanced with an increased consumption of fatty fish, reduced consumption of sugar-sweetened drinks and maintenance of a normal body weight, contributes to reducing the risk of RA. Further research on RA susceptibility will allow for more specific dietary recommendations to be made.
The therapeutic effect of probiotics on rheumatoid arthritis: a systematic review and meta-analysis of randomized control trials
Abstract
Rheumatoid arthritis is an autoimmune disease in which probiotics appears to have an immune modulating action along with decreased inflammatory process. Therefore, we aim to investigate the efficacy of probiotics as an adjuvant therapy for rheumatoid arthritis. A comprehensive literature search was performed using nine databases including PubMed and Web of Science. Interesting data was extracted and meta-analyzed. We assessed the risk of bias using Cochrane Collaboration's tool. The protocol was registered in PROSPERO (CRD 42016036769). We found nine studies involving 361 patients who met our eligibility criteria. Our meta-analysis indicated that pro-inflammatory cytokine IL-6 was significantly lower in the probiotics compared with the placebo group (standardized mean difference = - 0.708; 95% confidence interval (CI) - 1.370 to 0.047, P = 0.036). However, there was no difference between probiotics and placebo in disease activity score (mean difference 0.023; 95% CI - 0.584 to 0.631, P = 0.940). Probiotics lowered pro-inflammatory cytokines IL-6 in RA; however, its clinical effect is still unclear. Hence, many high-quality randomized controlled trials (RCTs) are still needed to prove this effect.
Keywords: Cytokines; Disease activity score; Meta-analysis; Probiotics; Rheumatoid arthritis; Systematic review.
Microbiome and probiotics: link to arthritis
Abstract
Purpose of review: The gut microbiome plays an integral role in the development and maintenance of the host immune system. Expanding knowledge about this microbial microenvironment has raised the possibility of new treatments based on this knowledge. In this review, we describe the recent evidence of the impact of the gut microbiome on arthritis and possible novel therapeutic approaches to alter the gut flora.
Recent findings: Recent studies support the growing evidence of microbiome as a causative agent underlying certain rheumatic diseases like ankylosing spondylitis and rheumatoid arthritis. There is intriguing yet still inconclusive evidence to support the use of probiotics as a treatment for these diseases.
Summary: There is recently a new level of understanding how the microbiome interacts with the immune system. Gene-environment interaction is another important element that sets the stage for initiation of autoimmune disease, which calls for further investigation. Probiotics could be an appealing therapeutic strategy, but further interventional studies exploring the dynamic interaction of microbiome and probiotics are still needed.
The Impact of Intermittent Fasting (Ramadan Fasting) on Psoriatic Arthritis Disease Activity, Enthesitis, and Dactylitis: A Multicentre Study
Abstract
Intermittent circadian fasting, namely Ramadan, is a common worldwide practice. Such fasting has a positive impact on psoriasis, but no data exist on its role in psoriatic arthritis (PsA)-a disease that is clearly linked to body mass index. We enrolled 37 patients (23 females and 14 males) with a mean age 43.32 ± 7.81 and they fasted for 17 h for one month in 2016. The baseline PsA characteristics were collected and 12 (32.4%) patients had peripheral arthritis, 13 (35.1%) had axial involvement, 24 (64.9%) had enthesitis, and 13 (35.1%) had dactylitis. Three patients (8.1%) were treated with methotrexate, 28 (75.7%) with TNF-α blockers, and 6 (16.2%) with IL-17 blockers. After a month of intermittent fasting, C-reactive protein (CRP) levels decreased from 14.08 ± 4.65 to 12.16 ± 4.46 (p < 0.0001), Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) decreased from 2.83 ± 1.03 to 2.08 ± 0.67 (p = 0.0078), Psoriasis Area Severity Index (PASI) decreased from 7.46 ± 2.43 to 5.86 ± 2.37 (p < 0.0001), and Disease Activity index for PSoriatic Arthritis (DAPSA) decreased from 28.11 ± 4.51 to 25.76 ± 4.48 (p < 0.0001). Similarly, enthesitis improved after fasting, with Leeds Enthesitis Index (LEI) decreasing from 2.25 ± 1.11 to 1.71 ± 0.86 (p < 0.0001) and dactylitis severity score (DSS) decreasing from 9.92 ± 2.93 to 8.54 ± 2.79 (p = 0.0001). Fasting was found to be a predictor of a decrease in PsA disease activity scores (DAPSA, BASDAI, LEI, DSS) even after adjustment for weight loss. IL-17 therapy was found to be an independent predictor of decreases in LEI after fasting. These preliminary data may support the use of chronomedicine in the context of rheumatic diseases, namely PsA. Further studies are needed to support our findings.
Keywords: chronomedicine; circadian rhythm and biological clock; intermittent fasting; psoriatic arthritis.
Antioxidants and antiinflammatory dietary supplements for osteoarthritis and rheumatoid arthritis
Abstract
Objective: To review efficacy studies of antioxidant and antiinflammatory dietary supplements used to manage osteoarthritis (OA) and rheumatoid arthritis (RA) and make conclusions about their place in therapy. Glucosamine, chondroitin, and methyl sulfonyl methane were excluded.
Data sources: A literature search was conducted using MEDLINE (1996 through January 2009), EMBASE, Cochrane Library, Natural Medicines Comprehensive Database, and Natural Standard, with bibliographic review of relevant articles. Cited studies from before our search range were included if they represented the only published human data available. Search words included "antioxidant," "antiinflammatory," "cat's claw," "ginger," "fish oil," "omega-3," "turmeric," "vitamin E," "vitamin C," "Baikal skullcap," "barberry," "Chinese goldthread," "green tea," "Indian holy basil," "hu zhang,""oregano," and"rosemary."
Study selection and data extraction: Efficacy studies published in English were included provided they evaluated the dietary supplements in patients with OA or RA.
Data synthesis: Our search strategy yielded 16 clinical studies (11 randomized, placebo-controlled clinical trials, three crossover trials, one case-controlled study, and one open-label study) in addition to one meta-analysis and one review article.
Conclusions: Three studies support cat's claw alone or in combination for OA, and two studies support omega-3 fatty acids for the treatment of RA. We cannot recommend use of vitamin E alone; vitamins A, C, and E in combination; ginger; turmeric; or Zyflamend (New Chapter, Brattleboro, Vermont) for the treatment of OA or RA or omega-3 fatty acids for OA. Whether any of these supplements can be effectively and safely recommended to reduce nonsteroidal antiinflammatory drug or steroid usage is unclear and requires more high-quality research.
Vitamin D Deficiency and Rheumatoid Arthritis
Abstract
Vitamin D (VitD) is a hormone primarily synthesized in human skin under the stimulation of ultraviolet radiation. Beyond its endocrine role in bone metabolism, VitD is endowed with remarkable immunomodulatory properties. The effects of VitD on the immune system include the enhancement of microbicidal ability of monocytes/macrophages and the down-modulation of inflammatory cytokines produced by T lymphocytes. VitD deficiency is involved in many health problems, including immune-mediated diseases such as autoimmune disorders. Rheumatoid arthritis (RA) is a chronic inflammatory systemic autoimmune disease that compromises the joints, causing cartilage destruction and bone erosion. RA treatment usually consists of combined therapies that generally suppress the entire immune response leading to increased susceptibility to infections. This review describes the main effects of VitD on innate and adaptive immune system and also VitD status in inflammatory rheumatic diseases such as RA. Despite some controversies, the majority of reports reinforce the idea that lower VitD levels correlate with more severe clinical manifestations in RA and other rheumatic diseases. Therefore, supplementation with VitD to achieve normal serum levels is worthwhile as an aforethought. Original data concerning the potential applicability of 1,25-dihydroxyvitamin D3 (VitD3), the active form of vitamin D, as a tolerogenic adjuvant are also included. In this sense, the effect of VitD3 associated with proteoglycan (PG), which is a specific cartilage antigen, was tested in the course of experimental arthritis. This association significantly lowered clinical scores and local histopathological alterations. Even though local analysis of T cell subsets and cytokine production did not reveal any difference between the experimental groups, VitD3+PG association significantly reduced cytokine production by spleen cells. These results suggest that VitD3 played a role as a tolerogenic adjuvant by down-modulating the course of experimental RA. Considering this tolerogenic effect of VitD3+PG association, further investigations will reveal its plausible use in human RA.
Keywords: Experimental arthritis; Immunomodulation; Proteoglycan; Rheumatoid arthritis; Tolerance; Vitamin D.
A randomized, pilot study to assess the efficacy and safety of curcumin in patients with active rheumatoid arthritis
Abstract
Curcumin is known to possess potent antiinflammatory and antiarthritic properties. This pilot clinical study evaluated the safety and effectiveness of curcumin alone, and in combination with diclofenac sodium in patients with active rheumatoid arthritis (RA). Forty-five patients diagnosed with RA were randomized into three groups with patients receiving curcumin (500 mg) and diclofenac sodium (50 mg) alone or their combination. The primary endpoints were reduction in Disease Activity Score (DAS) 28. The secondary endpoints included American College of Rheumatology (ACR) criteria for reduction in tenderness and swelling of joint scores. Patients in all three treatment groups showed statistically significant changes in their DAS scores. Interestingly, the curcumin group showed the highest percentage of improvement in overall DAS and ACR scores (ACR 20, 50 and 70) and these scores were significantly better than the patients in the diclofenac sodium group. More importantly, curcumin treatment was found to be safe and did not relate with any adverse events. Our study provides the first evidence for the safety and superiority of curcumin treatment in patients with active RA, and highlights the need for future large-scale trials to validate these findings in patients with RA and other arthritic conditions.
Abstract
Although turmeric and its curcumin-enriched extracts have been used for treating arthritis, no systematic review and meta-analysis of randomized clinical trials (RCTs) have been conducted to evaluate the strength of the research. We systemically evaluated all RCTs of turmeric extracts and curcumin for treating arthritis symptoms to elucidate the efficacy of curcuma for alleviating the symptoms of arthritis. Literature searches were conducted using 12 electronic databases, including PubMed, Embase, Cochrane Library, Korean databases, Chinese medical databases, and Indian scientific database. Search terms used were "turmeric," "curcuma," "curcumin," "arthritis," and "osteoarthritis." A pain visual analogue score (PVAS) and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) were used for the major outcomes of arthritis. Initial searches yielded 29 articles, of which 8 met specific selection criteria. Three among the included RCTs reported reduction of PVAS (mean difference: -2.04 [-2.85, -1.24]) with turmeric/curcumin in comparison with placebo (P < .00001), whereas meta-analysis of four studies showed a decrease of WOMAC with turmeric/curcumin treatment (mean difference: -15.36 [-26.9, -3.77]; P = .009). Furthermore, there was no significant mean difference in PVAS between turmeric/curcumin and pain medicine in meta-analysis of five studies. Eight RCTs included in the review exhibited low to moderate risk of bias. There was no publication bias in the meta-analysis. In conclusion, these RCTs provide scientific evidence that supports the efficacy of turmeric extract (about 1000 mg/day of curcumin) in the treatment of arthritis. However, the total number of RCTs included in the analysis, the total sample size, and the methodological quality of the primary studies were not sufficient to draw definitive conclusions. Thus, more rigorous and larger studies are needed to confirm the therapeutic efficacy of turmeric for arthritis.
Keywords: arthritis; curcuma; osteoarthritis; pain visual analogue score; systematic review; turmeric.
Anti-Inflammatory Effects of the Essential Oils of Ginger ( Zingiber officinale Roscoe ) in Experimental Rheumatoid Arthritis
Abstract
Ginger and its extracts have been used traditionally as anti-inflammatory remedies, with a particular focus on the medicinal properties of its phenolic secondary metabolites, the gingerols. Consistent with these uses, potent anti-arthritic effects of gingerol-containing extracts were previously demonstrated by our laboratory using an experimental model of rheumatoid arthritis, streptococcal cell wall (SCW)-induced arthritis. In this study, anti-inflammatory effects of ginger's other secondary metabolites, the essential oils (GEO), which contain terpenes with reported phytoestrogenic activity, were assessed in female Lewis rats with SCW-induced arthritis. GEO (28 mg/kg/d ip) prevented chronic joint inflammation, but altered neither the initial acute phase of joint swelling nor granuloma formation at sites of SCW deposition in liver. Pharmacologic doses of 17-β estradiol (200 or 600 μg/kg/d sc) elicited the same pattern of anti-inflammatory activity, suggesting that GEO could be acting as a phytoestrogen. However, contrary to this hypothesis, GEO had no in vivo effect on classic estrogen target organs, such as uterus or bone. En toto, these results suggest that ginger's anti-inflammatory properties are not limited to the frequently studied phenolics, but may be attributable to the combined effects of both secondary metabolites, the pungent-tasting gingerols and as well as its aromatic essential oils.
Keywords: arthritis; essential oil; estradiol; estrogen; ginger; gingerol; inflammation; mice; phytoestrogen; rats.
The effect of ginger supplementation on some immunity and inflammation intermediate genes expression in patients with active Rheumatoid Arthritis
Abstract
Objective: Rheumatoid Arthritis (RA) is an autoimmune disease. The aim of this study was to investigate the effect of ginger supplementation on the expression of some immunity and inflammation intermediate genes in patients who suffer from RA.
Methods: In this randomized double-blind placebo-controlled clinical trial, seventy active RA patients were allocated randomly into two groups who either received 1500 mg ginger powder or placebo daily for 12 weeks. Disease activity score and gene expression of NF-κB, PPAR-γ, FoxP3, T-bet, GATA-3, and RORγt as immunity and inflammation intermediate factors were measured using quantitative real-time PCR before and after the intervention.
Results: After the intervention, FoxP3 genes expression increased significantly within ginger group and between the two groups (P-value = 0.02). Besides, T-bet and RORγt genes expression decreased significantly between the two groups (P-value < 0.05). In ginger group, PPAR-γ genes expression increased significantly (P-value = 0.047) but the difference between the two groups wasn't statistically significant (P-value = 0.12). The reduction in disease activity score was statistically significant within ginger group and between the two groups after the intervention.
Conclusion: It seems that ginger can improve RA by decreasing disease manifestations via increasing FoxP3 genes expression and by decreasing RORγt and T-bet genes expression.
Keywords: Ginger; Immunity; Inflammation; Rheumatoid Arthritis; Zingiber officinale Roscoe.
The Mediterranean diet, fish oil supplements and Rheumatoid arthritis outcomes: evidence from clinical trials
Abstract
Objectives: Rheumatoid arthritis (RA) is a chronic, autoimmune inflammatory disease of multiple joints that puts the patient at high risk for developing cardiovascular diseases (CVDs). The aim of the present study was to conduct an up-to-date systematic review and meta-analysis of published randomized controlled trials (RCTs) to assess potential changes in RA disease activity, inflammation, and CVD risk after oral intake of ω-3 polyunsaturated fatty acids.
Methods: Publications up to July 31, 2016 were examined using the PubMed, SCOPUS, and EMBASE databases.
Inclusion criteria: English language; human subjects; both sexes; RCTs; oral intake of ω-3 fatty acids; minimum duration of 3 mo; and no medication change throughout intervention. The Cochrane Risk of Bias tool was used to assess quality of trials. We included 20 RCTs, involving 717 patients with RA in the intervention group and 535 RA patients in the control group.
Results: Despite the evidence of overall low quality of trials, consumption of ω-3 fatty acids was found to significantly improve eight disease-activity-related markers. Regarding inflammation, only leukotriene B4 was reduced (five trials, standardized mean difference [SMD], -0.440; 95% confidence interval [CI], -0.676 to -0.205; I2 = 46.5%; P < 0.001). A significant amelioration was found for blood triacylglycerol levels (three trials, SMD, -0.316; 95% CI, -0.561 to -0.070; I2 = 0.0%; P = 0.012).
Conclusion: The beneficial properties of ω-3 polyunsaturated fatty acids on RA disease activity confirm the results of previous meta-analyses. Among five proinflammatory markers evaluated, only leukotriene B4 was found to be reduced. However, a positive effect on blood lipid profile of patients with RA was evident, perhaps for the first time.
The antioxidant vitamins A, C, E and selenium in the treatment of arthritis: a systematic review of randomized clinical trials
Abstract
Objective. To systematically review the evidence from randomized clinical trials (RCTs) for the effectiveness of the antioxidant vitamins A, C, E or selenium or their combination in the treatment of arthritis.
Methods. A systematic search of computerized databases from inception to September 2006 for relevant RCTs, application of pre-defined inclusion/exclusion criteria and independent data extraction by two authors. Methodological quality was assessed using the Jadad scale.
Results. The searches identified 20 unique RCTs meeting the inclusion criteria: 11 in inflammatory arthritis and 9 in osteoarthritis (OA). The studies included are generally of poor quality. They fall into three main clusters: selenium for rheumatoid arthritis (n = 5); vitamin E for inflammatory arthritis (n = 5) and vitamin E for OA (n = 7). One RCT suggests superiority of vitamin E over placebo and three RCTs suggest equivalence between vitamin E and diclofenac in the treatment of inflammatory arthritis. In OA, four RCTs compared vitamin E with placebo. Two shorter-term studies were positive and two longer-term studies were negative. Two further RCTs suggest equivalence between vitamin E and diclofenac in the treatment of OA. Findings for selenium, vitamin A and a combination product in inflammatory arthritis and for vitamin A, and a combination product in OA were negative. An isolated positive result for vitamin C in OA is of doubtful clinical significance.
Conclusions. Clinical trials testing the efficacy of vitamin E in the treatment of OA and inflammatory arthritis have been methodologically weak and have produced contradictory findings. There is presently no convincing evidence that selenium, vitamin A, vitamin C or the combination product selenium ACE is effective in the treatment of any type of arthritis.
Systematic review of a marine nutriceutical supplement in clinical trials for arthritis: the effectiveness of the New Zealand green-lipped mussel Perna canaliculus
Abstract
Background
Nutritional supplements, such as Seatone, which contain freeze-dried tissue from the New Zealand green-lipped mussel Perna canaliculus, are sold in many countries to relieve arthritic symptoms and to aid in the regeneration of arthritic and injured joints.
Methods
Searches for all published controlled trials on the clinical effectiveness of green-lipped mussel, as a nutritional supplement with potential health benefits for arthritis, were carried out from four independent databases. No language restrictions were imposed, and the review was undertaken from extracted data and was assessed critically according to predefined criteria by the authors.
Results
Reports of clinical studies, using freeze-dried mussel powder, show mixed outcome measures and are not conclusive, with only two of five randomized controlled trials attesting benefits for rheumatoid and osteoarthritis patients. Similarly, animal studies have likewise yielded mixed findings. In both these cases possibly due to the lack of stabilization of the omega-3 polyunsaturated fatty acids, now known to be the basis of anti-inflammatory activity.
Conclusion
There is little consistent and compelling evidence, to date, in the therapeutic use of freeze-dried green-lipped mussel powder products for rheumatoid or osteoarthritis treatment, particularly in comparison to other cheaper alternative nutriceutical supplements of proven efficacy. However, further investigations are necessary to determine whether green-lipped mussel supplements, such as Seatone, are therapeutic options in the management of arthritis.
Improved arthritic knee health in a pilot RCT of phytotherapy
Abstract
Although practitioner-prescribed `western' herbal medicine (phytotherapy) is a popular complementary therapy in the UK, no clinical studies have been reported on patient-orientated outcomes. The objective of this pilot study was to investigate the effects of phytotherapy on symptoms of osteoarthritis of the knee. A previous study of Chinese herbal medicine for the treatment of irritable bowel syndrome, published in the Journal of the American Medical Association,1 acted as a model in the development of the protocol of this investigation.
Twenty adults, previously diagnosed with osteoarthritis of the knee, were recruited from two Inner London GP practices into this randomized, double-blind, placebo-controlled, pilot study carried out in a primary-care setting. All subjects were seen in consultation three times by a herbal practitioner who was blinded to the randomization coding. Each subject was prescribed treatment and given lifestyle advice according to usual practice: continuation of conventional medication where applicable, healthy-eating advice and nutrient supplementation. Individualized herbal medicine was prescribed for each patient, but only dispensed for those randomized to active treatment — the remainder were supplied with a placebo. At baseline and outcome (after ten weeks of treatment), subjects completed a food frequency questionnaire and the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) knee health and Measure Yourself Outcome Profile (MYMOP) wellbeing questionnaires. Subjects completing the study per protocol (n = 14) reported an increased intake of wholegrain foods (p = 0.045) and oily fish (p = 0.039) compared to baseline, but no increase in fruit and vegetables and dairy products intakes.
There was no difference in the primary outcome measure of knee health assessed as the difference in the mean response (baseline-week 10) in WOMAC score between the two treatment groups. However, there was, compared with baseline, improvement in the active group (n = 9) for the mean WOMAC stiffness sub-score at week 5 ( p = 0.035) and week 10 ( p = 0.060) but not in the placebo group (n = 5). Furthermore, for the active, but not the placebo group, the mean WOMAC total and sub-scores all showed clinically significant improvement (≥ 20%) in knee symptoms at weeks 5 and 10 compared with baseline. Moreover, the mean MYMOP symptom 2 sub-score, mostly relating to osteoarthritis (OA), showed significant improvement at week 5 ( p = 0.02) and week 10 ( p = 0.008) compared with baseline for the active, but not for the placebo group.
This pilot study showed that herbal medicine prescribed for the individual by a herbal practitioner resulted in improvement of symptoms of OA of the knee.
Fish oil and rheumatoid arthritis: past, present and future
Abstract
Meta- and mega-analysis of randomised controlled trials indicate reduction in tender joint counts and decreased use of non-steroidal anti-inflammatory drugs with fish-oil supplementation in long-standing rheumatoid arthritis (RA). Since non-steroidal anti-inflammatory drugs confer cardiovascular risk and there is increased cardiovascular mortality in RA, an additional benefit of fish oil in RA may be reduced cardiovascular risk via direct mechanisms and decreased non-steroidal anti-inflammatory drug use. Potential mechanisms for anti-inflammatory effects of fish oil include inhibition of inflammatory mediators (eicosanoids and cytokines), and provision of substrates for synthesis of lipid suppressors of inflammation (resolvins). Future studies need progress in clinical trial design and need to shift from long-standing disease to examination of recent-onset RA. We are addressing these issues in a current randomised controlled trial of fish oil in recent-onset RA, where the aim is to intervene before joint damage has occurred. Unlike previous studies, the trial occurs on a background of drug regimens determined by an algorithm that is responsive to disease activity and drug intolerance. This allows drug use to be an outcome measure whereas in previous trial designs, clinical need to alter drug use was a ‘problem’. Despite evidence for efficacy and plausible biological mechanisms, the limited clinical use of fish oil indicates there are barriers to its use. These probably include the pharmaceutical dominance of RA therapies and the perception that fish oil has relatively modest effects. However, when collateral benefits of fish oil are included within efficacy, the argument for its adjunctive use in RA is strong.
Osteoarthritis and nutrition. From nutraceuticals to functional foods: a systematic review of the scientific evidence
Abstract
The scientific and medical community remains skeptical regarding the efficacy of nutrition for osteoarthritis despite their broad acceptation by patients. In this context, this paper systematically reviews human clinical trials evaluating the effects of nutritional compounds on osteoarthritis. We searched the Medline, Embase, and Biosis databases from their inception to September 2005 using the terms random, double-blind method, trial, study, placebo, and osteoarthritis. We selected all peer-reviewed articles reporting the results of randomised human clinical trials (RCTs) in osteoarthritis that investigated the effects of oral interventions based on natural molecules. Studies on glucosamine and chondroitin sulfate were excluded. The quality of the RCTs was assessed with an osteoarthritic-specific standardised set of 12 criteria and a validated instrument. A best-evidence synthesis was used to categorise the scientific evidence behind each nutritional compound as good, moderate, or limited. A summary of the most relevant in vitro and animal studies is used to shed light on the potential mechanisms of action. Inclusion criteria were met by 53 RCTs out of the 2,026 identified studies. Good evidence was found for avocado soybean unsaponifiables. Moderate evidence was found for methylsulfonylmethane and SKI306X, a cocktail of plant extracts. Limited evidence was found for the Chinese plant extract Duhuo Jisheng Wan, cetyl myristoleate, lipids from green-lipped mussels, and plant extracts from Harpagophytum procumbens. Overall, scientific evidence exists for some specific nutritional interventions to provide symptom relief to osteoarthritic patients. It remains to be investigated whether nutritional compounds can have structure-modifying effects.
Efficacy of Turmeric Extracts and Curcumin for Alleviating the Symptoms of Joint Arthritis: A Systematic Review and Meta-Analysis of Randomized Clinical Trials
Abstract
Although turmeric and its curcumin-enriched extracts have been used for treating arthritis, no systematic review and meta-analysis of randomized clinical trials (RCTs) have been conducted to evaluate the strength of the research. We systemically evaluated all RCTs of turmeric extracts and curcumin for treating arthritis symptoms to elucidate the efficacy of curcuma for alleviating the symptoms of arthritis. Literature searches were conducted using 12 electronic databases, including PubMed, Embase, Cochrane Library, Korean databases, Chinese medical databases, and Indian scientific database. Search terms used were “turmeric,” “curcuma,” “curcumin,” “arthritis,” and “osteoarthritis.” A pain visual analogue score (PVAS) and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) were used for the major outcomes of arthritis. Initial searches yielded 29 articles, of which 8 met specific selection criteria. Three among the included RCTs reported reduction of PVAS (mean difference: −2.04 [−2.85, −1.24]) with turmeric/curcumin in comparison with placebo (P < .00001), whereas meta-analysis of four studies showed a decrease of WOMAC with turmeric/curcumin treatment (mean difference: −15.36 [−26.9, −3.77]; P = .009). Furthermore, there was no significant mean difference in PVAS between turmeric/curcumin and pain medicine in meta-analysis of five studies. Eight RCTs included in the review exhibited low to moderate risk of bias. There was no publication bias in the meta-analysis. In conclusion, these RCTs provide scientific evidence that supports the efficacy of turmeric extract (about 1000 mg/day of curcumin) in the treatment of arthritis. However, the total number of RCTs included in the analysis, the total sample size, and the methodological quality of the primary studies were not sufficient to draw definitive conclusions. Thus, more rigorous and larger studies are needed to confirm the therapeutic efficacy of turmeric for arthritis.
Intake of ω-3 polyunsaturated fatty acids in patients with rheumatoid arthritis: A systematic review and meta-analysis
Abstract
Objectives
Rheumatoid arthritis
(RA) is a chronic, autoimmune
inflammatory disease
of multiple joints that puts the patient at high risk for developing cardiovascular diseases (CVDs). The aim of the present study was to conduct an up-to-date systematic review and
meta-analysis
of published randomized controlled trials (RCTs) to assess potential changes in RA disease activity, inflammation, and CVD risk after oral intake of ω-3 polyunsaturated fatty acids.
Methods
Publications up to July 31, 2016 were examined using the PubMed, SCOPUS, and EMBASE databases. Inclusion criteria: English language; human subjects; both sexes; RCTs; oral intake of ω-3 fatty acids; minimum duration of 3 mo; and no medication change throughout intervention. The Cochrane Risk of Bias tool was used to assess quality of trials. We included 20 RCTs, involving 717 patients with RA in the intervention group and 535 RA patients in the control group.
Results
Despite the evidence of overall low quality of trials, consumption of ω-3 fatty acids was found to significantly improve eight disease-activity–related markers. Regarding inflammation, only
leukotriene B4
was reduced (five trials, standardized mean difference [SMD], –0.440; 95% confidence interval [CI], −0.676 to −0.205; I2 = 46.5%; P < 0.001). A significant amelioration was found for blood
triacylglycerol
levels (three trials, SMD, −0.316; 95% CI, −0.561 to −0.070; I2 = 0.0%; P = 0.012).
Conclusion
The beneficial properties of ω-3 polyunsaturated fatty acids on RA disease activity confirm the results of previous meta-analyses. Among five proinflammatory markers evaluated, only leukotriene B4 was found to be reduced. However, a positive effect on blood lipid profile of patients with RA was evident, perhaps for the first time.
The Dietary Approaches to Stop Hypertension (DASH) diet, Western diet, and risk of gout in men: prospective cohort study
Abstract
Objective To prospectively examine the relation between the Dietary Approaches to Stop Hypertension (DASH) and Western diets and risk of gout (ie, the clinical endpoint of hyperuricemia) in men.
Design Prospective cohort study.
Setting The Health Professionals Follow-up Study.
Participants 44 444 men with no history of gout at baseline. Using validated food frequency questionnaires, each participant was assigned a DASH dietary pattern score (based on high intake of fruits, vegetables, nuts and legumes, low fat dairy products, and whole grains, and low intake of sodium, sweetened beverages, and red and processed meats) and a Western dietary pattern score (based on high intake of red and processed meats, French fries, refined grains, sweets, and desserts).
Main outcome measure Risk of incident gout meeting the preliminary American College of Rheumatology survey criteria for gout, adjusting for potential confounders, including age, body mass index, hypertension, diuretic use, and alcohol intake.
Results During 26 years of follow-up, 1731 confirmed cases of incident gout were documented. A higher DASH dietary pattern score was associated with a lower risk for gout (adjusted relative risk for extreme fifths 0.68, 95% confidence interval 0.57 to 0.80, P value for trend <0.001). In contrast, a higher Western dietary pattern score was associated with an increased risk for gout (1.42, 1.16 to 1.74, P=0.005).
Conclusion The DASH diet is associated with a lower risk of gout, suggesting that its effect of lowering uric acid levels in individuals with hyperuricemia translates to a lower risk of gout. Conversely, the Western diet is associated with a higher risk of gout. The DASH diet may provide an attractive preventive dietary approach for men at risk of gout.
Dietary intake of fibre and risk of knee osteoarthritis in two US prospective cohorts
Abstract
Objectives Dietary fibre reduces body weight and inflammation both of which are linked with knee osteoarthritis (OA). We examined the association between fibre intake and risk of knee OA.
Methods We used data from the Osteoarthritis Initiative (OAI) of 4796 participants and Framingham Offspring Osteoarthritis Study (Framingham) of 1268 persons. Dietary intake of fibre was estimated at baseline, and incident radiographic OA (ROA) and symptomatic OA (SxOA) were followed annually until 48 months in OAI and assessed 9 years later in Framingham. Knee pain worsening was also examined in OAI. Generalised estimating equations were applied in multivariable regression models.
