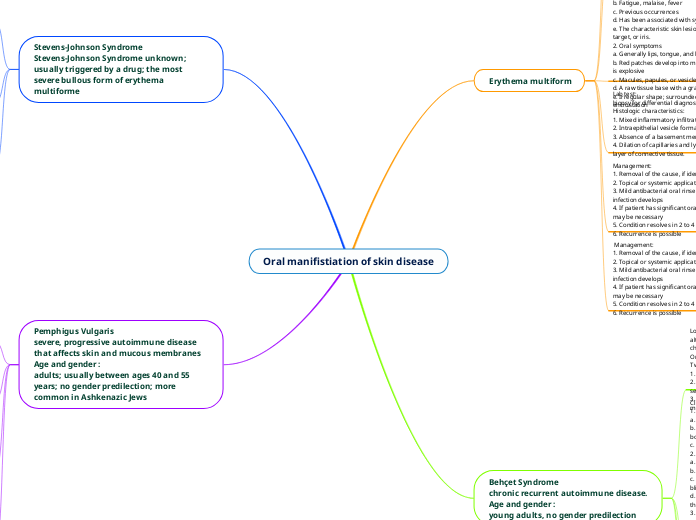
Oral manifistiation of skin disease
Erythema multiform
Def:Erythema Multiforme
1. Acute.
2- hypersensitivity reaction
3-triggered by herpes simplex virus (HSV )infection, tuberculosis, or histoplasmosis;drugs, e.g., barbituates and sulfonormides
3. Immunologic response
Epidimilogy :
young adults ;more common in males
Location:
1. Extremities
2. Skin—macular, papular, or bullous eruptions; characteristic “target” or “bull’s eye” lesions
3. Oral findings—lips, buccal mucosa, tongue
Clinical picture:
1. Systemic symptoms
a. Abrupt onset
b. Fatigue, malaise, fever
c. Previous occurrences
d. Has been associated with systemic conditions
e. The characteristic skin lesion is referred to as bull’s eye, target, or iris.
2. Oral symptoms
a. Generally lips, tongue, and buccal mucosa
b. Red patches develop into multiple, painful ulcerations; onset is explosive
c. Macules, papules, or vesicles ulcerate and bleed easily
d. A raw tissue base with a grayish, necrotic slough
e. Irregular shape; surrounded by a band of inflammation; encrustation
Lab test:
biopsy for differential diagnosis
Histologic characteristics:
1. Mixed inflammatory infiltrate
2. Intraepithelial vesicle formation and thinning
3. Absence of a basement membrane
4. Dilation of capillaries and lymphatic vessels in the surface layer of connective tissue.
Management:
1. Removal of the cause, if identified
2. Topical or systemic applications of corticosteroids
3. Mild antibacterial oral rinses; antibiotics if secondary infection develops
4. If patient has significant oral pain, intravenous rehydration may be necessary
5. Condition resolves in 2 to 4 weeks
6. Recurrence is possible
Management:
1. Removal of the cause, if identified
2. Topical or systemic applications of corticosteroids
3. Mild antibacterial oral rinses; antibiotics if secondary infection develops
4. If patient has significant oral pain, intravenous rehydration may be necessary
5. Condition resolves in 2 to 4 weeks
6. Recurrence is possible
Behçet Syndrome
chronic recurrent autoimmune disease.
Age and gender :
young adults, no gender predilection
Location :
although now considered a multisystem disorder, it is characterized by a triad of locations:
Oral, ocular, and genital areas are involved.
Two of the three areas must be involved for the diagnosis
1. Oral cavity—in most cases, the first manifestation
2. Eyes are involved in up to 85% of cases, with greater severity in men
3. Genital lesions occur in 75% of cases (more involvement in men)
Clinical features :
1. Oral lesions
a. Painful ulcerations similar to aphthous ulcers
b. Large ulcers with gray or yellow center surrounded by a red border,
c. Oral ulcerations involve the soft palate and oropharynx
2. Eye lesions
a. Begin with photophobia and irritation
b. Purulent conjunctivitis and uveitis
c. Healing may be followed by scarification and, consequently, blindness
d. Hypopyon (pus in the anterior chamber of the eye between the iris and the cornea) in severe cases; rare.
