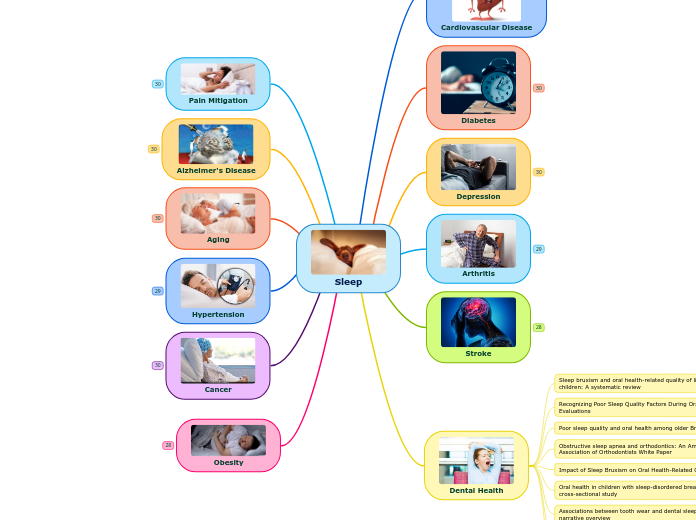
Sleep
Obesity
Does stress influence sleep patterns, food intake, weight gain, abdominal obesity and weight loss interventions and vice versa?
Abstract
Decades of research have reported only weak associations between the intakes of specific foods or drinks and weight gain and obesity. Randomized controlled dietary intervention trials have only shown very modest effects of changes in nutrient intake and diet composition on body weight in obese subjects. This review summarizes the scientific evidence on the role mental stress (either in or not in association with impaired sleep) may play in poor sleep, enhanced appetite, cravings and decreased motivation for physical activity. All these factors contribute to weight gain and obesity, possibly via decreasing the efficacy of weight loss interventions. We also review evidence for the role that lifestyle and stress management may play in achieving weight loss in stress-vulnerable individuals with overweight.
Sleep influences on obesity, insulin resistance, and risk of type 2 diabetes
Abstract
A large body of epidemiologic evidence has linked insufficient sleep duration and quality to the risk of obesity, insulin resistance and type 2 diabetes. To address putative causal mechanisms, this review focuses on laboratory interventions involving several nights of experimental sleep restriction, fragmentation or extension and examining metabolically relevant outcomes. Sleep restriction has been consistently shown to increase hunger, appetite and food intake, with the increase in caloric intake in excess of the energy requirements of extended wakefulness. Findings regarding decreases in hormones promoting satiety or increases in hormones promoting hunger have been less consistent, possibly because of confounding effects of changes in adiposity when energy intake was not controlled and sampling protocols that did not cover the entire 24-h cycle. Imaging studies revealed alterations in neuronal activity of brain regions involved in food reward. An adverse impact of experimental sleep restriction on insulin resistance, leading to reduced glucose tolerance and increased diabetes risk, has been well-documented. There is limited evidence indicating that sleep fragmentation without reduction in sleep duration also results in a reduction in insulin sensitivity. The adverse metabolic outcomes of sleep disturbances appear to involve multiple mechanistic pathways acting in concert. Emerging evidence supports the benefits of behavioral, but not pharmacological, sleep extension on appetite and glucose metabolism. Further research should focus on the feasibility and efficacy of strategies to optimize sleep duration and quality on obesity and diabetes risk in at-risk populations as well as those with established diseases. Further work is needed to identify mechanistic pathways.
Sleep Duration and Obesity in Children and Adolescents
Abstract
Increased rates of obesity internationally have drawn significant attention. In particular, researchers and practitioners are seeking new information about risk factors for obesity that could be areas for preventive interventions. Given that obesity rates in children and adolescents are increasing worldwide, particular attention to child and adolescent obesity is needed. A large, and growing, body of research indicates that inadequate sleep duration is linked to obesity. The current article reviews the extant literature concerning sleep duration and obesity in children and adolescents by reviewing current theories of obesity as well as available literature specifically evaluating the relationship of obesity and sleep in children and adolescents, including epidemiologic, experimental and intervention research. Overall, our literature review concludes that the relationship between shortened sleep and increased risk for obesity has research support internationally, including in the few Canadian articles available that are discussed in our review.
Sleep quality and obesity in young subjects: a meta-analysis
Abstract
Objectives: To assess the effect of poor sleep quality on Overweight/Obesity (Ow/Ob) in young subjects, and explore if this association is independent of sleep duration.
Methods: Pubmed, EMBASE, and MEDLINE databases were searched for papers on sleep quality and overweight/obesity, focusing on children, adolescents, and young adults. Studies based on subjects with medical/psychological problems or published in languages other than English were excluded. Quality effects model was used to pool studies for meta-analysis.
Results: Findings from the systematic review suggest a link between poor sleep quality and Ow/Ob in young subjects. Pooled estimate (from 26,553 subjects) suggest a role of inadequate sleep (including both short duration and poor quality) in Ow/Ob (OR: 1.27 95% CI: 1.05-1.53). Sub-group-analyses suggest considerably higher odds of Ow/Ob (OR = 1.46, 95% CI: 1.24-1.72) in young subjects with poor sleep quality (independent of duration).
Conclusions: Poor sleep quality seems to be associated with Ow/Ob, and some studies indicate this association to be independent of duration. Therefore, considering only sleep duration might not help in disentangling sleep-obesity association. However, this review is mostly composed of cross-sectional studies. Therefore, a causal link or the stability of the sleep quality and Ow/Ob association could not be established.
The epidemiology of sleep and obesity
Abstract
Sleep is a state of consciousness that is preserved across animal species whose exact function is not yet clear but which has a vital impact on health and well-being. Epidemiological evidence suggests sleep duration in both children and adults has been decreasing over the past half-century, while at the same time rates of overweight and obesity have been increasing. Short sleep duration along with other dimensions of poor sleep has been associated with obesity both cross-sectionally and longitudinally. These data suggest a potential causal relationship between poor sleep and greater rates of weight gain that may be related to effects of sleep on dietary intake or physical activity. However, there is also potential for reverse causation as obesity leads to many co-morbidities including sleep apnea that can disrupt sleep. Medium and long term interventional studies are needed to evaluate the potential for healthy sleep interventions to help combat the epidemic of obesity.
Sleep-obesity relation: underlying mechanisms and consequences for treatment
Abstract
Short sleep duration has been associated with obesity in numerous epidemiological studies. However, such association studies cannot establish evidence of causality. Clinical intervention studies, on the other hand, can provide information on a causal effect of sleep duration on markers of weight gain: energy intake and energy expenditure. Herein is an overview of the science related to the impact of sleep restriction, in the context of clinical intervention studies, on energy intake, energy expenditure and body weight. Additionally, studies that evaluate the impact of sleep restriction on weight loss and the impact of sleep extension on appetite are discussed. Information to date suggests that weight management is hindered when attempted in the context of sleep restriction, and the public should be made aware of the negative consequences of sleep restriction for weight regulation.
Obesity and sleep: a growing concern
Abstract
Purpose of review: The 'obesity epidemic' is a growing concern globally, and obesity trends are projected to continue increasing in both prevalence and overall mean BMI. Cardiovascular and metabolic comorbidities have historically been well described; however, obesity-related respiratory disease is now increasingly prevalent, in particular, sleep disordered breathing. The surge in clinically significant obstructive sleep apnoea and obesity hypoventilation syndrome is associated with increased cardiopulmonary morbidity, quality-of-life impairment, and a potential rise in the frequency of road traffic accidents.
Recent findings: We discuss recent trends in obesity and obesity-related sleep disordered breathing. We also discuss recently published international guidelines regarding the diagnosis and management of sleep disordered breathing, and in particular, the role of weight management interventions, such as bariatric surgery, in this area. We discuss possible approaches to meet the growing demand for sleep assessment and management in the future.
Summary: Obesity-related respiratory disease reflects an increasing proportion of patients in both inpatient and outpatient settings. It is important to recognize the impact of obesity on pulmonary physiology in order to appropriately care for this population, as well as plan for the future.
Chronobesity: role of the circadian system in the obesity epidemic
Abstract
Although obesity is considered to result from an imbalance between energy uptake and energy expenditure, the strategy of dietary changes and physical exercise has failed to tackle the global obesity epidemic. In search of alternative and more adequate treatment options, research has aimed at further unravelling the mechanisms underlying this excessive weight gain. While numerous studies are focusing on the neuroendocrine alterations that occur after bariatric Roux-en-Y gastric bypass surgery, an increasing amount of chronobiological studies have started to raise awareness concerning the pivotal role of the circadian system in the development and exacerbation of obesity. This internal timekeeping mechanism rhythmically regulates metabolic and physiological processes in order to meet the fluctuating demands in energy use and supply throughout the 24-h day. This review elaborates on the extensive bidirectional interaction between the circadian system and metabolism and explains how disruption of body clocks by means of shift work, frequent time zone travelling or non-stop consumption of calorie-dense foods can evoke detrimental metabolic alterations that contribute to obesity. Altering the body's circadian rhythms by means of time-related dietary approaches (chrononutrition) or pharmacological substances (chronobiotics) may therefore represent a novel and interesting way to prevent or treat obesity and associated comorbidities.
Potential circadian and circannual rhythm contributions to the obesity epidemic in elementary school age children
Abstract
Children gain weight at an accelerated rate during summer, contributing to increases in the prevalence of overweight and obesity in elementary-school children (i.e., approximately 5 to 11 years old in the US). Int J Behav Nutr Phys Act 14:100, 2017 explained these changes with the “Structured Days Hypothesis” suggesting that environmental changes in structure between the school year and the summer months result in behavioral changes that ultimately lead to accelerated weight gain. The present article explores an alternative explanation, the circadian clock, including the effects of circannual changes and social demands (i.e., social timing resulting from societal demands such as school or work schedules), and implications for seasonal patterns of weight gain. We provide a model for understanding the role circadian and circannual rhythms may play in the development of child obesity, a framework for examining the intersection of behavioral and biological causes of obesity, and encouragement for future research into bio-behavioral causes of obesity in children.
Circadian Rhythms in Diet-Induced Obesity
Abstract
The biological clocks of the circadian timing system coordinate cellular and physiological processes and synchronizes these with daily cycles, feeding patterns also regulates circadian clocks. The clock genes and adipocytokines show circadian rhythmicity. Dysfunction of these genes are involved in the alteration of these adipokines during the development of obesity. Food availability promotes the stimuli associated with food intake which is a circadian oscillator outside of the suprachiasmatic nucleus (SCN). Its circadian rhythm is arranged with the predictable daily mealtimes. Food anticipatory activity is mediated by a self-sustained circadian timing and its principal component is food entrained oscillator. However, the hypothalamus has a crucial role in the regulation of energy balance rather than food intake. Fatty acids or their metabolites can modulate neuronal activity by brain nutrient-sensing neurons involved in the regulation of energy and glucose homeostasis. The timing of three-meal schedules indicates close association with the plasma levels of insulin and preceding food availability. Desynchronization between the central and peripheral clocks by altered timing of food intake and diet composition can lead to uncoupling of peripheral clocks from the central pacemaker and to the development of metabolic disorders. Metabolic dysfunction is associated with circadian disturbances at both central and peripheral levels and, eventual disruption of circadian clock functioning can lead to obesity. While CLOCK expression levels are increased with high fat diet-induced obesity, peroxisome proliferator-activated receptor (PPAR) alpha increases the transcriptional level of brain and muscle ARNT-like 1 (BMAL1) in obese subjects. Consequently, disruption of clock genes results in dyslipidemia, insulin resistance and obesity. Modifying the time of feeding alone can greatly affect body weight. Changes in the circadian clock are associated with temporal alterations in feeding behavior and increased weight gain. Thus, shift work is associated with increased risk for obesity, diabetes and cardio-vascular diseases as a result of unusual eating time and disruption of circadian rhythm.
Links between the circadian rhythm, obesity and the microbiome
Summary Obesity is linked to a wide range of serious illnesses. In addition to the important impact on the health of the individual, obesity also has a substantial impact on the economy. Disruption of physiological day-night cycles could contribute to the increased incidence of obesity. According to the American National Sleep Federation, the percentage of the people who reported a sleep duration of six hours or less increased from 12 to 37 % over ten years. Insufficient sleep leads not only to an increase of the total calorie intake but changes the meal preference in favor of palatable foods and meals with high carbohydrate content. A decrease of leptin and increase of ghrelin levels caused by sleep deficiency can also play a role. In addition to the higher caloric intake, the timing of food consumption should be taken into account. The same meal eaten during the night versus the day is associated with increased postprandial glucose and triglyceride levels. The gut microbiome has also been recently understood as an endocrine system, with links between the gut microbiome and circadian rhythm changes possibly influencing increased obesity.
Sleep quality is inversely related to body mass index among university students
SUMMARY
OBJECTIVE:
The purpose of this study was to investigate the prevalence of overweight and obesity and its association with sleep quality in university students from the Anhui province in China.
METHODS:
A cross-sectional study was conducted in China with 1328 participants. The prevalence of underweight and obesity in university students was estimated according to the reference working group on obesity in China. The sleep quality was evaluated using the standard PSQI (Pittsburgh Sleep Quality Index).
RESULTS:
This study included 470 male and 858 female students from a university in Anhui; 4.4% of the females and 17.7% of the males were overweight or obese. The prevalence of obesity in males was significantly higher than in females, and the prevalence of obesity in higher years was greater than in other years (p<0.05). In general, the mean score for sleep quality was 4.91±2.67; 36.5% of male and 39.1% of female students had poor sleep quality (PSQI score >5). Among the seven components of sleep quality, sleep duration and the use of sleep medication showed significant differences between male and female students and different years (p<0.05). An obvious correlation was found between sleep quality and body mass index (BMI)(p<0.000) in females who took hypnotic drugs.
CONCLUSION:
This study suggests that the sleep quality of females is probably associated with their BMI. College students are a special group of young adults whose cause of poor sleeping quality and BMI may be significant to study, so the health status of university students can be improved.
[Poor sleep quality and inadequate sleep duration related to obesity in two Roma subgroups in Transylvania]
Abstract in
Introduction: Short sleep duration and poor sleep quality may be associated with weight gain; this association has not yet been studied in Roma (Gipsy) population. Aim: Our aim was to study sleep patterns in two adult Roma subgroups (the wealthy Gabor and the poor Lovari Roma), compared to the majority of Hungarian population, in relation to obesity, knowing that Roma population has specific socio-cultural characteristics, with a rapidly changing lifestyle. Method: A population-based cross-sectional survey was conducted in a rural region in Transylvania, where the above groups are cohabiting. The groups were age- and gender-matched. Results: Sleep duration was 7.18 ± 1.6 hours in the Gabor Roma, 7.67 ± 1.5 hours in the Lovari Roma and 7.37 ± 1.5 hours in the non-Roma group. In average, 70% of them had enough sleep (≥7 hours). 38.6% of Gabor Roma, 27.1% of Lovari Roma and 23.5% of non-Roma had poor-quality sleep (p = 0.05). Gabor Roma had significantly higher body mass index (31.1 ± 4.6 versus 27.4 ± 5.2 and 28.66 ± 5.7 kg/m2, p = 0.004), and this correlated inversely with sleep duration (F = 14.85, p<0.000). Conclusion: Gabor Roma had significantly higher percentage of poor-quality sleep. Sleep duration and sleep quality were linked with obesity, mainly in the Roma population. Orv Hetil. 2019; 160(32): 1279-1283.