Results In OAI, we identified 869 knees with SxOA, 152 knees with ROA and 1964 knees with pain worsening among 4051 subjects with valid dietary intake (baseline mean age: 61.2 years; mean body mass index (BMI): 28.6). In Framingham, 143 knees with SxOA and 176 knees with ROA among 971 such subjects (baseline mean age: 53.9 years; mean BMI: 27.0) were identified. In both cohorts, dietary total fibre was inversely associated with risk of SxOA (p trend <0.03) with significantly lower risk at the highest versus lowest quartile (OR (95% CI): 0.70 (0.52, 0.94) for OAI and 0.39 (0.17, 0.88) for Framingham). Furthermore, dietary total and cereal fibre were significantly inversely associated with knee pain worsening in OAI (p trend <0.02). No apparent association was found with ROA.
Conclusions Findings from two longitudinal studies consistently showed that higher total fibre intake was related to a lower risk of SxOA, while the relation to ROA was unclear.
Obesity
Nutrition knowledge, attitudes, and self-regulation as predictors of overweight and obesity
Abstract
Background and purpose: Nutrition knowledge, attitudes, and eating self-regulation are important determinants of overweight and obesity. Eating self-regulation is the link between eating intention and behavior. However, the extent to which these factors influence overweight and obesity has not been thoroughly studied. The study examined nutrition knowledge, attitudes, and eating self-regulation as predictors of overweight and obesity among adults in a community setting.
Methods: A total of 313 adults participated in an online survey, which included the General Nutrition Knowledge Questionnaire-Revised, the Nutrition Attitudes Questionnaire, and the Self-Regulation of Eating Behavior Questionnaire. Descriptive statistics, Kendall's tau tests, and multivariate logistic regression procedures were performed.
Conclusions: More than half of the participants were either overweight or obese (56.5%). The mean nutrition knowledge score was 74.1%, and only 28.1% correctly identified the body mass index for obesity. Positive predictors of overweight and obesity included poor eating self-regulation of giving up too easily on eating intentions (odds ratio [OR] = 3.81), male gender (OR = 2.0), and age (OR = 1.03), whereas nutrition attitudes were a negative predictor (OR = 0.74).
Implications for practice: The odds of overweight or obesity were nearly four times greater for those who gave up too easily on their eating intentions. Nurse practitioners can play a critical role in establishing healthy dietary habits to maintain weight control by promoting good eating self-regulation, despite the current obesogenic environment. After assessing patient readiness and motivation, it is important to help patients make eating self-regulation as manageable as possible to promote long-term weight management.
Position of the Academy of Nutrition and Dietetics: Interventions for the Treatment of Overweight and Obesity in Adults
Abstract
It is the position of the Academy of Nutrition and Dietetics that successful treatment of overweight and obesity in adults requires adoption and maintenance of lifestyle behaviors contributing to both dietary intake and physical activity. These behaviors are influenced by many factors; therefore, interventions incorporating more than one level of the socioecological model and addressing several key factors in each level may be more successful than interventions targeting any one level and factor alone. Registered dietitian nutritionists, as part of a multidisciplinary team, need to be current and skilled in weight management to effectively assist and lead efforts that can reduce the obesity epidemic. Using the Academy of Nutrition and Dietetics' Evidence Analysis Process and Evidence Analysis Library, this position paper presents the current data and recommendations for the treatment of overweight and obesity in adults. Evidence on intrapersonal influences, such as dietary approaches, lifestyle intervention, pharmacotherapy, and surgery, is provided. Factors related to treatment, such as intensity of treatment and technology, are reviewed. Community-level interventions that strengthen existing community assets and capacity and public policy to create environments that support healthy energy balance behaviors are also discussed.
Genetic background, nutrition and obesity: a review
Abstract
Objective: To summarize the latest information on the relationship between genes and common forms of obesity, and to review genetic markers (SNPs and miRNA) that play a role in predisposing to common forms of obesity and related disorders.
Materials and methods: We searched PubMed with the following keywords: (obesity[Title/Abstract]) AND predisposition[Title/Abstract]) AND miRNA[Title/Abstract]) OR polymorphism[Title/Abstract].
Results: From the search we obtained a total of 44 gene loci and 48 miRNAs associated with common obesity.
Conclusions: It is now widely accepted that obesity involves interactions between environmental risk factors (physical inactivity, excessive calorie intake, chronic stress, taste perception) and a genetic background of risk. Analysis of the genetic background of obese subjects is therefore an important way to determine the molecular mechanisms controlling the link between food intake and obesity, enabling a better understanding of how these interactions may differ from person to person.
The future of nutrition: Nutrigenomics and nutrigenetics in obesity and cardiovascular diseases
Abstract
Over time, the relationship between diet and health has aroused great interest, since nutrition can prevent and treat several diseases. It has been demonstrated that general recommendations on macronutrients and micronutrients do not affect to every individual in the same way because diet is an important environmental factor that interacts with genes. Thus, there is a growing necessity of improving a personalized nutrition to treat obesity and associated medical conditions, taking into account the interactions between diet, genes and health. Therefore, the knowledge of the interactions between the genome and nutrients at the molecular level, has led to the advent of nutritional genomics, which involves the sciences of nutrigenomics and nutrigenetics. In this review, we will comprehensively analyze the role of the most important genes associated with two interrelated chronic medical conditions, such as obesity and cardiovascular diseases.
Nutrition and its role in epigenetic inheritance of obesity and diabetes across generations
Abstract
Nutritional constraints including not only caloric restriction or protein deficiency, but also energy-dense diets affect metabolic health and frequently lead to obesity and insulin resistance, as well as glucose intolerance and type 2 diabetes. The effects of these environmental factors are often mediated via epigenetic modifiers that target the expression of metabolic genes. More recently, it was discovered that such parentally acquired metabolic changes can alter the metabolic health of the filial and grand-filial generations. In mammals, this epigenetic inheritance can either follow an intergenerational or transgenerational mode of inheritance. In the case of intergenerational inheritance, epimutations established in gametes persist through the first round of epigenetic reprogramming occurring during preimplantation development. For transgenerational inheritance, epimutations persist additionally throughout the reprogramming that occurs during germ cell development later in embryogenesis. Differentially expressed transcripts, genomic cytosine methylations, and several chemical modifications of histones are prime candidates for tangible marks which may serve as epimutations in inter- and transgenerational inheritance and which are currently being investigated experimentally. We review, here, the current literature in support of epigenetic inheritance of metabolic traits caused by nutritional constraints and potential mechanisms in man and in rodent model systems.
Vitamin E Metabolic Effects and Genetic Variants: A Challenge for Precision Nutrition in Obesity and Associated Disturbances
Abstract
Vitamin E (VE) has a recognized leading role as a contributor to the protection of cell constituents from oxidative damage. However, evidence suggests that the health benefits of VE go far beyond that of an antioxidant acting in lipophilic environments. In humans, VE is channeled toward pathways dealing with lipoproteins and cholesterol, underlining its relevance in lipid handling and metabolism. In this context, both VE intake and status may be relevant in physiopathological conditions associated with disturbances in lipid metabolism or concomitant with oxidative stress, such as obesity. However, dietary reference values for VE in obese populations have not yet been defined, and VE supplementation trials show contradictory results. Therefore, a better understanding of the role of genetic variants in genes involved in VE metabolism may be crucial to exert dietary recommendations with a higher degree of precision. In particular, genetic variability should be taken into account in targets concerning VE bioavailability per se or concomitant with impaired lipoprotein transport. Genetic variants associated with impaired VE liver balance, and the handling/resolution of oxidative stress might also be relevant, but the core information that exists at present is insufficient to deliver precise recommendations.
Nutrition in the First 1000 Days: Ten Practices to Minimize Obesity Emerging from Published Science
Abstract
The prevalence of childhood overweight and obesity has increased in most countries the last decades. Considering this in a simplistic way, we can say that obesity is the result of an imbalance between energy intake and energy expenditure. Moreover, the environment from conception to childhood could influence the child’s future health. The first 1000 days of life start with woman’s pregnancy, and offer a unique window of opportunity to contribute to obesity prevention. In light of the actual literature, the aim of our article is to discuss a proposal of 10 good practices to minimize obesity in the first 1000 days emerging from published science. (1) Both the mother’s and the father’s behaviors are important. A balanced diet with appropriate fat and protein intake, and favoring fruits and vegetables, is recommended for both parents during the conception period and pregnancy. Furthermore, overweight/obese women who are planning to become pregnant should reduce their weight before conception. (2) During pregnancy, at birth, and during early life, body composition measurements are crucial to monitor the baby’s growth. (3) Exclusive breastfeeding is recommended at the beginning of life until six months of age. (4) Four to six months of age is the optimal window to introduce complementary feeding. Until one year of age, breast milk or follow-on/commercial formula is the main recommended feeding source, and cow’s milk should be avoided until one year of age. (5) Fruit and vegetable introduction should begin early. Daily variety, diversity in a meal, and repeated exposure to the food, up to eight times, are efficient strategies to increase acceptance of food not well accepted at first. There is no need to add sugar, salt, or sugary fluids to the diet. (6) Respect the child’s appetite and avoid coercive “clean your plate” feeding practices. Adapt the portion of food and don’t use food as reward for good behavior. (7) Limit animal protein intake in early life to reduce the risk of an early adiposity rebound. Growing-up milk for children between one and three years of age should be preferred to cow’s milk, in order to limit intake and meet essential fatty acid and iron needs. (8) The intake of adequate fat containing essential fatty acids should be promoted. (9) Parents should be role models when feeding, with TV and other screens turned-off during meals. (10) Preventive interventions consisting of promoting physical activity and sufficient time dedicated to sleep should be employed. In fact, short sleep duration may be associated with increased risk of developing obesity. Based on literature reviews, and given the suggestions described in this manuscript, concerted public health efforts are needed to achieve the healthy objectives for obesity and nutrition, and to fight the childhood obesity epidemic.
Chrono-nutrition for the prevention and treatment of obesity and type 2 diabetes: from mice to men
Abstract
The proliferation in the rate of diagnosis of obesity and type 2 diabetes mellitus continues unabated, with current recommendations for primary lifestyle changes (i.e. modification to dietary patterns) having a limited impact in reducing the incidence of these metabolic diseases. Part of the reason for the failure to alter nutritional practices is that current dietary recommendations may be unrealistic for the majority of adults. Indeed, round-the-clock access to energy-dense, nutrient-poor food makes long-term changes to dietary habits challenging. Hence, there is urgent need for innovations in the delivery of evidence-based diet interventions to rescue some of the deleterious effects on circadian biology induced by our modern-day lifestyle. With the growing appreciation that the duration over which food is consumed during a day has profound effects on numerous physiological and metabolic processes, we discuss dietary protocols that modify the timing of food intake to deliberately alter the feeding–fasting cycle. Such chrono-nutrition functions to optimise metabolism by timing nutrient intake to the acrophases of metabolic rhythms to improve whole-body insulin sensitivity and glycaemic control, and thereby positively impact metabolic health.
Gene-Diet Interaction and Precision Nutrition in Obesity
Abstract
The rapid rise of obesity during the past decades has coincided with a profound shift of our living environment, including unhealthy dietary patterns, a sedentary lifestyle, and physical inactivity. Genetic predisposition to obesity may have interacted with such an obesogenic environment in determining the obesity epidemic. Growing studies have found that changes in adiposity and metabolic response to low-calorie weight loss diets might be modified by genetic variants related to obesity, metabolic status and preference to nutrients. This review summarized data from recent studies of gene-diet interactions, and discussed integration of research of metabolomics and gut microbiome, as well as potential application of the findings in precision nutrition.
Nutrition, the visceral immune system, and the evolutionary origins of pathogenic obesity
Abstract
The global obesity epidemic is the subject of an immense, diversely specialized research effort. An evolutionary analysis reveals connections among disparate findings, starting with two well-documented facts: Obesity-associated illnesses (e.g., type-2 diabetes and cardiovascular disease), are especially common in: (i) adults with abdominal obesity, especially enlargement of visceral adipose tissue (VAT), a tissue with important immune functions; and (ii) individuals with poor fetal nutrition whose nutritional input increases later in life. I hypothesize that selection favored the evolution of increased lifelong investment in VAT in individuals likely to suffer lifelong malnutrition because of its importance in fighting intraabdominal infections. Then, when increased nutrition violates the adaptive fetal prediction of lifelong nutritional deficit, preferential VAT investment could contribute to abdominal obesity and chronic inflammatory disease. VAT prioritization may help explain several patterns of nutrition-related disease: the paradoxical increase of chronic disease with increased food availability in recently urbanized and migrant populations; correlations between poor fetal nutrition, improved childhood (catch-up) growth, and adult metabolic syndrome; and survival differences between children with marasmus and kwashiorkor malnutrition. Fats and sugars can aggravate chronic inflammation via effects on intestinal bacteria regulating gut permeability to visceral pathogens. The extremes in a nutrition-sensitive trade-off between visceral (immune-function) vs. subcutaneous (body shape) adiposity may have been favored by selection in highly stratified premedicine societies. Altered adipose allocation in populations with long histories of social stratification and malnutrition may be the result of genetic accommodation of developmental responses to poor maternal/fetal conditions, increasing their vulnerability to inflammatory disease.
Microbial enterotypes in personalized nutrition and obesity management
Abstract
Human gut microbiota has been suggested to play an important role in nutrition and obesity. However, formulating meaningful and clinically relevant dietary advice based on knowledge about gut microbiota remains a key challenge. A number of recent studies have found evidence that stratification of individuals according to 2 microbial enterotypes (dominance of either Prevotella or Bacteroides) may be useful in predicting responses to diets and drugs. Here, we review enterotypes in a nutritional context and discuss how enterotype stratification may be used in personalized nutrition in obesity management. Enterotypes are characterized by distinct digestive functions with preference for specific dietary substrate, resulting in short-chain fatty acids that may influence energy balance in the host. Consequently, the enterotype potentially affects the individual's ability to lose weight when following a specific diet. In short, a high-fiber diet seems to optimize weight loss among Prevotella-enterotype subjects but not among Bacteroides-enterotype subjects. In contrast, increasing bifidobacteria in the gut among Bacteroides-enterotype subjects improves metabolic parameters, suggesting that this approach can be used as an alternative weight loss strategy. Thus, enterotypes, as a pretreatment gut microbiota biomarker, have the potential to become an important tool in personalized nutrition and obesity management, although further interventions assessing their applicability are warranted.
Contribution of macronutrients to obesity: implications for precision nutrition
Abstract
The specific metabolic contribution of consuming different energy-yielding macronutrients (namely, carbohydrates, protein and lipids) to obesity is a matter of active debate. In this Review, we summarize the current research concerning associations between the intake of different macronutrients and weight gain and adiposity. We discuss insights into possible differential mechanistic pathways where macronutrients might act on either appetite or adipogenesis to cause weight gain. We also explore the role of dietary macronutrient distribution on thermogenesis or energy expenditure for weight loss and maintenance. On the basis of the data discussed, we describe a novel way to manage excessive body weight; namely, prescribing personalized diets with different macronutrient compositions according to the individual’s genotype and/or enterotype. In this context, the interplay of macronutrient consumption with obesity incidence involves mechanisms that affect appetite, thermogenesis and metabolism, and the outcomes of these mechanisms are altered by an individual’s genotype and microbiota. Indeed, the interactions of the genetic make-up and/or microbiota features of a person with specific macronutrient intakes or dietary pattern consumption help to explain individualized responses to macronutrients and food patterns, which might represent key factors for comprehensive precision nutrition recommendations and personalized obesity management.
Paradoxical Effects of Fruit on Obesity
Abstract
Obesity is exponentially increasing regardless of its preventable characteristics. The current measures for preventing obesity have failed to address the severity and prevalence of obesity, so alternative approaches based on nutritional and diet changes are attracting attention for the treatment of obesity. Fruit contains large amounts of simple sugars (glucose, fructose, sucrose, etc.), which are well known to induce obesity. Thus, considering the amount of simple sugars found in fruit, it is reasonable to expect that their consumption should contribute to obesity rather than weight reduction. However, epidemiological research has consistently shown that most types of fruit have anti-obesity effects. Thus, due to their anti-obesity effects as well as their vitamin and mineral contents, health organizations are suggesting the consumption of fruit for weight reduction purposes. These contradictory characteristics of fruit with respect to human body weight management motivated us to study previous research to understand the contribution of different types of fruit to weight management. In this review article, we analyze and discuss the relationships between fruit and their anti-obesity effects based on numerous possible underlying mechanisms, and we conclude that each type of fruit has different effects on body weight.
Keywords: anti-obesity; fruit; obesity; pro-obesity.
Consumption of ultra-processed foods and body fat during childhood and adolescence: a systematic review
Abstract
Objective: To review the available literature on the association between consumption of ultra-processed foods and body fat during childhood and adolescence.
Design: A systematic review was conducted in the PubMed, Web of Science and LILACS databases. Studies that evaluated the association between consumption of ultra-processed food (exposure) and body fat (outcome) during childhood and adolescence were eligible.
Subjects: Healthy children and adolescents.
Results: Twenty-six studies that evaluated groups of ultra-processed foods (such as snacks, fast foods, junk foods and convenience foods) or specific ultra-processed foods (soft drinks/sweetened beverages, sweets, chocolate and ready-to-eat cereals) were selected. Most of the studies (n 15) had a cohort design. Consumption was generally evaluated by means of FFQ or food records; and body composition, by means of double indirect methods (bioelectrical impedance analysis and skinfolds). Most of the studies that evaluated consumption of groups of ultra-processed foods and soft drinks/sweetened beverages found positive associations with body fat.
Conclusions: Our review showed that most studies have found positive associations between consumption of ultra-processed food and body fat during childhood and adolescence. There is a need to use a standardized classification that considers the level of food processing to promote comparability between studies.
Household availability of ultra-processed foods and obesity in nineteen European countries
Abstract
Objective: To assess household availability of NOVA food groups in nineteen European countries and to analyse the association between availability of ultra-processed foods and prevalence of obesity.
Design: Ecological, cross-sectional study.
Setting: Europe.
Subjects: Estimates of ultra-processed foods calculated from national household budget surveys conducted between 1991 and 2008. Estimates of obesity prevalence obtained from national surveys undertaken near the budget survey time.
Results: Across the nineteen countries, median average household availability amounted to 33·9 % of total purchased dietary energy for unprocessed or minimally processed foods, 20·3 % for processed culinary ingredients, 19·6 % for processed foods and 26·4 % for ultra-processed foods. The average household availability of ultra-processed foods ranged from 10·2 % in Portugal and 13·4 % in Italy to 46·2 % in Germany and 50·4 % in the UK. A significant positive association was found between national household availability of ultra-processed foods and national prevalence of obesity among adults. After adjustment for national income, prevalence of physical inactivity, prevalence of smoking, measured or self-reported prevalence of obesity, and time lag between estimates on household food availability and obesity, each percentage point increase in the household availability of ultra-processed foods resulted in an increase of 0·25 percentage points in obesity prevalence.
Conclusions: The study contributes to a growing literature showing that the consumption of ultra-processed foods is associated with an increased risk of diet-related non-communicable diseases. Its findings reinforce the need for public policies and actions that promote consumption of unprocessed or minimally processed foods and make ultra-processed foods less available and affordable.
Consumption of ultra-processed foods and obesity in Brazilian adolescents and adults
Abstract
Objectives: The aim of this study was to evaluate the relationship between the consumption of ultra-processed foods and obesity indicators among Brazilian adults and adolescents.
Methods: We used cross-sectional data on 30,243 individuals aged ≥10 years from the 2008-2009 Brazilian Dietary Survey. Food consumption data were collected through 24-h food records. We classified food items according to characteristics of food processing. Ultra-processed foods were defined as formulations made by the food industry mostly from substances extracted from foods or obtained with the further processing of constituents of foods or through chemical synthesis, with little if any whole food. Examples included candies, cookies, sugar-sweetened beverages, and ready-to-eat dishes. Regression models were fitted to evaluate the association of the consumption of ultra-processed foods (% of energy intake) with body-mass-index, excess weight, and obesity status, controlling for socio-demographic characteristics, smoking, and physical activity.
Results: Ultra-processed foods represented 30% of the total energy intake. Those in the highest quintile of consumption of ultra-processed foods had significantly higher body-mass-index (0.94 kg/m(2); 95% CI: 0.42,1.47) and higher odds of being obese (OR=1.98; 95% CI: 1.26,3.12) and excess weight (OR=1.26; 95% CI: 0.95,1.69) compared with those in the lowest quintile of consumption.
Conclusion: Our findings support the role of ultra-processed foods in the obesity epidemic in Brazil.
The anti-obesity effect of starch in a whole grain-like structural form
Abstract
Obesity is a risk factor for many chronic diseases, and the anti-obesity effect of starch in a whole grain-like structural form (WGLSF) prepared through co-gelation with oat β-glucan and alginate was studied using high-fat (HF) induced obese male C57BL/6J mice. In vitro human fecal fermentation of WGLSF-starch showed a slower rate of fermentation and a higher production of butyric acid (132.0 μmol per 50 mg sample) when compared to the physical mixture counterpart of starch, β-glucan, and alginate (PM) (110.5 μmol per 50 mg) or β-glucan itself (96.2 μmol per 50 mg). The body weight gain of obese mice fed with a HF-WGLSF diet was significantly reduced (42.0% lower than the HF group, 30.2% lower than the physical mixture) with decreased cell size in white adipose tissue and similar levels of serum lipid profiles to the control of the low-fat (LF) group. Western blotting experiments showed the down-regulated lipogenic transcription factor of SREBP-1c and fatty acid synthase (FAS), but the lipid-oxidation related transcription factors of peroxisome proliferator-activated receptor-α (PPAR-α) and phosphorylated AMP-activated protein kinase (p-AMPK) were up-regulated. Energy metabolism analysis revealed increased lipid-sourced energy expenditure with higher heat production and respiratory exchange ratios. Consistently, the expression of hypothalamic pro-opiomelanocortin (POMC), favoring energy expenditure, was increased significantly while the neuropeptide Y (NPY) was reduced. Thus, the increased energy expenditure stimulated by starch in a whole-grain-like structural form is responsible for the reduced body weight gain of obese mice fed with a high fat-based diet.
Fat Quality Influences the Obesogenic Effect of High Fat Diets
Abstract
High fat and/or carbohydrate intake are associated with an elevated risk for obesity and chronic diseases such as diabetes and cardiovascular diseases. The harmful effects of a high fat diet could be different, depending on dietary fat quality. In fact, high fat diets rich in unsaturated fatty acids are considered less deleterious for human health than those rich in saturated fat. In our previous studies, we have shown that rats fed a high fat diet developed obesity and exhibited a decrease in oxidative capacity and an increase in oxidative stress in liver mitochondria. To investigate whether polyunsaturated fats could attenuate the above deleterious effects of high fat diets, energy balance and body composition were assessed after two weeks in rats fed isocaloric amounts of a high-fat diet (58.2% by energy) rich either in lard or safflower/linseed oil. Hepatic functionality, plasma parameters, and oxidative status were also measured. The results show that feeding on safflower/linseed oil diet attenuates the obesogenic effect of high fat diets and ameliorates the blood lipid profile. Conversely, hepatic steatosis and mitochondrial oxidative stress appear to be negatively affected by a diet rich in unsaturated fatty acids.
Soybean Oil Is More Obesogenic and Diabetogenic than Coconut Oil and Fructose in Mouse: Potential Role for the Liver
Abstract
The obesity epidemic in the U.S. has led to extensive research into potential contributing dietary factors, especially fat and fructose. Recently, increased consumption of soybean oil, which is rich in polyunsaturated fatty acids (PUFAs), has been proposed to play a causal role in the epidemic. Here, we designed a series of four isocaloric diets (HFD, SO-HFD, F-HFD, F-SO-HFD) to investigate the effects of saturated versus unsaturated fat, as well as fructose, on obesity and diabetes. C57/BL6 male mice fed a diet moderately high in fat from coconut oil and soybean oil (SO-HFD, 40% kcal total fat) showed statistically significant increases in weight gain, adiposity, diabetes, glucose intolerance and insulin resistance compared to mice on a diet consisting primarily of coconut oil (HFD). They also had fatty livers with hepatocyte ballooning and very large lipid droplets as well as shorter colonic crypt length. While the high fructose diet (F-HFD) did not cause as much obesity or diabetes as SO-HFD, it did cause rectal prolapse and a very fatty liver, but no balloon injury. The coconut oil diet (with or without fructose) increased spleen weight while fructose in the presence of soybean oil increased kidney weight. Metabolomics analysis of the liver showed an increased accumulation of PUFAs and their metabolites as well as γ-tocopherol, but a decrease in cholesterol in SO-HFD. Liver transcriptomics analysis revealed a global dysregulation of cytochrome P450 (Cyp) genes in SO-HFD versus HFD livers, most notably in the Cyp3a and Cyp2c families. Other genes involved in obesity (e.g., Cidec, Cd36), diabetes (Igfbp1), inflammation (Cd63), mitochondrial function (Pdk4) and cancer (H19) were also upregulated by the soybean oil diet. Taken together, our results indicate that in mice a diet high in soybean oil is more detrimental to metabolic health than a diet high in fructose or coconut oil.
Metabolic and inflammatory postprandial effect of a highly saturated fat meal and its relationship to abdominal obesity
Abstract
Introduction: The postprandial stage is associated with the increase of markers related to cardiovascular risk, and its intensity depends on the metabolic state. Objective: To determine the impact of a high-fat meal intake on the metabolic and inflammatory profile, and its relationship to abdominal obesity. Materials and methods: This clinical trial included 42 individuals (21 with abdominal obesity). We measured glucose, insulin, lipid profile, reactive C protein, lipopolysaccharides, and interleukin 6 in fasting blood, and four hours after eating. Results: Besides obesity, we found insulin resistance and higher levels of fasting triacylglycerides and C-reactive protein. There were higher postprandial responses to glucose, insulin, and triacylglycerides. Interleukin 6 decreased in the non-obese group, and lipopolysaccharides increased in both groups. Conclusions: A saturated high-fat food intake produced a greater impact on the glycemic variables in the group with obesity, while it affected the lipids in both groups. However, the increase of triacylglycerides was higher in the presence of a high basal concentration, and it promoted the increase of lipopolysaccharides. The basal and postprandial inflammatory state affected the group with obesity more. The postprandial moment reflected the most frequent state of the individuals on a normal day and evidenced the capacity of the metabolic response to food intake, as well as early metabolic risk states.
Keywords: Obesity; inflammation; postprandial period; diet; high-fat; insulin resistance; lipopolysaccharides.
Trans-Fatty Acids Aggravate Obesity, Insulin Resistance and Hepatic Steatosis in C57BL/6 Mice, Possibly by Suppressing the IRS1 Dependent Pathway
Abstract
Trans-fatty acid consumption has been reported as a risk factor for metabolic disorders and targeted organ damages. Nonetheless, little is known about the roles and mechanisms of trans-fatty acids in obesity, insulin resistance (IR) and hepatic steatosis. Adult C57BL/6 male mice were fed with four different diets for 20 weeks: normal diet (ND), high fat diet (HFD), low trans-fatty acids diet (LTD) and high trans-fatty acid diet (HTD). The diet-induced metabolic disorders were assessed by evaluating body weight, glucose tolerance test, hepatic steatosis and plasma lipid profiles post 20-week diet. Histological (H&E, Oil-Red-O) staining and western blot analysis were employed to assess liver steatosis and potential signaling pathways. After 20-weeks of diet, the body weights of the four groups were 29.61 ± 1.89 g (ND), 39.04 ± 4.27 g (HFD), 34.09 ± 2.62 g (LTD) and 43.78 ± 4.27 g (HTD) (p < 0.05), respectively. HFD intake significantly impaired glucose tolerance, which was impaired further in the mice consuming the HTD diet. The effect was further exacerbated by HTD diet. Moreover, the HTD group exhibited significantly more severe liver steatosis compared with HFD group possibly through regulating adipose triglyceride lipase. The group consuming the HTD also exhibited significantly reduced levels of IRS1, phosphor-PKC and phosphor-AKT. These results support our hypothesis that consumption of a diet high in trans-fatty acids induces higher rates of obesity, IR and hepatic steatosis in male C57BL/6 mice, possibly by suppressing the IRS1dependent pathway.
Keywords: hepatic steatosis; insulin resistance; obesity; trans-fatty acid.
Fat Quantity and Quality, as Part of a Low-Fat, Vegan Diet, Are Associated with Changes in Body Composition, Insulin Resistance, and Insulin Secretion. A 16-Week Randomized Controlled Trial
Abstract
Macronutrient composition of the diet influences the development of obesity and insulin resistance. The aim of this study was to assess the role of dietary fat quantity and fatty acid composition in body composition, insulin resistance, and insulin secretion. An open parallel randomized trial design was used. Overweight participants (n = 75) were randomized to follow a low-fat vegan (n = 38) or control diet (n = 37) for 16 weeks. Dual X-ray absorptiometry was used to measure body composition. Insulin resistance was assessed with the Homeostasis Model Assessment (HOMA-IR) index. Insulin secretion was assessed after stimulation with a liquid breakfast (Boost Plus, Nestle, Vevey, Switzerland). Self-reported 3-day diet records were used to assess dietary intake. A linear regression model was used to test the relationship between fat intake and body composition, insulin resistance, and insulin secretion. Changes in fat intake expressed as percent of total energy consumed correlated positively with changes in fat mass (r = 0.52; p < 0.001; and 0.347; p = 0.006, respectively), even after adjustment for changes in body-mass index (BMI) and energy intake (0.33; p = 0.01). Decreased intakes of C18:0 (r = 0.37, p = 0.004) and CLA-trans-10-cis12 (r = 0.40, p = 0.002), but increased intake of C18:2 (r = -0.40, p = 0.002) and C18:3 (p = -0.36, p = 0.006), were associated with a decrease in HOMA-IR, independent on changes in BMI and energy intake. The main fatty acids associated with changes in fasting insulin secretion were C12:0 (r = -0.31, p = 0.03), and TRANS 16:1 (r = -0.33, p = 0.02), both independent on changes in BMI and energy intake. Our findings demonstrate that, in the context of a low-fat vegan diet, decreased intake of saturated and trans fats and increased relative content of polyunsaturated fatty acids, particularly linoleic and α-linolenic acids, are associated with decreased fat mass and insulin resistance, and enhanced insulin secretion.
Sleep extension is a feasible lifestyle intervention in free-living adults who are habitually short sleepers: a potential strategy for decreasing intake of free sugars? A randomized controlled pilot study
ABSTRACT
Background
Evidence suggests that short sleep duration may be a newly identified modifiable risk factor for obesity, yet there is a paucity of studies to investigate this.
Objective
We assessed the feasibility of a personalized sleep extension protocol in adults aged 18–64 y who are habitually short sleepers (5 to <7 h), with sleep primarily measured by wrist actigraphy. In addition, we collected pilot data to assess the effects of extended sleep on dietary intake and quality measured by 7-d food diaries, resting and total energy expenditure, physical activity, and markers of cardiometabolic health.
