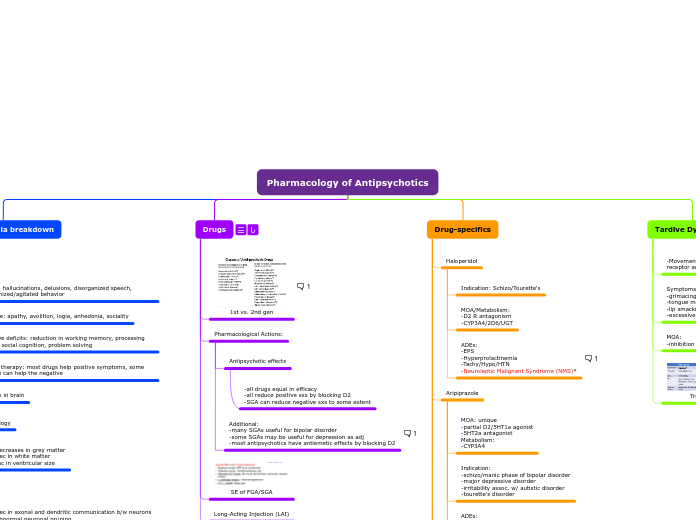
Pharmacology of Antipsychotics
Schizophrenia breakdown
Symptoms
Postive: hallucinations, delusions, disorganized speech, disorganized/agitated behavior
Negative: apathy, avolition, logia, anhedonia, sociality
Cognitive deficits: reduction in working memory, processing speech, social cognition, problem solving
Medical therapy: most drugs help positive symptoms, some 2nd gen can help the negative
Abnormalities in brain
Morphology
-decreases in grey matter
-dec in white matter
-inc in ventricular size
Cell
-dec in axonal and dendritic communication b/w neurons
-abnormal neuronal pruning
Neurotransmitter
Dopamine receptor abnormality
Dopamine hypothesis:
-D2 Dopamine receptor (DR) density is inc in certain regions of the schizo brain
-Antipsychotic drugs block D2 DR - good correlation b/w binding affinity/clinical potency
-dopamine agonists (used to treat PD) produce/exacerbate psychotic eps.
Dopamine pathways in the brain
Nigrostriatal:
-Substantia nigra to basal ganglia, fine
turning of movement
Mesolimbic:
-VTA --> nucleus accumbens
-regulates emotion/motivation and positive sxs
Mesocortical:
-VTA--> cortex
-rregulates attention/cognition and negative sxs
Tuberoinfundibular:
-hypothalamus --> anterior pituitary, controls
prolactin release
Multiple Receptor Systems
Not the whole picture
Drugs
1st vs. 2nd gen
Pharmacological Actions:
Antipsychotic effects
-all drugs equal in efficacy
-all reduce positive sxs by blocking D2
-SGA can reduce negative sxs to some extent
Additional:
-many SGAs useful for bipolar disorder
-some SGAs may be useful for depression as adj
-most antipsychotics have antiemetic effects by blocking D2
SE of FGA/SGA
Long-Acting Injection (LAI)
Use: pts unreliable in taking daily PO meds
-reduced 1st pass metabolism
-"flip-flop" kinetics AKA time to SS is a function of the absorption rate; conc. at SS is a func. of the elimination rate
Drugs:
-Fluphenazine
-Haloperidol
-Paliperidone
-Aripiprazole
-Olanzapine
-Risperidone
Drug-specifics
Haloperidol
Indication: Schizo/Tourette's
MOA/Metabolism:
-D2 R antagonism
-CYP3A4/2D6/UGT
ADEs:
-EPS
-Hyperprolactinemia
-Tachy/Hypo/HTN
-Neuroleptic Malignant Syndrome (NMS)*
Aripiprazole
MOA: unique
-partial D2/5HT1a agonist
-5HT2a antagonist
Metabolism:
-CYP3A4
Indication:
-schizo/manic phase of bipolar disorder
-major depressive disorder
-irritability assoc. w/ autistic disorder
-tourette's disorder
ADEs:
-somnolence/sedation/insomnia
-akathisia (fidgeting, restlessness)
-relatively low risk for weight gain
Similar drugs:
Brexipiprazole/Cariprazine/Lurasidone
Quetiapine and Ziprasidone
Paliperidone and Risperidone
Olanzapine
Indication:
-schizo
-Manic/mixed eps of bipolar disorder
-Together w/ fluoxetine, treat depressive eps of bipolar disorder
PK/MOA:
-Antagonist: D2/5HT
-Metab CYP1A2 (smoking induces CYP1A2)
ADEs:
-Weight gain
-Somnolence/sedation
-EPS
-DRESS
Combo: Olanzapine-Samidorphan
Sami: opioid antagonist
Metabolism:
-CYP1A2/UGT/CYP3A4
ADEs:
-weight gain
-somnolence
-EPS
Clozapine
MOA:
-does NOT block D receptor
-blocks D1/4, a1, 5HT, muscarinic receptors
Indication:
-treat schizo who fail standard antipsychotic drugs (NOT 1ST LINE)
-reduce risk of suicidal behavior
DDI:
-metabolized by CYP1A2/3A4/2D6
ADEs:
-Agranulocytosis/severe neutropenia
-Weight gain (one of the worst)
-somnolence
-orthostatic hypoTN
-constipation/GI hypo motility (may be fatal)
Lumateperone
MOA:
-D2/5HT antagonist
Metabolism:
-CYP3A4/UGT
ADEs:
-Somnolence/dry mouth
Indication: treat schizo
Tardive Dyskinesia
-Movement disorder due to chronic exposure to dopaminergic receptor antagonists (essppp FGA)
Symptoms:
-grimacing
-tongue movements
-lip smacking/puckering/pursing
-excessive eye blink
MOA:
-inhibition of VMAT2 --> dec release of dopamine
Treatment