Sleep patterns, diet quality and energy balance
Abstract
There is increasing evidence showing that sleep has an influence on eating behaviors. Short sleep duration, poor sleep quality, and later bedtimes are all associated with increased food intake, poor diet quality, and excess body weight. Insufficient sleep seems to facilitate the ingestion of calories when exposed to the modern obesogenic environment of readily accessible food. Lack of sleep has been shown to increase snacking, the number of meals consumed per day, and the preference for energy-rich foods. Proposed mechanisms by which insufficient sleep may increase caloric consumption include: (1) more time and opportunities for eating, (2) psychological distress, (3) greater sensitivity to food reward, (4) disinhibited eating, (5) more energy needed to sustain extended wakefulness, and (6) changes in appetite hormones. Globally, excess energy intake associated with not getting adequate sleep seems to be preferentially driven by hedonic rather than homeostatic factors. Moreover, the consumption of certain types of foods which impact the availability of tryptophan as well as the synthesis of serotonin and melatonin may aid in promoting sleep. In summary, multiple connections exist between sleep patterns, eating behavior and energy balance. Sleep should not be overlooked in obesity research and should be included as part of the lifestyle package that traditionally has focused on diet and physical activity.
Is shift work associated with a higher risk of overweight or obesity? A systematic review of observational studies with meta-analysis
Abstract
Background: An increasing number of original studies suggest that exposure to shift work could be associated with the risk of overweight and obesity, but the results remain conflicted and inconclusive. This study aimed to quantitatively synthesize available epidemiological evidence on the association between shift work and the risk of overweight and obesity by a meta-analysis.
Methods: The authors searched PubMed, Embase and the reference lists of all included studies up to April 2017, with a verification search in December 2017. Inclusion criteria were original studies that reported odds ratios, relative risks or hazard ratios (ORs, RRs or HRs, respectively) of at least one outcome of overweight or obesity. Summary risk estimates were calculated by random-effect models.
Results: Twenty-six studies (7 cohort studies, 18 cross-sectional studies and 1 case– control study) involving 311 334 participants were identified. Among these studies, the cut-off points of overweight and obesity varied greatly, so the heterogeneity was substantial; however, the results were stable. Shift work was found to be positively associated with the risk of overweight [RR: 1.25; 95% confidence interval (95% CI): 1.08–1.44] and obesity (RR: 1.17; 95% CI: 1.12–1.22).
Conclusions: Individuals involved in shift work are more likely to become overweight or obese. Appropriate preventive interventions in the organization of shift schedules according to ergonomic criteria would allow shift workers to avoid potential health impairment.
Night shift work exposure profile and obesity: Baseline results from a Chinese night shift worker cohort
Abstract
Aims: This study aimed to evaluate the associations between types of night shift work and different indices of obesity using the baseline information from a prospective cohort study of night shift workers in China.
Methods: A total of 3,871 workers from five companies were recruited from the baseline survey. A structured self-administered questionnaire was employed to collect the participants' demographic information, lifetime working history, and lifestyle habits. Participants were grouped into rotating, permanent and irregular night shift work groups. Anthropometric parameters were assessed by healthcare professionals. Multiple logistic regression models were used to evaluate the associations between night shift work and different indices of obesity.
Results: Night shift workers had increased risk of overweight and obesity, and odds ratios (ORs) were 1.17 (95% CI, 0.97-1.41) and 1.27 (95% CI, 0.74-2.18), respectively. Abdominal obesity had a significant but marginal association with night shift work (OR = 1.20, 95% CI, 1.01-1.43). A positive gradient between the number of years of night shift work and overweight or abdominal obesity was observed. Permanent night shift work showed the highest odds of being overweight (OR = 3.94, 95% CI, 1.40-11.03) and having increased abdominal obesity (OR = 3.34, 95% CI, 1.19-9.37). Irregular night shift work was also significantly associated with overweight (OR = 1.56, 95% CI, 1.13-2.14), but its association with abdominal obesity was borderline (OR = 1.26, 95% CI, 0.94-1.69). By contrast, the association between rotating night shift work and these parameters was not significant.
Conclusion: Permanent and irregular night shift work were more likely to be associated with overweight or abdominal obesity than rotating night shift work. These associations need to be verified in prospective cohort studies.
Meta-analysis on shift work and risks of specific obesity types
SummaryAims
This systematic review and meta‐analysis evaluated the associations between shift work patterns and risks of specific types of obesity.
Methods
PubMed was searched until March 2017 for observational studies that examined the relationships between shift work patterns and obesity. Odds ratio for obesity was extracted using a fixed‐effects or random‐effects model. Subgroup meta‐analyses were carried out for study design, specific obesity types and characteristics of shift work pattern.
Results
A total of 28 studies were included in this meta‐analysis. The overall odds ratio of night shift work was 1.23 (95% confidence interval = 1.17–1.29) for risk of obesity/overweight. Cross‐sectional studies showed a higher risk of 1.26 than those with the cohort design (risk ratio = 1.10). Shift workers had a higher frequency of developing abdominal obesity (odds ratio = 1.35) than other obesity types. Permanent night workers demonstrated a 29% higher risk than rotating shift workers (odds ratio 1.43 vs. 1.14).
Conclusion
This meta‐analysis confirmed the risks of night shift work for the development of overweight and obesity with a potential gradient association suggested, especially for abdominal obesity. Modification of working schedules is recommended, particularly for prolonged permanent night work. More accurate and detailed measurements on shift work patterns should be conducted in future research.
Shift work, overweight and obesity in health professionals: a systematic review and meta-analysis
Abstract
Shift work may have significant repercussions on the health of the worker, and has been linked to unhealthy lifestyles. The aim was to conduct a systematic review of the literature and to assess the relationship between night shift and overweight and obesity among health professionals. A literature search was performed using PubMed and Scopus. The keywords used included: "shift work", "night work", "obesity", "overweight", "nurses" "doctors" "physicians". The whole process of revision followed the PRISMA Statement. Two researchers independently, reviewed the search results, assessed the quality and extracted data. Six transversal and a cohort studies were found for the population of nurses. The meta-analysis did not produce significant results on the prevalence of obesity in the population of nurses (OR: 1.00; 95% CI 0.66-1.50). More high-quality studies and including a larger number of participants should be conducted, in order to assess whether there is real cause-effect relationship between the exposure to night shifts and weight gain as well as of obesity.
Non-invasive ventilation in obesity hypoventilation syndrome without severe obstructive sleep apnoea
Abstract
Background Non-invasive ventilation (NIV) is an effective form of treatment in patients with obesity hypoventilation syndrome (OHS) who have concomitant severe obstructive sleep apnoea (OSA). However, there is a paucity of evidence on the efficacy of NIV in patients with OHS without severe OSA. We performed a multicentre randomised clinical trial to determine the comparative efficacy of NIV versus lifestyle modification (control group) using daytime arterial carbon dioxide tension (PaCO2) as the main outcome measure.
Methods Between May 2009 and December 2014 we sequentially screened patients with OHS without severe OSA. Participants were randomised to NIV versus lifestyle modification and were followed for 2 months. Arterial blood gas parameters, clinical symptoms, health-related quality of life assessments, polysomnography, spirometry, 6-min walk distance test, blood pressure measurements and healthcare resource utilisation were evaluated. Statistical analysis was performed using intention-to-treat analysis.
Results A total of 365 patients were screened of whom 58 were excluded. Severe OSA was present in 221 and the remaining 86 patients without severe OSA were randomised. NIV led to a significantly larger improvement in PaCO2 of −6 (95% CI −7.7 to −4.2) mm Hg versus −2.8 (95% CI −4.3 to −1.3) mm Hg, (p<0.001) and serum bicarbonate of −3.4 (95% CI −4.5 to −2.3) versus −1 (95% CI −1.7 to −0.2 95% CI) mmol/L (p<0.001). PaCO2 change adjusted for NIV compliance did not further improve the inter-group statistical significance. Sleepiness, some health-related quality of life assessments and polysomnographic parameters improved significantly more with NIV than with lifestyle modification. Additionally, there was a tendency towards lower healthcare resource utilisation in the NIV group.
Conclusions NIV is more effective than lifestyle modification in improving daytime PaCO2, sleepiness and polysomnographic parameters. Long-term prospective studies are necessary to determine whether NIV reduces healthcare resource utilisation, cardiovascular events and mortality.
Obesity Hypoventilation Syndrome
Abstract
Obesity hypoventilation syndrome (OHS) is defined as a combination of obesity (body mass index ≥30 kg·m−2), daytime hypercapnia (arterial carbon dioxide tension ≥45 mmHg) and sleep disordered breathing, after ruling out other disorders that may cause alveolar hypoventilation. OHS prevalence has been estimated to be ∼0.4% of the adult population. OHS is typically diagnosed during an episode of acute-on-chronic hypercapnic respiratory failure or when symptoms lead to pulmonary or sleep consultation in stable conditions. The diagnosis is firmly established after arterial blood gases and a sleep study. The presence of daytime hypercapnia is explained by several co-existing mechanisms such as obesity-related changes in the respiratory system, alterations in respiratory drive and breathing abnormalities during sleep. The most frequent comorbidities are metabolic and cardiovascular, mainly heart failure, coronary disease and pulmonary hypertension. Both continuous positive airway pressure (CPAP) and noninvasive ventilation (NIV) improve clinical symptoms, quality of life, gas exchange, and sleep disordered breathing. CPAP is considered the first-line treatment modality for OHS phenotype with concomitant severe obstructive sleep apnoea, whereas NIV is preferred in the minority of OHS patients with hypoventilation during sleep with no or milder forms of obstructive sleep apnoea (approximately <30% of OHS patients). Acute-on-chronic hypercapnic respiratory failure is habitually treated with NIV. Appropriate management of comorbidities including medications and rehabilitation programmes are key issues for improving prognosis.
Sleep and eating in childhood: a potential behavioral mechanism underlying the relationship between poor sleep and obesity
Abstract
Objective: The goal of our study was to examine the associations between sleep and eating behaviors. Specifically, we examined associations between sleep duration and continuity with behaviors that promote eating regardless of true physiologic hunger state including emotional (food intake in response to emotional distress) external (eating in response to the sight or smell of food), and restrained eating (a paradoxical behavior; food intake is initially reduced to lose or maintain body weight, but followed by increased consumption and binge eating).
Participants: Fifty-six children (29 boys; 27 girls) ages 5 to 12 years participated in the study. Mean age was 7.7±1.9 years, and average body mass index (BMI) was within the healthy range (17.8±4.3 kg/m(2)).
Methods: Sleep duration, continuity and schedule were assessed using actigraphy and self-reports. The Child Dutch Eating Behavior Questionnaire-modified version (DEBQ-M) was used to examine levels of emotional, external and restrained eating in the children.
Results: Associations between the sleep and eating behaviors were examined using partial correlations and multiple regression analyses. External eating score was negatively associated with sleep duration; emotional eating score was associated with lower levels of sleep continuity; and restrained eating score were associated with a later sleep start and later bedtime.
Conclusions: Short sleep duration and poor sleep continuity were associated with higher levels of eating behaviors shown to be associated with increased food intake. Therefore, sleep loss may be associated with diminished self-regulation of appetite in children, increasing the risk for overeating and obesity.
Caffeine and Screen Time in Adolescence: Associations with Short Sleep and Obesity
Abstract
Objective: To investigate the associations between sleep duration and obesity incidence and risk factors among pre-adolescents and adolescents.
Design: Cross-sectional study of a community based cohort
Setting: The Tucson Children's Assessment of Sleep Apnea follow-up study (TuCASA) cohort.
Participants: 319 Caucasian and Hispanics between 10-17 years.
Main outcome: Parent-reported sleep duration and BMI z-score.
Outcome measures: Surveys of electronic screen time, dietary and caffeine intake, exercise and sleep habits by parents, and anthropometric measures.
Results: Parent-reported total sleep time (TST) was inversely associated with BMI z-score, but not significantly correlated with any of the examined nutritional variables or exercise components. Hispanic ethnicity was associated with significantly lower parent-reported TST and higher BMI z-score. Parent-reported TST was inversely related to electronic screen time and caffeine use, but these findings were differentially related to age. Caffeine consumption was associated with decreasing parent-reported TST primarily in older adolescents. Electronic screen time was associated with lower parent-reported TST in younger adolescents.
Conclusions: Hispanic ethnicity and parental reports of TST were found to be the most closely associated with BMI z-score. Decreased TST and increased caffeine intake and screen time may result in higher obesity risk in the adolescent population.
Sleep disorders, obesity, and aging: The role of orexin
Abstract
The hypothalamic neuropeptides orexin A and B (hypocretin 1 and 2) are important homeostatic mediators of central control of energy metabolism and maintenance of sleep/wake states. Dysregulation or loss of orexin signaling has been linked to narcolepsy, obesity, and age-related disorders. In this review, we present an overview of our current understanding of orexin function, focusing on sleep disorders, energy balance, and aging, in both rodents and humans. We first discuss animal models used in studies of obesity and sleep, including loss of function using transgenic or viral-mediated approaches, gain of function models using exogenous delivery of orexin receptor agonist, and naturally-occurring models in which orexin responsiveness varies by individual. We next explore rodent models of orexin in aging, presenting evidence that orexin loss contributes to age-related changes in sleep and energy balance. In the next section, we focus on clinical importance of orexin in human obesity, sleep, and aging. We include discussion of orexin loss in narcolepsy and potential importance of orexin in insomnia, correlations between animal and human studies of age-related decline, and evidence for orexin involvement in age-related changes in cognitive performance. Finally, we present a summary of recent studies of orexin in neurodegenerative disease. We conclude that orexin acts as an integrative homeostatic signal influencing numerous brain regions, and that this pivotal role results in potential dysregulation of multiple physiological processes when orexin signaling is disrupted or lost.
Does inadequate sleep play a role in vulnerability to obesity?