Design
Forty-two normal-weight healthy participants who were habitually short sleepers completed this free-living, 4-wk, parallel-design randomized controlled trial. The sleep extension group (n = 21) received a behavioral consultation session targeting sleep hygiene. The control group (n = 21) maintained habitual short sleep.
Results
Rates of participation, attrition, and compliance were 100%, 6.5%, and 85.7%, respectively. The sleep extension group significantly increased time in bed [0:55 hours:minutes (h:mm); 95% CI: 0:37, 1:12 h:mm], sleep period (0:47 h:mm; 95% CI: 0:29, 1:05 h:mm), and sleep duration (0:21 h:mm; 95% CI: 0:06, 0:36 h:mm) compared with the control group. Sleep extension led to reduced intake of free sugars (–9.6 g; 95% CI: –16.0, –3.1 g) compared with control (0.7 g; 95% CI: –5.7, 7.2 g) (P = 0.042). A sensitivity analysis in plausible reporters showed that the sleep extension group reduced intakes of fat (percentage), carbohydrates (grams), and free sugars (grams) in comparison to the control group. There were no significant differences between groups in markers of energy balance or cardiometabolic health.
Conclusions
We showed the feasibility of extending sleep in adult short sleepers. Sleep extension led to reduced free sugar intakes and may be a viable strategy to facilitate limiting excessive consumption of free sugars in an obesity-promoting environment. This trial was registered at
www.clinicaltrials.gov
as NCT02787577.
Perfluoroalkyl substances and changes in body weight and resting metabolic rate in response to weight-loss diets: A prospective study
Abstract
Background
The potential endocrine-disrupting effects of perfluoroalkyl substances (PFASs) have been demonstrated in animal studies, but whether PFASs may interfere with body weight regulation in humans is largely unknown. This study aimed to examine the associations of PFAS exposure with changes in body weight and resting metabolic rate (RMR) in a diet-induced weight-loss setting.
Methods and findings
In the 2-year POUNDS Lost randomized clinical trial based in Boston, Massachusetts, and Baton Rouge, Louisiana, that examined the effects of energy-restricted diets on weight changes, baseline plasma concentrations of major PFASs were measured among 621 overweight and obese participants aged 30–70 years. Body weight was measured at baseline and 6, 12, 18, and 24 months. RMR and other metabolic parameters, including glucose, lipids, thyroid hormones, and leptin, were measured at baseline and 6 and 24 months. Participants lost an average of 6.4 kg of body weight during the first 6 months (weight-loss period) and subsequently regained an average of 2.7 kg of body weight during the period of 6–24 months (weight regain period). After multivariate adjustment, baseline PFAS concentrations were not significantly associated with concurrent body weight or weight loss during the first 6 months. In contrast, higher baseline levels of PFASs were significantly associated with a greater weight regain, primarily in women. In women, comparing the highest to the lowest tertiles of PFAS concentrations, the multivariate-adjusted mean weight regain (SE) was 4.0 (0.8) versus 2.1 (0.9) kg for perfluorooctanesulfonic acid (PFOS) (Ptrend = 0.01); 4.3 (0.9) versus 2.2 (0.8) kg for perfluorooctanoic acid (PFOA) (Ptrend = 0.007); 4.7 (0.9) versus 2.5 (0.9) kg for perfluorononanoic acid (PFNA) (Ptrend = 0.006); 4.9 (0.9) versus 2.7 (0.8) kg for perfluorohexanesulfonic acid (PFHxS) (Ptrend = 0.009); and 4.2 (0.8) versus 2.5 (0.9) kg for perfluorodecanoic acid (PFDA) (Ptrend = 0.03). When further adjusted for changes in body weight or thyroid hormones during the first 6 months, results remained similar. Moreover, higher baseline plasma PFAS concentrations, especially for PFOS and PFNA, were significantly associated with greater decline in RMR during the weight-loss period and less increase in RMR during the weight regain period in both men and women. Limitations of the study include the possibility of unmeasured or residual confounding by socioeconomic and psychosocial factors, as well as possible relapse to the usual diet prior to randomization, which could have been rich in foods contaminated by PFASs through food packaging and also dense in energy.
Conclusions
In this diet-induced weight-loss trial, higher baseline plasma PFAS concentrations were associated with a greater weight regain, especially in women, possibly explained by a slower regression of RMR levels. These data illustrate a potential novel pathway through which PFASs interfere with human body weight regulation and metabolism. The possible impact of environmental chemicals on the obesity epidemic therefore deserves attention.
Changes in Intake of Fruits and Vegetables and Weight Change in United States Men and Women Followed for Up to 24 Years: Analysis from Three Prospective Cohort Studies
Abstract
Background
Current dietary guidelines recommend eating a variety of fruits and vegetables. However, based on nutrient composition, some particular fruits and vegetables may be more or less beneficial for maintaining or achieving a healthy weight. We hypothesized that greater consumption of fruits and vegetables with a higher fiber content or lower glycemic load would be more strongly associated with a healthy weight.
Methods and Findings
We examined the association between change in intake of specific fruits and vegetables and change in weight in three large, prospective cohorts of 133,468 United States men and women. From 1986 to 2010, these associations were examined within multiple 4-y time intervals, adjusting for simultaneous changes in other lifestyle factors, including other aspects of diet, smoking status, and physical activity. Results were combined using a random effects meta-analysis. Increased intake of fruits was inversely associated with 4-y weight change: total fruits -0.53 lb per daily serving (95% CI -0.61, -0.44), berries -1.11 lb (95% CI -1.45, -0.78), and apples/pears -1.24 lb (95% CI -1.62, -0.86). Increased intake of several vegetables was also inversely associated with weight change: total vegetables -0.25 lb per daily serving (95% CI -0.35, -0.14), tofu/soy -2.47 lb (95% CI, -3.09 to -1.85 lb) and cauliflower -1.37 lb (95% CI -2.27, -0.47). On the other hand, increased intake of starchy vegetables, including corn, peas, and potatoes, was associated with weight gain. Vegetables having both higher fiber and lower glycemic load were more strongly inversely associated with weight change compared with lower-fiber, higher-glycemic-load vegetables (p < 0.0001). Despite the measurement of key confounders in our analyses, the potential for residual confounding cannot be ruled out, and although our food frequency questionnaire specified portion size, the assessment of diet using any method will have measurement error.
Conclusions
Increased consumption of fruits and non-starchy vegetables is inversely associated with weight change, with important differences by type suggesting that other characteristics of these foods influence the magnitude of their association with weight change.
Kids Without Gardens More Likely to Get Fat
STOCKHOLM -- Children who grow up in dodgy neighborhoods and have little access to a garden or green space are at risk of
becoming obese
by the time they are 7 years old, researchers said here.
Children were 14% more likely to be overweight or obese if they lived in an area where access to green space was limited (OR 1.14, 95% CI 1.02-1.27) and were 35% more likely (OR 1.35, 95% CI 1.16-1.58)] if they grew up without a garden to frolic in, said
Giel Nijpels, MD, PhD,
professor of general practice medicine at the VU Medical Center, Amsterdam.
In his oral presentation at the annual meeting of the
European Association for the Study of Diabetes
, Nijpels also said the study of 6,467 children in the Millennium Cohort Study indicated that a poor neighborhood environment also was associated with a significant risk of being overweight.
AbstractObesity, which is caused by an energy imbalance between calorie intake and consumption, has become a major international health burden. Obesity increases the risk of insulin resistance and age‐related cognitive decline, accompanied by peripheral inflammation. (—)‐Epigallocatechin‐3‐gallate (EGCG), the major polyphenol in green tea, possesses antioxidant, anti‐inflammatory, and cardioprotective activities; however, few reports have focused on its potential effect on cognitive disorders. In this study, our goal was to investigate the protective effects of EGCG treatment on insulin resistance and memory impairment induced by a high‐fat and high‐fructose diet (HFFD). We randomly assigned 3‐mo‐old C57BL/6J mice to 3 groups with different diets: control group, HFFD group, and HFFD plus EGCG group. Memory loss was assessed by using the Morris water maze test, during which EGCG was observed to prevent HFFD‐elicited memory impairment and neuronal loss. Consistent with these results, EGCG attenuated HFFD‐induced neuronal damage. Of note, EGCG significantly ameliorated insulin resistance and cognitive disorder by up‐regulating the insulin receptor substrate‐1 (IRS‐1)/AKT and ERK/cAMP response element binding protein (CREB)/brain‐derived neurotrophic factor (BDNF) signaling pathways. Long‐term HFFD‐triggered neuroinflammation was restored by EGCG supplementation by inhibiting the MAPK and NF‐κB pathways, as well as the expression of inflammatory mediators, such as TNF‐α. EGCG also reversed high glucose and glucosamine‐induced insulin resistance in SH‐SY5Y neuronal cells by improving the oxidized cellular status and mitochondrial function. To our knowledge, this study is the first to provide compelling evidence that the nutritional compound EGCG has the potential to ameliorate HFFD‐triggered learning and memory loss.—Mi, Y., Qi, G., Fan, R., Qiao, Q., Sun, Y., Gao, Y., Liu, X. EGCG ameliorates high‐fat– and high‐fructose‐induced cognitive defects by regulating the IRS/AKT and ERK/CREB/BDNF signaling pathways in the CNS. FASEB J. 31, 4998–5011 (2017).
www.fasebj.org
Effect of Current Dietary Recommendations on Weight Loss and Cardiovascular Risk Factors
Abstract
Background
Dietary recommendations emphasize increased consumption of fruit, vegetables, and whole grain cereals for prevention of chronic disease.
Objectives
This study assessed the effect of dietary advice and/or food provision on body weight and
cardiovascular disease
risk factors.
Methods
Healthy overweight men (n = 209) and women (n = 710), mean age 44.7 years,
body mass index
[BMI] 32.4 kg/m2, were randomized between November 2005 and August 2009 to receive Health Canada’s food guide (control, n = 486) or 1 of 3 interventions: dietary advice consistent with both Dietary Approaches to Stop Hypertension (DASH) and dietary portfolio principles (n = 145); weekly food provision reflecting this advice (n = 148); or food delivery plus advice (n = 140). Interventions lasted 6 months with 12-month follow-up. Semiquantitative
food frequency questionnaires
and fasting blood,
anthropometric
and
blood pressure measurements
were obtained at baseline, 6 months, and 18 months.
Results
Participant retention at 6 and 18 months was 91% and 81%, respectively, after food provision compared to 67% and 57% when no food was provided (p < 0.0001). Test and control treatments showed small reductions in body weight (−0.8 to −1.2 kg),
waist circumference
(−1.1 to −1.9 cm), and
mean arterial pressure
(0.0 to −1.1 mm Hg) at 6 months and Framingham
coronary heart disease
risk score at 18 months (−0.19 to −0.42%), which were significant overall. Outcomes did not differ among test and control groups.
Conclusions
Provision of foods increased retention but only modestly increased intake of recommended foods. Current dietary recommendations showed small overall benefits in coronary heart disease risk factors. Additional dietary strategies to maximize these benefits are required. (Fruits, Vegetables, and Whole Grains: A
Community-based Intervention
;
NCT00516620
)
Tailoring dietary approaches for weight loss
Abstract
Although the ‘Low-Fat' diet was the predominant public health recommendation for weight loss and weight control for the past several decades, the obesity epidemic continued to grow during this time period. An alternative ‘low-carbohydrate' (Low-Carb) approach, although originally dismissed and even vilified, was comparatively tested in a series of studies over the past decade, and has been found in general to be as effective, if not more, as the Low-Fat approach for weight loss and for several related metabolic health measures. From a glass half full perspective, this suggests that there is more than one choice for a dietary approach to lose weight, and that Low-Fat and Low-Carb diets may be equally effective. From a glass half empty perspective, the average amount of weight lost on either of these two dietary approaches under the conditions studied, particularly when followed beyond 1 year, has been modest at best and negligible at worst, suggesting that the two approaches may be equally ineffective. One could resign themselves at this point to focusing on calories and energy intake restriction, regardless of macronutrient distributions. However, before throwing out the half-glass of water, it is worthwhile to consider that focusing on average results may mask important subgroup successes and failures. In all weight-loss studies, without exception, the range of individual differences in weight change within any particular diet groups is orders of magnitude greater than the average group differences between diet groups. Several studies have now reported that adults with greater insulin resistance are more successful with weight loss on a lower-carbohydrate diet compared with a lower-fat diet, whereas adults with greater insulin sensitivity are equally or more successful with weight loss on a lower-fat diet compared with a lower-carbohydrate diet. Other preliminary findings suggest that there may be some promise with matching individuals with certain genotypes to one type of diet over another for increasing weight-loss success. Future research to address the macronutrient intake component of the obesity epidemic should build on these recent insights and be directed toward effectively classifying individuals who can be differentially matched to alternate types of weight-loss diets that maximize weight-loss and weight-control success.
Keywords: insulin resistance, gene–diet interaction, weight-loss diets, low-fat, low-carbohydrate, high protein
A Systematic Review and Meta-Analysis of Changes in Body Weight in Clinical Trials of Vegetarian Diets
Abstract
In observational studies, vegetarians generally have lower body weights compared with omnivores. However, weight changes that occur when vegetarian diets are prescribed have not been well quantified. We estimated the effect on body weight when vegetarian diets are prescribed. We searched PubMed, EMBASE, and the Cochrane Central Register of Controlled Trials for articles through December 31, 2013. Additional articles were identified from reference lists. We included intervention trials in which participants were adults, interventions included vegetarian diets of ≥4 weeks’ duration without energy intake limitations, and effects on body weight were reported. Two investigators independently extracted data using predetermined fields. Estimates of body weight change, comparing intervention groups to untreated control groups, were derived using a random effects model to estimate the weighted mean difference. To quantify effects on body weight of baseline weight, sex, age, study duration, study goals, type of diet, and study authorship, additional analyses examined within-group changes for all studies reporting variance data. We identified 15 trials (17 intervention groups), of which 4 included untreated controls. Prescription of vegetarian diets was associated with a mean weight change of −3.4 kg (95% CI −4.4 to −2.4; P<0.001) in an intention-to-treat analysis and −4.6 kg (95% CI −5.4 to −3.8; P<0.001) in a completer analysis (omitting missing post-intervention values). Greater weight loss was reported in studies with higher baseline weights, smaller proportions of female participants, older participants, or longer durations, and in studies in which weight loss was a goal. Using baseline data for missing values, I 2 equaled 52.3 ( P=0.10), indicating moderate heterogeneity. When missing data were omitted, I 2 equaled 0 ( P=0.65), indicating low heterogeneity. Studies are relatively few, with variable quality. The prescription of vegetarian diets reduces mean body weight, suggesting potential value for prevention and management of weight-related conditions.
Comparison of the Atkins, Zone, Ornish, and LEARN Diets for Change in Weight and Related Risk Factors Among Overweight Premenopausal Women
Abstract
Context Popular diets, particularly those low in carbohydrates, have challenged current recommendations advising a low-fat, high-carbohydrate diet for weight loss. Potential benefits and risks have not been tested adequately.
Objective To compare 4 weight-loss diets representing a spectrum of low to high carbohydrate intake for effects on weight loss and related metabolic variables.
Design, Setting, and Participants Twelve-month randomized trial conducted in the United States from February 2003 to October 2005 among 311 free-living, overweight/obese (body mass index, 27-40) nondiabetic, premenopausal women.
Intervention Participants were randomly assigned to follow the Atkins (n = 77), Zone (n = 79), LEARN (n = 79), or Ornish (n = 76) diets and received weekly instruction for 2 months, then an additional 10-month follow-up.
Main Outcome Measures Weight loss at 12 months was the primary outcome. Secondary outcomes included lipid profile (low-density lipoprotein, high-density lipoprotein, and non–high-density lipoprotein cholesterol, and triglyceride levels), percentage of body fat, waist-hip ratio, fasting insulin and glucose levels, and blood pressure. Outcomes were assessed at months 0, 2, 6, and 12. The Tukey studentized range test was used to adjust for multiple testing.
Results Weight loss was greater for women in the Atkins diet group compared with the other diet groups at 12 months, and mean 12-month weight loss was significantly different between the Atkins and Zone diets (P<.05). Mean 12-month weight loss was as follows: Atkins, −4.7 kg (95% confidence interval [CI], −6.3 to −3.1 kg), Zone, −1.6 kg (95% CI, −2.8 to −0.4 kg), LEARN, −2.6 kg (−3.8 to −1.3 kg), and Ornish, −2.2 kg (−3.6 to −0.8 kg). Weight loss was not statistically different among the Zone, LEARN, and Ornish groups. At 12 months, secondary outcomes for the Atkins group were comparable with or more favorable than the other diet groups.
Conclusions In this study, premenopausal overweight and obese women assigned to follow the Atkins diet, which had the lowest carbohydrate intake, lost more weight and experienced more favorable overall metabolic effects at 12 months than women assigned to follow the Zone, Ornish, or LEARN diets. While questions remain about long-term effects and mechanisms, a low-carbohydrate, high-protein, high-fat diet may be considered a feasible alternative recommendation for weight loss.
Diabetes
Maternal nutrition: opportunities in the prevention of gestational diabetes
Abstract
Gestational diabetes mellitus (GDM) is currently defined as glucose intolerance that is of variable severity with onset or first recognition during pregnancy. The Hyperglycemia and Adverse Pregnancy Outcome Study, including 25 000 nondiabetic pregnant women in 15 centers across the world, reported that an average of 17.8% of pregnancies are affected by GDM and its frequency can be as high as 25.5% in some countries, based on the International Association of Diabetes and Pregnancy Study Groups criteria. Nevertheless, true global prevalence estimates of GDM are currently lacking due to the high level of heterogeneity in screening approaches, diagnostic criteria, and differences in the characteristics of the populations that were studied. The presence of systemic high blood glucose levels in pregnancy results in an adverse intrauterine environment, which has been shown to have a negative impact on short- and long-term health outcomes for both the mother and her offspring, including increased risks for the infant to develop obesity and for both mother and child to develop type 2 diabetes mellitus later in life. Epigenetic mechanisms that are directly influenced by environmental factors, including nutrition, may play a key role in shaping these future health risks and may be part of this vicious cycle. This article reviews the burden of GDM and the current evidence that supports maternal nutritional interventions as a promising strategy to break the cycle by addressing risk factors associated with GDM.
Diabetes UK evidence-based nutrition guidelines for the prevention and management of diabetes
Abstract
A summary of the latest evidence-based nutrition guidelines for the prevention and management of diabetes is presented. These guidelines are based on existing recommendations last published in 2011, and were formulated by an expert panel of specialist dietitians after a literature review of recent evidence. Recommendations have been made in terms of foods rather than nutrients wherever possible. Guidelines for education and care delivery, prevention of Type 2 diabetes, glycaemic control for Type 1 and Type 2 diabetes, cardiovascular disease risk management, management of diabetes-related complications, other considerations including comorbidities, nutrition support, pregnancy and lactation, eating disorders, micronutrients, food supplements, functional foods, commercial diabetic foods and nutritive and non-nutritive sweeteners are included. The sections on pregnancy and prevention of Type 2 diabetes have been enlarged and the weight management section modified to include considerations of remission of Type 2 diabetes. A section evaluating detailed considerations in ethnic minorities has been included as a new topic. The guidelines were graded using adapted 'GRADE' methodology and, where strong evidence was lacking, grading was not allocated. These 2018 guidelines emphasize a flexible, individualized approach to diabetes management and weight loss and highlight the emerging evidence for remission of Type 2 diabetes. The full guideline document is available at www.diabetes.org.uk/nutrition-guidelines.
Nutrition therapy within and beyond gestational diabetes
Abstract
With the global rising prevalence of gestational diabetes (GDM), an adaptable, economical approach to nutrition therapy that effectively controls maternal glycemia while promoting normal fetal growth will have far-reaching implications. The conventional focus has been to rigidly limit all types of carbohydrate. While controlling glucose, this approach fosters maternal anxiety and is a primary barrier to adherence. Many mothers substitute fat for carbohydrate, which may unintentionally enhance lipolysis, promote elevated free fatty acids (FFA), and worsen maternal insulin resistance (IR). Nutrition that worsens IR may facilitate nutrient shunting across the placenta, promoting excess fetal fat accretion. Evidence suggests that liberalizing higher quality, nutrient-dense carbohydrates results in controlled fasting/postprandial glucose, lower FFA, improved insulin action, vascular benefits, and may reduce excess infant adiposity. Thus, a less carbohydrate-restricted approach may improve maternal adherence when combined with higher quality carbohydrates, lower fat, appropriate caloric intake, and ethnically acceptable foods. Such a diet can be culturally sensitive, socioeconomically attentive, minimize further weight gain in GDM, with potential relevance for pregnancies complicated by overweight/obesity. Future research is needed to better understand the effect of macronutrient composition on the placenta and gut microbiome, the benefits/risks of nonnutritive sweeteners, and whether precision-nutrition is beneficial in pregnancy.
Abstract
Precision nutrition aims to prevent and manage chronic diseases by tailoring dietary interventions or recommendations to one or a combination of an individual's genetic background, metabolic profile, and environmental exposures. Recent advances in genomics, metabolomics, and gut microbiome technologies have offered opportunities as well as challenges in the use of precision nutrition to prevent and manage type 2 diabetes. Nutrigenomics studies have identified genetic variants that influence intake and metabolism of specific nutrients and predict individuals' variability in response to dietary interventions. Metabolomics has revealed metabolomic fingerprints of food and nutrient consumption and uncovered new metabolic pathways that are potentially modified by diet. Dietary interventions have been successful in altering abundance, composition, and activity of gut microbiota that are relevant for food metabolism and glycaemic control. In addition, mobile apps and wearable devices facilitate real-time assessment of dietary intake and provide feedback which can improve glycaemic control and diabetes management. By integrating these technologies with big data analytics, precision nutrition has the potential to provide personalised nutrition guidance for more effective prevention and management of type 2 diabetes. Despite these technological advances, much research is needed before precision nutrition can be widely used in clinical and public health settings. Currently, the field of precision nutrition faces challenges including a lack of robust and reproducible results, the high cost of omics technologies, and methodological issues in study design as well as high-dimensional data analyses and interpretation. Evidence is needed to support the efficacy, cost-effectiveness, and additional benefits of precision nutrition beyond traditional nutrition intervention approaches. Therefore, we should manage unrealistically high expectations and balance the emerging field of precision nutrition with public health nutrition strategies to improve diet quality and prevent type 2 diabetes and its complications.
Nutrition of children and adolescents with type 1 diabetes in the recommendations of the Mediterranean diet
Abstract in
Introduction: The nutrition of children and adolescents significantly affects the physical and mental development of those suffering from type 1 diabetes and their healthy peers. Nutrition rules for children and adolescents with type 1 diabetes do not differ from the principles of feeding their healthy peers. Hence, the demand for individual nutrients in type 1 diabetes and healthy people is the same. The nutrition of children and adolescents should meet the recommendations of the Institute of Food and Nutrition and the Polish Diabetes Association.
Aim of the study: Aim of the study is to present a pattern of nutrition for children and adolescents with type 1 diabetes, treated with intensive insulin therapy using the Mediterranean diet, which was recognised by the World Health Organization as a model of a healthy diet for both children and adults. Through the participation of a large number of natural products, it has antioxidant, chemopreventive, and anti-inflammatory effects, it reduces the level of triglycerides and cholesterol, as well as postprandial glycaemia.
Conclusions: Żywienie dzieci i młodzieży istotnie wpływa na rozwój fizyczny i psychiczny dziecka - zarówno chorego na cukrzycę typu 1, jak i zdrowego. Zasady odżywiania dzieci i młodzieży z cukrzycą typu 1 nie różnią się od zasad żywienia ich zdrowych rówieśników. Dlatego też zapotrzebowanie na poszczególne składniki pokarmowe u dzieci chorych na cukrzycę typu 1 oraz dla zdrowych jest takie samo. Sposób odżywiania dzieci i młodzieży powinien spełniać zalecenia Instytutu Żywności i Żywienia oraz Polskiego Towarzystwa Diabetologicznego.
Paradigm Shifts in Nutrition Therapy for Type 2 Diabetes
Abstract
Currently, the low-energy diet is the only recognized nutrition therapy for type 2 diabetes in Japan. However, in recent decades, many foreign scientific organizations have accepted various nutritional approaches to manage diabetes, such as the low-carbohydrate diet, the Mediterranean diet, diet approaches to stop hypertension (DASH), and the vegetarian diet. Moreover, growing evidence has called into question classical nutritional approaches such as the low-fat diet for the prevention of cardiovascular disease and the low-protein diet for the prevention of diabetic kidney disease. Similarly, the recommended nutrition therapy for diabetes may change in near future. Such changes in nutrition therapy must be dynamic and based on not only scientific evidence but also each patient's narrative.
Diabetes, Nutrition, and Exercise
Abstract
Aging is associated with body composition changes that lead to glucose intolerance and increased risk of diabetes. The incidence of diabetes increases with aging, and the prevalence has increased because of the increased life expectancy of the population. Lifestyle modifications through nutrition and exercise in combination with medications are the main components of diabetes management. The potential benefits of nutrition and exercise intervention in older people with diabetes are enormous. Nutrition and exercise training are feasible even in frail older people living in care homes and should take into consideration individual circumstances, cultural factors, and ethnic preferences.
The health effects of medical nutrition therapy by dietitians in patients with diabetes: A systematic review and meta-analysis: Nutrition therapy and diabetes
Abstract
Aims
Intensive lifestyle, dietary interventions and patient education have been recommended as key milestones in to facilitate the management of Diabetes and contain the growing incidence. We performed a systematic review and meta-analysis to assess the health benefits of medical nutrition therapy among patients with diabetes.
Design
A systematic search was performed in MEDLINE/PubMed, SCOPUS, and Cochrane library from onset up to February 2019 to identify trials investigating the health effect of Medical nutrition (MNT) in patients with diabetes. Random-effects models were used to calculate the effect sizes as weighted mean difference (WMD) and 95% confidence intervals (CI).
Results
Eleven studies containing 1227 participants were included in the meta-analysis. Pooled results showed a significant reduction in Fasting blood sugar (FBS) (WMD= −8.85 mg/dl, 95% CI: −14.41, −3.28), HbA1c (WMD: −0.43%, 95% CI: −0.69, −0.17), weight (WMD: −1.54 kg, 95% CI: −2.44, −0.64), Body mass index (BMI) (WMD: −0.34 Kg/m2, 95% CI: −0.52, −0.17), waist circumference (WMD: −2.16 cm, 95% CI: −4.09, −0.23), cholesterol (WMD: −4.06 mg/dl, 95% CI: −7.31, −0.81), Systolic blood pressure (SBP) (WMD: −7.90 mmHg, 95% CI: −13.03, −2.77). Results of meta-regression analysis based on age of participants and duration of intervention were not significant.
Conclusions
Patients with diabetes who received medical nutrition therapy showed significant improvements in outcome measures of FBS, HbA1c, weight, BMI, waist circumference, cholesterol, and SBP.
Summary
Precision
nutrition
aims to prevent and manage chronic diseases by tailoring dietary interventions or recommendations to one or a combination of an individual's genetic background, metabolic profile, and environmental exposures. Recent advances in genomics,
metabolomics
, and gut
microbiome
technologies have offered opportunities as well as challenges in the use of precision nutrition to prevent and manage type 2
diabetes
.
Nutrigenomics
studies have identified
genetic variants
that influence intake and metabolism of specific nutrients and predict individuals' variability in response to dietary interventions. Metabolomics has revealed metabolomic
fingerprints
of food and nutrient consumption and uncovered new
metabolic pathways
that are potentially modified by diet. Dietary interventions have been successful in altering abundance, composition, and activity of
gut microbiota
that are relevant for food metabolism and
glycaemic control
. In addition, mobile apps and wearable devices facilitate real-time assessment of dietary intake and provide feedback which can improve glycaemic control and diabetes management. By integrating these technologies with big data analytics, precision nutrition has the potential to provide personalised nutrition guidance for more effective prevention and management of type 2 diabetes. Despite these technological advances, much research is needed before precision nutrition can be widely used in clinical and public health settings. Currently, the field of precision nutrition faces challenges including a lack of robust and reproducible results, the high cost of
omics
technologies, and methodological issues in study design as well as high-dimensional data analyses and interpretation. Evidence is needed to support the efficacy, cost-effectiveness, and additional benefits of precision nutrition beyond traditional nutrition intervention approaches. Therefore, we should manage unrealistically high expectations and balance the emerging field of precision nutrition with
public health nutrition
strategies to improve diet quality and prevent type 2 diabetes and its complications.
Academy of Nutrition and Dietetics Nutrition Practice Guideline for Type 1 and Type 2 Diabetes in Adults: Nutrition Intervention Evidence Reviews and Recommendations
The Academy of Nutrition and Dietetics (Academy) Nutrition Practice Guideline (NPG) for Type 1 and Type 2 Diabetes in Adults is a newly developed guideline. 1
It has also been published in the Academy’s Evidence Analysis Library (EAL). 2
The NPG updates the 2008 Diabetes Type 1 and 2 Evidence-Based NPG for Adults. 3
, 4
Evidence for the effectiveness of medical nutrition therapy (MNT) provided by registered dietitian nutritionists (RDNs) and the integration of MNT into the Nutrition Care Process is reviewed in an accompanying article. 1
MNT plays a critical role in managing both types of diabetes, reducing the potential complications related to poor glycemic, lipid, and blood pressure control, and improving quality of life. 1
, 2
, 5
, 6
The need to provide clients with evidence-based nutrition care is essential for providing optimum diabetes care.
Etiologic effects and optimal intakes of foods and nutrients for risk of cardiovascular diseases and diabetes: Systematic reviews and meta-analyses from the Nutrition and Chronic Diseases Expert Group (NutriCoDE)
Abstract
Background
Dietary habits are major contributors to coronary heart disease, stroke, and diabetes. However, comprehensive evaluation of etiologic effects of dietary factors on cardiometabolic outcomes, their quantitative effects, and corresponding optimal intakes are not well-established.
Objective
To systematically review the evidence for effects of dietary factors on cardiometabolic diseases, including comprehensively assess evidence for causality; estimate magnitudes of etiologic effects; evaluate heterogeneity and potential for bias in these etiologic effects; and determine optimal population intake levels.
Methods
We utilized Bradford-Hill criteria to assess probable or convincing evidence for causal effects of multiple diet-cardiometabolic disease relationships. Etiologic effects were quantified from published or de novo meta-analyses of prospective studies or randomized clinical trials, incorporating standardized units, dose-response estimates, and heterogeneity by age and other characteristics. Potential for bias was assessed in validity analyses. Optimal intakes were determined by levels associated with lowest disease risk.
