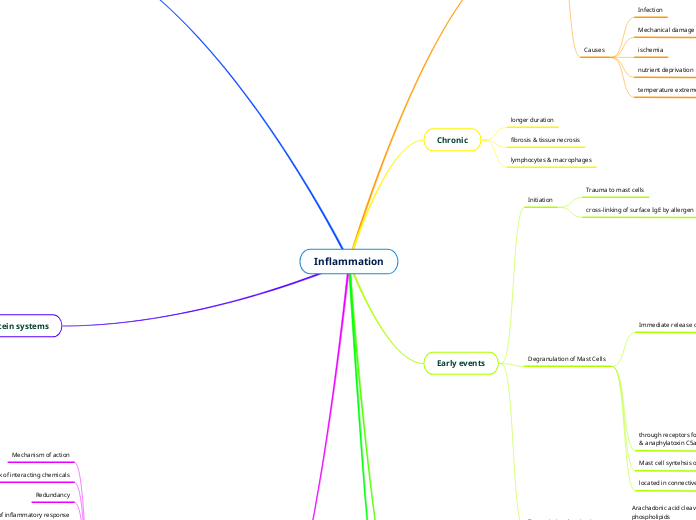
Inflammation
Chemical Mediators of Inflammation
Cellular Mediators
histamine, serotonin, lysosomal enzymes, prostaglandins,
leukotrienes, PAF, oxygen species, nitric oxide, cytokines
Cytokines
nitric oxide
potent vasodilator, reduces platelet
modulates inflammatory resonse locally
eicosanoids
can mediate virtually every step of inflammation
converted membrane lipid, short range, short 1/2 life
aspirin/NSAIDS block conversion of AA
into thromboxanes, prostacyclins & prostaglandins
Interferons
IFNa, IFNb, IFNy
protect against viral infections
Platelet Activating Factor
leukocyte adhesion & chemotaxis
bronchodilation & vasoconstriction,vasodilation & vascular permebility
phospholipid, aggregate platelets
IL1 & TNF
Master cytokines
released by & act on nearby cells
short 1/2 life
allows self killing of immune response
amplification & maintenance of inflammatory response
Redundancy
Network of interacting chemicals
Mechanism of action
Plasma protein systems
complement system
C5a
activates lipoxygenase pathway; increases leukocyte
C3a & C5a: anaphylatoxins
histamine & lysosomal enzyme release
alternate pathway
common pathway
classical pathway
coagulation system
plasmin is important in lysing fibrin clots
thrombin converts fibrinogen to fibrin
plasma protein
kinin system
bradykinin
activated by hageman factor (12a)
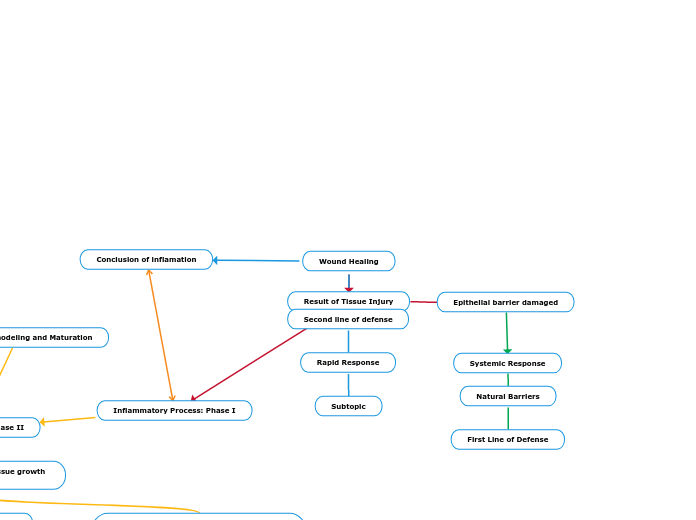
Acute
outcomes
Resolution
immune response - chronic inflammation
Repair
regeneration, fibrosis, scar
<6 weeks
edema
neutrophils
Resolution of acute inflamation
arachadonic acid metabolism
lipoxin & resolvins generated that have anti-inflammator
Eradication of offending agent
discontinuation of inflammatory response
platelet derived GF, transforming GF B (chemokines)
Phases
Cellular
Natural Killer cells
Platelets
results in degranulation
kill by releasing granules of protein
recognize & eliminate cells w/ viruses
Phagocytosis
Monocytes, Macrophages & eosinophils
Engulfment
Microbial Killing
Macrophage activating factor
Opsonization
Recognition
Vascular
fluid loss
concentration of RBC
slowed blood flow
WBC adherence & migration
chemotaxis
Increased capillary pressure
Exudate
Vasodilation
Increased blood vessel permeability
due to endothelial contractoin
allow plasma proteins & cells in
swelling
hestamine, serotonin, bradykinin, C3a & 5a, leukotrienes, PAF
blood pooling
redness & warmth
Increased blood flow
Hemostasis (bleeding stops)
cell adherence
transmigration of phagocytic cells
elimination of insult
histamine, prostaglandins, NO
Transient vasoconstriction
caused by initial trauma & low histamine levels
Main topic
Early events
Transcriptional activation
leukotrienes & chemokines
Arachadonic acid cleaved from mast cell membrane phospholipids
Degranulation of Mast Cells
located in connective tissue/adjacent to bloodvessels
Mast cell syntehsis of mediators reinforces
through receptors for IgE, IgG, histamine, bacterial products
& anaphylatoxin C5a, physical injury, cold & heat
Immediate release of chem mediators
platelet activating factor
histamine & serotonin
eosinophil chemotactic factor
eosinophils attracted
neutrophil chemotactic factor
neutrophils attracted to site
phagocytosis
histamine
histamine receptors
2: antiinflammatory
1: proinflammatory
dilation & increased permeability
exudate
cytokines
TNF a
incrased permeability & leukocyte emigration
IL-4
B cell proliferation & antibody production
tryptase
heparin
Initiation
cross-linking of surface IgE by allergen
Trauma to mast cells
Chronic
lymphocytes & macrophages
fibrosis & tissue necrosis
longer duration