Abstract
The prevalence of obesity is increasing rapidly worldwide, which is cause for concern because obesity increases the risk of cardiovascular disease and diabetes, reduces life expectancy, and impairs quality of life. A better understanding of the risk factors for obesity is therefore a critical global health concern, and human biologists can play an important role in identifying these risk factors in various populations. The objective of this review is to present the evidence that inadequate sleep may be a novel risk factor associated with increased vulnerability to obesity and associated cardiometabolic disease. Experimental studies have found that short-term sleep restriction is associated with impaired glucose metabolism, dysregulation of appetite, and increased blood pressure. Observational studies have observed cross-sectional associations between short sleep duration (generally <6 h per night) and increased body mass index or obesity, prevalent diabetes, and prevalent hypertension. Some studies also reported an association between self-reported long sleep duration (generally >8 h per night) and cardiometabolic disease. A few prospective studies have found a significant increased risk of weight gain, incident diabetes, and incident hypertension associated with inadequate sleep. Given the potential link between inadequate sleep and obesity, a critical next step is to identify the social, cultural, and environmental determinants of sleep, which would help to identify vulnerable populations. Future human biology research should consider variation in sleep characteristics among different populations and determine whether the associations between sleep and obesity observed in Western populations persist elsewhere.
Association between sleep disorders, obesity, and exercise: a review
Abstract
Decreased sleep duration and quality is associated with an increase in body weight and adiposity. Insomnia, obstructive sleep apnea, and restless legs syndrome are three of the most prevalent types of sleep disorder that lead to an increased risk for numerous chronic health conditions. Various studies have examined the impact of these sleep disorders on obesity, and are an important link in understanding the relationship between sleep disorders and chronic disease. Physical activity and exercise are important prognostic tools in obesity and chronic disease, and numerous studies have explored the relationship between obesity, sleep disorders, and exercise. As such, this review will examine the relationship between sleep disorders and obesity. In addition, how sleep disorders may impact the exercise response and how exercise may impact patient outcomes with regard to sleep disorders will also be reviewed.
Chapter 13 - Sleep and Obesity in Children and Adolescents
Synopsis
The purpose of the present review is to provide a comprehensive update of current epidemiological studies that have assessed the association between sleep and obesity risk. Data from 29 studies conducted in 16 countries suggest that short sleep is associated with an increased risk for being or becoming overweight/obese or having increased body fat. Late bedtimes were also found to be a risk factor for overweight/obesity. Findings also suggest that changes in eating pathways may lead to increased body fat. Future experimental studies are needed to enhance our understanding of the underlying mechanisms through which sleep may play a role in the development and maintenance of childhood obesity.
Sleep and obesity
Abstract
Purpose of review
This review summarizes the most recent evidence linking decreased sleep duration and poor sleep quality to obesity, focusing upon studies in adults.
Recent findings
Published and unpublished health examination surveys and epidemiological studies suggest that the worldwide prevalence of obesity has doubled since 1980. In 2008, 1 in 10 adults was obese, with women more likely to be obese than men. This obesity epidemic has been paralleled by a trend of reduced sleep duration. Poor sleep quality, which leads to overall sleep loss has also become a frequent complaint. Growing evidence from both laboratory and epidemiological studies points to short sleep duration and poor sleep quality as new risk factors for the development of obesity.
Summary
Sleep is an important modulator of neuroendocrine function and glucose metabolism and sleep loss has been shown to result in metabolic and endocrine alterations, including decreased glucose tolerance, decreased insulin sensitivity, increased evening concentrations of cortisol, increased levels of ghrelin, decreased levels of leptin, and increased hunger and appetite. Recent epidemiological and laboratory evidence confirm previous findings of an association between sleep loss and increased risk of obesity.
Associations between sleep loss and increased risk of obesity and diabetes
Abstract
During the past few decades, sleep curtailment has become a very common behavior in industrialized countries. This trend for shorter sleep duration has developed over the same time period as the dramatic increase in the prevalence of obesity and diabetes. There is rapidly accumulating evidence to indicate that chronic partial sleep loss may increase the risk of obesity and diabetes. Laboratory studies in healthy volunteers have shown that experimental sleep restriction is associated with an adverse impact on glucose homeostasis. Insulin sensitivity decreases rapidly and markedly without adequate compensation in beta cell function, resulting in an elevated risk of diabetes. Prospective epidemiologic studies in both children and adults are consistent with a causative role of short sleep in the increased risk of diabetes. Sleep curtailment is also associated with a dysregulation of the neuroendocrine control of appetite, with a reduction of the satiety factor leptin and an increase in the hunger-promoting hormone ghrelin. Thus, sleep loss may alter the ability of leptin and ghrelin to accurately signal caloric need, acting in concert to produce an internal misperception of insufficient energy availability. The adverse impact of sleep deprivation on appetite regulation is likely to be driven by increased activity in neuronal populations expressing the excitatory peptides orexins that promote both waling and feeding. Consistent with the laboratory evidence, multiple epidemiologic studies have shown an association between short sleep and higher body mass index after controlling for a variety of possible confounders.
Cancer
Parental Behaviors, Emotions at Bedtime, and Sleep Disturbances in Children with Cancer
Abstract
Background: Poor sleep is common for children during cancer treatment, but there is limited understanding of the nature of children's sleep throughout the treatment trajectory. The current exploratory study used an explanatory sequential mixed method approach to examine quantitative associations among sleep problems in children with cancer, parental behavior, and children's sleep hygiene, with follow-up qualitative characterizations of children's sleep across cancer treatment stages.
Procedure: Eighty parents of children with cancer (aged 2-10 years; in active treatment, maintenance treatment, or off treatment) completed an online survey querying the child's sleep quality (Sleep Disturbance Scale for Children-Disorders of Initiating and Maintaining Sleep subscale) and behaviors (Child Sleep Hygiene Scale) and sleep-related parenting behaviors (Parental Sleep Strategies). A subsample (n = 17 parents) participated in qualitative interviews to better characterize the processes of children's sleep and parents' sleep-related behaviors.
Results: Children's sleep quality, sleep hygiene, or parental sleep strategies were not significantly different by cancer treatment groups. Greater sleep disturbance in children was associated with their parents' tendency to accommodate the child's bedtime requests. Qualitatively, cancer treatment-related anxiety in both children and parents influence the onset of these disruptive sleep behaviors.
Conclusion: Parents' sleep-related behaviors affect children's sleep during cancer treatment. Parents' accommodation may start during active treatment to alleviate cancer-related challenges, and these behaviors may continue into maintenance therapy and off treatment to reinforce sleep disturbance. Behavioral interventions targeting unhelpful parental behaviors may improve sleep in children with cancer during and after cancer treatment.
Sleep-wake rhythm disruption is associated with cancer-related fatigue in pediatric acute lymphoblastic leukemia
Abstract
Study objectives: To compare sleep-wake rhythms, melatonin, and cancer-related fatigue in pediatric patients with acute lymphoblastic leukemia (ALL) to healthy children and to assess the association between sleep-wake outcomes and cancer-related fatigue.
Methods: A national cohort of ALL patients (2-18 years) was included. Sleep-wake rhythms were measured using actigraphy and generated the following variables: Interdaily stability (IS): higher IS reflects higher stability; intradaily variability (IV): lower IV indicates less fragmentation; L5 and M10 counts: activity counts during the five least and 10 most active hours, respectively; and relative amplitude (RA): the ratio of L5 and M10 counts (higher RA reflects a more robust rhythm). The melatonin metabolite, 6-sulfatoxymelatonin (aMT6s), was assessed in urine. Cancer-related fatigue was assessed with the PedsQL Multidimensional Fatigue Scale. Using regression models sleep-wake rhythms, aMT6s, and cancer-related fatigue were compared to healthy children and associations between sleep-wake outcomes and cancer-related fatigue were assessed in ALL patients.
Results: In total, 126 patients participated (response rate: 67%). IS, RA, and M10 counts were lower in patients compared to healthy children (p < 0.001). aMT6s levels were comparable to healthy children (p = 0.425). Patients with ALL were more fatigued compared to healthy children (p < 0.001). Lower IS, RA and M10 counts and higher IV were significantly associated with more parent-reported cancer-related fatigue. Associations between sleep-wake rhythms and self-reported cancer-related fatigue were not statistically significant.
Conclusions: Sleep-wake rhythm impairment is associated with more cancer-related fatigue in pediatric ALL patients. Interventions aimed to improve sleep hygiene and encourage physical activity may reduce cancer-related fatigue.
The effects of sleep hygiene education and reflexology on sleep quality and fatigue in patients receiving chemotherapy
Abstract
Introduction: This study was conducted to determine the effects of sleep hygiene education and reflexology on sleep quality and fatigue in the patients receiving chemotherapy.
Methods: The sample of the study consisted of 167 patients (84 in the experimental and 83 in the control group). The data were collected between October 2016 and November 2017 using an Introductory Information Form, the Pittsburgh Sleep Quality Index (PSQI) and the Fatigue Severity Scale (FSS).
Results: The mean -test score from the PSQI was 5.5 ± 2.1 for the experimental group and 13 ± 2.4 for the control group. The mean post- test score from the FSS was 22.6 ± 1.9 for the experimental group and 41.0 ± 4.2 for the control group. The difference between the mean scores of the groups was statistically significant (p = 0.000).
Conclusion: The patients receiving chemotherapy had lower mean scores from the PSQI and the FSS while they had increased sleep quality and decreased fatigue after sleep hygiene education and reflexology.
Meta-analysis: Exercise intervention for sleep problems in cancer patients
Abstract
Background: Sleep problems cause physical and mental distress and may influence the survival of cancer patients.
Objectives: This study aimed to explore the efficacy of exercise intervention to improve sleep in cancer patients.
Methods: Published papers from 1980 to 2018 were searched.
Results: The major findings included (a) exercise intervention had small positive effects on enhancing total subjective sleep quality (TSSQ; g = 0.38, 95% CI = 0.21-0.54) and objective sleep onset latency (g = 0.21, 95% CI = 0.01-0.41). (b) The characteristics in subgroups in regarding the small to large effects of an exercise programme on sleep were identified. First, the groups of a home-based exercise and a supervised exercise combined with a home-based exercise had a medium effect on TSSQ than the usual group. Second, interventions with aerobic exercise, especially the 4- to 8-week programmes and those with weekly volume of 80-149 min per week for cancer patients with ongoing or completed treatment also had a medium to large positive effect on TSSQ. Finally, patients with breast cancer and haematologic malignancies contributed a small effect in this meta-analysis.
Conclusions: Maintaining regular aerobic exercises, even of different durations and weekly volumes, benefits patient sleep quality.
Investigating causal relations between sleep traits and risk of breast cancer in women: mendelian randomisation study
Abstract
Objective: To examine whether sleep traits have a causal effect on risk of breast cancer.
Design: Mendelian randomisation study.
Setting: UK Biobank prospective cohort study and Breast Cancer Association Consortium (BCAC) case-control genome-wide association study.
Participants: 156 848 women in the multivariable regression and one sample mendelian randomisation (MR) analysis in UK Biobank (7784 with a breast cancer diagnosis) and 122 977 breast cancer cases and 105 974 controls from BCAC in the two sample MR analysis.
Exposures: Self reported chronotype (morning or evening preference), insomnia symptoms, and sleep duration in multivariable regression, and genetic variants robustly associated with these sleep traits.
Main outcome measure: Breast cancer diagnosis.
Results: In multivariable regression analysis using UK Biobank data on breast cancer incidence, morning preference was inversely associated with breast cancer (hazard ratio 0.95, 95% confidence interval 0.93 to 0.98 per category increase), whereas there was little evidence for an association between sleep duration and insomnia symptoms. Using 341 single nucleotide polymorphisms (SNPs) associated with chronotype, 91 SNPs associated with sleep duration, and 57 SNPs associated with insomnia symptoms, one sample MR analysis in UK Biobank provided some supportive evidence for a protective effect of morning preference on breast cancer risk (0.85, 0.70, 1.03 per category increase) but imprecise estimates for sleep duration and insomnia symptoms. Two sample MR using data from BCAC supported findings for a protective effect of morning preference (inverse variance weighted odds ratio 0.88, 95% confidence interval 0.82 to 0.93 per category increase) and adverse effect of increased sleep duration (1.19, 1.02 to 1.39 per hour increase) on breast cancer risk (both oestrogen receptor positive and oestrogen receptor negative), whereas evidence for insomnia symptoms was inconsistent. Results were largely robust to sensitivity analyses accounting for horizontal pleiotropy.
Conclusions: Findings showed consistent evidence for a protective effect of morning preference and suggestive evidence for an adverse effect of increased sleep duration on breast cancer risk.
Influence of Yoga on Cancer-Related Fatigue and on Mediational Relationships Between Changes in Sleep and Cancer-Related Fatigue: A Nationwide, Multicenter Randomized Controlled Trial of Yoga in Cancer Survivors
Abstract
Background: Cancer-related fatigue (CRF) often co-occurs with sleep disturbance and is one of the most pervasive toxicities resulting from cancer and its treatment. We and other investigators have previously reported that yoga therapy can improve sleep quality in cancer patients and survivors. No nationwide multicenter phase III randomized controlled trial (RCT) has investigated whether yoga therapy improves CRF or whether improvements in sleep mediate the effect of yoga on CRF. We examined the effect of a standardized, 4-week, yoga therapy program (Yoga for Cancer Survivors [YOCAS]) on CRF and whether YOCAS-induced changes in sleep mediated changes in CRF among survivors.
Study design and methods: Four hundred ten cancer survivors were recruited to a nationwide multicenter phase III RCT comparing the effect of YOCAS to standard survivorship care on CRF and examining the mediating effects of changes in sleep, stemming from yoga, on changes in CRF. CRF was assessed by the Multidimensional Fatigue Symptom Inventory. Sleep was assessed via the Pittsburgh Sleep Quality Index. Between- and within-group intervention effects on CRF were assessed by analysis of covariance and 2-tailed t test, respectively. Path analysis was used to evaluate mediation.
Results: YOCAS participants demonstrated significantly greater improvements in CRF compared with participants in standard survivorship care at post-intervention ( P < .01). Improvements in overall sleep quality and reductions in daytime dysfunction (eg, excessive napping) resulting from yoga significantly mediated the effect of yoga on CRF (22% and 37%, respectively, both P < .01).
Conclusions: YOCAS is effective for treating CRF among cancer survivors; 22% to 37% of the improvements in CRF from yoga therapy result from improvements in sleep quality and daytime dysfunction. Oncologists should consider prescribing yoga to cancer survivors for treating CRF and sleep disturbance.
Physical Activity and Sleep Quality in Breast Cancer Survivors: A Randomized Trial
Abstract
Purpose: Data from large randomized controlled trials confirming sleep quality improvements with aerobic physical activity have heretofore been lacking for post-primary treatment breast cancer survivors. Our primary purpose for this report was to determine the effects of a physical activity behavior change intervention, previously reported to significantly increase physical activity behavior, on sleep quality in post-primary treatment breast cancer survivors.
