produced by Mostafa alaa-college of medicin-university of Kerbala
Diabetes mellitus (D.M)
SYNTHETIC AMYLIN ANALOG
Pramlintide
it is an amylin analog that delays gastric emptying, decreases postprandial glucagon secretion, and improves satiety. Pramlintide is administered by subcutaneous injection and should be injected immediately prior to meals. It cannot be mixed with insulin.
Adverse effects: hypoglycemia, nausea, anorexia, and vomiting.
Intensive regimens
involving multiple daily injections (MDI) use long-acting insulin analogs to provide basal or background coverage, and rapid-acting insulin analogs to meet the mealtime requirements. The most sophisticated insulin regimen delivers rapid-acting insulin analogs through a continuous subcutaneous insulin infusion device.
INSULIN PREPARATIONS:
Insulin combinations
: such as 70-percent NPH insulin plus 30-percent regular insulin, 50 percent of each of these, and 75-percent NPL(neutral protamine lispro) insulin plus 25-percent insulin lispro
C.Long-acting insulin preparations:
2.Insulin detemir
has a fatty-acid side chain. This addition enhances association to albumin. Slow dissociation from albumin results in long-acting properties.
1.Insulin glargine
it precipitates at the injection leading to prolongation of its action. It is slower in onset than NPH insulin and has a flat, prolonged hypoglycemic effect with no peak. It must be given subcutaneously
B.Intermediate-acting insulin
Neutral protamine Hagedorn (NPH or called insulin isophane) insulin is a suspension of crystalline zinc insulin combined with polypeptide protamine (to delayed insulin absorption). NPH insulin has an onset of approximately 2–5 hours and duration of 4–12 hours
It should only be given subcutaneously (never IV) and is useful in treating all forms of diabetes except diabetic ketoacidosis and emergency hyperglycemia
A.Rapid-acting (with very fast onset and short duration insulin lispro, insulin aspart, and insulin glulisine.) and short-acting (with rapid onset regular insulin) insulin preparations
Regular insulin is short-acting, soluble, crystalline zinc insulin which rapidly lowers blood glucose. Its effect appears within 30 minutes and peaks between 2 and 3 hours after subcutaneous injection and generally lasts 5–8 hours
Insulin lispro differs from regular insulin in that lysine and proline at positions 28 and 29 in the B chain are reversed. This results in more rapid absorption after subcutaneous injection than is seen with regular insulin. The rapid-acting insulins permit more physiologic prandial insulin replacement because their rapid onset and early peak action more closely mimic normal endogenous prandial insulin secretion
Adverse reactions:
4-Development of resistance.
3-Allergic reactions.
2-Weight gain, lipodystrophy.
1-Hypoglycemia
Sources of insulin
Human insulin is produced by recombinant DNA technology using special strains of Escherichia coli or yeast. Insulin is inactivated by insulin-degrading enzyme (also called insulin protease), which is found mainly in the liver and kidney.
Insulin administration
4-Continuous subcutaneous insulin infusion (insulin pump).
3-Regular insulin is injected intravenously in hyperglycemic emergency.
2-Subcutaneous
1-orally not given because will degraded
Action of insulin
4-Intracellular accumulation of potassium and phosphate
which is linked to glucose transport in some tissues.
3-Effect on adipose tissue
Increased triglyceride storage, induction of Lipoprotein lipase.
2-Effect on muscle
Increased protein synthesis, Increases amino acid transport
1-On the liver
: Inhibits glycogenolysis, Inhibits conversion of fatty acids and amino acids to keto acids, Promotes glucose storage as glycogen and Increases triglyceride synthesis and very-low-density lipoprotein formation
note about insulin
value
normal = 5–15 U/mL
peak rise to 60–90 U/mL
The half-life of circulating insulin is 3–5 minutes
pharmacokinetiks
The liver (60%) and kidney (35–40%) are the two main organs that remove insulin from the circulation but this ratio is reversed if insulin is given exogenously.
Inhibitory signals
hronically elevated glucose and fatty acid
somatostatin
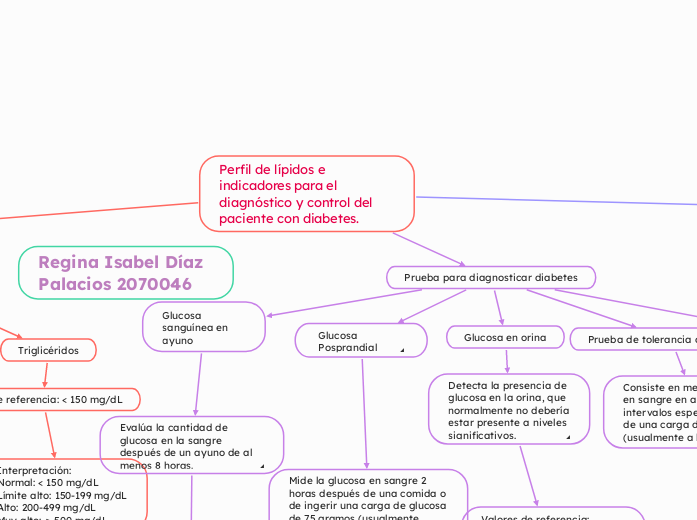
Definition
Insulin stimulants
vagal activity
hormones
cholecystokinin
glucagon
glucose-dependent insulinotropic polypeptide (GIP)
glucagon-like polypeptide-1 (GLP-1)
amino acids (e.g., leucine, arginine)
sugars
insulin work
NORMAL INSULIN