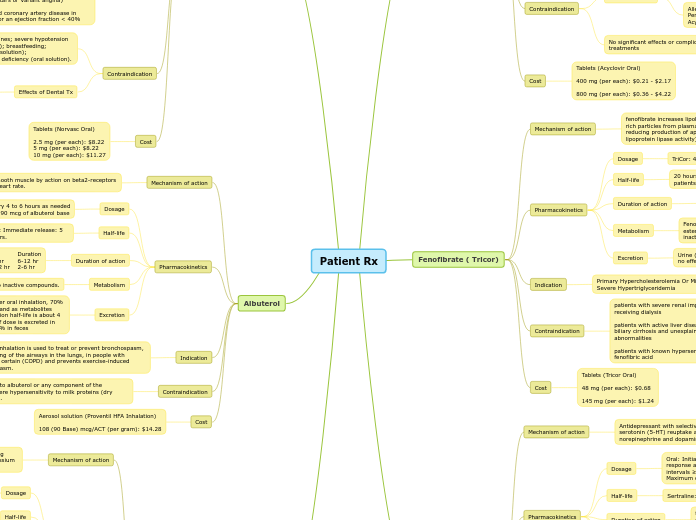
Patient Rx
Acyclovir (Zovirax)
Mechanism of action
Acyclovir triphosphate inhibits DNA synthesis and viral replication by competing with deoxyguanosine triphosphate for viral DNA polymerase and being incorporated into viral DNA.
Pharmacokinetics
Dosage
800mg/once a day
Half-life
Adults: ~2.5 hours (with normal renal function)
20 hours with End-Stage Renal Disease (ESRD)
Hemodialysis: ~5 hours
Duration of action
May take up to two hours to reach peak plasma concentrations after oral acyclovir administration.
Metabolism
Converted by viral enzymes to acyclovir monophosphate, and further converted to diphosphate then triphosphate (active form) by cellular enzymes
Excretion
Urine (62% to 91% as unchanged drug and metabolite)
Indication
The treatment of initial episodes of herpes genitalis. The suppression of unusually frequent recurrences of herpes genitalis (6 or more episodes per year). The acute treatment of herpes zoster (shingles) and varicella (chickenpox).
My Pt takes it for Chronic suppression of recurrent herpes labialis (cold sores)
Contraindication
Hypersensitivity
Cautions include renal failure/impairment, immunocompromised host, potential risk of thrombotic thrombocytopenic purpura (TTP), and hemolytic uremic syndrome (HUS)
Allergies:
Penciclovir Analogues
Acyclovir Analogues
No significant effects or complications reported for dental treatments
Cost
Tablets (Acyclovir Oral)
400 mg (per each): $0.21 - $2.17
800 mg (per each): $0.36 - $4.22
Fenofibrate ( Tricor)
Mechanism of action
fenofibrate increases lipolysis and elimination of triglyceride-rich particles from plasma by activating lipoprotein lipase and reducing production of apoprotein C-III (an inhibitor of lipoprotein lipase activity)
Pharmacokinetics
Dosage
TriCor: 48 to 145 mg once daily; maximum dose: 145 mg/day
Half-life
20 hours (range: 10 to 35 hours); half-life prolonged in patients with renal impairment
Duration of action
Peak plasma levels of fenofibric acid occur within 6 to 8 hours after administration.
Metabolism
Fenofibrate is metabolized in the tissue and plasma via esterases to the active form, fenofibric acid; undergoes inactivation by glucuronidation hepatically or renally
Excretion
Urine (~60% as metabolites); feces (25%); hemodialysis has no effect on removal of fenofibric acid from plasma
Indication
Primary Hypercholesterolemia Or Mixed Dyslipidemia
Severe Hypertriglyceridemia
Contraindication
patients with severe renal impairment, including those receiving dialysis
patients with active liver disease, including those with primary biliary cirrhosis and unexplained persistent liver function abnormalities
patients with known hypersensitivity to fenofibrate or fenofibric acid
Cost
Tablets (Tricor Oral)
48 mg (per each): $0.68
145 mg (per each): $1.24
Sertraline ( Zoloft)
Mechanism of action
Antidepressant with selective inhibitory effects on presynaptic serotonin (5-HT) reuptake and only very weak effects on norepinephrine and dopamine neuronal uptake.
Pharmacokinetics
Dosage
Oral: Initial: 25 mg once daily; may increase dose based on response and tolerability in increments of 25 to 50 mg at intervals ≥1 to 2 weeks. Usual dose: 50 to 150 mg/day. Maximum dose: 200 mg/day
Half-life
Sertraline: Mean: 26 hours
Duration of action
following oral once-daily dosing over the range of 50 to 200 mg for 14 days, mean peak plasma concentrations (Cmax) of sertraline occurred between 4.5 to 8.4 hours post-dosing.
Metabolism
Hepatic; involve CYP2C19 and CYP2D6; extensive first pass metabolism; forms metabolite N-desmethylsertraline
Excretion
Urine (40% to 45% as metabolites); feces (40% to 45%; 12% to 14% as unchanged drug)
Indication
treatment of obsessive-compulsive disorder, panic disorder, post-traumatic stress disorder, premenstrual dysphoric disorder, and social anxiety disorder.