Methods: Post-primary treatment breast cancer survivors (n = 222) were randomized to a 3-month physical activity behavior change intervention (Better Exercise Adherence after Treatment for Cancer [BEAT Cancer]) or usual care. Self-report (Pittsburgh Sleep Quality Index [PSQI]) and actigraphy (latency and efficiency) sleep outcomes were measured at baseline, 3 months (M3), and 6 months (M6).
Results: After adjusting for covariates, BEAT Cancer significantly improved PSQI global sleep quality when compared with usual care at M3 (mean between-group difference [M] = -1.4, 95% confidence interval [CI] = -2.1 to -0.7, P < 0.001) and M6 (M = -1.0, 95% CI = -1.7 to -0.2, P = 0.01). BEAT Cancer improved several PSQI subscales at M3 (sleep quality M = -0.3, 95% CI = -0.4 to -0.1, P = 0.002; sleep disturbances M = -0.2, 95% CI = -0.3 to -0.03, P = 0.016; daytime dysfunction M = -0.2, 95% CI = -0.4 to -0.02, P = 0.027) but not M6. A nonsignificant increase in percent of participants classified as good sleepers occurred. No significant between-group difference was noted for accelerometer latency or efficiency.
Conclusion: A physical activity intervention significantly reduced perceived global sleep dysfunction at 3 and 6 months, primarily because of improvements in sleep quality aspects not detected with accelerometer.
Sleep duration and the risk of cancer: a systematic review and meta-analysis including dose-response relationship
Abstract
Background: The effect of sleep duration on cancer risk remains controversial. We aimed to quantify the available evidence on this relationship using categorical and dose-response meta-analyses.
Methods: Population-based cohort studies and case-control studies with at least three categories of sleep duration were identified by searching PubMed, EMBASE, and the Cochrane Library database up to July 2017.
Results: Sixty-five studies from 25 articles were included, involving 1,550,524 participants and 86,201 cancer cases. The categorical meta-analysis revealed that neither short nor long sleep duration was associated with increased cancer risk (short: odds ratio [OR] = 1.01, 95% confidence intervals [CI] = 0.97-1.05; long: OR = 1.02, 95% CI = 0.97-1.07). Subgroup analysis revealed that short sleep duration was associated with cancer risk among Asians (OR = 1.36; 95% CI: 1.02-1.80) and long sleep duration significantly increased the risk of colorectal cancer (OR = 1.21; 95% CI: 1.08-1.34). The dose-response meta-analysis showed no significant relationship between sleep duration and cancer risk. When treated as two linear piecewise functions with a cut point of 7 h, similar nonsignificant associations were found (per 1-h reduction: OR = 1.02, 95% CI = 0.98-1.07; per 1-h increment: OR = 1.003, 95% CI = 0.97-1.03).
Conclusion: Categorical meta-analysis indicated that short sleep duration increased cancer risk in Asians and long sleep duration increased the risk of colorectal cancer, but these findings were not consistent in the dose-response meta-analysis. Long-term randomized controlled trials and well-designed prospective studies are needed to establish causality and to elucidate the mechanism underlying the association between sleep duration and cancer risk.
The effect of melatonin on sleep and quality of life in patients with advanced breast cancer
Abstract
Background: Fatigue and sleep problems are prevalent in cancer patients and can be associated with disruption of circadian rhythmicity. In this prospective phase II trial, we sought to assess the effect of melatonin on circadian biomarkers, sleep, and quality of life in breast cancer patients.
Methods: Thirty-two patients with metastatic breast cancer, receiving hormonal or trastuzumab therapy, took 5 mg of melatonin at bedtime for 2 months. Before starting and after 2 months on melatonin therapy, sleep and circadian rhythmicity were assessed by actigraphy, diurnal patterns of serum cortisol, and the expression of the core clock genes PER2 and BMAL1 in peripheral blood mononuclear cells. The European Organisation for Research and Treatment of Cancer (EORTC) QLQ-C30 questionnaire was completed for subjective parameters.
Results: Bedtime melatonin was associated with a significant improvement in a marker of objective sleep quality, sleep fragmentation and quantity, subjective sleep, fatigue severity, global quality of life, and social and cognitive functioning scales. Morning clock gene expression was increased following bedtime melatonin intake. Melatonin did not affect actigraphy measure of circadian rhythmicity, or the diurnal cortisol pattern.
Conclusion: These results invite further investigation of melatonin as a potentially useful therapeutic agent for improving sleep and quality of life in cancer patients.
Exercise, sleep and cancer-related fatigue: Are they related?
Abstract
Cancer-related fatigue (CRF) is a commonly reported and debilitating side effect of cancer and/or cancer treatment. Sleep disorders are also highly reported in the cancer population; however it is unknown if sleep is associated with fatigue. In the general population, exercise has been shown to improve sleep, however in the cancer population this idea is under investigation. The primary purposes of this review were to: (i) review the prevalence and causes of sleep disorders in cancer patients and survivors, (ii) examine the relationship between sleep and CRF and (iii) review the impact of exercise interventions on sleep in cancer patients and survivors. A scoping review of the literature was conducted regarding exercise interventions in cancer patients and survivors with sleep as at least one outcome measure. A search of the literature revealed limited studies (n=21) assessing the effect of exercise on sleep disorders in the cancer population. Methodological issues are evident because assessing sleep is often not the main outcome of interest. The reviewed studies revealed that exercise positively impacts sleep quality and quantity. There seems to be possible relationship between sleep disorders, exercise and CRF. Further investigation of this relationship is necessary, specifically using objective measurement tools, in large, controlled studies, focusing on sleep as the primary outcome.
Measurements and status of sleep quality in patients with cancers
Abstract
Sleep disturbance is identified as a prominent concern in cancer patients with detrimental effect on health outcome, which accompanies a decline in functional status, reduces quality of life, and even accelerates deterioration of disease. Therefore, in order to design safe and effective therapy, and improve the quality of life in cancer patients, it is necessary to seek the optimal measures of sleep quality evaluation, which include the objective assessments (e.g., polysomnography [PSG], the bispectral index [BIS], actigraphy) and subjective assessments (e.g., Pittsburgh Sleep Quality Index [PSQI], Insomnia Severity Index [ISI], Epworth Sleepiness Scale [ESS], Consensus Sleep Diary [CSD]) and understand the status of sleep quality in cancer patients, especially patients with cancers in the breast, lung, head and neck, ovaries, and uterus. This review summarizes the common methods used to measure sleep quality and compares the sensitivity, specificity, and practicability of these methods. In addition, the status of sleep disturbance in patients with cancer is analyzed.
Abstract
Purpose: Epidemiological studies suggest that short sleep duration and poor sleep quality may increase breast cancer risk. However, whether sleep is associated with breast tumor aggressiveness characteristics has largely been unexplored.
Methods: The study included 4171 non-Hispanic whites (NHW) and 235 African Americans (AA) diagnosed with incident, primary, invasive breast cancer in the Women's Health Initiative (WHI) Observational Study (1994-2013). We used logistic regression to examine the association of baseline sleep (sleep duration, sleep quality, WHI Insomnia Rating Scale) with tumor grade, stage, hormone receptor status, HER2 status.
Results: In NHW, women who reported 6 h of sleep/night were more likely to have tumors classified as regional/distant stage at diagnosis compared to women who slept 7-8 h/night (adjusted odds ratio (OR): 1.25, 95% confidence interval (CI): 1.05-1.48). AA women who reported their typical night's sleep as 'average quality' or 'restless or very restless sleep' were more likely to be diagnosed with triple-negative tumors than those who reported 'sound or restful' sleep (adjusted ORs: 2.91 (1.11, 7.63) and 3.74 (1.10, 12.77), respectively).
Conclusions: Our findings provide indications that aspects of sleep (sleep duration and quality), partially modifiable health behaviors, may be associated with development of aggressive tumor characteristics in postmenopausal women. The role of these sleep attributes may differ for NHW and AA women; however, further study in robust, racial diverse samples is needed. This study provides evidence that facets of sleep behavior are associated with the development of aggressive tumor features and these associations differ by race.
Association between shift work and risk of prostate cancer: a systematic review and meta-analysis of observational studies
Abstract
Observational studies suggest that shift work may be associated with prostate cancer. However, the results are inconsistent. The objective of this study is to quantitatively assess the association between shift work and the risk of prostate cancer. Relevant studies were identified by a comprehensive search of the PubMed, Embase, Web of Science and China National Knowledge Infrastructure databases to September 2017. We also reviewed the reference lists from retrieved articles. Observational studies that reported relative risk (RR) with 95% confidence intervals (CIs) for the association between shift work and the risk of prostate cancer were included. Linear and non-linear dose-response meta-analyses were performed. Fifteen studies with 16 independent reports involving 2 546 822 individuals and 10 715 patients with prostate cancer were included. The pooled adjusted RR for the association between ever exposure to shift work and prostate cancer risk was 1.23 (95% CI, 1.08-1.41; P < 0.001). A non-linear association of prostate cancer risk with duration of shift work was identified (P for non-linearity = 0.001). Subgroup analysis demonstrated a higher pooled RR of prostate cancer for studies among Asian populations (RR = 1.98, 95% CI, 1.34-2.93; P = 0.618). A positive association was observed in rotating shift groups (RR = 1.10, 95% CI, 1.00-1.26; P = 0.156), but not in other shift groups. Integrated evidence from this meta-analysis suggests that shift work is significantly associated with an increased risk of prostate cancer, and a non-linear association between duration of shift work and prostate cancer was found.
Night Shift Work and Breast Cancer Incidence: Three Prospective Studies and Meta-analysis of Published Studies
Abstract
Background: It has been proposed that night shift work could increase breast cancer incidence. A 2007 World Health Organization review concluded, mainly from animal evidence, that shift work involving circadian disruption is probably carcinogenic to humans. We therefore aimed to generate prospective epidemiological evidence on night shift work and breast cancer incidence.
Methods: Overall, 522 246 Million Women Study, 22 559 EPIC-Oxford, and 251 045 UK Biobank participants answered questions on shift work and were followed for incident cancer. Cox regression yielded multivariable-adjusted breast cancer incidence rate ratios (RRs) and 95% confidence intervals (CIs) for night shift work vs no night shift work, and likelihood ratio tests for interaction were used to assess heterogeneity. Our meta-analyses combined these and relative risks from the seven previously published prospective studies (1.4 million women in total), using inverse-variance weighted averages of the study-specific log RRs.
Results: In the Million Women Study, EPIC-Oxford, and UK Biobank, respectively, 673, 28, and 67 women who reported night shift work developed breast cancer, and the RRs for any vs no night shift work were 1.00 (95% CI = 0.92 to 1.08), 1.07 (95% CI = 0.71 to 1.62), and 0.78 (95% CI = 0.61 to 1.00). In the Million Women Study, the RR for 20 or more years of night shift work was 1.00 (95% CI = 0.81 to 1.23), with no statistically significant heterogeneity by sleep patterns or breast cancer risk factors. Our meta-analysis of all 10 prospective studies included 4660 breast cancers in women reporting night shift work; compared with other women, the combined relative risks were 0.99 (95% CI = 0.95 to 1.03) for any night shift work, 1.01 (95% CI = 0.93 to 1.10) for 20 or more years of night shift work, and 1.00 (95% CI = 0.87 to 1.14) for 30 or more years.
Conclusions: The totality of the prospective evidence shows that night shift work, including long-term shift work, has little or no effect on breast cancer incidence.
Night Shift Work and Risk of Breast Cancer
Abstract
Purpose of review: Night work is increasingly common and a necessity in certain sectors of the modern 24-h society. The embedded exposure to light-at-night, which suppresses the nocturnal hormone melatonin with oncostatic properties and circadian disruption, i.e., misalignment between internal and external night and between cells and organs, are suggested as main mechanisms involved in carcinogenesis. In 2007, the International Agency for Research on Cancer (IARC) classified shift work that involves circadian disruption as probably carcinogenic to humans based on limited evidence from eight epidemiologic studies on breast cancer, in addition to sufficient evidence from animal experiments. The aim of this review is a critical update of the IARC evaluation, including subsequent and the most recent epidemiologic evidence on breast cancer risk after night work.
Recent findings: After 2007, in total nine new case-control studies, one case-cohort study, and eight cohort studies are published, which triples the number of studies. Further, two previous cohorts have been updated with extended follow-up. The assessment of night shift work is different in all of the 26 existing studies. There is some evidence that high number of consecutive night shifts has impact on the extent of circadian disruption, and thereby increased breast cancer risk, but this information is missing in almost all cohort studies. This in combination with short-term follow-up of aging cohorts may explain why some cohort studies may have null findings. The more recent case-control studies have contributed interesting results concerning breast cancer subtypes in relation to both menopausal status and different hormonal subtypes. The large differences in definitions of both exposure and outcome may contribute to the observed heterogeneity of results from studies of night work and breast cancer, which overall points in the direction of an increased breast cancer risk, in particular after over 20 years of night shifts. Overall, there is a tendency of increased risk of breast cancer either after over 20 years of night shift or after shorter periods with many consecutive shifts. More epidemiologic research using standardized definitions of night work metrics and breast cancer subtypes as well as other cancers is needed in order to improve the epidemiologic evidence in combination with animal models of night work. Also, evidence-based preventive interventions are needed.
Timing Matters: Circadian Rhythm in Sepsis, Obstructive Lung Disease, Obstructive Sleep Apnea, and Cancer
Abstract
Physiological and cellular functions operate in a 24-hour cyclical pattern orchestrated by an endogenous process known as the circadian rhythm. Circadian rhythms represent intrinsic oscillations of biological functions that allow for adaptation to cyclic environmental changes. Key clock genes that affect the persistence and periodicity of circadian rhythms include BMAL1/CLOCK, Period 1, Period 2, and Cryptochrome. Remarkable progress has been made in our understanding of circadian rhythms and their role in common medical conditions. A critical review of the literature supports the association between circadian misalignment and adverse health consequences in sepsis, obstructive lung disease, obstructive sleep apnea, and malignancy. Circadian misalignment plays an important role in these disease processes and can affect disease severity, treatment response, and survivorship. Normal inflammatory response to acute infections, airway resistance, upper airway collapsibility, and mitosis regulation follows a robust circadian pattern. Disruption of normal circadian rhythm at the molecular level affects severity of inflammation in sepsis, contributes to inflammatory responses in obstructive lung diseases, affects apnea length in obstructive sleep apnea, and increases risk for cancer. Chronotherapy is an underused practice of delivering therapy at optimal times to maximize efficacy and minimize toxicity. This approach has been shown to be advantageous in asthma and cancer management. In asthma, appropriate timing of medication administration improves treatment effectiveness. Properly timed chemotherapy may reduce treatment toxicities and maximize efficacy. Future research should focus on circadian rhythm disorders, role of circadian rhythm in other diseases, and modalities to restore and prevent circadian disruption.
