por Qabas Al-Jobori hace 1 año
112
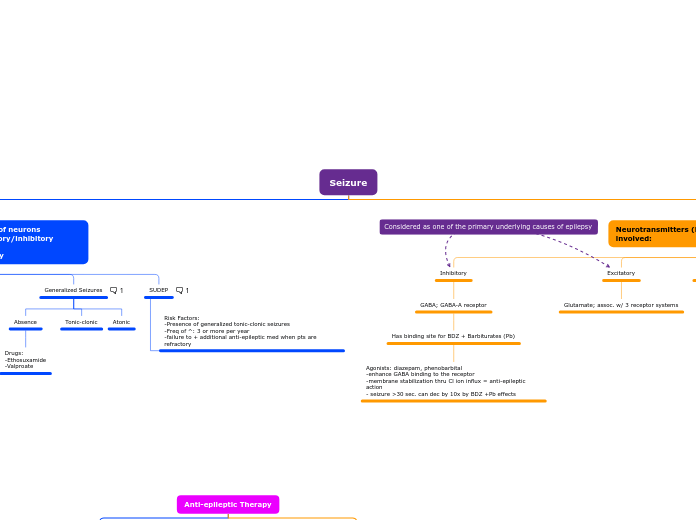
Seizure
A multi-faceted approach is crucial for managing epilepsy, encompassing both non-pharmacologic and pharmacologic strategies. Vagal Nerve Stimulation (VNS) is a safe non-pharmacologic option, though it may cause minor side effects like voice changes and coughing.