Results
We identified 10 foods and 7 nutrients with evidence for causal cardiometabolic effects, including protective effects of fruits, vegetables, beans/legumes, nuts/seeds, whole grains, fish, yogurt, fiber, seafood omega-3s, polyunsaturated fats, and potassium; and harms of unprocessed red meats, processed meats, sugar-sweetened beverages, glycemic load, trans-fats, and sodium. Proportional etiologic effects declined with age, but did not generally vary by sex. Established optimal population intakes were generally consistent with observed national intakes and major dietary guidelines. In validity analyses, the identified effects of individual dietary components were similar to quantified effects of dietary patterns on cardiovascular risk factors and hard endpoints.
Conclusions
These novel findings provide a comprehensive summary of causal evidence, quantitative etiologic effects, heterogeneity, and optimal intakes of major dietary factors for cardiometabolic diseases, informing disease impact estimation and policy planning and priorities.
Nutrition Therapy in Gestational Diabetes Mellitus: Time to Move Forward
Nutrition therapy remains the conventional first-line approach to treatment of gestational diabetes mellitus (GDM). It will reach every woman with GDM across differing diagnostic criteria (1) and phenotypic heterogeneity (2). The goal of nutrition in pregnancy is to support maternal, placental, and fetal metabolic needs, and it may be the first introduction to a lifetime of healthy eating (3). In this way, nutrition therapy in GDM becomes an early-stage intervention in the vicious cycle of intergenerational obesity and diabetes (4). Importantly, because the prevalence of GDM has reached an alarming ≥20% of pregnancies (5), a cost-effective approach to management is urgently needed. While controlling fetal exposure to maternal hyperglycemia and overnutrition, effective nutrition can treat GDM in a way that is fiscally reasonable and culturally sensitive, ultimately reducing the need for medication and intensified health care resource use (1).
The importance of nutrition therapy in GDM is a premise unlikely to be contested. Yet, the widely accepted approach rooted in carbohydrate restriction was challenged more than a decade ago based on concerns related to higher fat intake and exacerbation of maternal insulin resistance by free fatty acids (6,7). The dietary management of diabetes in pregnancy has remained in limbo ever since, with no specific guidelines for nutrition therapy in GDM, a travesty that has resulted in non–evidence-based, fragmented, and inconsistent approaches globally (8–12). Action is necessary not only because of the powerful influence of nutrition on fetal programming and development (13,14) but also because of the ability to positively impact the health of millions of mother-infant dyads. Currently, nutrition therapy appears to have become our Achilles heel, such that despite our strength, we have limped forward in generating clinical evidence to substantiate …
Diabetes UK evidence‐based nutrition guidelines for the prevention and management of diabetes
Abstract
A summary of the latest evidence‐based nutrition guidelines for the prevention and management of diabetes is presented. These guidelines are based on existing recommendations last published in 2011, and were formulated by an expert panel of specialist dietitians after a literature review of recent evidence. Recommendations have been made in terms of foods rather than nutrients wherever possible. Guidelines for education and care delivery, prevention of Type 2 diabetes, glycaemic control for Type 1 and Type 2 diabetes, cardiovascular disease risk management, management of diabetes‐related complications, other considerations including comorbidities, nutrition support, pregnancy and lactation, eating disorders, micronutrients, food supplements, functional foods, commercial diabetic foods and nutritive and non‐nutritive sweeteners are included. The sections on pregnancy and prevention of Type 2 diabetes have been enlarged and the weight management section modified to include considerations of remission of Type 2 diabetes. A section evaluating detailed considerations in ethnic minorities has been included as a new topic. The guidelines were graded using adapted ‘GRADE’ methodology and, where strong evidence was lacking, grading was not allocated. These 2018 guidelines emphasize a flexible, individualized approach to diabetes management and weight loss and highlight the emerging evidence for remission of Type 2 diabetes.
Nutrition Therapy for Adults With Diabetes or Prediabetes: A Consensus Report
This Consensus Report is intended to provide clinical professionals with evidence-based guidance about individualizing nutrition therapy for adults with diabetes or prediabetes. Strong evidence supports the efficacy and cost-effectiveness of nutrition therapy as a component of quality diabetes care, including its integration into the medical management of diabetes; therefore, it is important that all members of the health care team know and champion the benefits of nutrition therapy and key nutrition messages. Nutrition counseling that works toward improving or maintaining glycemic targets, achieving weight management goals, and improving cardiovascular risk factors (e.g., blood pressure, lipids, etc.) within individualized treatment goals is recommended for all adults with diabetes and prediabetes.
Though it might simplify messaging, a “one-size-fits-all” eating plan is not evident for the prevention or management of diabetes, and it is an unrealistic expectation given the broad spectrum of people affected by diabetes and prediabetes, their cultural backgrounds, personal preferences, co-occurring conditions (often referred to as comorbidities), and socioeconomic settings in which they live. Research provides clarity on many food choices and eating patterns that can help people achieve health goals and quality of life. The American Diabetes Association (ADA) emphasizes that medical nutrition therapy (MNT) is fundamental in the overall diabetes management plan, and the need for MNT should be reassessed frequently by health care providers in collaboration with people with diabetes across the life span, with special attention during times of changing health status and life stages (
1
–
3
).
This Consensus Report now includes information on prediabetes, and previous ADA nutrition position statements, the last of which was published in 2014 (
4
), did not. Unless otherwise noted, the research reviewed was limited to those studies conducted in adults diagnosed with prediabetes, type 1 diabetes, and/or type 2 diabetes. Nutrition therapy for children with diabetes or women with gestational diabetes mellitus is not addressed in this review but is covered in other ADA publications, specifically Standards of Medical Care in Diabetes (
5
,
6
).
The Effectiveness and Cost of Lifestyle Interventions Including Nutrition Education for Diabetes Prevention: A Systematic Review and Meta-Analysis
Abstract
Background
Type 2 diabetes is a significant public health concern. With the completion of the Diabetes Prevention Program, there has been a proliferation of studies attempting to translate this evidence base into practice. However, the cost, effectiveness, and cost-effectiveness of these adapted interventions is unknown.
Objective
The purpose of this systematic review was to conduct a comprehensive meta-analysis to synthesize the effectiveness, cost, and cost-effectiveness of lifestyle diabetes prevention interventions and compare effects by intervention delivery agent (dietitian vs non-dietitian) and channel (in-person vs technology-delivered).
Methods
English and full-text research articles published up to July 2015 were identified using the Cochrane Library, PubMed, Education Resources Information Center, CAB Direct, Science Direct, and Google Scholar. Sixty-nine studies met inclusion criteria. Most employed both dietary and physical activity intervention components (four of 69 were diet-only interventions). Changes in weight, fasting and 2-hour blood glucose concentration, and hemoglobin A1c were extracted from each article. Heterogeneity was measured by the I 2 index, and study-specific effect sizes or mean differences were pooled using a random effects model when heterogeneity was confirmed.
Results
Participants receiving intervention with nutrition education experienced a reduction of 2.07 kg (95% CI 1.52 to 2.62; P<0.001; I 2=90.99%, 95% CI 88.61% to 92.87%) in weight at 12 months with effect sizes over time ranging from small (0.17, 95% CI 0.04 to 0.30; P=0.012; I 2= 86.83%, 95% CI 80.42% to 91.14%) to medium (0.65, 95% CI 0.49 to 0.82; P<0.001; I 2=98.75%, 95% CI 98.52% to 98.94). Effect sizes for 2-hour blood glucose and hemoglobin A1c level changes ranged from small to medium. The meta-regression analysis revealed a larger relative weight loss in dietitian-delivered interventions than in those delivered by nondietitians (full sample: –1.0 kg; US subsample: –2.4 kg), and did not find statistical evidence that the delivery channel was an important predictor of weight loss. The average cost per kilogram weight loss ranged from $34.06 over 6 months to $1,005.36 over 12 months. The cost of intervention per participant delivered by dietitians was lower than interventions delivered by non-dietitians, although few studies reported costs.
Conclusions
Lifestyle interventions are effective in reducing body weight and glucose-related outcomes. Dietitian-delivered interventions, compared with those delivered by other personnel, achieved greater weight reduction. No consistent trend was identified across different delivery channels.
Acceptability of a very‐low‐energy diet in Type 2 diabetes: patient experiences and behaviour regulation
Abstract
Aims
To evaluate the acceptability of an 8‐week very‐low‐energy diet for remission of Type 2 diabetes, and to identify barriers and facilitators of adherence and behaviour‐regulation strategies used by participants in the Counterbalance study.
Methods
Eighteen of 30 participants in the Counterbalance study (ISRCTN88634530) took part in semi‐structured interviews. Of these, 15 participants were interviewed before and after the 8‐week very‐low‐energy diet intervention. Thematic analysis was used to analyse the narratives.
Results
The prospect of diabetes remission, considerable weight loss, and long‐term health improvement provided participants with substantial initial motivation. This motivation was sustained through the experience of rapid weight loss, improvements in blood glucose levels, social support and increased physical and psychological well‐being. Overall, adherence to the very‐low‐energy diet for 8 weeks was perceived as much easier than anticipated, but required personal effort. Participants addressed challenges by removing food from the environment, planning, avoidance of tempting situations or places, and self‐distraction. Weight loss and improvements in blood glucose levels lead to a sense of achievement and improvements in physical and psychological wellbeing.
Conclusions
Dietary treatment for reversal of Type 2 diabetes is acceptable and feasible in motivated participants, and the process is perceived as highly gratifying. Research outside of controlled trial settings is needed to gauge the generalisability of these findings.
Fresh fruit consumption in relation to incident diabetes and diabetic vascular complications: A 7-y prospective study of 0.5 million Chinese adults
Abstract
Background
Despite the well-recognised health benefits of fresh fruit consumption, substantial uncertainties remain about its potential effects on incident diabetes and, among those with diabetes, on risks of death and major vascular complications.
Methods and findings
Between June 2004 and July 2008, the nationwide China Kadoorie Biobank study recruited 0.5 million adults aged 30–79 (mean 51) y from ten diverse localities across China. During ~7 y of follow-up, 9,504 new diabetes cases were recorded among 482,591 participants without prevalent (previously diagnosed or screen-detected) diabetes at baseline, with an overall incidence rate of 2.8 per 1,000 person-years. Among 30,300 (5.9%) participants who had diabetes at baseline, 3,389 deaths occurred (overall mortality rate 16.5 per 1,000), along with 9,746 cases of macrovascular disease and 1,345 cases of microvascular disease. Cox regression yielded adjusted hazard ratios (HRs) associating each disease outcome with self-reported fresh fruit consumption, adjusting for potential confounders such as age, sex, region, socio-economic status, other lifestyle factors, body mass index, and family history of diabetes. Overall, 18.8% of participants reported consuming fresh fruit daily, and 6.4% never/rarely (non-consumers), with the proportion of non-consumers about three times higher in individuals with previously diagnosed diabetes (18.9%) than in those with screen-detected diabetes (6.7%) or no diabetes (6.0%). Among those without diabetes at baseline, higher fruit consumption was associated with significantly lower risk of developing diabetes (adjusted HR = 0.88 [95% CI 0.83–0.93] for daily versus non-consumers, p < 0.001, corresponding to a 0.2% difference in 5-y absolute risk), with a clear dose–response relationship. Among those with baseline diabetes, higher fruit consumption was associated with lower risks of all-cause mortality (adjusted HR = 0.83 [95% CI 0.74–0.93] per 100 g/d) and microvascular (0.72 [0.61–0.87]) and macrovascular (0.87 [0.82–0.93]) complications (p < 0.001), with similar HRs in individuals with previously diagnosed and screen-detected diabetes; estimated differences in 5-y absolute risk between daily and non-consumers were 1.9%, 1.1%, and 5.4%, respectively. The main limitation of this study was that, owing to its observational nature, we could not fully exclude the effects of residual confounding.
Conclusion
In this large epidemiological study in Chinese adults, higher fresh fruit consumption was associated with significantly lower risk of diabetes and, among diabetic individuals, lower risks of death and development of major vascular complications.
EGCG ameliorates high‐fat– and high‐fructose‐induced cognitive defects by regulating the IRS/AKT and ERK/CREB/BDNF signaling pathways in the CNS
AbstractObesity, which is caused by an energy imbalance between calorie intake and consumption, has become a major international health burden. Obesity increases the risk of insulin resistance and age‐related cognitive decline, accompanied by peripheral inflammation. (—)‐Epigallocatechin‐3‐gallate (EGCG), the major polyphenol in green tea, possesses antioxidant, anti‐inflammatory, and cardioprotective activities; however, few reports have focused on its potential effect on cognitive disorders. In this study, our goal was to investigate the protective effects of EGCG treatment on insulin resistance and memory impairment induced by a high‐fat and high‐fructose diet (HFFD). We randomly assigned 3‐mo‐old C57BL/6J mice to 3 groups with different diets: control group, HFFD group, and HFFD plus EGCG group. Memory loss was assessed by using the Morris water maze test, during which EGCG was observed to prevent HFFD‐elicited memory impairment and neuronal loss. Consistent with these results, EGCG attenuated HFFD‐induced neuronal damage. Of note, EGCG significantly ameliorated insulin resistance and cognitive disorder by up‐regulating the insulin receptor substrate‐1 (IRS‐1)/AKT and ERK/cAMP response element binding protein (CREB)/brain‐derived neurotrophic factor (BDNF) signaling pathways. Long‐term HFFD‐triggered neuroinflammation was restored by EGCG supplementation by inhibiting the MAPK and NF‐κB pathways, as well as the expression of inflammatory mediators, such as TNF‐α. EGCG also reversed high glucose and glucosamine‐induced insulin resistance in SH‐SY5Y neuronal cells by improving the oxidized cellular status and mitochondrial function. To our knowledge, this study is the first to provide compelling evidence that the nutritional compound EGCG has the potential to ameliorate HFFD‐triggered learning and memory loss.—Mi, Y., Qi, G., Fan, R., Qiao, Q., Sun, Y., Gao, Y., Liu, X. EGCG ameliorates high‐fat– and high‐fructose‐induced cognitive defects by regulating the IRS/AKT and ERK/CREB/BDNF signaling pathways in the CNS.
A Low-Fat Vegan Diet Improves Glycemic Control and Cardiovascular Risk Factors in a Randomized Clinical Trial in Individuals With Type 2 Diabetes
Abstract
OBJECTIVE—We sought to investigate whether a low-fat vegan diet improves glycemic control and cardiovascular risk factors in individuals with type 2 diabetes.
RESEARCH DESIGN AND METHODS—Individuals with type 2 diabetes (n = 99) were randomly assigned to a low-fat vegan diet (n = 49) or a diet following the American Diabetes Association (ADA) guidelines (n = 50). Participants were evaluated at baseline and 22 weeks.
RESULTS—Forty-three percent (21 of 49) of the vegan group and 26% (13 of 50) of the ADA group participants reduced diabetes medications. Including all participants, HbA1c (A1C) decreased 0.96 percentage points in the vegan group and 0.56 points in the ADA group (P = 0.089). Excluding those who changed medications, A1C fell 1.23 points in the vegan group compared with 0.38 points in the ADA group (P = 0.01). Body weight decreased 6.5 kg in the vegan group and 3.1 kg in the ADA group (P < 0.001). Body weight change correlated with A1C change (r = 0.51, n = 57, P < 0.0001). Among those who did not change lipid-lowering medications, LDL cholesterol fell 21.2% in the vegan group and 10.7% in the ADA group (P = 0.02). After adjustment for baseline values, urinary albumin reductions were greater in the vegan group (15.9 mg/24h) than in the ADA group (10.9 mg/24 h) (P = 0.013).
CONCLUSIONS—Both a low-fat vegan diet and a diet based on ADA guidelines improved glycemic and lipid control in type 2 diabetic patients. These improvements were greater with a low-fat vegan diet.
Prevention and Management of Type 2 Diabetes: Dietary Components and Nutritional Strategies
In the past couple of decades, evidence from prospective observational studies and clinical trials has converged to support the importance of individual nutrients, foods, and dietary patterns in the prevention and management of type 2 diabetes. The quality of dietary fats and carbohydrates consumed is more crucial than the quantity of these macronutrients. Diets rich in whole grains, fruits, vegetables, legumes, nuts, moderate in alcohol consumption, and lower in refined grains, red/processed meats, and sugar-sweetened beverages have demonstrated to reduce diabetes risk and improve glycemic control and blood lipids in patients with diabetes. Several healthful dietary patterns emphasizing the overall diet quality can be adapted to appropriate personal and cultural food preferences and calorie needs for weight control and diabetes prevention and management. Although considerable progress has been made in developing and implementing evidence-based nutrition recommendations in developed countries, concerted global efforts and policies are warranted to alleviate regional disparities.
Dietary reversal of Type 2 diabetes motivated by research knowledge
Reversal of Type 2 diabetes in the context of bariatric surgery is currently of great interest. Discussion of the rapid and dramatic effects of bariatric surgery upon the pathophysiology of Type 2 diabetes has concentrated almost exclusively on surgically induced change in the incretin hormones [
1
,
2
]. Little consideration has been given to reversal of Type 2 diabetes by the effects of caloric restriction alone. We report a person with Type 2 diabetes who returned to normal fasting blood glucose and glycated haemoglobin (HbA1c) after reading a notice about a grant award in Balance concerning the effects of a hypocaloric diet on glucose control.
A 46‐year‐old woman was found to have diabetes on routine screening [oral glucose tolerance test (OGTT) January 2009: 8.1 mmol/l fasting; 14.4 mmol/l 2‐h]. At the time of diagnosis HbA1c was 6.9% and weight was 120.2 kg, with body mass index of 42.6 kg/m2. On diagnosis of diabetes she joined Diabetes UK and read in Balance of a grant award for research on the mechanism of hypocaloric reversal of diabetes. She enquired about being a subject, but National Health Service (NHS) ethics, NHS Research and Development (R&D), Primary Care Trust (PCT) R&D and Caldicott permissions had yet to be granted. She asked to participate in due course but set about losing weight. She attended weekly meetings of Overeaters Anonymous Great Britain for support. By the time the research permissions had been obtained 8 months later, weight had fallen to 108.9 kg with fasting blood glucose of 4.8 mmol/l and HbA1c 5.9%.
Motivation to bring about sustained weight loss was provided by the information that this would result in normalization of blood glucose control. Although this may not appear remarkable to many diabetologists who have observed similar effects of weight loss in individual cases, this has rarely been described in the literature. The phenomenon was first described by Claude Bouchardet who observed that glucose disappeared from his patients’ urine during food shortage in the siege of Paris in 1870 [
3
]. More recently, dietary therapy alone was reported to achieve normal glucose tolerance in 20% of people with Type 2 diabetes [
4
]. The key to response lies in compliance and the longer‐term difficulty lies in sustaining the negative calorie balance.
Close examination of the hypotheses based upon unique changes of incretins following bariatric surgery suggests inconsistencies. The ‘hindgut hypothesis’ postulates that expedited delivery of nutrients to the distal small intestine enhances glucagon‐like peptide 1 (GLP‐1) secretion, possibly with other incretins. However, the absolute increase in GLP‐1 secretion reported is small [
5
] and not observed in Type 2 diabetes [
6
]. High‐dose replacement by GLP‐1 agonists brings about only modest improvement in glucose control [
7
]. The ‘foregut hypothesis’ postulates that reversal of diabetes occurs as a result of exclusion of the duodenum and proximal jejunum from exposure to nutrients [
2
]. This has been postulated to decrease postprandial gastric inhibitory polypeptide (GIP) and decrease glucagon secretion [
1
]. However, not all studies show GIP to be decreased and some show increased secretion in the weeks after gastric bypass [
5
,
8
].
Whereas the incretin hormones achieve fine regulation, substrate supply drives metabolism. The basic metabolic fact has been overlooked that the restriction of calorie intake which necessarily follows bariatric surgery will bring about a rapid decrease in the fatty liver typical of Type 2 diabetes. The degree of restriction relates to the extent of the surgical procedure. Even moderate dietary restriction is associated with profound change in hepatic insulin sensitivity and marked fall in hepatic glucose output early during a hypocaloric diet [
9
]. The associated time course of decrease in liver volume is over days [
10
]. Conversely, the period before onset of Type 2 diabetes is characterized by accumulation of liver fat [
11
].
The observation of reversal of Type 2 diabetes, by diet rather than by surgery, is most important. This should inform advice given to people with Type 2 diabetes at the time of diagnosis.
Precision nutrition for prevention and management of type 2 diabetes
Summary
Precision nutrition aims to prevent and manage chronic diseases by tailoring dietary interventions or recommendations to one or a combination of an individual's genetic background, metabolic profile, and environmental exposures. Recent advances in genomics, metabolomics, and gut microbiome technologies have offered opportunities as well as challenges in the use of precision nutrition to prevent and manage type 2 diabetes. Nutrigenomics studies have identified genetic variants that influence intake and metabolism of specific nutrients and predict individuals' variability in response to dietary interventions. Metabolomics has revealed metabolomic fingerprints of food and nutrient consumption and uncovered new metabolic pathways that are potentially modified by diet. Dietary interventions have been successful in altering abundance, composition, and activity of gut microbiota that are relevant for food metabolism and glycaemic control. In addition, mobile apps and wearable devices facilitate real-time assessment of dietary intake and provide feedback which can improve glycaemic control and diabetes management. By integrating these technologies with big data analytics, precision nutrition has the potential to provide personalised nutrition guidance for more effective prevention and management of type 2 diabetes. Despite these technological advances, much research is needed before precision nutrition can be widely used in clinical and public health settings. Currently, the field of precision nutrition faces challenges including a lack of robust and reproducible results, the high cost of omics technologies, and methodological issues in study design as well as high-dimensional data analyses and interpretation. Evidence is needed to support the efficacy, cost-effectiveness, and additional benefits of precision nutrition beyond traditional nutrition intervention approaches. Therefore, we should manage unrealistically high expectations and balance the emerging field of precision nutrition with public health nutrition strategies to improve diet quality and prevent type 2 diabetes and its complications.
Very Low-Calorie Diet and 6 Months of Weight Stability in Type 2 Diabetes: Pathophysiological Changes in Responders and Nonresponders
Abstract
OBJECTIVE Type 2 diabetes mellitus (T2DM) is generally regarded as an irreversible chronic condition. Because a very low-calorie diet (VLCD) can bring about acute return to normal glucose control in some people with T2DM, this study tested the potential durability of this normalization. The underlying mechanisms were defined.
RESEARCH DESIGN AND METHODS People with a T2DM duration of 0.5–23 years (n = 30) followed a VLCD for 8 weeks. All oral agents or insulins were stopped at baseline. Following a stepped return to isocaloric diet, a structured, individualized program of weight maintenance was provided. Glucose control, insulin sensitivity, insulin secretion, and hepatic and pancreas fat content were quantified at baseline, after return to isocaloric diet, and after 6 months to permit the primary comparison of change between post–weight loss and 6 months in responders. Responders were defined as achieving fasting blood glucose <7 mmol/L after return to isocaloric diet.
RESULTS Weight fell (98.0 ± 2.6 to 83.8 ± 2.4 kg) and remained stable over 6 months (84.7 ± 2.5 kg). Twelve of 30 participants achieved fasting plasma glucose <7 mmol/L after return to isocaloric diet (responders), and 13 of 30 after 6 months. Responders had a shorter duration of diabetes and a higher initial fasting plasma insulin level. HbA1c fell from 7.1 ± 0.3 to 5.8 ± 0.2% (55 ± 4 to 40 ± 2 mmol/mol) in responders (P < 0.001) and from 8.4 ± 0.3 to 8.0 ± 0.5% (68 ± 3 to 64 ± 5 mmol/mol) in nonresponders, remaining constant at 6 months (5.9 ± 0.2 and 7.8 ± 0.3% [41 ± 2 and 62 ± 3 mmol/mol], respectively). The responders were characterized by return of first-phase insulin response.
CONCLUSIONS A robust and sustainable weight loss program achieved continuing remission of diabetes for at least 6 months in the 40% who responded to a VLCD by achieving fasting plasma glucose of <7 mmol/L. T2DM is a potentially reversible condition.
Restoring normoglycaemia by use of a very low calorie diet in long‐ and short‐duration Type 2 diabetes
AbstractAims
To establish whether an 8‐week very‐low‐calorie diet could improve glycaemic control in Type 2 diabetes of long duration.
Methods
A total of 29 people with Type 2 diabetes [short‐duration group (diabetes duration < 4 years), n = 15; long‐duration group (diabetes duration > 8 years), n = 14] completed an 8‐week very‐low‐calorie diet, with assessments of fasting anthropometry, blood tests and blood pressure at baseline and weeks 1, 4 and 8 of the diet.
Results
Similar weight loss was achieved in the short‐ and long‐duration groups (14.8 ± 0.8% and 14.4 ± 0.7% respectively; P = 0.662). The glucose response to acute calorie restriction was heterogeneous in the long‐duration group with some responding similarly to those in the short‐duration group, some responding, but only slowly, and others not responding at all. Overall, HbA1c concentration in the short‐ vs. long‐duration groups fell to 44 ± 2 vs. 64 ± 6 mmol/l (6.2 ± 0.2 vs. 8.0 ± 0.5%; P = 0.002). Fasting plasma glucose levels decreased to 5.8 ± 0.2 vs. 8.4 ± 1.1 mmol/l (P = 0.024) respectively. A total of 87% of the short‐duration group and 50% of the long‐duration group achieved non‐diabetic fasting plasma glucose levels at week 8. Clinically significant improvements in blood pressure and lipid profile were seen regardless of diabetes duration.
Conclusion
In people with Type 2 diabetes of > 8 years' duration, a therapeutic trial of a very‐low‐calorie diet may be undertaken with a 50% chance of achieving non‐diabetic fasting glucose levels off all antidiabetic therapies.
Diet and diabetes revisited, yet again
Dietary modification has the potential to appreciably reduce the risk of progression of prediabetes to type 2 diabetes (T2D)3, with several high-profile randomized controlled trials (RCTs) conducted in persons of varying ethnicities in different countries that consistently show a halving of risk (1). The benefit appears to persist many years after the conclusion of the interventions (2). Medical nutrition therapy is the mainstay of treatment of T2D. Compliance with dietary advice results in improvement in glycemic control and reduction in cardiovascular risk regardless of duration of disease. A meaningful reduction in glycated hemoglobin after intensified nutrition therapy has been observed in patients with longstanding T2D whose oral hypoglycemic or insulin treatment had been optimized (3). Given that most people at risk of or with T2D are overweight or obese, it is hardly surprising that weight loss (typically ≥5% of initial body weight) has been the most consistent nutrition-related determinant of positive outcomes (4). Reducing excess adiposity is the cornerstone of all nutrition recommendations for prevention and treatment of T2D. Two systematic reviews and meta-analyses published in this issue of the Journal relate to aspects of nutrition for which there is less universal agreement (5, 6).
Livesey et al (6) explored whether there is a dose-response relation between dietary glycemic load (GL) and risk of developing T2D. The meta-analysis, which included 24 prospective cohort studies and 7.5 million person-years of follow-up, showed a relative risk for T2D of 1.45 (95% CI: 1.31, 1.61) for a 100-g increment in GL, a relation apparent at all doses of GL >95 g/2000 kcal. A further additional novel finding was that 97% of the heterogeneity between studies was explained by validity of the dietary instrument, sex (the association between GL and T2D was significant only in women), and ethnicity (the association was stronger in European Americans than in other ethnicities combined). The sex difference may be explained by sex differences in dietary behavior or standard of recording rather than inherent/genetic differences, and the more striking effect among European Americans may be explained by the fact that they constituted the substantial majority of the individuals included in the meta-analysis.
Very Low–Calorie Diet Mimics the Early Beneficial Effect of Roux-en-Y Gastric Bypass on Insulin Sensitivity and β-Cell Function in Type 2 Diabetic Patients
Abstract
Marked improvement in glycemic control occurs in patients with type 2 diabetes mellitus shortly after Roux-en-Y gastric bypass surgery (RYGB) and before there is major weight loss. The objective of this study was to determine whether the magnitude of this change is primarily due to caloric restriction or is unique to the surgical procedure. We studied eleven subjects who underwent RYGB and fourteen subjects mean-matched for BMI, HbA1c, and diabetes duration who were admitted to our inpatient research unit and given a very low–calorie diet (VLCD) of 500 kcal/day with a macronutrient content similar to that consumed by patients after RYGB. Frequently sampled intravenous glucose tolerance tests were performed before and after interventions. Both groups lost an equivalent amount of weight over a mean study period of 21 days. Insulin sensitivity, acute insulin secretion after intravenous glucose administration, and β-cell function as determined by disposition index improved to a similar extent in both groups. Likewise, changes in fasting glucose and fructosamine levels were similar. Based on these data, VLCD improves insulin sensitivity and β-cell function just as well as RYGB in the short term.
Reversal of type 2 diabetes in youth who adhere to a very-low-energy diet: a pilot study
Abstract
Aims/hypothesis
The aim of the study was to investigate whether a very-low-energy diet (VLED) is a feasible and acceptable treatment option for type 2 diabetes in children and adolescents, and whether adherence can lead to rapid weight loss, reversal of type 2 diabetes and reduced liver fat as seen in adult studies.
Methods
Eight participants with type 2 diabetes and obesity, aged 7–16 years, non-medicated (n = 1) or treated with metformin (n = 7) and in some cases insulin (n = 3), followed a VLED (<3360 kJ/day) for 8 weeks, then transitioned to a hypocaloric diet (∼6300 kJ/day) that they followed to 34 weeks. HbA1c, fasting glucose and 2 h post-glucose load plasma glucose (2hG) were determined from fasting blood and an OGTT. Liver fat concentration was quantified using proton magnetic resonance spectroscopy. Adherence was defined as ≥5% weight loss during the 8 week VLED.
Results
Adherers (n = 5) and non-adherers (n = 3) had median weight loss of 7.5% and 0.5%, respectively, at 8 weeks. Overall, HbA1c (mean [SE] 8.1% [0.7%] to 6.6% [0.5%]; p = 0.004) and 2hG (15.6 [1.6] mmol/l to 11.3 [1.0] mmol/l; p = 0.009) were significantly reduced at 8 weeks compared with baseline. Liver fat was also significantly reduced from baseline (14.7% [2.2%]) to 8 weeks (5.8% [1.7%]; p = 0.001). Only three out of eight participants met non-alcoholic fatty liver disease (NAFLD) criteria (≥5.5%) at 8 weeks, compared with eight out of eight at baseline. The three participants on insulin therapy at baseline were able to cease therapy during the 8 week VLED. At 34 weeks, adherers (n = 5) achieved 12.3% weight loss, none met NAFLD criteria and four did not meet American Diabetes Association criteria for type 2 diabetes.