Circadian Clocks and Cancer: Timekeeping Governs Cellular Metabolism
Abstract
The circadian clock is a biological mechanism that dictates an array of rhythmic physiological processes. Virtually all cells contain a functional clock whose disruption results in altered timekeeping and detrimental systemic effects, including cancer. Recent advances have connected genetic disruption of the clock with multiple transcriptional and signaling networks controlling tumor initiation and progression. An additional feature of this circadian control relies on cellular metabolism, both within the tumor microenvironment and the organism systemically. A discussion of major advances related to cancer metabolism and the circadian clock will be outlined, including new efforts related to metabolic flux of transformed cells, metabolic heterogeneity of tumors, and the implications of circadian control of these pathways.
Interplay between Circadian Clock and Cancer: New Frontiers for Cancer Treatment
Abstract
Circadian clocks constitute the evolutionary molecular machinery that dictates the temporal regulation of physiology to maintain homeostasis. Disruption of the circadian rhythm plays a key role in tumorigenesis and facilitates the establishment of cancer hallmarks. Conversely, oncogenic processes directly weaken circadian rhythms. Pharmacological modulation of core clock genes is a new approach in cancer therapy. The integration of circadian biology into cancer research offers new options for making cancer treatment more effective, encompassing the prevention, diagnosis, and treatment of this devastating disease. This review highlights the role of the circadian clock in tumorigenesis and cancer hallmarks, and discusses how pharmacological modulation of circadian clock genes can lead to new therapeutic options.
Epigenetic Basis of Circadian Rhythm Disruption in Cancer
Abstract
Self-sustained and synchronized to environmental stimuli, circadian clocks are under genetic and epigenetic regulation. Recent findings have greatly increased our understanding of epigenetic plasticity governed by circadian clock. Thus, the link between circadian clock and epigenetic machinery is reciprocal. Circadian clock can affect epigenetic features including genomic DNA methylation, noncoding RNA, mainly miRNA expression, and histone modifications resulted in their 24-h rhythms. Concomitantly, these epigenetic events can directly modulate cyclic system of transcription and translation of core circadian genes and indirectly clock output genes. Significant findings interlocking circadian clock, epigenetics, and cancer have been revealed, particularly in breast, colorectal, and blood cancers. Aberrant methylation of circadian gene promoter regions and miRNA expression affected circadian gene expression, together with 24-h expression oscillation pace have been frequently observed.
Association Between Subjective Sleep Quality and Depression on Immunocompetence in Low-Income Women at Risk for Cervical Cancer
Abstract
Objective
The purpose of this study was to investigate whether subjective sleep quality is more strongly associated with immunocompetence than depression among women at risk for cervical cancer.
Methods
Participants were 91 women referred for colposcopy because of abnormal results on a Pap smear. On the day of the procedure, participants completed the Center for Epidemiological Studies Depression Scale, two indices of subjective sleep quality (ie, satisfaction with sleep obtained and degree of sleep restfulness), and a health behaviors assessment questionnaire. Levels of peripheral blood lymphocyte subpopulations (helper T, cytotoxic/suppressor T, NK, and B cells) were also assessed at this time. Approximately 10 days later, the presence of depressive disorder was assessed using the Structured Clinical Interview for DSM-III-R.
Results
Hierarchical regression analyses revealed that satisfaction with the amount of sleep obtained was significantly associated with the circulating number and percentage of helper T cells (TH/CD4+) and the percentage of cytotoxic/suppressor T cells (TC/CD8+), after controlling for confounder variables (ie, age, smoking status, and drug use). Depression was significantly associated only with the percentage of TC cells. Sleep satisfaction remained significantly associated with the number and percentage of TH cells and percentage of TC cells after controlling for the variance explained by depression.
Conclusions
Results of this study suggest that subjective sleep quality shares a significant and independent portion of the variance with immunity that is not accounted for by depression. Although the long-term impact of these immune alterations on disease progression needs to be directly explored, it may be important to systematically screen for and manage sleep disturbance in women at high risk for cervical cancer.
Sleep quality, duration, and breast cancer aggressiveness
Abstract
Purpose
Epidemiological studies suggest that short sleep duration and poor sleep quality may increase breast cancer risk. However, whether sleep is associated with breast tumor aggressiveness characteristics has largely been unexplored.
Methods
The study included 4171 non-Hispanic whites (NHW) and 235 African Americans (AA) diagnosed with incident, primary, invasive breast cancer in the Women’s Health Initiative (WHI) Observational Study (1994–2013). We used logistic regression to examine the association of baseline sleep (sleep duration, sleep quality, WHI Insomnia Rating Scale) with tumor grade, stage, hormone receptor status, HER2 status.
Results
In NHW, women who reported 6 h of sleep/night were more likely to have tumors classified as regional/distant stage at diagnosis compared to women who slept 7–8 h/night (adjusted odds ratio (OR): 1.25, 95% confidence interval (CI): 1.05–1.48). AA women who reported their typical night’s sleep as ‘average quality’ or ‘restless or very restless sleep’ were more likely to be diagnosed with triple-negative tumors than those who reported ‘sound or restful’ sleep (adjusted ORs: 2.91 (1.11, 7.63) and 3.74 (1.10, 12.77), respectively).
Conclusions
Our findings provide indications that aspects of sleep (sleep duration and quality), partially modifiable health behaviors, may be associated with development of aggressive tumor characteristics in postmenopausal women. The role of these sleep attributes may differ for NHW and AA women; however, further study in robust, racial diverse samples is needed. This study provides evidence that facets of sleep behavior are associated with the development of aggressive tumor features and these associations differ by race.
Exercise, sleep quality, and mediators of sleep in breast and prostate cancer patients receiving radiation therapy
Abstract
Cancer patients often report impaired sleep quality. Impaired sleep quality may be due to increased levels of sleep-mediating cytokines resulting from cancer treatment. Exercise may have a positive influence on sleep-mediating cytokines, such as interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-α), and soluble tumor necrosis factor-alpha receptor (sTNF-R), which may improve sleep quality. This two-arm pilot study compared the influence of a home-based exercise intervention with standard care/control on sleep quality and mediators of sleep. Breast and prostate cancer patients (n = 38) beginning radiation therapy were randomized to a 4-week exercise program or no exercise arm. Global sleep quality, subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbances, use of sleep medication, and daytime dysfunction were assessed with the Pittsburgh Sleep Quality Index. IL-6, TNF-α, and sTNF-R were measured before and after intervention. There was a greater improvement in sleep quality in the exercise group from pre- to postintervention, although the difference was not significant. Additionally, there were associations between IL-6 and sleep efficiency and duration, suggesting that regulation of sleep-mediating cytokines by exercise may mediate improvements in sleep-quality components.
The effect of sleep disturbance on quality of life in women with ovarian cancer☆
Abstract
Objective
To estimate the prevalence of sleep disturbances, and to determine if there is an association between sleep disturbances with quality of life (QOL), depression or clinical demographic variables.
Methods
Patients diagnosed with ovarian,
fallopian tube
or
primary peritoneal cancer
during the last 5 years completed questionnaires regarding sleep patterns and disturbances [Pittsburgh Sleep Quality Index (PSQI)], depression [Beck Depression inventory (BDI)], and QOL [The Functional Assessment of Cancer Therapy-Ovarian (FACT-O), fatigue module (− F)]. Data were analyzed by
Student's t-test
or Pearson correlation coefficient to determine if there were differences between
PSQI
score with QOL, depression or clinical demographic variables.
Results
86/275 (31% response) of patients returned the surveys. Mean age was 58.1 (SD = 14.6) years and 70% had advanced disease at diagnosis. Thirty-six percent had current disease of which 81% were receiving chemotherapy. Sixty-seven percent of patients had a PSQI score ≥ 5 corresponding to overall poor sleep quality and 46% of patients reported using sleep medication at least once during the prior month. PSQI score was significantly inversely correlated with all QOL domains (physical: r = −.599, p < .001, functional: r = −.692, p < .001, social: r = −.212, p < .001, emotional: r = −.379, p < .001, fatigue; r = −.655 p < .001) and with depression (r = .539, p < .001). PSQI was not correlated with age, time since diagnosis, number of previous
chemotherapy regimens
. PSQI score did not differ by current disease or chemotherapy status.
Conclusions
Sleep disturbances reduce QOL, a prognostic indicator for survival, in ovarian cancer patients. These patients should undergo routine screening and would benefit from interventions that aim to promote restful sleep.
Effect of mindfulness-based stress reduction on sleep quality: Results of a randomized trial among Danish breast cancer patients
Abstract
The prevalence of sleep disturbance is high among cancer patients, and the sleep problems tend to last for years after the end of treatment. As part of a large randomized controlled clinical trial (the MICA trial, NCT00990977) of the effect of mindfulness-based stress reduction (MBSR) on psychological and somatic symptoms among breast cancer patients, the aim of the current study was to evaluate the effect of MBSR on the secondary outcome, ‘sleep quality’. Material and methods. A total of 336 women operated on for breast cancer stage I–III 3–18 months previously were randomized to MBSR (n = 168) or treatment as usual (n = 168); both groups received standard clinical care. The intervention consisted of an eight-week MBSR program (psycho-education, meditation and gentle yoga). Sleep quality was assessed on the Medical Outcome Study sleep scale at baseline, after the intervention and at six- and 12-months’ follow-up. Results. The mean sleep problem scores were significantly lower in the MBSR group than in controls immediately after the intervention. Quantile regression analyses showed that the effect was statistically significant only for the participants represented by the lower percentile of change between baseline and post-intervention, i.e. those who had more sleep problems; the MBSR group had a significantly smaller increase in sleep problems than the control group. After the 12-month follow-up, there was no significant between-group effect of MBSR on sleep quality in intention-to-treat analyses. Conclusion. MBSR had a statistically significant effect on sleep quality just after the intervention but no long-term effect among breast cancer patients. Future trials in which participation is restricted to patients with significant sleep problems are recommended for evaluating the effect of MBSR on sleep quality.
One-Year Outcomes of a Behavioral Therapy Intervention Trial on Sleep Quality and Cancer-Related Fatigue
Abstract
Purpose
To determine 1-year outcomes of a four-component behavioral therapy (BT) sleep intervention (Individualized Sleep Promotion Plan [ISPP]) versus a healthy eating control (HEC) on cancer-related fatigue in women receiving breast cancer adjuvant chemotherapy treatment (CTX).
Patients and Methods
A total of 219 participants from 12 oncology clinics were randomly assigned in a clinical trial. Before CTX, research nurses coached intervention participants to develop a BT plan including stimulus control, modified sleep restriction, relaxation therapy, and sleep hygiene. BT plans were revised before each CTX and 30, 60, and 90 days after the last CTX and reinforced 7 to 9 days later. HEC participants received nutritional information and equal attention. Pittsburgh Sleep Quality Index (PSQI), Daily Diary, Wrist Actigraph, and Piper Fatigue Scale measures and Repeated Linear Mixed Model analysis following the Intent to Treat paradigm were used.
Results
Sleep quality differed over 1 years time (F [4,162] = 7.7, P < .001; by group, F [1,173] = 4.8, P = .029; and over time by group, F [4,162] = 3.3, P = .013). Pairwise comparisons revealed significant differences between groups at 90 days (P = .002) but not at 1 year (P = .052). Seven days of diary and actigraphy data did not corroborate with monthly reflections (PSQI). The night awakenings (Actigraph) pattern was significantly different by group over time (P = .046), with no differences between groups at 90 days or at 1 year. Fatigue was lower at 1 year than before CTX; no group effects were found.
Conclusion
The BT group, on average, experienced significant improvement on global sleep quality compared with the HEC group, but not on objective sleep or fatigue outcomes.
Multicenter, Randomized Controlled Trial of Yoga for Sleep Quality Among Cancer Survivors
Abstract
Purpose
Thirty percent to 90% of cancer survivors report impaired sleep quality post-treatment, which can be severe enough to increase morbidity and mortality. Lifestyle interventions, such as exercise, are recommended in conjunction with drugs and cognitive behavioral therapy for the treatment of impaired sleep. Preliminary evidence indicates that yoga—a mind-body practice and form of exercise—may improve sleep among cancer survivors. The primary aim of this randomized, controlled clinical trial was to determine the efficacy of a standardized yoga intervention compared with standard care for improving global sleep quality (primary outcome) among post-treatment cancer survivors.
Patients and Methods
In all, 410 survivors suffering from moderate or greater sleep disruption between 2 and 24 months after surgery, chemotherapy, and/or radiation therapy were randomly assigned to standard care or standard care plus the 4-week yoga intervention. The yoga intervention used the Yoga for Cancer Survivors (YOCAS) program consisting of pranayama (breathing exercises), 16 Gentle Hatha and Restorative yoga asanas (postures), and meditation. Participants attended two 75-minute sessions per week. Sleep quality was assessed by using the Pittsburgh Sleep Quality Index and actigraphy pre- and postintervention.
Results
In all, 410 survivors were accrued (96% female; mean age, 54 years; 75% had breast cancer). Yoga participants demonstrated greater improvements in global sleep quality and, secondarily, subjective sleep quality, daytime dysfunction, wake after sleep onset, sleep efficiency, and medication use at postintervention (all P ≤ .05) compared with standard care participants.
Conclusion
Yoga, specifically the YOCAS program, is a useful treatment for improving sleep quality and reducing sleep medication use among cancer survivors.
Shift work and cancer risk: Potential mechanistic roles of circadian disruption, light at night, and sleep deprivation
Summary
Shift work that includes a nighttime rotation has become an unavoidable attribute of today's 24-h society. The related disruption of the human circadian time organization leads in the short-term to an array of jet-lag-like symptoms, and in the long-run it may contribute to weight gain/obesity, metabolic syndrome/type II diabetes, and cardiovascular disease.
Epidemiologic studies
also suggest increased cancer risk, especially for breast cancer, in night and rotating female shift workers. If confirmed in more controlled and detailed studies, the carcinogenic effect of night and shift work will constitute additional serious medical, economic, and social problems for a substantial proportion of the working population. Here, we examine the possible multiple and interconnected cancer-promoting mechanisms as a consequence of shift work, i.e., repeated disruption of the circadian system,
pineal hormone
melatonin
suppression by exposure to light at night, sleep-deprivation-caused impairment of the immune system, plus metabolic changes favoring obesity and generation of proinflammatory
reactive oxygen species
.
Behavioral therapy intervention trial to improve sleep quality and cancer‐related fatigue
AbstractBackground: To determine whether sleep quality and fatigue associated with breast cancer adjuvant chemotherapy treatments can be improved with behavioral therapy (BT) [Individualized Sleep Promotion Plan (ISPP©)] including modified stimulus control, modified sleep restriction, relaxation therapy, and sleep hygiene.