Contraindication
Use of MAOIs including linezolid or methylene blue (concurrently or within 14 days of stopping an MAOI or sertraline); concurrent use with pimozide; hypersensitivity (eg, anaphylaxis, angioedema) to sertraline or any component of the formulation; concurrent use with disulfiram
Dental Interaction:
enhance the antiplatelet effect of Aspirin ( increased risk of bleeding)
Xerostomia
Cost
Tablets (Zoloft Oral)
25 mg (per each): $14.04
50 mg (per each): $14.04
100 mg (per each): $14.04
AmLODIPine (Norvasc)
Mechanism of action
nhibits calcium ion from entering the “slow channels” or select voltage-sensitive areas of vascular smooth muscle and myocardium during depolarization, producing a relaxation of coronary vascular smooth muscle and coronary vasodilation
Pharmacokinetics
Dosage
Hypertension:
Oral: Initial: 2.5 to 5 mg once daily; titrate every 1 to 2 weeks as needed based on patient response; maximum: 10 mg/day
Half-life
Terminal (biphasic): 30 to 50 hours; increased with hepatic dysfunction
Duration of action
At least 24 hours
Metabolism
Amlodipine is heavily (approximately 90%) converted to inactive metabolites via hepatic breakdown with 10% of the parent compound and 60% of the metabolites found excreted in the urine
Excretion
Urine (10% of total dose as unchanged drug, 60% of total dose as metabolites)
Clearance: May be decreased in patients with hepatic insufficiency or moderate to severe heart failure; weight-adjusted clearance in children >6 years of age is similar to adult
Indication
Hypertension
• Coronary artery disease
• Chronic stable angina
• Vasospastic angina (Prinzmetal’s or Variant angina)
• Angiographically documented coronary artery disease in patients without heart failure or an ejection fraction < 40%
Contraindication
ypersensitivity to other dihydropyridines; severe hypotension (systolic blood pressure <90 mm Hg); breastfeeding; hereditary fructose intolerance (oral solution); hyperglycerolemia or glycerol kinase deficiency (oral solution).
Effects of Dental Tx
ingival hyperplasia with amlodipine than with other calcium channel blockers (usually resolves upon discontinuation)
xerostomia, orthostatic hypotension, and erythema multiforme (severe oral ulcerations that respond well to systemic steroid therapy)
Cost
Tablets (Norvasc Oral)
2.5 mg (per each): $8.22
5 mg (per each): $8.22
10 mg (per each): $11.27
Albuterol
Mechanism of action
Relaxes bronchial smooth muscle by action on beta2-receptors with little effect on heart rate.
Pharmacokinetics
Dosage
2 inhalations every 4 to 6 hours as needed
each actuation = 90 mcg of albuterol base
Half-life
Oral inhalation: 3.8 to ~5 hours; Oral: Immediate release: 5 to 6 hours, Extended release: 9.3 hours.
Duration of action
Route Onset Peak Duration
P.O. 15-30 min 2-3 hr 6-12 hr
Inhalation 5-15 min 1/2-2 hr 2-6 hr
Metabolism
Extensively metabolized in the liver to inactive compounds.
Excretion
Rapidly excreted in urine and feces. After oral inhalation, 70% of dose is excreted in urine unchanged and as metabolites within 24 hours; 10% in feces. Elimination half-life is about 4 hours. After oral administration, 75% of dose is excreted in urine within 72 hours as metabolites; 4% in feces
Indication
Albuterol inhalation is used to treat or prevent bronchospasm, or narrowing of the airways in the lungs, in people with asthma or certain (COPD) and prevents exercise-induced bronchospasm.
Contraindication
Hypersensitivity to albuterol or any component of the formulation; severe hypersensitivity to milk proteins (dry powder inhalers).
Cost
Aerosol solution (Proventil HFA Inhalation)
108 (90 Base) mcg/ACT (per gram): $14.28
HydroCHLOROthiazide (Microzide)
Mechanism of action
inhibits sodium re-absorption in the distal tubules causing increased excretion of sodium and water as well as potassium and hydrogen ions
Pharmacokinetics
Dosage
Hypertension:
nitial: 12.5 to 25 mg once daily; titrate as needed based on patient response up to 50 mg once daily
Half-life
6 to 15 hours.
Duration of action
Onset of action occurs within 2 hours of dosing, peak effect is observed at about 4 hours, and activity persists for up to 24 hours.
Metabolism
is not metabolized, and a majority is excreted in the urine unchanged. It also causes a loss of potassium and bicarbonate
Excretion
Urine (≥61% as unchanged drug).
Indication
management of hypertension.
management of edema associated with congestive heart failure, hepatic cirrhosis, nephrotic syndrome, acute glomerulonephritis, chronic renal failure, and corticosteroid and estrogen therapy.
Contraindication
Hypersensitivity to hydrochlorothiazide, any component of the formulation, or sulfonamide-derived drugs; anuria
Effects on Dental Treatment:
Patients may experience orthostatic hypotension as they stand up after treatment; especially if lying in dental chair for extended periods of time
Cost
Capsules (hydroCHLOROthiazide Oral)
12.5 mg (per each): $0.42 - $0.43
Tablets (hydroCHLOROthiazide Oral)
12.5 mg (per each): $0.17 - $0.82
25 mg (per each): $0.08 - $0.13
50 mg (per each): $0.13 - $0.16