Conclusions/interpretation
A VLED appears to be a feasible treatment option for some youth with type 2 diabetes on metformin therapy. Youth who agree to participate and adhere to a VLED achieve rapid weight loss, dramatic reductions in liver fat and reversal of type 2 diabetes. This highlights the capacity of a VLED to be used as a first-line treatment option in newly diagnosed youth. A larger trial with a control group and longer follow-up will be required to encourage a change in standard treatment.
Fasting-mimicking diet promotes Ngn3-driven β-cell regeneration to reverse diabetes
Summary
Stem cell-based therapies can potentially reverse organ dysfunction and diseases but the removal of impaired tissue and reactivation of the program leading to organ regeneration pose major challenges. In mice, a four-day fasting mimicking diet (FMD) induces a step-wise expression of Sox17 and Pdx-1, resembling that observed during pancreatic development, followed by Ngn3-driven generation of insulin-producing β-cells. FMD cycles restore insulin secretion and glucose homeostasis in both a type 2 and type 1 diabetes mouse models. In human type 1 diabetes pancreatic islets, fasting conditions reduce PKA and mTOR activity and induce Sox2 and Ngn3 expression and insulin production. The effects of the FMD are reversed by IGF-1 treatment and recapitulated by PKA and mTOR inhibition. These results indicate that a FMD promotes the reprogramming of pancreatic cells to restore insulin generation in islets from T1D patients and reverse both T1D and T2D phenotypes in mouse models.
Association Between Dietary Factors and Mortality From Heart Disease, Stroke, and Type 2 Diabetes in the United States
Abstract
IMPORTANCE
In the United States, national associations of individual dietary factors with specific cardiometabolic diseases are not well established.
OBJECTIVE
To estimate associations of intake of 10 specific dietary factors with mortality due to heart disease, stroke, and type 2 diabetes (cardiometabolic mortality) among US adults.
DESIGN, SETTING, AND PARTICIPANTS
A comparative risk assessment model incorporated data and corresponding uncertainty on population demographics and dietary habits from National Health and Nutrition Examination Surveys (1999–2002: n = 8104; 2009–2012: n = 8516); estimated associations of diet and disease from meta-analyses of prospective studies and clinical trials with validity analyses to assess potential bias; and estimated disease-specific national mortality from the National Center for Health Statistics.
EXPOSURES
Consumption of 10 foods/nutrients associated with cardiometabolic diseases: fruits, vegetables, nuts/seeds, whole grains, unprocessed red meats, processed meats, sugar-sweetened beverages (SSBs), polyunsaturated fats, seafood omega-3 fats, and sodium.
MAIN OUTCOMES AND MEASURES
Estimated absolute and percentage mortality due to heart disease, stroke, and type 2 diabetes in 2012. Disease-specific and demographic-specific (age, sex, race, and education) mortality and trends between 2002 and 2012 were also evaluated.
RESULTS
In 2012, 702 308 cardiometabolic deaths occurred in US adults, including 506 100 from heart disease (371 266 coronary heart disease, 35 019 hypertensive heart disease, and 99 815 other cardiovascular disease), 128 294 from stroke (16 125 ischemic, 32 591 hemorrhagic, and 79 578 other), and 67 914 from type 2 diabetes. Of these, an estimated 318 656 (95% uncertainty interval [UI], 306 064–329 755; 45.4%) cardiometabolic deaths per year were associated with suboptimal intakes—48.6% (95% UI, 46.2%–50.9%) of cardiometabolic deaths in men and 41.8% (95% UI, 39.3%–44.2%) in women; 64.2% (95% UI, 60.6%–67.9%) at younger ages (25–34 years) and 35.7% (95% UI, 33.1%–38.1%) at older ages (≥75 years); 53.1% (95% UI, 51.6%–54.8%) among blacks, 50.0% (95% UI, 48.2%–51.8%) among Hispanics, and 42.8% (95% UI, 40.9%–44.5%) among whites; and 46.8% (95% UI, 44.9%–48.7%) among lower-, 45.7% (95% UI, 44.2%–47.4%) among medium-, and 39.1% (95% UI, 37.2%–41.2%) among higher-educated individuals. The largest numbers of estimated diet-related cardiometabolic deaths were related to high sodium (66 508 deaths in 2012; 9.5% of all cardiometabolic deaths), low nuts/seeds (59 374; 8.5%), high processed meats (57 766; 8.2%), low seafood omega-3 fats (54 626; 7.8%), low vegetables (53 410; 7.6%), low fruits (52 547; 7.5%), and high SSBs (51 694; 7.4%). Between 2002 and 2012, population-adjusted US cardiometabolic deaths per year decreased by 26.5%. The greatest decline was associated with insufficient polyunsaturated fats (−20.8% relative change [95% UI, −18.5% to −22.8%]), nuts/seeds (−18.0% [95% UI, −14.6% to −21.0%]), and excess SSBs (−14.5% [95% UI, −12.0% to −16.9%]). The greatest increase was associated with unprocessed red meats (+14.4% [95% UI, 9.1%–19.5%]).
CONCLUSIONS AND RELEVANCE
Dietary factors were estimated to be associated with a substantial proportion of deaths from heart disease, stroke, and type 2 diabetes. These results should help identify priorities, guide public health planning, and inform strategies to alter dietary habits and improve health.
Aging
Epigenetics: Linking Nutrition to Molecular Mechanisms in Aging
Abstract
Healthy aging has become a major goal of public health. Many studies have provided evidence and theories to explain molecular mechanisms of the aging process. Recent studies suggest that epigenetic mechanisms are responsible for life span and the progression of aging. Epigenetics is a fascinating field of molecular biology, which studies heritable modifications of DNA and histones that regulate gene expression without altering the DNA sequence. DNA methylation is a major epigenetic mark that shows progressive changes during aging. Recent studies have investigated aging-related DNA methylation as a biomarker that predicts cellular age. Interestingly, growing evidence proposes that nutrients play a crucial role in the regulation of epigenetic modifiers. Because various nutrients and their metabolites function as substrates or cofactors for epigenetic modifiers, nutrition can modulate or reverse epigenetic marks in the genome as well as expression patterns. Here, we will review the results on aging-associated epigenetic modifications and the possible mechanisms by which nutrition, including nutrient availability and bioactive compounds, regulate epigenetic changes and affect aging physiology.
Nutritional Considerations for Healthy Aging and Reduction in Age-Related Chronic Disease
Abstract
A projected doubling in the global population of people aged ≥60 y by the year 2050 has major health and economic implications, especially in developing regions. Burdens of unhealthy aging associated with chronic noncommunicable and other age-related diseases may be largely preventable with lifestyle modification, including diet. However, as adults age they become at risk of "nutritional frailty," which can compromise their ability to meet nutritional requirements at a time when specific nutrient needs may be high. This review highlights the role of nutrition science in promoting healthy aging and in improving the prognosis in cases of age-related diseases. It serves to identify key knowledge gaps and implementation challenges to support adequate nutrition for healthy aging, including applicability of metrics used in body-composition and diet adequacy for older adults and mechanisms to reduce nutritional frailty and to promote diet resilience. This review also discusses management recommendations for several leading chronic conditions common in aging populations, including cognitive decline and dementia, sarcopenia, and compromised immunity to infectious disease. The role of health systems in incorporating nutrition care routinely for those aged ≥60 y and living independently and current actions to address nutritional status before hospitalization and the development of disease are discussed.
Aging and nutrition. Paving the way to better health
Abstract
Sufficient caloric intake is important to maintain the balanced health status, especially during the period of aging, as aging and sickness share paths. Maintaining adequate nutritional balance is the best preventive measure to counteract the risk of malnutrition. There are several causes for malnutrition in elderly people, and some techniques such as anthropometric measurements, laboratory and clinical parameters could help to diagnose malnutrition in these patients. The use of a simple validated questionnaire called the 'Mini Nutritional Assessment' measures the nutritional status of elderly patients. In this review, we discuss about the malnutrition in elderly people with and without a known cause and we present some of nutritional intervention. There are promising strategies that help overcoming malnutrition.
Nutrition Across the Lifespan for Healthy Aging: Proceedings of a Workshop
Excerpt
In September 2016, the National Academies of Sciences, Engineering, and Medicine convened a workshop to examine trends and patterns in aging and factors related to healthy aging in the United States, with a focus on nutrition, and how nutrition can sustain and promote healthy aging, not just in late adulthood, but beginning in pregnancy and early childhood and extending throughout the lifespan. Participants discussed the role of nutrition in the aging process at various stages in life, changes in organ systems over the lifespan and changes that occur with age related to cognitive, brain, and mental health, and explored opportunities to move forward in promoting healthy aging in the United States. This publication summarizes the presentations and discussions from the workshop.
Nutrition Recommendations in Elderly and Aging
Abstract
Maintaining optimal health and well-being in the older adult requires understanding of how physiologic changes influence nutritional status, familiarity with the available validated tools to assess status, identification of factors predisposing older adults to malnutrition, and evidence-based practice regarding the nutritional needs of this age group. Evidence-based guidance on these core practice components is provided to the clinician in this article.
Diet and Skin Aging-From the Perspective of Food Nutrition
Abstract
We regularly face primary challenges in deciding what to eat to maintain young and healthy skin, defining a healthy diet and the role of diet in aging. The topic that currently attracts maximum attention is ways to maintain healthy skin and delay skin aging. Skin is the primary barrier that protects the body from external aggressions. Skin aging is a complex biological process, categorized as chronological aging and photo-aging, and is affected by internal factors and external factors. With the rapid breakthrough of medicine in prolonging human life and the rapid deterioration of environmental conditions, it has become urgent to find safe and effective methods to treat skin aging. For diet, as the main way for the body to obtain energy and nutrients, people have gradually realized its importance to the skin. Therefore, in this review, we discuss the skin structure, aging manifestations, and possible mechanisms, summarize the research progress, challenges, possible directions of diet management, and effects of foodborne antioxidants on skin aging from the perspective of food and nutrition.
Personalized nutrition and healthy aging
Abstract
The human lifespan and quality of life depend on complex interactions among genetic, environmental, and lifestyle factors. Aging research has been remarkably advanced by the development of high-throughput “omics” technologies. Differences between chronological and biological ages, and identification of factors (eg, nutrition) that modulate the rate of aging can now be assessed at the individual level on the basis of telomere length, the epigenome, and the metabolome. Nevertheless, the understanding of the different responses of people to dietary factors, which is the focus of precision nutrition research, remains incomplete. The lack of reliable dietary assessment methods constitutes a significant challenge in nutrition research, especially in elderly populations. For practical and successful personalized diet advice, big data techniques are needed to analyze and integrate the relevant omics (ie, genomic, epigenomic, metabolomics) with an objective and longitudinal capture of individual nutritional and environmental information. Application of such techniques will provide the scientific evidence and knowledge needed to offer actionable, personalized health recommendations to transform the promise of personalized nutrition into reality.
Aging Gut Microbiota at the Cross-Road between Nutrition, Physical Frailty, and Sarcopenia: Is There a Gut–Muscle Axis?
Abstract
Inadequate nutrition and physical inactivity are the mainstays of primary sarcopenia–physiopathology in older individuals. Gut microbiota composition is strongly dependent on both of these elements, and conversely, can also influence the host physiology by modulating systemic inflammation, anabolism, insulin sensitivity, and energy production. The bacterial metabolism of nutrients theoretically influences skeletal muscle cell functionality through producing mediators that drive all of these systemic effects. In this study, we review the scientific literature supporting the concept of the involvement of gut microbiota in primary sarcopenia physiopathology. First, we examine studies associating fecal microbiota alterations with physical frailty, i.e., the loss of muscle performance and normal muscle mass. Then, we consider studies exploring the effects of exercise on gut microbiota composition. Finally, we examine studies demonstrating the possible effects of mediators produced by gut microbiota on skeletal muscle, and intervention studies considering the effects of prebiotic or probiotic administration on muscle function. Even if there is no evidence of a distinct gut microbiota composition in older sarcopenic patients, we conclude that the literature supports the possible presence of a “gut–muscle axis”, whereby gut microbiota may act as the mediator of the effects of nutrition on muscle cells.
Nutrition and other lifestyle influences on arterial aging
Abstract
As our world’s population ages, cardiovascular diseases (CVD) will become an increasingly urgent public health problem. A key antecedent to clinical CVD and many other chronic disorders of aging is age-related arterial dysfunction, characterized by increased
arterial stiffness
and impaired arterial endothelial function. Accumulating evidence demonstrates that diet and nutrition may favorably modulate these arterial functions with aging, but many important questions remain. In this review, we will summarize the available information on
dietary patterns
and nutritional factors that have been studied for their potential to reduce arterial stiffness and improve endothelial function with age, with an emphasis on: 1) underlying physiological mechanisms, and 2) emerging areas of research on nutrition and arterial aging that may hold promise for preventing age-related CVD.
Dietary patterns, food groups and telomere length: a systematic review of current studies
Abstract
Telomere length (TL) is recognized as a biomarker of aging and shorter telomeres are linked with shorter lifespan. Inter-individual variability in telomere length is highly heritable. However, there has been a resurgence of interest in the controversial relationship between diet and TL. Evaluating the impact of diet at the food group and dietary pattern level will provide greater insight into the effect of diet on TL dynamics, which are of significant importance in health and longevity. This article reports the first systematic review of the relation between food groups, dietary patterns and TL in human populations based on PRISMA guidelines.
Design: PubMed, Science Direct, The Cochrane Library and Google Scholar databases were electronically searched for all relevant studies, up to November 2015. Among the 17 included studies, 3 and 10 of them were regarding the effect of dietary patterns and various food groups on TL, respectively. Also, in 4 studies, both dietary patterns and different food groups were assessed in relation to TL. Mediterranean dietary pattern was related to longer TL in 3 studies. Five studies indicated beneficial effect of fruits or vegetables on TL. In 7 studies, a reverse association between TL and intake of cereals, processed meat, and fats and oils was reported. Our systematic review supports the health benefits of adherence to Mediterranean diet on TL. Except for the fruits and vegetables, which showed positive association with TL, results were inconsistent for other dietary factors. Also, certain food categories including processed meat, cereals and sugar-sweetened beverages may be associated with shorter TLs. However, additional epidemiological evidence and clinical trials should be considered in future research in order to develop firm conclusions in this regard.
Ultra-processed food consumption and the risk of short telomeres in an elderly population of the Seguimiento Universidad de Navarra (SUN) Project
Abstract
Background: Telomere length (TL) is a marker of biological age that may be affected by dietary factors through oxidation and inflammation mechanisms. In addition, ultra-processed food (UPF) consumption has increased worldwide and it has been associated with the risk of developing several diseases.
Objectives: We aimed to evaluate the association between UPF consumption and the risk of having short telomeres in an elderly population of the Seguimiento Universidad de Navarra (SUN) Project.
Methods: This is a cross-sectional study of 886 participants (645 men and 241 women) aged 57-91 y recruited from the SUN Project (Spain, 1999-2018). TL was measured from saliva samples by real-time qPCR at baseline and UPF consumption was collected using a validated 136-item FFQ and classified according to the NOVA system. We evaluated the association between consumption of energy-adjusted UPF categorized into quartiles (low, medium-low, medium-high, and high consumption) and the risk of having short telomeres (<20th percentile) using logistic regression models.
Results: Those participants with the highest UPF consumption had almost twice the odds of having short telomeres compared with those with the lowest consumption (adjusted OR: 1.82; 95% CI: 1.05, 3.22; P-trend = 0.03).
Conclusions: A higher consumption of UPF (>3 servings/d) was associated with higher risk of having shorter telomeres in an elderly Spanish population of the SUN Project.This trial was registered at clinicaltrials.gov as
NCT02669602
.
Keywords: SUN cohort; cross-sectional studies; diet; telomere length; ultra-processed food.
Telomeres, Nutrition, and Longevity: Can We Really Navigate Our Aging?
Abstract
Telomeres are dynamic chromosome-end structures that serve as guardians of genome stability. They are known to be one of the major determinants of aging and longevity in higher mammals. Studies have demonstrated a direct correlation between telomere length and life expectancy, stress, DNA damage, and onset of aging-related diseases. This review discusses the most important factors that influence our telomeres. Various genetic and environmental factors such as diet, physical activity, obesity, and stress are known to influence health and longevity as well as telomere dynamics. Individuals currently have the opportunity to modulate the dynamics of their aging and health span, monitor these processes, and even make future projections by following their telomere dynamics. As telomeres react to positive as well as negative health factors, we should be able to directly influence our telomere metabolism, slow their deterioration, and diminish our aging and perhaps extend our life and health span.
Plant-Rich Dietary Patterns, Plant Foods and Nutrients, and Telomere Length
Abstract
The world's population is aging as a consequence of an increased global life expectancy. Identifying simple strategies to promote healthy aging (i.e., absence of major chronic diseases, preserved physical and cognitive functions, intact mental health, and good quality of life) have emerged as a major public health concern. Identifying biomarkers to better characterize the aging process is a research priority. Telomeres are repetitive DNA sequences at chromosome ends that prevent the loss of genomic DNA, protecting its physical integrity. Telomere length (TL) is considered a biomarker of aging: shorter telomeres are associated with a decreased life expectancy and increased rates of age-related chronic diseases. Telomere attrition has been shown to be accelerated by oxidative stress and inflammation. Since edible plants contain plenty of compounds with antioxidant and anti-inflammatory properties, it is plausible that their sustained consumption might help counteract telomere attrition. In this narrative review, we update evidence on the association between plant-rich dietary patterns and plant-based foods and TL. First, we summarize findings from observational studies on the association between TL and 1) adherence to plant-rich dietary patterns (mainly, but not only, focused on the Mediterranean diet); 2) consumption of seeds (mostly focused on nuts, grains, and coffee); and 3) intake of carotenoids, one of the plant-derived bioactives most studied in health and disease. Second, we summarize the main randomized controlled trials evaluating the effect on TL of dietary interventions involving either plant-rich dietary patterns or plant foods. Even though evidence from trials is very limited, several observational studies have reinforced the suggestive benefits of adherence to the Mediterranean diet (a plant-rich dietary pattern), consumption of seeds (and its derivatives), and dietary intake of carotenoids on TL, which further supports the research benefits of plant-rich dietary patterns and plant foods to promote health and longevity.
The effects of calorie restriction, intermittent fasting and vegetarian diets on bone health
Abstract
Uncountable health care organizations, clinicians, and individuals are striving to prevent obesity and the many chronic medical conditions linked to it by advocating a healthy lifestyle that includes measures such as reducing dietary calorie intake (i.e., calorie restriction = CR and intermittent fasting = IF) or limiting/abolishing animal source foods (i.e., practices termed vegetarianism and veganism). Although these regimens are traditionally considered healthy, their real impact on bone health has yet to be established, and some studies have reported that they have negative effects on bone outcomes. The current work provides an overview of the studies carried out to examine the effect/s of CR, IF and vegetarian/vegan diets on bone health, and, in particular, on bone mineral density (BMD) and fracture risk. Although data on this subject are limited to small studies and there is no information specifically referring to fractures, CR, but not IF, seems to reduce BMD but does not seem to affect bone quality. Vegetarian diets (particularly vegan ones) are associated with significantly lower BMD values with respect to omnivorous ones and could, potentially, increase the risk of fractures. Given these considerations, individuals who decide to follow these diets should be aware of the risk of osteoporosis and of bone fractures and should introduce dietary sources of calcium and Vitamin D and/or supplementation. Future studies examining fracture/osteoporosis incidence in selected populations will be able expand our knowledge about the safety of these diets and the risks linked to them.
Plant-Based Dietary Patterns, Plant Foods, and Age-Related Cognitive Decline
Abstract
The aging population is expanding, as is the prevalence of age-related cognitive decline (ARCD). Of the several risk factors that predict the onset and progression of ARCD, 2 important modifiable risk factors are diet and physical activity. Dietary patterns that emphasize plant foods can exert neuroprotective effects. In this comprehensive review, we examine studies in humans of plant-based dietary patterns and polyphenol-rich plant foods and their role in either preventing ARCD and/or improving cognitive function. As yet, there is no direct evidence to support the benefits of a vegetarian diet in preventing cognitive decline. However, there is emerging evidence for brain-health-promoting effects of several plant foods rich in polyphenols, anti-inflammatory dietary patterns, and plant-based dietary patterns such as the Mediterranean diet that include a variety of fruits, vegetables, legumes, nuts, and whole grains. The bioactive compounds present in these dietary patterns include antioxidant vitamins, polyphenols, other phytochemicals, and unsaturated fatty acids. In animal models these nutrients and non-nutrients have been shown to enhance neurogenesis, synaptic plasticity, and neuronal survival by reducing oxidative stress and neuroinflammation. In this review, we summarize the mounting evidence in favor of plant-centered dietary patterns, inclusive of polyphenol-rich foods for cognitive well-being. Randomized clinical trials support the role of plant foods (citrus fruits, grapes, berries, cocoa, nuts, green tea, and coffee) in improving specific domains of cognition, most notably frontal executive function. We also identify knowledge gaps and recommend future studies to identify whether plant-exclusive diets have an added cognitive advantage compared with plant-centered diets with fish and/or small amounts of animal foods.
Healthy aging diets other than the Mediterranean: a focus on the Okinawan diet
Abstract
The traditional diet in Okinawa is anchored by root vegetables (principally sweet potatoes), green and yellow vegetables, soybean-based foods, and medicinal plants. Marine foods, lean meats, fruit, medicinal garnishes and spices, tea, alcohol are also moderately consumed. Many characteristics of the traditional Okinawan diet are shared with other healthy dietary patterns, including the traditional Mediterranean diet, DASH diet, and Portfolio diet. All these dietary patterns are associated with reduced risk for cardiovascular disease, among other age-associated diseases. Overall, the important shared features of these healthy dietary patterns include: high intake of unrefined carbohydrates, moderate protein intake with emphasis on vegetables/legumes, fish, and lean meats as sources, and a healthy fat profile (higher in mono/polyunsaturated fats, lower in saturated fat; rich in omega-3). The healthy fat intake is likely one mechanism for reducing inflammation, optimizing cholesterol, and other risk factors. Additionally, the lower caloric density of plant-rich diets results in lower caloric intake with concomitant high intake of phytonutrients and antioxidants. Other shared features include low glycemic load, less inflammation and oxidative stress, and potential modulation of aging-related biological pathways. This may reduce risk for chronic age-associated diseases and promote healthy aging and longevity.
Human gut microbiota and healthy aging: Recent developments and future prospective
Abstract
The human gut microbiota alters with the aging process. In the first 2-3 years of life, the gut microbiota varies extensively in composition and metabolic functions. After this period, the gut microbiota demonstrates adult-like more stable and diverse microbial species. However, at old age, deterioration of physiological functions of the human body enforces the decrement in count of beneficial species (e.g. Bifidobacteria) in the gut microbiota, which promotes various gut-related diseases (e.g. inflammatory bowel disease). Use of plant-based diets and probiotics/prebiotics may elevate the abundance of beneficial species and prevent gut-related diseases. Still, the connections between diet, microbes, and host are only partially known. To this end, genome-scale metabolic modeling can help to explore these connections as well as to expand the understanding of the metabolic capability of each species in the gut microbiota. This systems biology approach can also predict metabolic variations in the gut microbiota during ageing, and hereby help to design more effective probiotics/prebiotics.
Chapter 49 - Prebiotics and Probiotics in Aging Population: Effects on the Immune-Gut Microbiota Axis
Abstract
Nowadays, the strict collaboration between the immune system and
microbiota
is the subject of intensive investigation.
Especially at gut level, the immune cells and microbial components of the microbiota are able to keep each other in equilibrium, thus contributing to human health. Inappropriate dietary regimens seem to account for the subversion of the gut immunity/microbiota axis, thus leading to a regional, as well as a systemic, inflammatory status. In the elderly, both the immune system and microbiota undergo modifications which may account for a condition of inflammaging, thus aggravating the clinical course of age-related disease. In the light of these considerations, experimental and clinical trials have been performed in aged animals and human beings, using prebiotics and probiotics or a combination of the two, the so-called synbiotics. The most of the available data support beneficial effects of these compounds on the recovery of the immune system and normalization of
gut microbiota
in elderly. However, additional work is necessary to identify the most efficient combinations of pre- and probiotics and synbiotics, taking into consideration that variability of human responses is likely attributable to differences in microbiota composition among subjects.
Anti-Aging Effects of Probiotics
Abstract
The body of evidence demonstrating the beneficial effects of probiotics on the skin continues to grow in the published literature. Insights into their effects at the molecular level, in animal models, and in human clinical trials build the case for their role in slowing the skin manifestations of both intrinsic and extrinsic aging. The reports reviewed in this manuscript demonstrate that probiotics can restore acidic skin pH, alleviate oxidative stress, attenuate photoaging, improve skin barrier function, and enhance hair quality.
Reduced vitamin D receptor (VDR) expression and plasma vitamin D levels are associated with aging‐related prostate lesions
AbstractBackground
Protective roles have been proposed for vitamin D in prostate cancer, which has the advanced age as the major risk factor. However, little is known about the expression of the vitamin D receptor (VDR) in the aging prostate and its association with the development of epithelial lesions that affect tissue homeostasis and may precede prostate tumors.
Methods
VDR expression in the prostatic complex of young adults to senile Wistar rats, a natural model to study age‐related prostatic disorders, was evaluated by immunohistochemical, Western blotting, and image‐assisted analyzes. Results were correlated with the plasma levels of vitamin D and testosterone, the occurrence of punctual histopathological changes in the aging prostate, and the expression of retinoid X receptors (RXR).
Results
VDR was widely distributed in the prostatic complex at all ages analyzed, with the highest immunoexpression found in basal epithelial cells. As the animals aged, VDR levels increased, except in punctual areas with intraepithelial proliferation, metaplasia, or proliferative inflammatory atrophy, which had reduced expression of this receptor concomitantly with increased cell proliferation. Interestingly, RXR expression in the aging prostate was similar to that found for its partner VDR, indicating that components of the VDR/RXR complex required for vitamin D signaling are affected in aging‐related prostatic lesions. Moreover, plasma vitamin D levels declined at the same ages when prostatic alterations appeared. Although circulating levels of testosterone also decreased with aging, the changes observed in the components of the vitamin D system were not correlated with androgens.
Conclusions
Our data indicate that the aging prostate suffers from an imbalance on the intricate mechanism of tissue regulation by the vitamin D responsive system. We argue that the status of VDR expression might be determinant for the development of histopathological alterations in the aging prostate, which include premalignant lesions.
Effects of Vitamin D3 Supplementation on Epigenetic Aging in Overweight and Obese African Americans With Suboptimal Vitamin D Status: A Randomized Clinical Trial
Abstract
Background
We have previously shown that vitamin D supplementation increases telomerase activity, suggesting an anti-aging effect. In this study, we aim to test the hypothesis that vitamin D supplementation would slow down epigenetic aging, a new marker of biological aging.
Methods
A randomized clinical trial was previously conducted among 70 overweight/obese African Americans with serum 25-hydroxyvitamin D [25(OH)D] < 50 nmol/L, who were randomly assigned into four groups of 600 IU/d, 2,000 IU/d, 4,000 IU/d of vitamin D3 supplements or placebo followed by 16-week interventions. Whole genome-wide DNA methylation analysis was conducted in 51 participants. DNA methylation ages were calculated according to the Horvath and the Hannum methods. Methylation-based age acceleration index (∆Age) is defined as the difference between DNA methylation age and chronological age in years. Mixed-effects models were used to evaluate the treatment effects.
Results
Fifty-one participants (aged 26.1 ± 9.3 years, 16% are male) were included in the study. After the adjustment of multi-covariates, vitamin D3 supplementation of 4,000 IU/d was associated with 1.85 years decrease in Horvath epigenetic aging compared with placebo (p value = .046), and 2,000 IU/d was associated with 1.90 years decrease in Hannum epigenetic aging (p value = .044). Serum 25(OH)D concentrations were significantly associated with decreased Horvath ∆Age only (p values = .002), regardless of treatments.
Conclusions
Our results suggest that vitamin D supplementation may slow down Horvath epigenetic aging. But the effect on Hannum epigenetic aging is not conclusive. Large-scale and longer duration clinical trials are needed to replicate the findings.
Low Intake of Vitamin E Accelerates Cellular Aging in Patients With Established Cardiovascular Disease: The CORDIOPREV Study
Abstract
Leukocyte telomere length (LTL) shortening is a biomarker of cellular aging that can be decelerated by diet. We aimed to investigate the effect of dietary intake of vitamin E on biomarkers of cellular senescence in patients with established cardiovascular disease. To this end, DNA from 1,002 participants of the CORDIOPREV study (NCT00924937) was isolated and LTL was measured by real-time PCR. Dietary information was collected using a 146-item food frequency questionnaire, and several oxidative stress and damage biomarkers were determined. We found that patients with an inadequate intake of vitamin E according to the European Food Safety Authority, U.S. Food and Nutrition Board, and Spanish dietary recommendation had shorter LTL than those with an adequate intake (p = .004, p = .015, and p = .005, respectively). Moreover, we observed a positive correlation between olive oil, fish consumption and LTL (r2 = .083, p = .010; r2 = .090, p = .006, respectively). Subjects who consumed more than 30 mL olive oil/day had longer LTL than subjects with lower consumption (p = .013). Furthermore, we observed higher glutathione peroxidase activity in subjects consuming less vitamin E (p = .031). Our findings support the importance of an adequate consumption of the antioxidant vitamin E, and the value of the diet as a modulating tool of the senescence process.
Cholesterol and cognitive aging: Between-person and within-person associations in a population-based representative sample not on lipid-lowering medication.
Abstract
Previous studies suggest that cholesterol metabolic dysregulation, characterized by abnormally low or high serum total cholesterol (TC) values, constitutes a risk for pronounced cognitive decline in old age. We tested this prediction using a population-based representative Swedish sample (N = 382), born in 1901–1902, and subsequently assessed on TC and 3 cognitive outcomes (verbal ability, spatial ability, and perceptual-motor-speed) at ages 70, 75, 79, 85, 88, and 90. None of the participants were on lipid-lowering medication, as prescription availability for these medications were not initiated in Sweden until the mid-1990s. We used a 3-level hierarchical model, with cognitive tests nested within time, nested within individuals. Estimates from this model revealed a nonlinear between-person association between TC and cognition, indicating that low, and to some degree high, TC values were associated with poorer cognition. This association was stronger among nondementia-cases (n = 255). Among subsequent dementia cases (n = 127), the data suggested a linear trend, indicating that lower TC values were associated with poorer cognition. TC levels declined over time in the vast majority (96%), and the steepness of this decline was associated with the rate of cognitive decline. This within-person association was particularly strong among incident dementia cases with low TC values. Our findings indicate an optimal range of TC values associated with better cognition in old age and that the within-person association between TC and cognition is related to dementia pathologies. Further, our findings demonstrate the need to separate between-person from within-person associations when evaluating the relation between TC and cognition in old age. (PsycInfo Database Record (c) 2020 APA, all rights reserved)
The association between hydration status and cognitive function among free-living elderly volunteers
Abstract
Background: Ageing is inevitably associated with a progressive cognitive decline. With the rising percentage of the elderly in society, the number of people with dementia and cognitive impairment increases. Water is a vital ingredient that must be included in the diet. The impact of hydration status on cognitive performance has been studied only a little so far.