Methods: Randomized‐controlled trial based on Piper Integrated Fatigue Model, 219 stages I–IIIA breast cancer patients. Prior to the initial chemotherapy treatment, BT participants developed an ISPP plan that was regularly reinforced and revised. Controls received healthy eating information and attention. Pittsburgh Sleep Quality Index (PSQI), daily diary, actigraph, and Piper Fatigue Scale (PFS) data were collected 2 days prior, during the 7 days after each treatment, and 30 days after the last treatment. Repeated measures analysis of variance was used.
Results: Prior to chemotherapy, participants reported mild fatigue and fairly poor sleep quality. All variables changed over time. A group by time interaction was found for sleep quality (PSQI) improving in the BT group. Diary revealed group differences on number of awakenings, minutes awake after sleep onset, and sleep efficiency. Fatigue (PFS) was similar between groups.
Conclusions: The BT group showed improved sleep quality over time and better sleep (diary). Perceptions of improved sleep quality over time are not consistently associated with diary or actigraph, or result in lower fatigue. Copyright © 2008 John Wiley & Sons, Ltd.
A Home-Based Exercise Program to Improve Function, Fatigue, and Sleep Quality in Patients With Stage IV Lung and Colorectal Cancer: A Randomized Controlled Trial
Abstract
Context
Exercise benefits patients with cancer, but studies of home-based approaches, particularly among those with Stage IV disease, remain small and exploratory.
Objectives
To conduct an adequately powered trial of a home-based exercise intervention that can be facilely integrated into established delivery and
reimbursement
structures.
Methods
Sixty-six adults with Stage IV lung or
colorectal cancer
were randomized, in an eight-week trial, to usual care or incremental walking and home-based strength training. The exercising participants were instructed during a single physiotherapy visit and subsequently exercised four days or more per week; training and step-count goals were advanced during bimonthly telephone calls. The primary outcome measure was mobility assessed with the Ambulatory
Post Acute Care
Basic Mobility Short Form. Secondary outcomes included ratings of pain and sleep quality as well as the ability to perform daily activities (Ambulatory Post Acute Care Daily Activities Short Form), quality of life (Functional Assessment of Cancer Therapy-General), and fatigue (Functional Assessment of Cancer Therapy-Fatigue).
Results
Three participants dropped out and seven died (five in the intervention and two in the control group, P = 0.28). At Week 8, the intervention group reported improved mobility (P = 0.01), fatigue (P = 0.02), and sleep quality (P = 0.05) compared with the usual care group, but did not differ on the other measures.
Conclusion
A home-based exercise program seems capable of improving the mobility, fatigue, and sleep quality of patients with Stage IV lung and colorectal cancer.
Habitual sleep–wake behaviors and lifestyle as predictors of diurnal cortisol patterns in young breast cancer survivors: A longitudinal study
Summary
Objective
This study aimed to identify predictors of changes in diurnal cortisol patterns during the 8-month follow up period for young breast cancer survivors. Among the potential predictors were tumor size, lymph node metastasis, changes in sleep problems, habitual time of awakening and bedtime, physical activity levels, body mass index (BMI), and depressive levels across 8 months.
Methods
The participants were 62 breast cancer women who were aged 40 years and below, and had completed active breast cancer treatment. The longitudinal data were collected at four points: baseline assessment (T0) and three follow-ups after baseline: T1 (in the 2nd month), T2 (in the 5th month), and T3 (in the 8th month). The participants collected their salivary cortisol at home at six time points: upon waking, 30 and 45 min after waking, and at 1200 h, 1700 h, and 2100 h. They also completed several questionnaires: the Medical Outcomes Study Sleep scale; the Beck Depression Inventory-II, physical activity levels on a 10-point scale, time of going to bed, time of awakening, and total sleep hours.
Results
This study found that the main predictors of changes toward flatter diurnal cortisol patterns during the 8-month follow ups were greater tumor sizes, increases of BMI scores, and habitually later times of awakening.
Conclusions
While greater tumor sizes represent biological vulnerability of disruption of cortisol circadian rhythm, maintaining an appropriate BMI and good sleep habits could be a protective factor for normal cortisol regulation, which likely helps to reduce early mortality in young breast cancer survivors.
Hypertension
Sleep Quality and Associated Factors among Diabetes, Hypertension, and Heart Failure Patients at Debre Markos Referral Hospital, Northwest Ethiopia
Abstract
Background: Chronic illnesses have a negative impact on the quality of sleep; however, patients with chronic illness do not bring sleep issues while they are coming to a health institution for a follow-up. As a result, poor sleep quality among patients with chronic illness is often unrecognized and untreated, and it results to a negative impact on the prognosis of chronic illness.
Methods: An institutional-based cross-sectional study design was employed from February 22, 2018, to April 6, 2018. The total sample size was 396. The study employed a stratified random sampling technique, and study participants were selected by systematic sampling. The data were collected by a Pittsburgh Sleep Quality Index (PSQI) questionnaire which is a validated and standardized tool. The data were analyzed by SPSS version 25; text, tables, and figures were utilized for data presentation. By considering a 95% confidence level and P value of 0.05, binary logistic regression and Kruskal-Wallis test were enrolled.
Results: The prevalence of poor sleep quality among diabetes, hypertension, and heart failure patients was 36.5%. The odds of being a poor sleeper are increased when age increased. Patients who have poor perception towards the prognosis of their illness were four times more likely to be a poor sleeper compared to patients with good perception (AOR = 4.21, 95%CI = 1.94-9.13, P = 0.001). Patients who have anxiety were four times more likely to be a poor sleeper compared with patients without anxiety (AOR = 3.69, 95%CI = 2.19-6.20, P = 0.001). The educational level and residence were other factors associated with sleep quality. There was a statistically significant difference of sleep quality between patients with diabetes and hypertension, and diabetes and heart failure (F (2, 384) = 10.92, P = 0.004). Conclusion and Recommendations. In this study, over one-third of patients had poor sleep quality. Age, educational level, residence, perception towards prognosis of illness, and anxiety were factors associated with sleep quality. All health care providers should assess and provide advice about sleep hygiene and influencing factors. Assessment of sleep quality for every diabetes, hypertension, and heart failure patients in every visit should be incorporated in the care package.
Renalase and hypertension-demographic and clinical correlates in obstructive sleep apnea
Abstract
Background: Renalase plays an important role in blood pressure regulation. Obstructive sleep apnea (OSA) is a common respiratory disorder associated with hypertension and cardiovascular complications. The aim of the study was to assess the relationship between sleep apnea and renalase concentration.
Material and methods: Adult patients (n = 113) were evaluated for OSA in a sleep laboratory using polysomnography. The respiratory events were scored according to the standards developed by the American Academy of Sleep Medicine. The blood renalase concentration was determined by the ELISA (enzyme-linked immunosorbent assay) test.
Results: OSA (AHI ≥ 5) was diagnosed in 71% (n = 80) of the studied population. Renalase concentration was statistically significantly lower in the group with moderate-to-severe OSA (AHI ≥ 15) compared with the group without OSA (AHI < 5) (139.56 ± 175.72 ng/ml vs. 230.97 ± 240.50 ng/ml, p = 0.042). We have found statistically significant negative correlation between renalase and AHI in hypertensives, but not in normotensives. The statistically significant negative correlation was observed between AHI and renalase in the whole studied group, in males, and in the group of age < 60 years old. There was not such a correlation in females and in the group > 60 years old. Based on the regression model, it was shown that lower renalase concentration, hypertension, higher BMI, and male gender are independently associated with higher AHI.
Conclusions: There is a relationship between the blood renalase concentration and the severity of OSA, which may influence hypertension development in OSA.
[Arterial hypertension and obstructive sleep apnea syndrome: state of knowledge]
Abstract
Obstructive sleep apnea syndrome (OSAS) and arterial hypertension (HT) are two frequent, often concomitant diseases, who are both associated with an increased cardiovascular risk. In the last years, an association between these two entities has been established. The purpose of this article is to review the current knowledge about the link between HT and OSAS, the pathophysiological mechanisms involved in the common genesis of the two conditions and the characteristics suggesting an underlying OSAS in a hypertensive subject. We will also update readers about the current screening of OSAS in which primary care physicians are directly involved, and review the pros and cons of different treatment options for HT in OSAS.
Sleep and Cardio-Metabolic Disease
Abstract
Purpose of review: This review summarises and discusses the epidemiological evidence suggesting a causal relationship between sleep duration and cardio-metabolic risk and outcomes in population.
Recent findings: Sleep duration is affected by a variety of cultural, social, psychological, behavioural, pathophysiological and environmental influences. Changes in modern society-like longer working hours, more shift-work, 24/7 availability of commodities and 24-h global connectivity-have been associated with a gradual reduction in sleep duration and sleeping patterns across westernised populations. We review the evidence of an association between sleep disturbances and the development of cardio-metabolic risk and disease and discuss the implications for causality of these associations. Prolonged curtailment of sleep duration is a risk factor for the development of obesity, diabetes, hypertension, heart disease and stroke and may contribute, in the long-term, to premature death.
Secondary Hypertension: Discovering the Underlying Cause
Abstract
Most patients with hypertension have no clear etiology and are classified as having primary hypertension. However, 5% to 10% of these patients may have secondary hypertension, which indicates an underlying and potentially reversible cause. The prevalence and potential etiologies of secondary hypertension vary by age. The most common causes in children are renal parenchymal disease and coarctation of the aorta. In adults 65 years and older, atherosclerotic renal artery stenosis, renal failure, and hypothyroidism are common causes. Secondary hypertension should be considered in the presence of suggestive symptoms and signs, such as severe or resistant hypertension, age of onset younger than 30 years (especially before puberty), malignant or accelerated hypertension, and an acute rise in blood pressure from previously stable readings. Additionally, renovascular hypertension should be considered in patients with an increase in serum creatinine of at least 50% occurring within one week of initiating angiotensin-converting enzyme inhibitor or angiotensin receptor blocker therapy; severe hypertension and a unilateral smaller kidney or difference in kidney size greater than 1.5 cm; or recurrent flash pulmonary edema. Other underlying causes of secondary hypertension include hyperaldosteronism, obstructive sleep apnea, pheochromocytoma, Cushing syndrome, thyroid disease, coarctation of the aorta, and use of certain medications.
Obstructive Sleep Apnea, Hypertension, and Cardiovascular Risk: Epidemiology, Pathophysiology, and Management
Abstract
Purpose of review: Given the rising prevalence of obstructive sleep apnea (OSA), we aimed to review the epidemiologic and pathophysiologic relationship of OSA, hypertension, and cardiovascular disease, and to summarize recent advances in the treatment of OSA.
Recent findings: OSA is associated with an elevated risk of hypertension and cardiovascular disease. Several pathophysiologic factors contribute to the relationship between OSA and vascular risk, including neurohormonal dysregulation, endothelial dysfunction, and inflammation. While CPAP reduces blood pressure, it has not been demonstrated to reduce cardiovascular risk. The combination of CPAP and weight loss has a synergistic effect on blood pressure and several metabolic parameters. Adherence to CPAP is poor across studies, potentially contributing to the attenuation of perceived cardiovascular benefit from CPAP therapy. A greater emphasis on adherence to CPAP and the combination of CPAP and weight loss are central to reducing cardiovascular risk among individuals with OSA.
Sleep Disorders, Including Sleep Apnea and Hypertension
Abstract
There is mounting evidence for an association between sleep disorders and hypertension. In obstructive sleep apnea (OSA), there are plausible biological reasons for the development of hypertension, and treatment of OSA results in modest (2-3 mm Hg), adherence-dependent decreases in blood pressure, with larger effects evident in those with resistant hypertension. However, prospective, population-based cohort studies have not yet convincingly demonstrated a link between OSA and incident hypertension, and adequately powered controlled trials of CPAP for the prevention or treatment or hypertension are lacking. While associations have been identified between short sleep duration, insomnia, restless legs syndrome (RLS), shift work, and hypertension, the causative role of these conditions/circumstances is not proven, and further well-designed pathophysiological and/or interventional studies are needed. Particular emphasis should be placed on defining subgroups of hypertensive OSA patients that stand to benefit most from OSA treatment and in understanding the link between sleep apnea and hypertensive disorders of pregnancy. Well-controlled intervention studies are needed in populations with short sleep duration, insomnia, shift work sleep disorder, and RLS to confirm their putative links with hypertension.
Sleep and Resistant Hypertension
Abstract
Purpose of review: The goal of the present review is to describe the current findings on the association of sleep with resistant hypertension (hypertension that remains uncontrolled despite the use of three or more antihypertensive medications from different classes, including a diuretic).
Recent findings: Sleep disturbances, particularly obstructive sleep apnea (OSA), are highly prevalent among adults who have resistant hypertension. Randomized controlled trials indicate that treating OSA has modest effects on blood pressure lowering among those with the highest initial blood pressure. There is a paucity of research on the association of habitual sleep and other sleep disturbances with resistant hypertension. Of note, the most recent observational studies describing the association of OSA with resistant hypertension are comprised primarily of non-white race/ethnic groups who are far more likely to have resistant hypertension. OSA is associated with resistant hypertension, but there is limited data on associations between sleep characteristics and resistant hypertension. Future studies should investigate whether treating OSA can reduce disparities in resistant hypertension and whether other aspects of sleep also contribute to resistant hypertension.
Sympathetic Nervous System, Sleep, and Hypertension
Abstract
To evaluate the relation between sleep alterations, with or without breathing disorders, and incidence of hypertension and other cardiovascular diseases RECENT FINDINGS: Several studies have clearly shown the mechanisms linking sleep disorders and cardiovascular diseases. The sympathetic hyperactivity seems to play a fundamental role in favoring and sustaining the increase in blood pressure values. Several other mechanisms also contribute to this effect and to the increase cardiovascular risk. The mechanisms responsible for the increase in blood pressure values in subjects with alteration in sleep quantity and quality, with or without breathing disorders, have been clearly established. The recent findings refer to the result of meta-analysis of cross-sectional studies or longitudinal studies showing a significant association between short sleep duration and hypertension. It has also been shown that sleep fragmentation could be considered the main determinant of the sympathetic activation independently of the frequency and severity of oxygen desaturation.
Sleep loss and hypertension: a systematic review
Abstract
Hypertension and insomnia are very common and often coexist. There is evidence to suggest that the increasing prevalence of arterial hypertension in the past decade might be related both to an increased prevalence of insomnia and to the decline of sleep duration due to modern lifestyle. The aim of this paper is to reconsider both the clinical evidence of the relationship between conditions of sleep loss and of perceived impairment in sleep quality with hypertension and the potential pathophysiological mechanisms underlying the biological plausibility of their relationship. Through a systematic search from MEDLINE, EMBASE, PsychINFO we selected articles, which reported experimental sleep deprivation designs, or studied sleep duration or insomnia and their relationship with blood pressure or hypertension in participants over 18 years. This analysis shows that experimental sleep deprivation, short sleep duration, and persistent insomnia are associated with increased blood pressure and increased risk of hypertension, even after controlling for other risk factors. Pathophysiological mechanisms underlying this association might be related to inappropriate arousal ("hyperarousal") due to an overactivation of stress system functions. According this hypothesis, prolonged sleep loss or alterations of sleep quality might act as a neurobiological and physiologic stressor that impair brain functions and contribute to allostatic load, compromising stress resilience and somatic health.