3. Genital lesions
a. In females—painful ulcerations in the vulval folds and labia majora
b. In males—painful ulcerations on the scrotum and the base of the penis
4. Systemic symptoms
a. Occasionally fever; pallor
b. Complications can involve the central nervous, cardiac, and pulmonary systems
Lab. Tests
1. Cutaneous pathergy test is positive in many patients with Behçet syndrome
2. Specific changes involving the neutrophils .
Histologic characteristics
1. Endothelial proliferation in lesions
2. Other characteristics similar to those of aphthous stomatitis
Treatment :
1. Systemic and topical corticosteroids
2. Other immunosuppressive drugs are given for systemic and ocular involvement
3. Lesions last 2 to 4 weeks
4. Disease is long lasting with remission periods.
Stevens-Johnson Syndrome
Stevens-Johnson Syndrome unknown; usually triggered by a drug; the most severe bullous form of erythema multiforme
Etiology:
children and young adults under 25 years; more common in males; history of previous similar illness
Location:
oral cavity, skin; lesions involving the eyes or genitalia must be present for the diagnosis to be made.
Clinical features :
1. Oral symptoms—bullae rupture, leaving ulcerations with a raw base; eating becomes
impossible; lips are severely encrusted and bleed easily
2. Skin lesions—severe, numerous; cover wide areas of the body (face, chest, abdomen)
3. Eye involvement—severe conjunctivitis, photophobia, corneal ulceration, scarring, and
blindness.
Managemant:
1. Antibiotics and corticosteroids to control severity
2. Sometimes antiviral medications to reduce recurrent episodes if HSV recurs
3. Duration of 1 to 4 weeks
4. Some patients require hospitalization
5. Prognosis is good.
Pemphigus Vulgaris
severe, progressive autoimmune disease that affects skin and mucous membranes
Age and gender :
adults; usually between ages 40 and 55 years; no gender predilection; more common in Ashkenazic Jews
Location and clinical features :
anywhere on the oral mucosa; eyes, skin
Location
1. In over 50% of cases, the oral lesions appear first. Skin lesions can erupt many months or even a year later
2. Blisters (caused by an abnormal production of autoantibodies), vesicles, or bullae collapse as soon as they are formed
a. Vary in shape and size (from several millimeters to several centimeters)
b. Ragged peripheral borders; flat or shallow; base intensely red and raw; may extend into the lips with crusting
3. Filmy, necrotic slough of tissue can be detached from underlying tissue
4. Neighboring soft tissue appears normal
5. Nikolsky sign present—an intraoral bulla can form under light pressure from air
syringe or tongue blade; same reaction can occur if pressure is applied to skin
6. Pain may be severe, and the person is unable to eat
7. Salivation is profuse; mouth odor
8. Gingival desquamation
Lab. Tests :
1. Biopsy and most conclusive microscopic analysis
2. Direct immunofluorescence used to identify antibodies (intercellular)
3. Indirect immunofluorescence is positive for 80% to 90% of patients with pemphigus vulgaris, showing circulating autoantibodies in the serum. It is also used to monitor the patient’s therapy
Histological features :
1. The vesicle is entirely intraepithelial above the basal cell layer, producing a distinctive “split”; the basement layer stays attached to underlying connective tissue
2. Intercellular bridges between epithelial cells disappear, with loss of cohesiveness; epithelial cells separate (acantholysis)
3. Clumps of rounded epithelial cells, called Tzanck cells, are present
4. Some inflammatory cell infiltration in connective tissue
Treatment and prognosis
1. Systemic corticosteroids
2. Other immunosuppressive drugs such as azathioprine and methotrexate are used in
addition to corticosteroids
3. Indirect immunofluorescence
4. Patient may experience periods of remission; never a “cure”; mortality is under 10% and
associated with complications from long-term corticosteroid therapy