Aims: The objective of the study was to investigate the relation between the hydration status and the cognitive function.
Methods: The study was conducted among 60 free-living volunteers, aged 60-93 years. Data on water consumption were gathered based on 3-day records. The hydration status was assessed in morning urine samples by evaluating urine specific gravity. The cognitive function was tested using the Mini Mental State Examination (MMSE), the Babcock Story Recall Test and the Trail Making Test. Information about depression was gathered by the Geriatric Depression Scale.
Results: The mean daily total water intake was 2441 ± 622 ml, and 70% of respondents met the reference values for an adequate intake. The mean urine specific gravity (1.013 g/cm3, range of 1.004-1.025 g/cm3) indicated that most of the individuals were in a good hydration state. The average result of MMSE was 27.8, which is connected with mild cognitive impairment. There was no significant relationship between the hydration status and the results of the cognitive function test in the studied population.
Discussion/conclusion: As the elderly volunteers had a good hydration status, there was no significant relationship between cognitive performance and urine specific gravity. It is necessary to replicate the findings of this study with a larger and more diverse sample of older adults.
A Collagen Supplement Improves Skin Hydration, Elasticity, Roughness, and Density: Results of a Randomized, Placebo-Controlled, Blind Study
Abstract
The purpose of this randomized, placebo-controlled, blind study was to investigate the effects of the drinkable nutraceutical ELASTEN® (QUIRIS Healthcare, Gütersloh, Germany) on skin aging and skin health. Drinking ampoules provides a blend of 2.5 g of collagen peptides, acerola fruit extract, vitamin C, zinc, biotin, and a native vitamin E complex. This controlled interventional trial was performed on 72 healthy women aged 35 years or older. They received either the food supplement (n = 36) or a placebo (n = 36) for twelve weeks. A skin assessment was carried out and based on objective validated methods, including corneometry (skin hydration), cutometry (elasticity), the use of silicon skin replicas with optical 3D phase-shift rapid in-vivo measurements (PRIMOS) (roughness), and skin sonography (density). The verum group was followed for an additional four weeks (without intake of the test product) to evaluate the sustainability of the changes induced by the intake of the test product. The test product significantly improved skin hydration, elasticity, roughness, and density. The differences between the verum group and the placebo group were statistically significant for all test parameters. These positive effects were substantially retained during the follow-up. The measured effects were fully consistent with the subjective assessments of the study participants. The nutraceutical was well tolerated.
Caloric restriction: beneficial effects on brain aging and Alzheimer's disease
Abstract
Dietary interventions such as caloric restriction (CR) extend lifespan and health span. Recent data from animal and human studies indicate that CR slows down the aging process, benefits general health, and improves memory performance. Caloric restriction also retards and slows down the progression of different age-related diseases, such as Alzheimer's disease. However, the specific molecular basis of these effects remains unclear. A better understanding of the pathways underlying these effects could pave the way to novel preventive or therapeutic strategies. In this review, we will discuss the mechanisms and effects of CR on aging and Alzheimer's disease. A potential alternative to CR as a lifestyle modification is the use of CR mimetics. These compounds mimic the biochemical and functional effects of CR without the need to reduce energy intake. We discuss the effect of two of the most investigated mimetics, resveratrol and rapamycin, on aging and their potential as Alzheimer's disease therapeutics. However, additional research will be needed to determine the safety, efficacy, and usability of CR and its mimetics before a general recommendation can be proposed to implement them.
Fasting or caloric restriction for healthy aging
Abstract
Aging is associated with a host of biological changes that contribute to a progressive decline in cognitive and physical function, ultimately leading to a loss of independence, and increased risk of mortality. To date, prolonged caloric restriction (i.e., a reduction in caloric intake without malnutrition) is the only non-genetic intervention that has consistently been found to extend both mean and maximal life span across a variety of species. Most individuals have difficulty sustaining prolonged caloric restriction, which has led to a search for alternative approaches that can produce similar to benefits as caloric restriction. A growing body of evidence indicates that fasting periods and intermittent fasting regimens in particular can trigger similar biological pathways as caloric restriction. For this reason, there is increasing scientific interest in further exploring the biological and metabolic effects of intermittent fasting periods, as well as whether long-term compliance may be improved by this type of dietary approach. This special will highlight the latest scientific findings related to the effects of both caloric restriction and intermittent fasting across various species including yeast, fruit flies, worms, rodents, primates, and humans. A specific emphasis is placed on translational research with findings from basic bench to bedside reviewed and practical clinical implications discussed.
Calcium signaling in cognition and aging-dependent cognitive decline
Abstract
Calcium-dependent signals are key triggers of the molecular mechanisms underlying learning and memory and dysregulation of calcium homeostasis in the aging brain has been proposed to underlie aging-dependent cognitive decline. Mechanisms triggered by calcium in neurons include activity-dependent activation of transcription responsible for the synthesis of molecules underlying the long-term changes of neuronal function. Effectors of calcium signaling with a primordial role in transcription regulation are calcium signal-regulated transcription factors. In this review, we summarize the current knowledge of the contribution of key calcium signal-regulated transcription factors, namely CREB, NFAT, and DREAM, to memory formation. We further describe evidence for dysregulation of the activity of these factors during aging.
[Aging and homeostasis. Calcium metabolism and aging]
Abstract
About 99% of total body calcium is present in bone. Therefore, negative calcium balance usually means reduction of bone mass. Negative calcium balance is induced by aging from several mechanisms such as reduced renal production of 1,25-dihydroxyvitamin D[1,25(OH)2D], intestinal resistance to 1,25(OH)2D and increased renal excretion of calcium. However, it is largely unknown how calcium balance is physiologically maintained.
Nutrients for the aging eye
Abstract
The incidence of age-related eye diseases is expected to rise with the aging of the population. Oxidation and inflammation are implicated in the etiology of these diseases. There is evidence that dietary antioxidants and anti-inflammatories may provide benefit in decreasing the risk of age-related eye disease. Nutrients of interest are vitamins C and E, β-carotene, zinc, lutein, zeaxanthin, and the omega-3 fatty acids eicosapentaenoic acid and docosahexaenoic acid. While a recent survey finds that among the baby boomers (45–65 years old), vision is the most important of the five senses, well over half of those surveyed were not aware of the important nutrients that play a key role in eye health. This is evident from a national survey that finds that intake of these key nutrients from dietary sources is below the recommendations or guidelines. Therefore, it is important to educate this population and to create an awareness of the nutrients and foods of particular interest in the prevention of age-related eye disease.
Cancer
The effect of nutrition intervention in lung cancer patients undergoing chemotherapy and/or radiotherapy: a systematic review
Abstract
The prevalence of malnutrition in lung cancer patients across a variety of treatment modalities and disease stages ranges from 45% to 69%. Malnutrition is associated with poorer clinical outcomes in cancer patients. This systematic review examined whether dietary counseling or oral supplements during chemotherapy and/or radiotherapy in patients with lung cancer affect patient or clinical outcomes. Relevant nutrition intervention studies from 1980 to March 2012 were identified. Articles meeting predetermined inclusion/exclusion criteria were critically appraised and included in the review. The outcomes of interest included dietary intake, weight, nutritional status, quality of life, functional status, treatment response, and survival. Five eligible studies were identified including 3 randomized controlled trials, 1 historical cohort, and 1 case series. These studies suggest dietary counseling improves energy and protein intake during chemotherapy in patients with lung cancer but has no benefit to other outcomes during chemotherapy. There is insufficient evidence regarding the effect on patient or clinical outcomes during radiotherapy. Randomized trials examining dietary counseling in patients with lung cancer during radiotherapy are required.
The Role of Nutrition in Cancer Patients
Abstract
In a very simplistic way, the human body has an extremely complex system of cell division that determines the growth of new cells and the death of senescent cells. However, the organism is not perfect and sometimes fails. In the course of the interaction between genetic and environmental factors, including nutritional factors, oncological disease can arise. Of course, no food alone has properties capable of preventing a tumor. In recent years there has been an increase in the number of new cases of cancer. Malnutrition in cancer patients is a consequence of the increase in inflammatory cytokines associated with cancer, metabolic alterations and concomitant inadequate availability of nutrients, due to anorexia caused by the disease and systemic treatments. Malnutrition, combined with loss of muscle mass, is very common in this group of patients and has a negative effect on the prognosis. What to expect from the doctor? It is one of the key questions in this theme.
The Past, Present, and Future of Nutrition and Cancer: Part 1-Was A Nutritional Association Acknowledged a Century Ago?
Abstract
Professional interest in the association of diet and nutrition with cancer first appeared in the early 1800s, if not before. Yet, progress in understanding this association over the past two centuries has been exceedingly slow and confusing. Without addressing this confusion, progress in using diet and nutrition information to prevent and even to treat cancer, will remain uncertain. To better understand this issue, the present paper is the first of two to explore the history of the diet and cancer relationship prior to a 1982 National Academy of Sciences (NAS) report on Diet, Nutrition and Cancer. This report was a milestone in the nutrition and cancer history because it was the first science-based, institutional report on this topic. But, based on the evidence cited in that report, it could be inferred that this topic was relatively new, perhaps beginning around 1940. While it attracted great public interest, it also generated great controversy, some of which was a natural response from affected industries. Exploring the history prior to 1940, therefore, might provide clues on the present-day confusion concerning the relationship between diet and cancer. This investigation asks three questions. First (the subject of this paper), was the relationship of nutrition to cancer even considered prior to 1940 and, if so, what was said? Second (the subject of the upcoming paper), assuming that nutrition was seriously considered, why then was it ignored or forgotten? Third, has the forgotten information contributed to the contemporary confusion surrounding the relationship to cancer? The answer to the first question, considered here, is that, yes, nutrition as a possible cause of cancer was not only hypothesized, it was a major topic for discussion in some quarters. But it also was a topic struggling to be heard among the authorities who had most of the power and influence in the professional cancer community. This paper documents that history and the corresponding struggle for this message to be heard. One figure, Frederick Hoffman, founder of the American Cancer Society and prodigious researcher, led much of that effort during the period of 1913-1943, but his contributions have remained almost totally unknown.
The Impact of Preoperative Immune Modulating Nutrition on Outcomes in Patients Undergoing Surgery for Gastrointestinal Cancer
Abstract
Objective:
To define the influence of preoperative immune modulating nutrition (IMN) on postoperative outcomes in patients undergoing surgery for gastrointestinal cancer.
Background:
Although studies have shown that perioperative IMN may reduce postoperative infectious complications, many of these have included patients with benign and malignant disease, and the optimal timing of such an intervention is not clear.
Methods:
The Embase, Medline, and Cochrane databases were searched from 2000 to 2018, for prospective randomized controlled trials evaluating preoperative oral or enteral IMN in patients undergoing surgery for gastrointestinal cancer. The primary endpoint was the development of postoperative infectious complications. Secondary endpoints included postoperative noninfectious complications, length of stay, and up to 30-day mortality. The analysis was performed using RevMan v5.3 software.
Results:
Sixteen studies reporting on 1387 patients (715 IMN group, 672 control group) were included. Six of the included studies reported on a mixed population of patients undergoing all gastrointestinal cancer surgery. Of the remaining, 4 investigated IMN in colorectal cancer surgery, 2 in pancreatic surgery, and another 2 in patients undergoing surgery for gastric cancer. There was 1 study each on liver and esophageal cancer. The formulation of nutrition used in all studies in the treated patients was Impact (Novartis/Nestlé), which contains ω-3 fatty acids, arginine, and nucleotides. Preoperative IMN in patients undergoing surgery for gastrointestinal cancer reduced infectious complications [odds ratio (OR) 0.52, 95% confidence interval (CI) 0.38–0.71, P < 0.0001, I2 = 16%, n = 1387] and length of hospital stay (weighted mean difference −1.57 days, 95% CI −2.48 to −0.66, P = 0.0007, I2 = 34%, n = 995) when compared with control (isocaloric isonitrogeneous feed or normal diet). It, however, did not affect noninfectious complications (OR 0.98, 95% CI 0.73–1.33, P = 0.91, I2 = 0%, n = 1303) or mortality (OR 0.55, 95% CI 0.18–1.68, P = 0.29, I2 = 0%, n = 955).
Conclusion:
Given the significant impact on infectious complications and a tendency to shorten length of stay, preoperative IMN should be encouraged in routine practice in patients undergoing surgery for gastrointestinal cancer.
Nutrition impact symptoms and associated outcomes in post-chemoradiotherapy head and neck cancer survivors: a systematic review
Purpose
It is estimated that more than 90% of head and neck cancer (HNC) survivors who underwent chemoradiotherapy experience one or more nutrition impact symptoms (NIS) in the months or years thereafter. Despite the high prevalence, there is limited research addressing long-term impact of NIS on outcomes such as nutrition and quality of life in HNC survivors treated with chemoradiotherapy.
Objective
To conduct a systematic review of the literature pertaining to the presence of nutrition impact symptoms and their associated outcomes in post-chemoradiotherapy head and neck cancer survivors.
Evidence review
A systematic review was conducted across three databases according to PRISMA guidelines and used to identify current literature regarding NIS in HNC survivors. A keyword search was conducted in PubMed, Scopus, and Web of Science from 2007 to 2017. Studies that met all of the following criteria were included in the review: (1) studies must include human subjects with a HNC diagnosis; (2) study participants must have received chemoradiotherapy; (3) study participants must have been post-treatment for a minimum of 3 months at the time of data collection; (4) full-text articles must have appeared in peer-reviewed journals; (5) papers must have been published in English; (6) studies must be quantitative in nature; (7) studies must have reported at least one NIS; and (8) studies must address at least one of the following outcomes: nutrition, functional status, or quality of life. Two independent reviewers assessed study quality using a predefined set of criteria.
Findings
A systematic search yielded 1119 papers, of which 15 met the inclusion criteria. The study reviewed existing evidence of NIS in a variety of HNC survivors ranging from 3 months to greater than 10 years post-chemoradiotherapy treatment. Eight hundred forty-nine study participants were included in the review. Of the 15 studies, 10 were designed as prospective cohort studies, 4 were cross-sectional studies, and 1 was a retrospective cohort study. Functional impairments as a result of chemoradiotherapy to the head and neck are prevalent in research and include dysphagia, xerostomia, trismus, salivary issues, mucositis, and oral pain.
Conclusions
NIS negatively influence HNC survivors beyond the acute phase of treatment. These symptoms are associated with decreased nutrition and quality of life. Interventions are necessary to improve survivors’ eating challenges beyond the completion of treatment. If practitioners do not follow patients long term, patients may suffer consequences of NIS including malnutrition risk, weight loss, and decreased food intake and quality of life.
Correlation between Oxidative Stress, Nutrition, and Cancer Initiation
Abstract
Inadequate or excessive nutrient consumption leads to oxidative stress, which may disrupt oxidative homeostasis, activate a cascade of molecular pathways, and alter the metabolic status of various tissues. Several foods and consumption patterns have been associated with various cancers and approximately 30–35% of the cancer cases are correlated with overnutrition or malnutrition. However, several contradictory studies are available regarding the association between diet and cancer risk, which remains to be elucidated. Concurrently, oxidative stress is a crucial factor for cancer progression and therapy. Nutritional oxidative stress may be induced by an imbalance between antioxidant defense and pro-oxidant load due to inadequate or excess nutrient supply. Oxidative stress is a physiological state where high levels of reactive oxygen species (ROS) and free radicals are generated. Several signaling pathways associated with carcinogenesis can additionally control ROS generation and regulate ROS downstream mechanisms, which could have potential implications in anticancer research. Cancer initiation may be modulated by the nutrition-mediated elevation in ROS levels, which can stimulate cancer initiation by triggering DNA mutations, damage, and pro-oncogenic signaling. Therefore, in this review, we have provided an overview of the relationship between nutrition, oxidative stress, and cancer initiation, and evaluated the impact of nutrient-mediated regulation of antioxidant capability against cancer therapy.
The World Cancer Research Fund/American Institute for Cancer Research Third Expert Report on Diet, Nutrition, Physical Activity, and Cancer: Impact and Future Directions
ABSTRACT
The Third Expert Report on Diet, Nutrition, Physical Activity, and Cancer: A Global Perspective by the World Cancer Research Fund (WCRF) and the American Institute for Cancer Research (AICR) represents the most comprehensive, detailed, and objective analysis of the accumulated research in the discipline. The report provides a framework for public health efforts around the globe by governments and other organizations with the goal of significantly reducing the burden of cancer, enhancing health, and improving quality of life for cancer survivors. Coupled with the WCRF/AICR Continuous Update Panel reports on specific cancers, these efforts also provide guidance to healthcare practitioners engaged in counseling individuals who may benefit from diet and lifestyle changes. Most critically, this report defines priorities for future research efforts that will improve the evidence base of future recommendations both for population-based public health efforts and increasingly for more personalized strategies targeting individuals who are cancer survivors or at risk due to genetic predisposition or carcinogenic exposures.
Nutrition and Breast Cancer: A Literature Review on Prevention, Treatment and Recurrence
Abstract
Breast cancer (BC) is the second most common cancer worldwide and the most commonly occurring malignancy in women. There is growing evidence that lifestyle factors, including diet, body weight and physical activity, may be associated with higher BC risk. However, the effect of dietary factors on BC recurrence and mortality is not clearly understood. Here, we provide an overview of the current evidence obtained from the PubMed databases in the last decade, assessing dietary patterns, as well as the consumption of specific food-stuffs/food-nutrients, in relation to BC incidence, recurrence and survival. Data from the published literature suggest that a healthy dietary pattern characterized by high intake of unrefined cereals, vegetables, fruit, nuts and olive oil, and a moderate/low consumption of saturated fatty acids and red meat, might improve overall survival after diagnosis of BC. BC patients undergoing chemotherapy and/or radiotherapy experience a variety of symptoms that worsen patient quality of life. Studies investigating nutritional interventions during BC treatment have shown that nutritional counselling and supplementation with some dietary constituents, such as EPA and/or DHA, might be useful in limiting drug-induced side effects, as well as in enhancing therapeutic efficacy. Therefore, nutritional intervention in BC patients may be considered an integral part of the multimodal therapeutic approach. However, further research utilizing dietary interventions in large clinical trials is required to definitively establish effective interventions in these patients, to improve long-term survival and quality of life
Nutrition, inflammation and cancer
Abstract
Quantitative and qualitative aspects of nutrition have a profound effect on leukocytes and thereby affect proinflammatory carcinogenic effects or anticancer immune responses. As a result, nutrition affects the incidence, natural progression and therapeutic response of malignant diseases, both in humans and in preclinical animal models. Here we discuss the molecular mechanisms through which alimentary cues modulate metabolic, microbial and neuroendocrine circuitries and thus affect the probability of developing premalignant lesions that progress to clinically manifested disease and the response to therapeutic intervention. We examine each of the connections that compose the triangle of nutrition, immunological and inflammatory reactions and cancer while focusing on the mechanistic aspects of these relationships.
Colorectal Cancer and Nutrition
Abstract
Colorectal Cancer is the third most common cancer diagnosed in the US. While the incidence and the mortality rate of colorectal cancer has decreased due to effective cancer screening measures, there has been an increase in number of young patients diagnosed in colon cancer due to unclear reasons at this point of time. While environmental and genetic factors play a major role in the pathogenesis of colon cancer, extensive research has suggested that nutrition may play both a causal and protective role in the development of colon cancer. In this review article, we aim to provide a review of factors that play a major role in development of colorectal cancer.
Whole grain consumption and risk of cardiovascular disease, cancer, and all cause and cause specific mortality: systematic review and dose-response meta-analysis of prospective studies
Abstract
Objective: To quantify the dose-response relation between consumption of whole grain and specific types of grains and the risk of cardiovascular disease, total cancer, and all cause and cause specific mortality.
Data sources: PubMed and Embase searched up to 3 April 2016.
Study selection: Prospective studies reporting adjusted relative risk estimates for the association between intake of whole grains or specific types of grains and cardiovascular disease, total cancer, all cause or cause specific mortality.
Data synthesis: Summary relative risks and 95% confidence intervals calculated with a random effects model.
Results: 45 studies (64 publications) were included. The summary relative risks per 90 g/day increase in whole grain intake (90 g is equivalent to three servings-for example, two slices of bread and one bowl of cereal or one and a half pieces of pita bread made from whole grains) was 0.81 (95% confidence interval 0.75 to 0.87; I(2)=9%, n=7 studies) for coronary heart disease, 0.88 (0.75 to 1.03; I(2)=56%, n=6) for stroke, and 0.78 (0.73 to 0.85; I(2)=40%, n=10) for cardiovascular disease, with similar results when studies were stratified by whether the outcome was incidence or mortality. The relative risks for morality were 0.85 (0.80 to 0.91; I(2)=37%, n=6) for total cancer, 0.83 (0.77 to 0.90; I(2)=83%, n=11) for all causes, 0.78 (0.70 to 0.87; I(2)=0%, n=4) for respiratory disease, 0.49 (0.23 to 1.05; I(2)=85%, n=4) for diabetes, 0.74 (0.56 to 0.96; I(2)=0%, n=3) for infectious diseases, 1.15 (0.66 to 2.02; I(2)=79%, n=2) for diseases of the nervous system disease, and 0.78 (0.75 to 0.82; I(2)=0%, n=5) for all non-cardiovascular, non-cancer causes. Reductions in risk were observed up to an intake of 210-225 g/day (seven to seven and a half servings per day) for most of the outcomes. Intakes of specific types of whole grains including whole grain bread, whole grain breakfast cereals, and added bran, as well as total bread and total breakfast cereals were also associated with reduced risks of cardiovascular disease and/or all cause mortality, but there was little evidence of an association with refined grains, white rice, total rice, or total grains.
Conclusions: This meta-analysis provides further evidence that whole grain intake is associated with a reduced risk of coronary heart disease, cardiovascular disease, and total cancer, and mortality from all causes, respiratory diseases, infectious diseases, diabetes, and all non-cardiovascular, non-cancer causes. These findings support dietary guidelines that recommend increased intake of whole grain to reduce the risk of chronic diseases and premature mortality.
The effect of vitamin E and beta carotene on the incidence of lung cancer and other cancers in male smokers
Abstract
Background: Epidemiologic evidence indicates that diets high in carotenoid-rich fruits and vegetables, as well as high serum levels of vitamin E (alpha-tocopherol) and beta carotene, are associated with a reduced risk of lung cancer.
Methods: We performed a randomized, double-blind, placebo-controlled primary-prevention trial to determine whether daily supplementation with alpha-tocopherol, beta carotene, or both would reduce the incidence of lung cancer and other cancers. A total of 29,133 male smokers 50 to 69 years of age from southwestern Finland were randomly assigned to one of four regimens: alpha-tocopherol (50 mg per day) alone, beta carotene (20 mg per day) alone, both alpha-tocopherol and beta carotene, or placebo. Follow-up continued for five to eight years.
Results: Among the 876 new cases of lung cancer diagnosed during the trial, no reduction in incidence was observed among the men who received alpha-tocopherol (change in incidence as compared with those who did not, -2 percent; 95 percent confidence interval, -14 to 12 percent). Unexpectedly, we observed a higher incidence of lung cancer among the men who received beta carotene than among those who did not (change in incidence, 18 percent; 95 percent confidence interval, 3 to 36 percent). We found no evidence of an interaction between alpha-tocopherol and beta carotene with respect to the incidence of lung cancer. Fewer cases of prostate cancer were diagnosed among those who received alpha-tocopherol than among those who did not. Beta carotene had little or no effect on the incidence of cancer other than lung cancer. Alpha-tocopherol had no apparent effect on total mortality, although more deaths from hemorrhagic stroke were observed among the men who received this supplement than among those who did not. Total mortality was 8 percent higher (95 percent confidence interval, 1 to 16 percent) among the participants who received beta carotene than among those who did not, primarily because there were more deaths from lung cancer and ischemic heart disease.
Conclusions: We found no reduction in the incidence of lung cancer among male smokers after five to eight years of dietary supplementation with alpha-tocopherol or beta carotene. In fact, this trial raises the possibility that these supplements may actually have harmful as well as beneficial effects.
Antioxidant and Anticoagulant Status Were Improved by Personalized Dietary Intervention Based on Biochemical and Clinical Parameters in Cancer Patients
Abstract
We investigated whether personalized dietary intervention could improve clinical measurements such as immune cell-mediated cytotoxicity, serum albumin, derivatives of reactive oxygen metabolites (D-ROMS), D-dimer, and fibrinogen. Cancer patients received either a treatment support diet (TD, for those with chemotherapy), or a remission support diet (RD; for those in remission) for at least 3 wk (21-61 days). Both diets were low glycemic, low fat, and high plant protein diets; the diet for the TD group contained an additional 0.5 servings of protein. Based on clinical values, additional amounts of garlic, onion, tomato, shiitake, rice bran, kale, blueberry, pineapples, and/or turmeric powder were provided in regular meals. Estimated daily intake of protein, plant fat, garlic, onion, allicin, and quercetin was greater in the TD compared to the RD. An increased intake of vitamin A, vitamin C, vitamin E and selenium and a reduction in D-dimer were noted compared to baseline diets in both groups. A decrease in D-ROMS in the RD and an increase in albumin and an increased tendency in cytotoxicity in the TD were observed. In conclusion, personalized diets with supplemented functional ingredients improved antioxidant status and/or anticoagulant activity in cancer patients undergoing chemotherapy and in remission.
Differences in Fecal Gut Microbiota, Short-Chain Fatty Acids and Bile Acids Link Colorectal Cancer Risk to Dietary Changes Associated with Urbanization Among Zimbabweans
Abstract
The incidence of colorectal cancer (CRC) is gradually rising in sub-Saharan Africa. This may be due to dietary changes associated with urbanization, which may induce tumor-promoting gut microbiota composition and function. We compared fecal microbiota composition and activity in 10 rural and 10 urban Zimbabweans for evidence of a differential CRC risk. Dietary intake was assessed by a food frequency questionnaire. Fecal microbiota composition, metabolomic profile, functional microbial genes were analyzed, and bile acids and short chain fatty acids quantified. Animal protein intake was higher among urban volunteers, but carbohydrate and fiber intake were similar. Bacteria related to Blautia obeum, Streptococcus bovis, and Subdoligranulum variabile were higher in urban residents, whereas bacteria related to Oscillospira guillermondii and Sporobacter termitidis were higher in rural volunteers. Fecal levels of primary bile acids, cholic acid, and chenodeoxycholic acid (P < 0.05), and secondary bile acids, deoxycholic acid (P < 0.05) and ursodeoxycholic acid (P < 0.001) were higher in urban residents. Fecal levels of acetate and propionate, but not butyrate, were higher in urban residents. The gut microbiota composition and activity among rural and urban Zimbabweans retain significant homogeneity (possibly due to retention of dietary fiber), but urban residents have subtle changes, which may indicate a higher CRC risk.
Randomized Study of the Effect of Dietary Counseling During Adjuvant Chemotherapy on Chemotherapy Induced Nausea and Vomiting, and Quality of Life in Patients With Breast Cancer
Abstract
Patients with breast cancer (PsBC) usually face with chemotherapy induced nausea and vomiting (CINV). The aim of this study was to assess the impact of nutritional counseling on CINV and quality of life (QoL) of PsBC. 150 PsBC were randomly assigned for receiving a personalized diet, which contained 1.2-1.5 g/kg of protein, 30% of energy from fat and 55-60% of energy from carbohydrate, a face to face nutrition education, and a pamphlet which contained beneficial nutrition information to reduce the severity of CINV before each chemotherapy session for three times (n = 75) or regular care (n = 75). CINV, QoL, and dietary intake were evaluated after each chemotherapy session. Nausea rating index, overall nausea index, and visual analog scale (P < 0.001) were dramatically lower in the intervention group. Global health status/QoL as well as physical functioning, role functioning, emotional functioning, and cognitive functioning (P < 0.001) were significantly better in the intervention group. Patients in the control group experienced more fatigue, nausea and vomiting, pain, dyspnea, loss of appetite, constipation, and diarrhea (P < 0.001). Nutrition counseling during adjuvant chemotherapy among PsBC reduced the occurrence of CINV and led to significant improvements in the QoL.
Omega-3 Polyunsaturated Fatty Acids and Lung Cancer: nutrition or Pharmacology?
Abstract
Omega-3 polyunsaturated fatty acid (ω-3 PUFA) supplements for chemoprevention of different types of cancer including lung cancer has been investigated in recent years. ω-3 PUFAs are considered immunonutrients, commonly used in the nutritional therapy of cancer patients. ω-3 PUFAs play essential roles in cell signaling and in cell structure and fluidity of membranes. They participate in the resolution of inflammation and have anti-inflammatory effects. Lung cancer patients suffer complications, such as anorexia-cachexia syndrome, pain and depression. The European Society for Clinical Nutrition and Metabolism (ESPEN) 2017 guidelines for cancer patients only discuss the use of ω-3 PUFAs for cancer-cachexia treatment, leaving aside other cancer-related complications that could potentially be managed by ω-3 PUFAs. This review aims to elucidate whether the effects of ω-3 PUFAs in lung cancer is supplementary, pharmacological or both. In addition, clinical studies, evidence in cell lines and animal models suggest how ω-3 PUFAs induce anticancer effects. ω-3 PUFAs and their metabolites are suggested to modulate pivotal pathways underlying the progression or complications of lung cancer, indicating that this is a promising field to be explored. Further investigation is still required to analyze the benefits of ω-3 PUFAs as supplementation or pharmacological treatment in lung cancer.