Abstract
Sleep is increasingly recognized as an important lifestyle contributor to health. However, this has not always been the case, and an increasing number of Americans choose to curtail sleep in favor of other social, leisure, or work-related activities. This has resulted in a decline in average sleep duration over time. Sleep duration, mostly short sleep, and sleep disorders have emerged as being related to adverse cardiometabolic risk, including obesity, hypertension, type 2 diabetes mellitus, and cardiovascular disease. Here, we review the evidence relating sleep duration and sleep disorders to cardiometabolic risk and call for health organizations to include evidence-based sleep recommendations in their guidelines for optimal health.
Sleep quality, sleep duration, and their association with hypertension prevalence among low-income oldest-old in a rural area of China: A population-based study
Abstract
Objective
The relationship among sleep quality, sleep duration and hypertension prevalence is controversial in different age groups and genders. This study aimed to investigate sleep quality, sleep duration and their association with hypertension prevalence among low-income oldest-old in a rural area of China.
Methods
A cross-sectional survey was conducted in a representative sample of 1066 adults aged 80–99 years in 2017. Logistic regression analysis was performed.
Results
Among males, sleep durations of <6 h and 6–<7 h were significantly associated with hypertension prevalence, with odds ratios (ORs) of 3.15 (95% confidence interval (CI) 1.37 to 7.23) and 2.38 (95% CI 1.22 to 4.63), respectively. Among females, only the sleep duration of <6 h was associated with increased OR of hypertension of 3.49 (95% CI 1.50 to 8.09). Poor sleep quality was associated with hypertension for both genders (ORmen 1.67, 95% CI 1.12 to 2.49; ORwomen 1.91, 95% CI 1.29 to 2.82). For women, a combination of poor sleep quality and any group of sleep duration, except for 7–<8 h, was associated with higher hypertension prevalence. For men, only the combination of poor sleep quality and short sleep duration (<7 h) was associated with high hypertension prevalence.
Conclusion
Short sleep duration and poor sleep quality are associated with hypertension prevalence of oldest-old. The prevention of hypertension in older adults should be investigated from the perspective of sleep improvement.
Subjective sleep quality, blood pressure, and hypertension: a meta-analysis
Abstract
Sleep quality is an important aspect of sleep, but no meta-analysis has elucidated its relationship with blood pressure (BP) and hypertension. A meta-analysis was conducted in October 2016 using multiple databases, including Embase and Medline. Studies that assessed subjective sleep quality and BP or hypertension were included. Upon full-text evaluation, 29 articles from 45 041 patients were selected, of which 22 articles were included in the meta-analysis and seven were presented narratively. Poor sleep quality was significantly associated with a greater likelihood of hypertension (odds ratio, 1.48; P value = .01). Poor sleepers had higher average systolic BP (mean difference = 4.37, P value = .09) and diastolic BP (mean difference = 1.25, P value = .32) than normal sleepers without statistical significance. Patients with hypertension had significantly worse sleep quality scores (mean difference = 1.51, P value < .01), while BP dippers had significantly better scores (mean difference = −1.67, P value < .01). The findings highlight the relationship between sleep quality and hypertension.
Changes in sleep duration and subsequent risk of hypertension in healthy adults
Abstract
Study Objectives It is unknown whether changes in sleep duration are associated with hypertension risk. The aim of this study was to investigate whether changes in sleep duration were associated with subsequent risk of developing hypertension in young and middle-aged women and men. Methods We analyzed data from 106,385 participants who were free of hypertension and cardiovascular disease during the exposure period and who underwent a health checkup exam, including repeated measures of sleep duration. Results Over 250,907.5 person-years, we documented 4,750 incident cases of hypertension. Both a decrease in sleep duration and persistently short sleep were associated with an elevated risk of hypertension during the subsequent 2.4 years. In analyses for relevant covariates during the exposure period, a decrease of ≥2 hours of sleep and an increase of ≥2 hours of sleep compared with no change in sleep duration were associated with a higher risk of incident hypertension in women (hazard ratio [HR]: 1.46; 95% confidence interval [CI] 1.08–1.98) and men (HR: 1.31; 95% CI 1.10–1.56). Women with persistently shorter sleep durations compared with those who maintained 7 hours of sleep, were at greater risk of developing hypertension during the subsequent follow-up period. Conclusion In this large study of young and middle-aged women and men, we found that individuals with either considerable changes in sleep duration or persistently short sleep were at an increased risk of incident hypertension, underscoring the importance of maintaining moderate sleep duration to prevent hypertension.
Insomnia, Short Sleep Duration, and High Blood Pressure: Recent Evidence and Future Directions for the Prevention and Management of Hypertension
Abstract
Purpose of review: To summarize research from the past 2 years on the association between insomnia, short sleep duration, and hypertension and provide a critical analysis of the evidence and suggestions for future directions in this field.
Recent findings: Evidence indicates that the association between insomnia and elevated blood pressure (BP) or stage 1 and 2 hypertension is stronger in those with chronic insomnia, as compared to those with isolated insomnia symptoms, and primarily found in those with the insomnia with objective short sleep duration phenotype. There is a key gap in ambulatory BP monitoring across the sleep-wake cycle as well as in randomized clinical trials testing the effectiveness of pharmacological or cognitive-behavioral insomnia therapies in lowering BP. Insomnia is a strong candidate to join the list of risk factors for hypertension along with obstructive sleep apnea. In the meantime, chronic insomnia should become part of the routine assessment of patients with elevated BP and should be a source for referral, diagnostic evaluation, and treatment, rather than regarded as a symptom of the underlying medical disorder.
Insomnia and hypertension: A systematic review
Abstract
Insomnia is a prevalent sleep disorder that is associated with a multitude of health consequences. Particularly, insomnia has been associated with cardiovascular disease and its precursors, such as hypertension and blood pressure (BP) non-dipping. The present systematic review aimed to summarize the evidence on the concurrent and prospective associations between insomnia and hypertension and/or BP. Using electronic search engines (PubMed, SCOPUS, PsycINFO), 5,618 articles published from January 1970 to December 2017 were identified, and 64 met the inclusion criteria (26 to 162,121 participants; age range: 18-100; 46.4% male). Insomnia was based on diagnostic or non-diagnostic criteria. Hypertension was based on self-or physician-reports, antihypertensive medication use, and/or measured BP. Findings indicate that when insomnia is frequent, chronic, and/or accompanied with short sleep duration or objective markers of arousal, there is a strong association with hypertension/BP. Based on limited studies, hypertension did not significantly predict future insomnia in middle-aged adults, but did in older adults. Based on a majority of case-control studies, no differences in BP were found between participants with and without insomnia. Further research is needed to identify putative pathophysiological mechanisms underlying the link between insomnia and hypertension. The impact of insomnia therapy on BP should also be further examined in the future.
Sleep, insomnia, and hypertension: current findings and future directions
Abstract
Blood pressure (BP) varies over 24 hours. During normal sleep, BP typically decreases by 10% or more. Research suggests that disordered sleep, particularly sleep deprivation and obstructive sleep apnea, is associated with increased BP and risk of hypertension. Less is known about the relationship between insomnia and hypertension. Population-based studies have reported an association between insomnia symptoms and both prevalent and incident hypertension, particularly in the context of short sleep duration. Furthermore, a number of mechanisms have been proposed to explain the relationship between insomnia and hypertension. However, few studies have examined these proposed mechanisms, and even fewer clinical trials have been conducted to determine if improved sleep improves BP and/or reverses a nondipping BP pattern. Methodological concerns, particularly with respect to the diagnosis of insomnia, no doubt impact the strength of any observed association. Additionally, a large majority of studies have only examined the association between insomnia symptoms and clinic BP. Therefore, future research needs to focus on careful consideration of the diagnostic criteria for insomnia, as well as inclusion of either home BP or ambulatory BP monitoring. Finally, clinical trials aimed at improving the quality of sleep should be conducted to determine if improved sleep impacts 24-hour BP.
Decreased Slow Wave Sleep Increases Risk of Developing Hypertension in Elderly Men
Abstract
The importance of sleep to health and cardiovascular disease has become increasingly apparent. Sleep-disordered breathing, sleep duration, and sleep architecture may all influence metabolism and neurohormonal systems, yet no previous study has evaluated these sleep characteristics concurrently in relation to incident hypertension. Our objective was to determine whether incident hypertension is associated with polysomnography measures of sleep-disordered breathing, sleep duration, and sleep architecture in older men. Participants were 784 community-dwelling, ambulatory men ≥65 years of age (mean age: 75.1±4.9 years) from the Outcomes of Sleep Disorders in Older Men Study who did not have hypertension at the time of their in-home polysomnography sleep studies (2003-2005) and who returned for follow-up (2007-2009). Of 784 older men included in this report, 243 met criteria for incident hypertension after a mean follow-up of 3.4 years. In unadjusted analyses, incident hypertension was associated with increased hypoxemia, increased sleep stages N1 and N2, and decreased stage N3 (slow wave sleep [SWS]). After adjustment for age, nonwhite race, study site, and body mass index, the only sleep index to remain significantly associated with incident hypertension was SWS percentage (odds ratio for lowest to highest quartile of SWS: 1.83 [95% CI: 1.18 to 2.85]). No attenuation of this association was seen after accounting for sleep duration, sleep fragmentation, and indices of sleep-disordered breathing. Percentage time in SWS was inversely associated with incident hypertension, independent of sleep duration and fragmentation, and sleep-disordered breathing. Selective deprivation of SWS may contribute to adverse blood pressure in older men.
Sleep in women: Normal values for sleep stages and position and the effect of age, obesity, sleep apnea, smoking, alcohol and hypertension
Abstract
Objectives: To define normal values for total sleep time, sleep latency, sleep efficiency, sleep stages and sleeping positions in women and to investigate how sleep is affected by age, obesity, sleep apnea, smoking, alcohol dependency and hypertension.
Methods: In a population-based study, 400 Swedish women aged 20-70 years with over-sampling of snorers were investigated using overnight in-home polysomnography. All results are weighted.
Results: The mean normal total sleep time was 392 min, sleep latency 22 min and sleep efficiency 82%. Women spent 31 min in sleep stage 1, 244 min in stage 2, 41 min in stage 3/4 and 76 min in rapid eye movement (REM) sleep. They spent 41% of their sleep time in the supine position, 50% in the lateral position and 9% in the prone position. Multivariate analyses revealed that sleep efficiency was lower in older women and in women with hypertension. Sleep latency was short in women with severe sleep apnea and long in smokers, alcohol-dependent and hypertensive women. Sleep stage 3/4 was inversely related to age and body mass index. Less REM sleep occurred in alcohol-dependent women. Women younger than 45 years old slept a mean of 42% in the lateral position while women of 45 years and older slept 57% in the lateral position (p<0.001).
Conclusions: In this population-based study of women, we present normal values for sleep stages and sleeping position. We conclude that age, body mass index, obstructive sleep apnea, smoking, alcohol and hypertension reduce sleep quality. With age, women spend more time sleeping in the lateral position.
Sleep Structure in Essential Hypertensive Patients: Differences between Dippers and Non-Dippers
Abstract
The objective of this study was to determine whether the macrostructure and microstructure of sleep were altered in non-dipper essential hypertensive patients. Patients included 9 non-dipper essential hypertensive patients and 10 dippers. We measured blood pressure beat-to-beat by Finapres and all stages of sleep by polysomnografically recording simultaneously during spontaneous nocturnal sleep. We analysed blood pressure pattern for 4-min long random periods while the patients were awake and during all stages of sleep; sleep-efficiency (SE), sleep-latency (SL), delta sleep-latency (dL-SL), REM sleep-latency (REM-SL), St. 1, St. 2, St. 3, St. 4 and REM duration and percentage (%) values, and microtructural aspects of sleep (arousal and microarousal temporisation and features). Dipper patients showed a fall in blood pressure (BP) greater than 10% in all stages of NREM sleep; in the non-dipper patients BP fell by less than 10% of waking values in all NREM stages. REM sleep as well as HR were similar in both groups during all stages of sleep. Non-dippers showed the same number of arousals but more microarousals than dippers (p < 0.001). During and after microarousals BP and HR increased in non-dippers, but showed light variation in dippers. Microarousals induced several stage shifts towards lighter sleep. For this reason non-dippers spent less time in stage 4 than dippers (p < 0.001). In conclusion, non-dipper essential hypertensive patients are a subset of patients with central sympathetic hyperactivity responsible for quantitative and qualitative alteration of sleep.
Manifestation of Pulmonary Hypertension During REM Sleep in Obstructive Sleep Apnea Syndrome
Abstract
The effect of sleep stage change on pulmonary circulation has not been well documented in patients with obstructive sleep apnea syndrome (OSAS). We investigated whether or not stage-specific change can affect pulmonary artery pressure (Ppa) in patients with OSAS. Thirty-one patients with OSAS underwent right cardiac catheterization in the daytime and the following night, including 19 patients in whom Ppa could be measured throughout non-rapid eye movement (NREM) and rapid eye movement (REM) sleep. Ten of the 19 patients had daytime pulmonary hypertension (PH) defined by a mean Ppa (Ppa) >/= 20 mm Hg. Then we analyzed Ppa response to hypoxia spontaneously occurring during the period of sleep apnea. The slopes of the regression lines between arterial oxygen saturation measured by pulse oximeter (SpO2) and Ppa curves were almost the same in both NREM and REM patient groups with or without daytime PH, whereas the response curve was significantly shifted upward in REM compared with NREM patients with daytime PH. Furthermore, Ppa was elevated more markedly in association with REM burst, phasic REM, compared with tonic REM. We conclude that vascular tone of pulmonary artery could be elevated in association with REM sleep which is independent of the degree of hypoxia, and that this state-specific change is manifested in patients with daytime PH.
Obstructive Sleep Apnea during REM Sleep and Hypertension. Results of the Wisconsin Sleep Cohort
Abstract
Rationale: Obstructive sleep apnea (OSA) is associated with hypertension.
Objectives: We aimed to quantify the independent association of OSA during REM sleep with prevalent and incident hypertension.