Onion and Garlic Intake and Breast Cancer, a Case-Control Study in Puerto Rico
Abstract
Studies show an inverse association between onion and garlic intake and risk of cancers of the lung, prostate, and stomach. There is limited evidence on the association between onion and garlic intake and breast cancer. We assessed this association in a population-based, case-control study in Puerto Rico. Incident, primary breast cancer cases (n = 314) were identified among women aged 30-79 from hospital and clinic records. Controls (n = 346) were women with no history of cancer other than nonmelanoma skin cancer, residents of the same area. Dietary intake was estimated using a food frequency questionnaire. Total onion and garlic intake included sofrito (a popular garlic- and onion-based condiment) intake frequency. Unconditional logistic regression assessed the association between onion and garlic consumption and breast cancer adjusting for age, education, parity, family history, body mass index, age at menarche, total energy, and smoking. Inverse associations with breast cancer were observed for moderate (OR (odds ratio) = 0.59, 95% CI (confidence interval): 0.35, 1.01) and high consumption (OR = 0.51, 95% CI: 0.30, 0.87) compared to low consumption of onion and garlic (Ptrend = 0.02). Results were similar when stratified by menopausal status. Study results suggest that high onion and garlic consumption is protective against breast cancer in this population.
A Randomized Controlled Trial to Increase Navy Bean or Rice Bran Consumption in Colorectal Cancer Survivors
Abstract
Consumption of navy beans (NB) and rice bran (RB) have been shown to inhibit colon carcinogenesis. Given the overall poor diet quality in colorectal cancer (CRC) survivors and low reported intake of whole grains and legumes, practical strategies to increase consumption merit attention. This study determined feasibility of increasing NB or RB intake in CRC survivors to increase dietary fiber and examined serum inflammatory biomarkers and telomere lengths. Twenty-nine subjects completed a randomized controlled trial with foods that included cooked NB powder (35 g/day), heat-stabilized RB (30 g/day), or no additional ingredient. Fasting blood, food logs, and gastrointestinal health questionnaires were collected. The amount of NB or RB consumed equated to 4-9% of subjects' daily caloric intake and no major gastrointestinal issues were reported with increased consumption. Dietary fiber amounts increased in NB and RB groups at Weeks 2 and 4 compared to baseline and to control (P ≤ 0.01). Telomere length correlated with age and HDL cholesterol at baseline, and with improved serum amyloid A (SAA) levels at Week 4 (P ≤ 0.05). This study concludes feasibility of increased dietary NB and RB consumption to levels associated with CRC chemoprevention and warrants longer-term investigations with both foods in high-risk populations that include cancer prevention and control outcomes.
The Effect of Evidence-Based Nutrition Clinical Care Pathways on Nutrition Outcomes in Adult Patients Receiving Non-Surgical Cancer Treatment: A Systematic Review
Abstract
Nutritional decline associated with non-surgical cancer treatment has been well documented. The implementation of an evidence-based nutrition care pathway is one approach suggested to improve the nutrition outcomes of this group of patients. We aimed to systematically review published original research to determine whether evidence-based nutrition clinical care pathways, as compared with usual care, improve outcomes for patients receiving non-surgical cancer treatment. The review was registered with PROSPERO (CRD42017048816) and followed PRISMA guidelines. The search strategy was conducted in four databases, and supplemented by an internet search, from inception to October 2016. Study quality was assessed using the Quality Criteria Checklist for Primary Research. Results were synthesized descriptively. Six reports of five studies formed the final library with a range of interventions and control practices investigated across several diagnostic groups. Nutrition outcomes were reported using multiple approaches with either no effect, or in favor of the clinical pathway intervention. Risk of bias was low in two studies with some risk in the remaining three studies. It was not possible to determine whether the effect on nutritional outcomes was attributable to care pathway implementation. The need to extend the evidence base through high-quality clinical trials was evident.
Epigenetics: a new link between nutrition and cancer
Abstract
Emerging studies suggest that dietary components can affect gene expression through epigenetic mechanisms. Epigenetic modifications are heritable and potentially reversible changes in gene expression that do not require changes in the DNA sequence. The main mechanisms of epigenetic control in mammals are DNA methylation, histone modifications, and RNA silencing. The potential reversibility of epigenetic changes suggests that they could be modulated by nutrition and bioactive food compounds. Thus, epigenetic modifications could mediate environmental signals and provide a link between susceptibility genes and environmental factors in the etiology of cancer. Elucidating the impact of nutrition on epigenetic mechanisms may serve as a tool to predict an individuals' susceptibility to cancer, provide dietary recommendations, or provide therapeutic applications of natural compounds against cancer. The optimal duration and the dose necessary for a chemopreventive effect require further studies. There is limited information about tissue specificity and temporal aspects of dietary treatments. Species differences need to be considered when interpreting results from various models. Importantly, molecular mechanisms of bioactive dietary components should be investigated in greater detail in human intervention studies. Although some of these issues remain controversial, this review mainly focuses on promising data that support the developing field of Nutritional Epigenetics.
Similar articles
Healthy living is the best revenge: findings from the European Prospective Investigation Into Cancer and Nutrition-Potsdam study
Abstract
Background: Our objective was to describe the reduction in relative risk of developing major chronic diseases such as cardiovascular disease, diabetes, and cancer associated with 4 healthy lifestyle factors among German adults.
Methods: We used data from 23,153 German participants aged 35 to 65 years from the European Prospective Investigation Into Cancer and Nutrition-Potsdam study. End points included confirmed incident type 2 diabetes mellitus, myocardial infarction, stroke, and cancer. The 4 factors were never smoking, having a body mass index lower than 30 (calculated as weight in kilograms divided by height in meters squared), performing 3.5 h/wk or more of physical activity, and adhering to healthy dietary principles (high intake of fruits, vegetables, and whole-grain bread and low meat consumption). The 4 factors (healthy, 1 point; unhealthy, 0 points) were summed to form an index that ranged from 0 to 4.
Results: During a mean follow-up of 7.8 years, 2006 participants developed new-onset diabetes (3.7%), myocardial infarction (0.9%), stroke (0.8%), or cancer (3.8%). Fewer than 4% of participants had zero healthy factors, most had 1 to 3 healthy factors, and approximately 9% had 4 factors. After adjusting for age, sex, educational status, and occupational status, the hazard ratio for developing a chronic disease decreased progressively as the number of healthy factors increased. Participants with all 4 factors at baseline had a 78% (95% confidence interval [CI], 72% to 83%) lower risk of developing a chronic disease (diabetes, 93% [95% CI, 88% to 95%]; myocardial infarction, 81% [95% CI, 47% to 93%]; stroke, 50% [95% CI, -18% to 79%]; and cancer, 36% [95% CI, 5% to 57%]) than participants without a healthy factor.
Conclusion: Adhering to 4 simple healthy lifestyle factors can have a strong impact on the prevention of chronic diseases.
Vegetarian, vegan diets and multiple health outcomes: A systematic review with meta-analysis of observational studies
Abstract
Background: Beneficial effects of vegetarian and vegan diets on health outcomes have been supposed in previous studies.
Objectives: Aim of this study was to clarify the association between vegetarian, vegan diets, risk factors for chronic diseases, risk of all-cause mortality, incidence, and mortality from cardio-cerebrovascular diseases, total cancer and specific type of cancer (colorectal, breast, prostate and lung), through meta-analysis.
Methods: A comprehensive search of Medline, EMBASE, Scopus, The Cochrane Library, and Google Scholar was conducted.
Results: Eighty-six cross-sectional and 10 cohort prospective studies were included. The overall analysis among cross-sectional studies reported significant reduced levels of body mass index, total cholesterol, LDL-cholesterol, and glucose levels in vegetarians and vegans versus omnivores. With regard to prospective cohort studies, the analysis showed a significant reduced risk of incidence and/or mortality from ischemic heart disease (RR 0.75; 95% CI, 0.68 to 0.82) and incidence of total cancer (RR 0.92; 95% CI 0.87 to 0.98) but not of total cardiovascular and cerebrovascular diseases, all-cause mortality and mortality from cancer. No significant association was evidenced when specific types of cancer were analyzed. The analysis conducted among vegans reported significant association with the risk of incidence from total cancer (RR 0.85; 95% CI, 0.75 to 0.95), despite obtained only in a limited number of studies.
Conclusions: This comprehensive meta-analysis reports a significant protective effect of a vegetarian diet versus the incidence and/or mortality from ischemic heart disease (-25%) and incidence from total cancer (-8%). Vegan diet conferred a significant reduced risk (-15%) of incidence from total cancer.
Keywords: Vegetarian; diet; meta-analysis; vegan.
Low Protein Intake Is Associated with a Major Reduction in IGF-1, Cancer, and Overall Mortality in the 65 and Younger but Not Older Population
Summary
Mice and humans with growth hormone receptor/IGF-1 deficiencies display major reductions in age-related diseases. Because protein restriction reduces GHR-IGF-1 activity, we examined links between protein intake and mortality. Respondents aged 50–65 reporting high protein intake had a 75% increase in overall mortality and a 4-fold increase in cancer death risk during the following 18 years. These associations were either abolished or attenuated if the proteins were plant derived. Conversely, high protein intake was associated with reduced cancer and overall mortality in respondents over 65, but a 5-fold increase in diabetes mortality across all ages. Mouse studies confirmed the effect of high protein intake and GHR-IGF-1 signaling on the incidence and progression of breast and melanoma tumors, but also the detrimental effects of a low protein diet in the very old. These results suggest that low protein intake during middle age followed by moderate to high protein consumption in old adults may optimize healthspan and longevity.
Dietary Fiber Intake in Young Adults and Breast Cancer Risk
Abstract
OBJECTIVE: We evaluated fiber intake during adolescence and early adulthood in relation to breast cancer (BC) risk in the Nurses’ Health Study II.
METHODS: Among 90 534 premenopausal women who completed a dietary questionnaire in 1991, we documented 2833 invasive BC cases during 20 years of follow-up. In 1998, 44 263 of these women also completed a questionnaire about their diet during high school; among these women, we documented 1118 cases of BC by end of follow-up. Multivariable-adjusted Cox proportional hazards regression was used to model relative risks (RRs) and 95% confidence intervals (CIs) for BC across categories of dietary fiber.
RESULTS: Among all women, early adulthood total dietary fiber intake was associated with significantly lower BC risk (RR for highest versus lowest quintile 0.81; 95% CI 0.72–0.91; Ptrend = .002). Higher intakes of soluble fiber (RR for highest versus lowest quintile 0.86; 95% CI 0.77–0.97; Ptrend = .02) and insoluble fiber (RR for highest versus lowest quintile 0.80; 95% CI 0.71–0.90; Ptrend < .001) were each associated with lower BC risk. Total dietary fiber intake in adolescence was also associated with lower BC risk (RR for highest versus lowest quintile 0.84; 95% CI 0.70–1.01; Ptrend = .04). For the average of fiber intake during adolescence and early adult life, the RR comparing highest with lowest quintiles was 0.75 (95% CI 0.62–0.91, Ptrend = .004).
CONCLUSIONS: Our findings support the hypothesis that higher fiber intakes reduce BC risk and suggest that intake during adolescence and early adulthood may be particularly important.
Increased Fiber Intake Decreases Premenopausal Breast Cancer Risk
There is growing interest in the relationship between dietary habits and cancer. Dietary fibers are a complex group of oligosaccharides, polysaccharides, resistant starch, and resistant dextrins. There is longstanding evidence that dietary fibers may reduce circulating estrogen levels through changes in the gut microbiome and increased excretion of estrogens in the gastrointestinal tract. Soluble fibers are believed to decrease intestinal cholesterol absorption, and there is emerging evidence that cholesterol byproducts may have estrogenic effects.
1
Fiber intake would be an easily modifiable risk factor to reduce the development of breast cancer.
Until recently, there have been no studies showing a clear relationship between dietary fiber and breast cancer risk. In addition, there has been no significant evaluation of the short- and long-term impact of fiber intake during breast development in the adolescent years. However, in recent months, several new studies have suggested a protective effect of fiber in the risk of breast cancer.
2
–
4
Farvid et al
5
evaluated >44 000 women in the ongoing NHSII (Nurse’s Health Study II) prospective cohort study and found that increasing adolescent and early adulthood fiber intake was associated with significantly lower risk of invasive breast cancer. The women reporting the highest quintile of fiber intake had an impressively lower risk of breast cancer compared with the lowest quintile (relative risk, 0.75), and this finding was stronger in premenopausal breast cancer (relative risk, 0.68). However, the women were surveyed about their adolescent diet when they were in their 30s and 40s. Although the investigators discuss the validation of the dietary survey, the recollection of dietary habits more than a decade earlier must be questioned. They used rigorous methodology to attempt to control for confounding factors, and although there may be confounding dietary or lifestyle factors also contributing to these findings, the associations are interesting and deserve further study. In particular, the association between dietary fiber and weight must be examined prospectively to understand the clinical impact of the authors’ findings. It is reasonable for pediatricians to encourage a high-fiber diet and include decreasing breast cancer risk as one of the potential benefits.
VEGETARIAN DIETS AND THE INCIDENCE OF CANCER IN A LOW-RISK POPULATION
Abstract
Background
Cancer is the second leading cause of death in the US. Dietary factors account for at least 30% of all cancers in Western countries. Since people do not consume individual foods but rather combinations of them, the assessment of dietary patterns may offer valuable information when determining associations between diet and cancer risk.
Methods
We examined the association between dietary patterns (non-vegetarians, lacto, pesco, vegan, and semi-vegetarian) and the overall cancer incidence among 69,120 participants of the Adventist Health Study-2. Cancer cases were identified by matching to cancer registries. Cox-proportional hazard regression analysis was performed to estimate hazard ratios, with “attained age” as the time variable.
Results
2,939 incident cancer cases were identified. The multivariate HR of overall cancer risk among vegetarians compared to non-vegetarians was statistically significant (HR=0.92; 95%CI: 0.85, 0.99) for both genders combined. Also, a statistically significant association was found between vegetarian diet and cancers of the gastrointestinal tract (HR=0.76; 95%CI: 0.63, 0.90). When analyzing the association of specific vegetarian dietary patterns, vegan diets showed statistically significant protection for overall cancer incidence (HR=0.84; 95%CI: 0.72, 0.99) in both genders combined and for female-specific cancers (HR=0.66; 95%CI: 0.47, 0.92). Lacto-ovo-vegetarians appeared to be associated with decreased risk of cancers of the gastrointestinal system (HR=0.75; 95%CI: 0.60, 0.92).
Conclusion
Vegetarian diets seem to confer protection against cancer.
Impact
Vegan diet seems to confer lower risk for overall and female-specific cancer compared to other dietary patterns. The lacto-ovo-vegetarian diets seem to confer protection from cancers of the gastrointestinal tract.
Keywords: cancer, vegetarian dietary patterns, diet, vegan, lacto-ovo-vegetarians
Lifestyle, nutrition and breast cancer: facts and presumptions for consideration
Abstract
Breast cancer is the most common cancer in women worldwide, and the high incidence of this cancer coupled with improvements in initial treatments has led to an ever-increasing number of breast cancer survivors. Among the prospective epidemiological studies on diet and breast cancer incidence and recurrence, to date, there is no association that is strong, reproducible and statistically significant, with the exception of alcohol intake, overweight, and weight gain. Nevertheless, many beliefs about food and breast cancer persist in the absence of supporting scientific evidence.
After a comprehensive review regarding the role of lifestyle on breast cancer outcomes and a thorough study of the dissemination field including mass media, clinical institutions, and academic figures, we briefly reported the most common presumptions and also facts from the literature regarding lifestyle, nutrition, and breast cancer.
The randomised controlled trial is the best study-design that could provide direct evidence of a causal relationship; however, there are methodological difficulties in applying and maintaining a lifestyle intervention for a sufficient period; consequently, there is a lack of this type of study in the literature. Instead, it is possible to obtain indirect evidence from observational prospective studies. In this article, it becomes clear that for now the best advice for women’s health is to follow the World Cancer Research Fund/American Institute of Cancer Research (WCRF/AICR) recommendations on diet, nutrition, physical activity, and weight management for cancer prevention, because they are associated with a lower risk of developing most types of cancer, including breast cancer. Despite current awareness of the role of nutrition in cancer outcomes, there is inadequate translation from research findings into clinical practice. We suggest the establishment of a multidisciplinary research consortium to demonstrate the real power of lifestyle interventions.
Keywords: breast cancer, lifestyle, nutrition, cancer prevention, body weight
High- and Low-Fat Dairy Intake, Recurrence, and Mortality After Breast Cancer Diagnosis
Abstract
Background
Dietary fat in dairy is a source of estrogenic hormones and may be related to worse breast cancer survival. We evaluated associations between high- and low-fat dairy intake, recurrence, and mortality after breast cancer diagnosis.
Methods
We included 1893 women from the Life After Cancer Epidemiology study diagnosed with early-stage invasive breast cancer from 1997 to 2000, who completed the Fred Hutchinson Cancer Research Center Food Frequency Questionnaire after diagnosis. A total of 349 women had a recurrence and 372 died during a median follow-up of 11.8 years, with 189 deaths from breast cancer. We used delayed entry Cox proportional hazards regression to evaluate associations between categories of the cumulative average of dairy fat at baseline and at follow-up 5 to 6 years later and subsequent outcomes. Tests of statistical significance were two-sided.
Results
In multivariable-adjusted analyses, overall dairy intake was unrelated to breast cancer–specific outcomes, although it was positively related to overall mortality. Low-fat dairy intake was unrelated to recurrence or survival. However, high-fat dairy intake was positively associated with outcomes. Compared with the reference (0 to <0.5 servings/day), those consuming larger amounts of high-fat dairy had higher breast cancer mortality (0.5 to <1.0 servings/day: hazard ratio [HR] = 1.20, 95% confidence interval [CI] = 0.82 to 1.77; and ≥1.0 servings/day: HR = 1.49, 95% CI = 1.00 to 2.24, P trend = .05), higher all-cause mortality (P trend < .001), and higher non–breast cancer mortality (P trend = .007); the relationship with breast cancer recurrence was positive but not statistically significant. The higher risk appeared consistent across different types of high-fat dairy products.
Conclusions
Intake of high-fat dairy, but not low-fat dairy, was related to a higher risk of mortality after breast cancer diagnosis.
Dietary and Policy Priorities for Cardiovascular Disease, Diabetes, and Obesity – A Comprehensive Review
Abstract
Suboptimal nutrition is a leading cause of poor health. Nutrition and policy science have advanced rapidly, creating confusion yet also providing powerful opportunities to reduce the adverse health and economic impacts of poor diets. This review considers the history, new evidence, controversies, and corresponding lessons for modern dietary and policy priorities for cardiovascular diseases, obesity, and diabetes. Major identified themes include the importance of evaluating the full diversity of diet-related risk pathways, not just obesity and blood lipids; focusing on foods and overall diet patterns, rather than single isolated nutrients; recognizing the complex influences of different foods on long-term weight regulation, rather than simply counting calories; and characterizing and implementing evidence-based strategies, including policy approaches, for lifestyle change. Evidence-informed dietary priorities include increased fruits, nonstarchy vegetables, nuts, legumes, fish, vegetable oils, yogurt, and minimally processed whole grains; and fewer red meats, processed (e.g., sodium-preserved) meats, and foods rich in refined grains, starch, added sugars, salt, and trans fat. More investigation is needed on cardiometabolic effects of phenolics, dairy fat, probiotics, fermentation, coffee, tea, cocoa, eggs, specific vegetable and tropical oils, vitamin D, individual fatty acids, and diet-microbiome interactions. Little evidence to-date supports cardiometabolic relevance of other popular priorities: e.g., local, organic, grass-fed, farmed/wild, non-GMO. Evidence-based personalized nutrition appears to depend more on non-genetic characteristics (e.g., physical activity, abdominal adiposity, gender, socioeconomic status, culture) than genetic factors. Food choices must be strongly supported by clinical behavior change efforts, health systems reforms, novel technologies, and robust policy strategies, including those targeting economic incentives, schools and workplaces, neighborhood environments, and the food system. Scientific advances provide crucial new insights on optimal targets and best practices to reduce burdens of diet-related cardiometabolic diseases.
Keywords: diet, nutrition, cardiovascular disease, obesity, diabetes, behavior change, health systems, policy, review
Changes in prostate gene expression in men undergoing an intensive nutrition and lifestyle intervention
ABSTRACT
Epidemiological and prospective studies indicate that comprehensive lifestyle changes may modify the progression of prostate cancer. However, the molecular mechanisms by which improvements in diet and lifestyle might affect the prostate microenvironment are poorly understood. We conducted a pilot study to examine changes in prostate gene expression in a unique population of men with low-risk prostate cancer who declined immediate surgery, hormonal therapy, or radiation and participated in an intensive nutrition and lifestyle intervention while undergoing careful surveillance for tumor progression. Consistent with previous studies, significant improvements in weight, abdominal obesity, blood pressure, and lipid profile were observed (all P < 0.05), and surveillance of low-risk patients was safe. Gene expression profiles were obtained from 30 participants, pairing RNA samples from control prostate needle biopsy taken before intervention to RNA from the same patient's 3-month postintervention biopsy. Quantitative real-time PCR was used to validate array observations for selected transcripts. Two-class paired analysis of global gene expression using significance analysis of microarrays detected 48 up-regulated and 453 down-regulated transcripts after the intervention. Pathway analysis identified significant modulation of biological processes that have critical roles in tumorigenesis, including protein metabolism and modification, intracellular protein traffic, and protein phosphorylation (all P < 0.05). Intensive nutrition and lifestyle changes may modulate gene expression in the prostate. Understanding the prostate molecular response to comprehensive lifestyle changes may strengthen efforts to develop effective prevention and treatment. Larger clinical trials are warranted to confirm the results of this pilot study.
Keywords: exercise, lifestyle changes, prostate cancer, SHOC2, stress management
Fasting-mimicking diet and markers/risk factors for aging, diabetes, cancer, and cardiovascular disease
Abstract
Calorie restriction or changes in dietary composition can enhance healthy aging, but the inability of most subjects to adhere to chronic and extreme diets, as well as potentially adverse effects, limits their application. We randomized 100 generally healthy participants from the United States into two study arms and tested the effects of a fasting-mimicking diet (FMD)—low in calories, sugars, and protein but high in unsaturated fats—on markers/risk factors associated with aging and age-related diseases. We compared subjects who followed 3 months of an unrestricted diet to subjects who consumed the FMD for 5 consecutive days per month for 3 months. Three FMD cycles reduced body weight, trunk, and total body fat; lowered blood pressure; and decreased insulin-like growth factor 1 (IGF-1). No serious adverse effects were reported. After 3 months, control diet subjects were crossed over to the FMD program, resulting in a total of 71 subjects completing three FMD cycles. A post hoc analysis of subjects from both FMD arms showed that body mass index, blood pressure, fasting glucose, IGF-1, triglycerides, total and low-density lipoprotein cholesterol, and C-reactive protein were more beneficially affected in participants at risk for disease than in subjects who were not at risk. Thus, cycles of a 5-day FMD are safe, feasible, and effective in reducing markers/risk factors for aging and age-related diseases. Larger studies in patients with diagnosed diseases or selected on the basis of risk factors are warranted to confirm the effect of the FMD on disease prevention and treatment.
General Lifestyle Management
Before the beginning: nutrition and lifestyle in the preconception period and its importance for future health
Abstract
A woman who is healthy at the time of conception is more likely to have a successful pregnancy and a healthy child. We reviewed published evidence and present new data from low-income, middle-income, and high-income countries on the timing and importance of preconception health for subsequent maternal and child health. We describe the extent to which pregnancy is planned, and whether planning is linked to preconception health behaviours. Observational studies show strong links between health before pregnancy and maternal and child health outcomes, with consequences that can extend across generations, but awareness of these links is not widespread. Poor nutrition and obesity are rife among women of reproductive age, and differences between high-income and low-income countries have become less distinct, with typical diets falling far short of nutritional recommendations in both settings and especially among adolescents. Several studies show that micronutrient supplementation starting in pregnancy can correct important maternal nutrient deficiencies, but effects on child health outcomes are disappointing. Other interventions to improve diet during pregnancy have had little effect on maternal and newborn health outcomes. Comparatively few interventions have been made for preconception diet and lifestyle. Improvements in the measurement of pregnancy planning have quantified the degree of pregnancy planning and suggest that it is more common than previously recognised. Planning for pregnancy is associated with a mixed pattern of health behaviours before conception. We propose novel definitions of the preconception period relating to embryo development and actions at individual or population level. A sharper focus on intervention before conception is needed to improve maternal and child health and reduce the growing burden of non-communicable diseases. Alongside continued efforts to reduce smoking, alcohol consumption, and obesity in the population, we call for heightened awareness of preconception health, particularly regarding diet and nutrition. Importantly, health professionals should be alerted to ways of identifying women who are planning a pregnancy.
Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women: the HALE project
Abstract
Context: Dietary patterns and lifestyle factors are associated with mortality from all causes, coronary heart disease, cardiovascular diseases, and cancer, but few studies have investigated these factors in combination.
Objective: To investigate the single and combined effect of Mediterranean diet, being physically active, moderate alcohol use, and nonsmoking on all-cause and cause-specific mortality in European elderly individuals.
Design, setting, and participants: The Healthy Ageing: a Longitudinal study in Europe (HALE) population, comprising individuals enrolled in the Survey in Europe on Nutrition and the Elderly: a Concerned Action (SENECA) and the Finland, Italy, the Netherlands, Elderly (FINE) studies, includes 1507 apparently healthy men and 832 women, aged 70 to 90 years in 11 European countries. This cohort study was conducted between 1988 and 2000.
Main outcome measures: Ten-year mortality from all causes, coronary heart disease, cardiovascular diseases, and cancer.
Results: During follow-up, 935 participants died: 371 from cardiovascular diseases, 233 from cancer, and 145 from other causes; for 186, the cause of death was unknown. Adhering to a Mediterranean diet (hazard ratio [HR], 0.77; 95% confidence interval [CI], 0.68-0.88), moderate alcohol use (HR, 0.78; 95% CI, 0.67-0.91), physical activity (HR, 0.63; 95% CI, 0.55-0.72), and nonsmoking (HR, 0.65; 95% CI, 0.57-0.75) were associated with a lower risk of all-cause mortality (HRs controlled for age, sex, years of education, body mass index, study, and other factors). Similar results were observed for mortality from coronary heart disease, cardiovascular diseases, and cancer. The combination of 4 low risk factors lowered the all-cause mortality rate to 0.35 (95% CI, 0.28-0.44). In total, lack of adherence to this low-risk pattern was associated with a population attributable risk of 60% of all deaths, 64% of deaths from coronary heart disease, 61% from cardiovascular diseases, and 60% from cancer.
Conclusion: Among individuals aged 70 to 90 years, adherence to a Mediterranean diet and healthful lifestyle is associated with a more than 50% lower rate of all-causes and cause-specific mortality.
Association of Iron Deficiency Anemia With Hearing Loss in US Adults
Abstract
Importance Hearing loss in the US adult population is linked to hospitalization, poorer self-reported health, hypertension, diabetes, and tobacco use. Because iron deficiency anemia (IDA) is a common and easily correctable condition, further understanding of the association between IDA and all types of hearing loss in a population of US adults may help to open new possibilities for early identification and appropriate treatment.
Objective To evaluate the association between sensorineural hearing loss (SNHL) and conductive hearing loss and IDA in adults aged 21 to 90 years in the United States.
Design, Setting, and Participants The prevalence of IDA and hearing loss (International Classification of Diseases, Ninth Revision codes 389.1 [SNHL], 389.0 [conductive hearing loss], and 389 [combined hearing loss]) was identified in this retrospective cohort study at the Penn State Milton S. Hershey Medical Center, Hershey, Pennsylvania. Iron deficiency anemia was determined by low hemoglobin and ferritin levels for age and sex in 305 339 adults aged 21 to 90 years. Associations between hearing loss and IDA were evaluated using χ2 testing, and logistic regression was used to model the risk of hearing loss among those with IDA. The study was conducted from January 1, 2011, to October 1, 2015.
Main Outcomes and Measures Hearing loss.
Results Of 305 339 patients in the study population, 132 551 were men (43.4%); mean (SD) age was 50.1 (18.5) years. There was a 1.6% (n = 4807) prevalence of combined hearing loss and 0.7% (n = 2274) prevalence of IDA. Both SNHL (present in 26 of 2274 individuals [1.1%] with IDA; P = .005) and combined hearing loss (present in 77 [3.4%]; P < .001) were significantly associated with IDA. Logistic regression analysis confirmed increased odds of SNHL (adjusted odds ratio [OR], 1.82; 95% CI, 1.18-2.66) and combined hearing loss (adjusted OR, 2.41; 95% CI, 1.90-3.01) among adults with IDA, after adjusting for sex.
Conclusions and Relevance Iron deficiency anemia was associated with SNHL and combined hearing loss in a population of adult patients. Further research is needed to better understand the potential links between IDA and hearing loss and whether screening and treatment of IDA in adults could have clinical implications in patients with hearing loss.
The Association of Hot Red Chili Pepper Consumption and Mortality: A Large Population-Based Cohort Study
Abstract
The evidence base for the health effects of spice consumption is insufficient, with only one large population-based study and no reports from Europe or North America. Our objective was to analyze the association between consumption of hot red chili peppers and mortality, using a population-based prospective cohort from the National Health and Nutritional Examination Survey (NHANES) III, a representative sample of US noninstitutionalized adults, in which participants were surveyed from 1988 to 1994. The frequency of hot red chili pepper consumption was measured in 16,179 participants at least 18 years of age. Total and cause-specific mortality were the main outcome measures. During 273,877 person-years of follow-up (median 18.9 years), a total of 4,946 deaths were observed. Total mortality for participants who consumed hot red chili peppers was 21.6% compared to 33.6% for those who did not (absolute risk reduction of 12%; relative risk of 0.64). Adjusted for demographic, lifestyle, and clinical characteristics, the hazard ratio was 0.87 (P = 0.01; 95% Confidence Interval 0.77, 0.97). Consumption of hot red chili peppers was associated with a 13% reduction in the instantaneous hazard of death. Similar, but statistically nonsignificant trends were seen for deaths from vascular disease, but not from other causes. In this large population-based prospective study, the consumption of hot red chili pepper was associated with reduced mortality. Hot red chili peppers may be a beneficial component of the diet.
Citrus fruit antioxidants may prevent chronic diseases caused by obesity
Citrus fruits contain several
antioxidants
that may prevent a range of health concerns. According to a
recent article
exploring the health benefits of popular foods, citrus fruits may lower ischemic
stroke
risk, maintain
blood pressure
, and support heart health.
Fruits and vegetables contain antioxidants called flavonoids, which are the largest group of phytonutrients – plant chemicals – with more than 6,000 types. Phytonutrients along with carotenoids are responsible for the vivid colors of fruits and vegetables.
There are several groups of flavonoids, including anthocyanidins, flavanols, flavones, flavanones and isoflavones. Flavanones, such as hesperidin, eriocitrin, and eriodictyol, are abundant in citrus fruits and have been associated with lowering oxidative stress in vitro and animal models.
“Our results indicate that in the future we can use citrus flavanones, a class of antioxidants, to prevent or delay chronic diseases caused by
obesity
in humans,” says Paula S. Ferreira, a graduate student with the research team.
The investigators are presenting the results of the study at the 252nd National Meeting & Exposition of the American Chemical Society (ACS).
Frequency of a diagnosis of glaucoma in individuals who consume coffee, tea and/or soft drinks
Abstract
Aims To evaluate the association between consumption of coffee, tea or soft drinks, and glaucoma in the participants of the 2005–2006 National Health and Nutrition Examination Survey (NHANES).
Methods The exposures of interest of this retrospective cross-sectional study were caffeinated and decaffeinated coffee, iced tea, hot tea and soft drinks. The outcome of interest was a clinical diagnosis of glaucoma based on the Rotterdam criteria. Analysis of the correlation between the frequency of consumption of each type of beverage and glaucoma was performed using logistic regression modelling while controlling for age, body mass index, gender, ethnicity, smoking status and diabetes. Data were weighted using the multistage NHANES sampling design.
Results Among a total of 1678 survey participants, the overall prevalence of glaucoma was 5.1% (n=84). Most participants were non-Hispanic white (n=892; 53.2%). There were no statistically significant associations between consumption of caffeinated and decaffeinated coffee, iced tea and soft drinks, and glaucoma. Participants who consumed at least one cup of hot tea daily had a 74% decreased odds of having glaucoma compared with those who did not consume hot tea (adjusted OR=0.26, 95% CI 0.09 to 0.72, P=0.004 for trend); however, no statistically significant association existed for decaffeinated hot tea and glaucoma.
Conclusion In NHANES, participants who consumed hot tea daily were less likely to have glaucoma than those who did not consume hot tea. No significant associations were found between the consumption of coffee, iced tea, decaffeinated tea and soft drinks, and glaucoma risk. This study is limited by its cross-sectional design and use of multiple statistical testing, and larger prospective studies are needed to investigate the proposed association between tea consumption and decreased glaucoma risk.
Diet quality is associated with disability and symptom severity in multiple sclerosis
Abstract
Objective To assess the association between diet quality and intake of specific foods with disability and symptom severity in people with multiple sclerosis (MS).
Methods In 2015, participants in the North American Research Committee on MS (NARCOMS) Registry completed a dietary screener questionnaire that estimates intake of fruits, vegetables and legumes, whole grains, added sugars, and red/processed meats. We constructed an overall diet quality score for each individual based on these food groups; higher scores denoted a healthier diet. We assessed the association between diet quality and disability status as measured using Patient-Determined Disease Steps (PDDS) and symptom severity using proportional odds models, adjusting for age, sex, income, body mass index, smoking status, and disease duration. We assessed whether a composite healthy lifestyle measure, a healthier diet, healthy weight (body mass index <25), routine physical activity, and abstinence from smoking was associated with symptom severity.
Results Of the 7,639 (68%) responders, 6,989 reported physician-diagnosed MS and provided dietary information. Participants with diet quality scores in the highest quintile had lower levels of disability (PDDS; proportional odds ratio [OR] for Q5 vs Q1 0.80; 95% confidence interval [CI] 0.69–0.93) and lower depression scores (proportional OR for Q5 vs Q1 0.82; 95% CI 0.70–0.97). Individuals reporting a composite healthy lifestyle had lower odds of reporting severe fatigue (0.69; 95% CI 0.59–0.81), depression (0.53; 95% CI 0.43–0.66), pain (0.56; 95% CI 0.48–0.67), or cognitive impairment (0.67; 95% CI 0.55–0.79).
Conclusions Our large cross-sectional survey suggests a healthy diet and a composite healthy lifestyle are associated with lesser disability and symptom burden in MS.
Fruit and vegetable consumption and risk of COPD: a prospective cohort study of men FREE
Abstract
Background Antioxidants present in fruits and vegetables may protect the lung from oxidative damage and prevent COPD.
Aims To determine the association between fruit and vegetable consumption and risk of COPD by smoking status in men.
Methods The population-based prospective Cohort of Swedish Men included 44 335 men, aged 45–79 years, with no history of COPD at baseline. Fruit and vegetable consumption was assessed with a self-administered questionnaire.
Results During a mean follow-up of 13.2 years, 1918 incident cases of COPD were ascertained. A strong inverse association between total fruit and vegetable consumption and COPD was observed in smokers but not in never-smokers (p-interaction=0.02). The age-standardised incidence rate per 100 000 person-years in the lowest quintile (<2 servings/day) of total fruit and vegetable consumption was 1166 in current smokers and 506 in ex-smokers; among those in the highest quintile (≥5.3 servings/day), 546 and 255 per 100 000 person-years, respectively. The multivariable HR of COPD comparing extreme quintiles of total fruit and vegetable consumption was 0.60 (95% CI 0.47 to 0.76, p-trend <0.0001) in current smokers and 0.66 (95% CI 0.51 to 0.85, p-trend=0.001) in ex-smokers. Each one serving per day increment in total fruit and vegetable consumption decreased risk of COPD significantly by 8% (95% CI 4% to 11%) in current smokers and by 4% (95% CI 0% to 7%) in ex-smokers.
Conclusions These results indicate that high consumption of fruits and vegetables is associated with reduced COPD incidence in both current and ex-smokers but not in never-smokers.
Low carbohydrate diets may increase risk of neural tube defects
AbstractBackground
Folic acid fortification significantly reduced the prevalence of neural tube defects (NTDs) in the United States. The popularity of “low carb” diets raises concern that women who intentionally avoid carbohydrates, thereby consuming fewer fortified foods, may not have adequate dietary intake of folic acid.
Methods
To assess the association between carbohydrate intake and NTDs, we analyzed data from the National Birth Defects Prevention Study from 1,740 mothers of infants, stillbirths, and terminations with anencephaly or spina bifida (cases), and 9,545 mothers of live born infants without a birth defect (controls) conceived between 1998 and 2011. Carbohydrate and folic acid intake before conception were estimated from food frequency questionnaire responses. Restricted carbohydrate intake was defined as ≤5th percentile among controls. Odds ratios were estimated with logistic regression and adjusted for maternal race/ethnicity, education, alcohol use, folic acid supplement use, study center, and caloric intake.
Results
Mean dietary intake of folic acid among women with restricted carbohydrate intake was less than half that of other women (p < .01), and women with restricted carbohydrate intake were slightly more likely to have an infant with an NTD (AOR = 1.30, 95% CI: 1.02, 1.67).
Conclusions
This is the first study to examine the association between carbohydrate intake and NTDs among pregnancies conceived postfortification. We found that women with restricted carbohydrate intake were 30% more likely to have an infant with anencephaly or spina bifida. However, more research is needed to understand the pathways by which restricted carbohydrate intake might increase the risk of NTDs.
Adherence to the Mediterranean diet and IVF success rate among non-obese women attempting fertility
Abstract
STUDY QUESTION
Is adherence to the Mediterranean diet (MedDiet) associated with better IVF performance in women attempting fertility?
SUMMARY ANSWER
Greater adherence to the MedDiet, defined using the validated Mediterranean diet score (MedDietScore), was associated with a higher likelihood of achieving clinical pregnancy and live birth among non-obese women <35 years of age.
WHAT IS KNOWN ALREADY
Diet impacts fertility and certain nutrients and food groups appear to have a greater effect on reproductive health, but there are relatively few published data on the role of dietary patterns, and the MedDiet in particular, on assisted reproductive performance.
STUDY DESIGN, SIZE, DURATION
This prospective cohort study included 244 non-obese women (22–41 years of age; BMI < 30 kg/m2) who underwent a first IVF treatment in an Assisted Conception Unit in Athens, Greece, between November 2013 and September 2016. The study was designed to evaluate the influence of habitual dietary intake and lifestyle on fertility outcomes.
PARTICIPANTS/MATERIALS, SETTING, METHODS
Diet was assessed before the IVF treatment via a validated food-frequency questionnaire. Adherence to the MedDiet was assessed through the MedDietScore (range: 0–55), with higher scores indicating greater adherence. Intermediate outcomes (oocyte yield, fertilization rate and embryo quality measures) and clinical endpoints (implantation, clinical pregnancy and live birth) were abstracted from electronic medical records. Associations between MedDietScore and IVF outcomes were analysed using generalized linear models adjusting for age, ovarian stimulation protocol, BMI, physical activity, anxiety levels, infertility diagnosis, caloric intake and supplements use.
MAIN RESULTS AND THE ROLE OF CHANCE
No association of MedDietScore with any of the intermediate outcomes or with implantation was found. However, compared with women in the highest tertile of the MedDietScore (≥36, n = 86), women in the lowest tertile (≤30, n = 79) had significantly lower rates of clinical pregnancy (29.1 vs 50.0%, P = 0.01) and live birth (26.6 vs 48.8%, P = 0.01). The multivariable-adjusted relative risk (95% CI) for clinical pregnancy comparing women in the lowest with women in the highest tertile of the MedDietScore was 0.35 (0.16–0.78; P-trend=0.01), and for live birth it was 0.32 (0.14–0.71; P-trend = 0.01). These associations were significantly modified by women’s age (P-interaction <0.01 for both outcomes). MedDietScore was positively related to clinical pregnancy and live birth among women <35 years old (P ≤ 0.01) but not among women ≥35 years. Among women <35 years, a beneficial 5-point increase in the MedDietScore was associated with ~2.7 times higher likelihood of achieving clinical pregnancy and live birth.
LIMITATIONS, REASONS FOR CAUTION
Our finding cannot be generalized to the whole reproductive population nor to obese women nor to women attending infertility clinics around the world. In addition, due to the observational study design, causal inference is limited.
WIDER IMPLICATIONS OF THE FINDINGS
The results suggest that diet modifications and greater compliance to the Mediterranean diet may help increase the chances of a successful pregnancy and delivering a live baby for women undergoing IVF treatment.
STUDY FUNDING/COMPETING INTEREST(S)
This work was partially supported by a grand from Harokopio University (KE321). All authors declare no conflicts of interest.
Association Between Dietary Fiber and Lower Risk of All-Cause Mortality: A Meta-Analysis of Cohort Studies
Although in vitro and in vivo experiments have suggested that dietary fiber might have beneficial effects on health, results on the association between fiber intake and all-cause mortality in epidemiologic studies have been inconsistent. Therefore, we conducted a meta-analysis of prospective cohort studies to quantitatively assess this association. Pertinent studies were identified by searching articles in PubMed and Web of Knowledge through May 2014 and reviewing the reference lists of the retrieved articles. Study-specific risk estimates were combined using random-effects models. Seventeen prospective studies (1997–2014) that had a total of 67,260 deaths and 982,411 cohort members were included. When comparing persons with dietary fiber intakes in the top tertile with persons whose intakes were in the bottom tertile, we found a statistically significant inverse association between fiber intake and all-cause mortality, with an overall relative risk of 0.84 (95% confidence interval: 0.80, 0.87; I2 = 41.2%). There was a 10% reduction in risk for per each 10-g/day increase in fiber intake (relative risk = 0.90; 95% confidence interval: 0.86, 0.94; I2 = 77.2%). The combined estimate was robust across subgroup and sensitivity analyses. No publication bias was detected. A higher dietary fiber intake was associated with a reduced risk of death. These findings suggest that fiber intake may offer a potential public health benefit in reducing all-cause mortality.
Specific Dietary Fats in Relation to Total and Cause-Specific Mortality
Abstract
Importance
Previous studies have shown distinct associations between specific dietary fat and cardiovascular disease. However, evidence on specific dietary fats and mortality remains limited and inconsistent.
Objective
To examine the associations of specific dietary fats with total and cause-specific mortality in two large ongoing prospective cohort studies.
Design, setting, and participants
We investigated 83,349 women from the Nurses’ Health Study (1980-2012) and 42,884 men from the Health Professionals Follow-up Study (1986-2012) who were free from cardiovascular disease, cancer and diabetes at baseline. Dietary fat intake was assessed at baseline and updated every 2 to 4 years.
Main outcomes and measures
We performed systematic searches of the vital records of states and of the National Death Index, supplemented by reports from family members or postal authorities.
Results
We documented 33,304 deaths during 3,439,954 person-years of follow-up. After adjustment for known and suspected risk factors, dietary total fat, compared to total carbohydrate, was inversely associated with total mortality (P for trend <0.001). The hazard ratios (HRs) of total mortality comparing extreme quintiles of specific dietary fats was 1.08, (95% confidence interval (CI), 1.03-1.14) for saturated fat, 0.81 (95% CI, 0.78-0.84) for polyunsaturated fat, 0.89 (95% CI, 0.84-0.94) for monounsaturated fat and 1.13 (95% CI, 1.07-1.18) for trans fat (P for trend <0.001 for all). Replacing 5% of energy from saturated fats with equivalent energy from polyunsaturated fats and monounsaturated fats was associated with 27% (HR =0.73, 95% CI, 0.70-0.77) and 13% (HR =0.87, 95% CI, 0.82-0.93) estimated reductions in total mortality, respectively. HR of total mortality comparing extreme quintiles of n-6 polyunsaturated fat intake was 0.85 (95% CI, 0.81-0.89). Intake of n-6 polyunsaturated fat, especially linoleic acid, was inversely associated with mortality due to most major causes, while marine n-3 polyunsaturated fat intake was associated with a modestly lower total mortality (HR comparing extreme quintiles =0.96, 95% CI, 0.93-1.00).
Conclusions and relevance
Different types of dietary fats have divergent associations with total and cause-specific mortality. These findings support current dietary recommendations to replace saturated and trans fat with unsaturated fats.
Keywords: Fatty acids, Mortality, Cardiovascular diseases, Cancer, Saturated fat, Polyunsaturated fat, Diet
Anatomy of health effects of Mediterranean diet: Greek EPIC prospective cohort study
Abstract
Objective To investigate the relative importance of the individual components of the Mediterranean diet in generating the inverse association of increased adherence to this diet and overall mortality.
Design Prospective cohort study.
Setting Greek segment of the European Prospective Investigation into Cancer and nutrition (EPIC).
Participants 23 349 men and women, not previously diagnosed with cancer, coronary heart disease, or diabetes, with documented survival status until June 2008 and complete information on nutritional variables and important covariates at enrolment.
Main outcome measure All cause mortality.
Results After a mean follow-up of 8.5 years, 652 deaths from any cause had occurred among 12 694 participants with Mediterranean diet scores 0-4 and 423 among 10 655 participants with scores of 5 or more. Controlling for potential confounders, higher adherence to a Mediterranean diet was associated with a statistically significant reduction in total mortality (adjusted mortality ratio per two unit increase in score 0.864, 95% confidence interval 0.802 to 0.932). The contributions of the individual components of the Mediterranean diet to this association were moderate ethanol consumption 23.5%, low consumption of meat and meat products 16.6%, high vegetable consumption 16.2%, high fruit and nut consumption 11.2%, high monounsaturated to saturated lipid ratio 10.6%, and high legume consumption 9.7%. The contributions of high cereal consumption and low dairy consumption were minimal, whereas high fish and seafood consumption was associated with a non-significant increase in mortality ratio.
Conclusion The dominant components of the Mediterranean diet score as a predictor of lower mortality are moderate consumption of ethanol, low consumption of meat and meat products, and high consumption of vegetables, fruits and nuts, olive oil, and legumes. Minimal contributions were found for cereals and dairy products, possibly because they are heterogeneous categories of foods with differential health effects, and for fish and seafood, the intake of which is low in this population.
Analysis and valuation of the health and climate change cobenefits of dietary change
Abstract
What we eat greatly influences our personal health and the environment we all share. Recent analyses have highlighted the likely dual health and environmental benefits of reducing the fraction of animal-sourced foods in our diets. Here, we couple for the first time, to our knowledge, a region-specific global health model based on dietary and weight-related risk factors with emissions accounting and economic valuation modules to quantify the linked health and environmental consequences of dietary changes. We find that the impacts of dietary changes toward less meat and more plant-based diets vary greatly among regions. The largest absolute environmental and health benefits result from diet shifts in developing countries whereas Western high-income and middle-income countries gain most in per capita terms. Transitioning toward more plant-based diets that are in line with standard dietary guidelines could reduce global mortality by 6–10% and food-related greenhouse gas emissions by 29–70% compared with a reference scenario in 2050. We find that the monetized value of the improvements in health would be comparable with, or exceed, the value of the environmental benefits although the exact valuation method used considerably affects the estimated amounts. Overall, we estimate the economic benefits of improving diets to be 1–31 trillion US dollars, which is equivalent to 0.4–13% of global gross domestic product (GDP) in 2050. However, significant changes in the global food system would be necessary for regional diets to match the dietary patterns studied here.
Association of Changes in Diet Quality with Total and Cause-Specific Mortality
Abstract
BACKGROUND
Few studies have evaluated the relationship between changes in diet quality over time and the risk of death.
METHODS
We used Cox proportional-hazards models to calculate adjusted hazard ratios for total and cause-specific mortality among 47,994 women in the Nurses’ Health Study and 25,745 men in the Health Professionals Follow-up Study from 1998 through 2010. Changes in diet quality over the preceding 12 years (1986–1998) were assessed with the use of the Alternate Healthy Eating Index–2010 score, the Alternate Mediterranean Diet score, and the Dietary Approaches to Stop Hypertension (DASH) diet score.
RESULTS
The pooled hazard ratios for all-cause mortality among participants who had the greatest improvement in diet quality (13 to 33% improvement), as compared with those who had a relatively stable diet quality (0 to 3% improvement), in the 12-year period were the following: 0.91 (95% confidence interval [CI], 0.85 to 0.97) according to changes in the Alternate Healthy Eating Index score, 0.84 (95 CI%, 0.78 to 0.91) according to changes in the Alternate Mediterranean Diet score, and 0.89 (95% CI, 0.84 to 0.95) according to changes in the DASH score. A 20-percentile increase in diet scores (indicating an improved quality of diet) was significantly associated with a reduction in total mortality of 8 to 17% with the use of the three diet indexes and a 7 to 15% reduction in the risk of death from cardiovascular disease with the use of the Alternate Healthy Eating Index and Alternate Mediterranean Diet. Among participants who maintained a high-quality diet over a 12-year period, the risk of death from any cause was significantly lower — by 14% (95% CI, 8 to 19) when assessed with the Alternate Healthy Eating Index score, 11% (95% CI, 5 to 18) when assessed with the Alternate Mediterranean Diet score, and 9% (95% CI, 2 to 15) when assessed with the DASH score — than the risk among participants with consistently low diet scores over time.
CONCLUSIONS
Improved diet quality over 12 years was consistently associated with a decreased risk of death. (Funded by the National Institutes of Health.)
Baseline fatty acids, food groups, a diet score and 50-year all-cause mortality rates. An ecological analysis of the Seven Countries Study
Abstract
Objectives: This analysis deals with the ecologic relationships of dietary fatty acids, food groups and the Mediterranean Adequacy Index (MAI, derived from 15 food groups) with 50-year all-cause mortality rates in 16 cohorts of the Seven Countries Study.
Material and methods: A dietary survey was conducted at baseline in cohorts subsamples including chemical analysis of food samples representing average consumptions. Ecologic correlations of dietary variables were computed across cohorts with 50-year all-cause mortality rates, where 97% of men had died.
Results: There was a 12-year average age at death population difference between extreme cohorts. In the 1960s the average population intake of saturated (S) and trans (T) fatty acids and hard fats was high in the northern European cohorts while monounsaturated (M), polyunsaturated (P) fatty acids and vegetable oils were high in the Mediterranean areas and total fat was low in Japan. The 50-year all-cause mortality rates correlated (r= −0.51 to −0.64) ecologically inversely with the ratios M/S, (M + P)/(S + T) and vegetable foods and the ratio hard fats/vegetable oils. Adjustment for high socio-economic status strengthened (r= −0.62 to −0.77) these associations including MAI diet score.
Conclusion: The protective fatty acids and vegetable oils are indicators of the low risk traditional Mediterranean style diets.
Low carbohydrate diets: going against the grain
Low carbohydrate high fat (LCHF) diets continue to attract media attention, despite a substantial body of evidence showing that a range of dietary patterns promote health and reduce risk of chronic disease. LCHF diets invariably involve radical restriction of total carbohydrate (typically <12% of energy intake) and largely unrestricted intakes of foods rich in saturated fat. Support for LCHF diets has been partly fuelled by the publication of some papers apparently suggestive of benefit.
1
,
2
,
3
Recent evidence, however, confirms the established cornerstones of dietary advice—reduce saturated fat, free sugars, and sodium and increase wholegrain cereals and fibre—although changing disease patterns and additional data have necessitated some changes in emphasis.
Biodiversity conservation: The key is reducing meat consumption
Abstract
The consumption of animal-sourced food products by humans is one of the most powerful negative forces affecting the conservation of
terrestrial ecosystems
and biological diversity.
Livestock production
is the single largest driver of habitat loss, and both livestock and feedstock production are increasing in developing tropical countries where the majority of biological diversity resides.
Bushmeat
consumption in Africa and southeastern Asia, as well as the high growth-rate of per capita livestock consumption in China are of special concern. The projected land base required by 2050 to support livestock production in several megadiverse countries exceeds 30–50% of their current agricultural areas. Livestock production is also a leading cause of climate change, soil loss, water and nutrient pollution, and decreases of apex predators and wild herbivores, compounding pressures on ecosystems and biodiversity. It is possible to greatly reduce the impacts of animal product consumption by humans on natural ecosystems and biodiversity while meeting nutritional needs of people, including the projected 2–3 billion people to be added to human population. We suggest that impacts can be remediated through several solutions: (1) reducing demand for animal-based food products and increasing proportions of plant-based foods in diets, the latter ideally to a global average of 90% of food consumed; (2) replacing ecologically-inefficient ruminants (e.g. cattle, goats, sheep) and bushmeat with monogastrics (e.g. poultry, pigs), integrated
aquaculture
, and other more-efficient protein sources; and (3) reintegrating livestock production away from single-product, intensive, fossil-fuel based systems into diverse, coupled systems designed more closely around the structure and functions of ecosystems that conserve energy and nutrients. Such efforts would also impart positive impacts on human health through reduction of diseases of nutritional extravagance.
Can We Say What Diet Is Best for Health?
Abstract
Diet is established among the most important influences on health in modern societies. Injudicious diet figures among the leading causes of premature death and chronic disease. Optimal eating is associated with increased life expectancy, dramatic reduction in lifetime risk of all chronic disease, and amelioration of gene expression. In this context, claims abound for the competitive merits of various diets relative to one another. Whereas such claims, particularly when attached to commercial interests, emphasize distinctions, the fundamentals of virtually all eating patterns associated with meaningful evidence of health benefit overlap substantially. There have been no rigorous, long-term studies comparing contenders for best diet laurels using methodology that precludes bias and confounding, and for many reasons such studies are unlikely. In the absence of such direct comparisons, claims for the established superiority of any one specific diet over others are exaggerated. The weight of evidence strongly supports a theme of healthful eating while allowing for variations on that theme. A diet of minimally processed foods close to nature, predominantly plants, is decisively associated with health promotion and disease prevention and is consistent with the salient components of seemingly distinct dietary approaches. Efforts to improve public health through diet are forestalled not for want of knowledge about the optimal feeding of Homo sapiens but for distractions associated with exaggerated claims, and our failure to convert what we reliably know into what we routinely do. Knowledge in this case is not, as of yet, power; would that it were so.
Position of the Academy of Nutrition and Dietetics: Vegetarian Diets
Abstract
It is the position of the Academy of Nutrition and Dietetics that appropriately planned vegetarian, including vegan, diets are healthful, nutritionally adequate, and may provide health benefits for the prevention and treatment of certain diseases. These diets are appropriate for all stages of the life cycle, including pregnancy, lactation, infancy, childhood, adolescence, older adulthood, and for athletes. Plant-based diets are more environmentally sustainable than diets rich in animal products because they use fewer natural resources and are associated with much less environmental damage. Vegetarians and vegans are at reduced risk of certain health conditions, including ischemic heart disease, type 2 diabetes, hypertension, certain types of cancer, and obesity. Low intake of saturated fat and high intakes of vegetables, fruits, whole grains, legumes, soy products, nuts, and seeds (all rich in fiber and phytochemicals) are characteristics of vegetarian and vegan diets that produce lower total and low-density lipoprotein cholesterol levels and better serum glucose control. These factors contribute to reduction of chronic disease. Vegans need reliable sources of vitamin B-12, such as fortified foods or supplements.
Association of Animal and Plant Protein Intake With All-Cause and Cause-Specific Mortality
Abstract
Importance: Defining what represents a macronutritionally balanced diet remains an open question and a high priority in nutrition research. Although the amount of protein may have specific effects, from a broader dietary perspective, the choice of protein sources will inevitably influence other components of diet and may be a critical determinant for the health outcome.
Objective: To examine the associations of animal and plant protein intake with the risk for mortality.
Design, setting, and participants: This prospective cohort study of US health care professionals included 131 342 participants from the Nurses' Health Study (1980 to end of follow-up on June 1, 2012) and Health Professionals Follow-up Study (1986 to end of follow-up on January 31, 2012). Animal and plant protein intake was assessed by regularly updated validated food frequency questionnaires. Data were analyzed from June 20, 2014, to January 18, 2016.
Main outcomes and measures: Hazard ratios (HRs) for all-cause and cause-specific mortality.
Results: Of the 131 342 participants, 85 013 were women (64.7%) and 46 329 were men (35.3%) (mean [SD] age, 49 [9] years). The median protein intake, as assessed by percentage of energy, was 14% for animal protein (5th-95th percentile, 9%-22%) and 4% for plant protein (5th-95th percentile, 2%-6%). After adjusting for major lifestyle and dietary risk factors, animal protein intake was not associated with all-cause mortality (HR, 1.02 per 10% energy increment; 95% CI, 0.98-1.05; P for trend = .33) but was associated with higher cardiovascular mortality (HR, 1.08 per 10% energy increment; 95% CI, 1.01-1.16; P for trend = .04). Plant protein was associated with lower all-cause mortality (HR, 0.90 per 3% energy increment; 95% CI, 0.86-0.95; P for trend < .001) and cardiovascular mortality (HR, 0.88 per 3% energy increment; 95% CI, 0.80-0.97; P for trend = .007). These associations were confined to participants with at least 1 unhealthy lifestyle factor based on smoking, heavy alcohol intake, overweight or obesity, and physical inactivity, but not evident among those without any of these risk factors. Replacing animal protein of various origins with plant protein was associated with lower mortality. In particular, the HRs for all-cause mortality were 0.66 (95% CI, 0.59-0.75) when 3% of energy from plant protein was substituted for an equivalent amount of protein from processed red meat, 0.88 (95% CI, 0.84-0.92) from unprocessed red meat, and 0.81 (95% CI, 0.75-0.88) from egg.
Conclusions and relevance: High animal protein intake was positively associated with cardiovascular mortality and high plant protein intake was inversely associated with all-cause and cardiovascular mortality, especially among individuals with at least 1 lifestyle risk factor. Substitution of plant protein for animal protein, especially that from processed red meat, was associated with lower mortality, suggesting the importance of protein source.
Mortality from different causes associated with meat, heme iron, nitrates, and nitrites in the NIH-AARP Diet and Health Study: population based cohort study
Abstract
Objective To determine the association of different types of meat intake and meat associated compounds with overall and cause specific mortality.
Design Population based cohort study.
Setting Baseline dietary data of the NIH-AARP Diet and Health Study (prospective cohort of the general population from six states and two metropolitan areas in the US) and 16 year follow-up data until 31 December 2011.
Participants 536 969 AARP members aged 50-71 at baseline.
Exposures Intake of total meat, processed and unprocessed red meat (beef, lamb, and pork) and white meat (poultry and fish), heme iron, and nitrate/nitrite from processed meat based on dietary questionnaire. Adjusted Cox proportional hazards regression models were used with the lowest fifth of calorie adjusted intakes as reference categories.
Main outcome measure Mortality from any cause during follow-up.
Results An increased risk of all cause mortality (hazard ratio for highest versus lowest fifth 1.26, 95% confidence interval 1.23 to 1.29) and death due to nine different causes associated with red meat intake was observed. Both processed and unprocessed red meat intakes were associated with all cause and cause specific mortality. Heme iron and processed meat nitrate/nitrite were independently associated with increased risk of all cause and cause specific mortality. Mediation models estimated that the increased mortality associated with processed red meat was influenced by nitrate intake (37.0-72.0%) and to a lesser degree by heme iron (20.9-24.1%). When the total meat intake was constant, the highest fifth of white meat intake was associated with a 25% reduction in risk of all cause mortality compared with the lowest intake level. Almost all causes of death showed an inverse association with white meat intake.
Conclusions The results show increased risks of all cause mortality and death due to nine different causes associated with both processed and unprocessed red meat, accounted for, in part, by heme iron and nitrate/nitrite from processed meat. They also show reduced risks associated with substituting white meat, particularly unprocessed white meat.
Fruit and vegetable intake, physical activity, and mortality in older community-dwelling women
Abstract
Objectives: To examine the relationship between fruit and vegetable intake, physical activity, and all-cause mortality in older women.
Design: Six Cox proportional hazards models examined independent and additive relationships between physical activity, carotenoids, and all-cause mortality. Additional models tested whether physical activity and carotenoids were conjointly related to mortality. Models were adjusted for age, education, and race and ethnicity.
Setting: Baltimore, Maryland.
Participants: Seven hundred thirteen women aged 70 to 79 participating in the Women's Health and Aging Studies.
Measurements: Total serum carotenoids, a marker of fruit and vegetable intake, and physical activity were measured at baseline. Physical activity was measured according to kilocalorie expenditure.
Results: During 5 years of follow-up, 82 (11.5%) participants died. Measured continuously, physical activity improved survival (HR = 0.52, 95% CI = 0.41-0.66, P < .001). The most active women were more likely to survive than the least physically active women (HR = 0.28, 95% CI = 0.13-0.59, P < .001). Continuous measures of carotenoids improved survival (HR = 0.67, 95% CI = 0.51-0.89, P = .01). Women in the highest tertile of total carotenoids were more likely to survive those in the lowest (HR = 0.50, 95% CI = 0.27-0.91, P = .03). When examined in the same model, continuous measures of physical activity (HR = 0.54, 95% CI = 0.42-0.68, P < .001) and carotenoids (HR = 0.76, 95% CI = 0.59-0.98, P = .04) predicted survival during follow-up.
Conclusion: The combination of low total serum carotenoids and low physical activity, both modifiable risk factors, strongly predicted earlier mortality. These findings provide preliminary support that higher fruit and vegetable intake and exercise improve survival.