Methods: We included adults enrolled in the longitudinal community-based Wisconsin Sleep Cohort Study with at least 30 minutes of REM sleep obtained from overnight in-laboratory polysomnography. Studies were repeated at 4-year intervals to quantify OSA. Repeated measures logistic regression models were fitted to explore the association between REM sleep OSA and prevalent hypertension in the entire cohort (n = 4,385 sleep studies on 1,451 individuals) and additionally in a subset with ambulatory blood pressure data (n = 1,085 sleep studies on 742 individuals). Conditional logistic regression models were fitted to longitudinally explore the association between REM OSA and development of hypertension. All models controlled for OSA events during non-REM sleep, either by statistical adjustment or by stratification.
Measurements and Main Results: Fully adjusted models demonstrated significant dose-relationships between REM apnea–hypopnea index (AHI) and prevalent hypertension. The higher relative odds of prevalent hypertension were most evident with REM AHI greater than or equal to 15. In individuals with non-REM AHI less than or equal to 5, a twofold increase in REM AHI was associated with 24% higher odds of hypertension (odds ratio, 1.24; 95% confidence interval, 1.08–1.41). Longitudinal analysis revealed a significant association between REM AHI categories and the development of hypertension (P trend = 0.017). Non-REM AHI was not a significant predictor of hypertension in any of the models.
Conclusions: Our findings indicate that REM OSA is cross-sectionally and longitudinally associated with hypertension. This is clinically relevant because treatment of OSA is often limited to the first half of the sleep period leaving most of REM sleep untreated.
Multidimensional fatigue in pulmonary hypertension: prevalence, severity and predictors
Abstract
Pulmonary hypertension is a potentially fatal disease. Despite pharmacological advances in pulmonary hypertension, fatigue remains common in patients with pulmonary hypertension. A convenience sample of 120 participants at an international patient conference completed the Multidimensional Fatigue Inventory (MFI)-20 scale. Data on New York Heart Association Functional Class, body mass index, oxygen use and medication type/use were also collected. There was a high prevalence of "severe" to "very severe" fatigue for each dimension: General Fatigue (60%), Physical Fatigue (55.8%), Reduced Activity (41.7%), Reduced Motivation (32.5%) and Mental Fatigue (27.5%). The mean±sd overall MFI-20 score was 58±5.1. Dimensions with the highest averaged levels were General Fatigue (13.40±3.61), Physical Fatigue (13.23±3.67) and Reduced Activity (11.33±4.16). Body mass index correlated with higher fatigue scores. Phosphodiesterase inhibitor plus endothelin receptor antagonist combination negatively predicted General Fatigue, Physical Fatigue, Reduced Motivation and Reduced Activity. Triple therapy was a significant predictor of General Fatigue, Physical Fatigue and Reduced Activity. There were no significant predictors of Mental Fatigue. Multidimensional fatigue is common and severe in patients with pulmonary hypertension. Phosphodiesterase inhibitor plus endothelin receptor antagonist combination resulted in lower scores in most fatigue dimensions. Comprehensive assessment of fatigue should be considered in the clinical care of patients with pulmonary hypertension and clinical research to develop formal interventions that target this disabling symptom.
Chronic fatigue syndrome and idiopathic intracranial hypertension: Different manifestations of the same disorder of intracranial pressure?
Abstract
Though not discussed in the medical literature or considered in clinical practice, there are similarities between chronic fatigue syndrome and idiopathic intracranial hypertension (IIH) which ought to encourage exploration of a link between them. The cardinal symptoms of each - fatigue and headache - are common in the other and their multiple other symptoms are frequently seen in both. The single discriminating factor is raised intracranial pressure, evidenced in IIH usually by the sign of papilloedema, regarded as responsible for the visual symptoms which can lead to blindness. Some patients with IIH, however, do not have papilloedema and these patients may be clinically indistinguishable from patients with chronic fatigue syndrome. Yet IIH is rare, IIH without papilloedema (IIHWOP) seems rarer still, while chronic fatigue syndrome is common. So are the clinical parallels spurious or is there a way to reconcile these conflicting observations? We suggest that it is a quirk of clinical measurement that has created this discrepancy. Specifically, that the criteria put in place to define IIH have led to a failure to appreciate the existence, clinical significance or numerical importance of patients with lower level disturbances of intracranial pressure. We argue that this has led to a grossly implausible distortion of the epidemiology of IIH such that the milder form of the illness (IIHWOP) is seen as less common than the more severe and that this would be resolved by recognising a connection with chronic fatigue syndrome. We hypothesise, therefore, that IIH, IIHWOP, lesser forms of IIH and an undetermined proportion of chronic fatigue cases are all manifestations of the same disorder of intracranial pressure across a spectrum of disease severity, in which this subset of chronic fatigue syndrome would represent the most common and least severe and IIH the least common and most extreme.
Salt sensitivity and circadian rhythm of blood pressure: the keys to connect CKD with cardiovasucular events
Abstract
In healthy subjects, blood pressure (BP) drops by 10–20% during the night. Conversely, in patients with the salt-sensitive type of hypertension or chronic kidney disease, nighttime BP does not fall, resulting in an atypical pattern of circadian BP rhythm that does not dip. This pattern is referred to as the ‘non-dipper’ pattern. Loss of renal functional reserve, due to either reduced ultrafiltration capacity or enhanced tubular sodium reabsorption, induces the salt-sensitive type of hypertension. When salt intake is excessive in patients with salt-sensitive hypertension, the defect in sodium excretory capability becomes evident, resulting in elevated BP during the night. This nocturnal hypertension compensates for diminished natriuresis during the daytime and enhances pressure natriuresis during the night. Nocturnal hypertension and the non-dipper pattern of circadian BP rhythm cause cardiovascular events. When excess salt intake is loaded in patients who are in a salt-sensitive state, glomerular capillary pressure is also elevated, resulting in glomerular sclerosis and eventual renal failure. In this way, salt sensitivity and excess salt intake contribute to both cardiovascular and renal damage at the same time. We propose that salt sensitivity of BP and excess salt intake have important roles in the genesis of the cardiorenal connection. Salt sensitivity and circadian rhythm of BP are the keys to understanding the connections between cardiovascular and renal complications.
Hypertension and disrupted blood pressure circadian rhythm in Type 2 diabetic db/db mice
Abstract
Human Type 2 diabetes is associated with increased incidence of hypertension and disrupted blood pressure (BP) circadian rhythm. Db/db mice have been used extensively as a model of Type 2 diabetes, but their BP is not well characterized. In this study, we used radiotelemetry to define BP and the circadian rhythm in db/db mice. We found that the systolic, diastolic, and mean arterial pressures were each significantly increased by 11, 8, and 9 mmHg in db/db mice compared with controls. In contrast, no difference was observed in pulse pressure or heart rate. Interestingly, both the length of time db/db mice were active (locomotor) and the intensity of locomotor activity were significantly decreased in db/db mice. In contrast to controls, the 12-h light period average BP in db/db mice did not dip significantly from the 12-h dark period. A partial Fourier analysis of the continuous 72-h BP data revealed that the power and the amplitude of the 24-h period length rhythm were significantly decreased in db/db mice compared with the controls. The acrophase was centered at 0141 in control mice, but became scattered from 1805 to 0236 in db/db mice. In addition to BP, the circadian rhythms of heart rate and locomotor activity were also disrupted in db/db mice. The mean arterial pressure during the light period correlates with plasma glucose, insulin, and body weight. Moreover, the oscillations of the clock genes DBP and Bmal1 but not Per1 were significantly dampened in db/db mouse aorta compared with controls. In summary, our data show that db/db mice are hypertensive with a disrupted BP, heart rate, and locomotor circadian rhythm. Such changes are associated with dampened oscillations of clock genes DBP and Bmal1 in vasculature.
Alterations in heart rate variability and its circadian rhythm in hypertensive patients with left ventricular hypertrophy free of coronary artery disease
Abstract
Heart rate variability (HRV) and its circadian rhythm were evaluated in 22 patients with treated hypertension and left ventricular hypertrophy in whom coronary artery disease was excluded by stress thallium or angiography. By using 24-hour Holter monitoring, HRV and its spectral components were measured. Findings were compared with 11 age-matched normal controls. The difference between mean R-R intervals during sleep (11 PM to 7 AM) and while awake (9 AM to 9 PM) (73 +/- 33 vs 263 +/- 63 msec, p < 0.0001) and the mean 24-hour SD of the R-R intervals (55 +/- 6.3 vs 93 +/- 11, p < 0.0001) were lower among the hypertensive patients compared with controls. The percentage of difference between successive R-R intervals that exceeded 50 msec, a measure of parasympathetic tone, was also lower among the hypertensive patients (6.8 +/- 7.1 vs 13.6 +/- 8.9, p < 0.002); it increased at night and decreased during the day among the controls, and this circadian rhythm was blunted among the patients. Spectral analysis showed that power in the high-frequency range (0.15 to 0.40 Hz) was lower among the hypertensive patients during 21 of 24 hours but that the difference was statistically significant only during 9 hours (p ranging from < 0.05 to 0.009). Power in the low-frequency range (0.04 to 015 Hz) was lower at night, increased in the morning, and higher during the day among controls; this circadian rhythm was absent among hypertensive patients.(ABSTRACT TRUNCATED AT 250 WORDS)
Circadian rhythms of atrial natriuretic peptide, renin, aldosterone, cortisol, blood pressure and heart rate in normal and hypertensive subjects.
Abstract
The occurrence and extent of a circadian rhythm in the circulating concentrations of atrial natriuretic peptide (ANP) are still matters of controversy. Only a few data are available in humans relating the time structure of plasma ANP levels with the circadian patterns of other hormones and cardiovascular variables. In a group of hospitalized normal volunteers (six men and four women, 16-76 years old), and in a group of hospitalized hypertensives (seven men and three women, 18-76 years old), we investigated the circadian variability of ANP and its temporal relationship with the circadian rhythms of blood pressure (BP) and heart rate (HR), and plasma renin activity (PRA), plasma aldosterone (PA) and plasma cortisol (PC) levels, by using a chronobiological inferential statistic method. At the end of a synchronizing period of 1 week (the diet and daily schedule were standardized), the subjects underwent automatic BP and HR monitoring, and blood sampling for 24 h. A statistically significant mean circadian rhythm was demonstrated for ANP, BP, HR, PRA, PA and PC in both normal and hypertensive subjects. The mean circadian acrophase of ANP (calculated to occur at around 04.00 h) anticipated the corresponding acrophases of the other hormones; BP and HR rhythms appeared to be in antiphase with ANP rhythm, i.e. the peak of BP and HR rhythms more or less coincided with the trough in ANP rhythm. A significant increase in the daily levels (assessed by the circadian mesor) of ANP was present in hypertensive subjects when compared with normal controls. In essential hypertension the circadian rhythm of ANP was set at higher circulating levels, but otherwise it was similar to the circadian rhythm found in normals. ANP mesors correlated significantly with renin and aldosterone mesors in normal subjects but not in hypertensive patients. ANP appears to anticipate awakening in its circadian periodic rise. On the basis of the considerable acrophase asynchronism, it seems possible to exclude any causal relations between the periodic changes of ANP and the rhythmic fluctuations of the other hormones that we studied. In contrast, important relations may be hypothesized between ANP levels and BP and HR values, on the basis of their antiphase rhythms.
Circadian rhythm of blood pressure and the relation to cardiovascular events
Abstract
Incidences of potentially life-threatening cardiovascular events display a diurnal pattern, tending to be higher in the morning than at other times of day. The recording of blood pressure at pre-defined intervals under everyday circumstances is facilitated by ambulatory blood pressure monitoring (ABPM). This technique shows that systolic and diastolic blood pressures display a circadian rhythm in most individuals. Typically, at the end of the night on arousal, blood pressure surges. This surge coincides with increased cardiovascular events. A recent prospective study conducted in Japan, where the incidence of stroke is high, provides further evidence for the link between cardiovascular events and morning blood pressure surge. Prevalence of both silent ischaemic events and multiple cerebrovascular infarcts was highest among the elderly subjects studied, with the largest increase in blood pressure on awakening. An increased risk of cardiovascular morbidity and mortality is also seen in 'non-dippers' (i.e. individuals in whom the normal nocturnal fall in blood pressure is absent or blunted). ABPM is superior to clinic blood pressure in predicting cardiovascular morbidity and mortality, and this suggests that 24-h blood pressure control may be necessary to gain complete benefit from blood pressure-lowering therapy. Antihypertensive agents with a long duration of action have the potential to provide blood pressure control throughout the dosing interval and thus cover the critical early morning period when the blood pressure surges. Clinical studies that have compared telmisartan with shorter-acting angiotensin II receptor blockers and angiotensin-converting enzyme inhibitors demonstrate that telmisartan has a sustained duration of action, with proven efficacy over the entire 24-h period between doses, including the critical early morning period.
Aging
Objective and subjective sleep measures are associated with neurocognition in aging adults with and without HIV
Abstract
Poor sleep quality is related to worse neurocognition in older adults and in people with HIV (PWH); however, many previous studies have relied only on self-report sleep questionnaires, which are inconsistently correlated with objective sleep measures. We examined relationships between objective and subjective sleep quality and neurocognition in persons with and without HIV, aged 50 and older. Method: Eighty-five adults (PWH n = 52, HIV-negative n = 32) completed comprehensive neuropsychological testing to assess global and domain-specific neurocognition. Objective sleep quality was assessed with wrist actigraphy (total sleep time, efficiency, sleep fragmentation) for five to 14 nights. Subjective sleep quality was assessed with the Pittsburgh Sleep Quality Index. Results: Objective and subjective sleep measures were unrelated (p's > 0.30). Compared to HIV-negative participants, PWH had greater sleep efficiency (80% vs. 75%, p = 0.05) and were more likely to be using prescription and/or over the counter sleep medication (p = 0.04). In the whole sample, better sleep efficiency (p < 0.01) and greater total sleep time (p = 0.05) were associated with better learning. Less sleep fragmentation was associated with better learning (p < 0.01) and recall (p = 0.04). While PWH had slightly stronger relationships between total sleep time and sleep fragmentation, it is not clear if these differences are clinically meaningful. Better subjective sleep quality was associated with better executive function (p < 0.01) and working memory (p = 0.05); this relationship was primarily driven by the HIV-negative group. Conclusions: Objective sleep quality was associated with learning and recall whereas subjective sleep quality was associated with executive function and working memory. Therefore, assessing objective and subjective sleep quality could be clinically useful, as they are both related to important domains of cognition frequently impacted in HIV-associated neurocognitive disorders as well as neurodegenerative disorders associated with aging. Future studies should evaluate if behavioral sleep interventions can improve neurocognition.
Buying time: a proof-of-concept randomized controlled trial to improve sleep quality and cognitive function among older adults with mild cognitive impairment
Abstract
Background: Current evidence suggests that good quality sleep is associated with preserved cognitive function and reduced dementia risk in older adults. Sleep complaints are especially common among older adults with mild cognitive impairment (MCI), and this may contribute to their increased risk for progression to dementia. Thus, improving their sleep may be important for maintaining their cognitive health. Chronotherapy is a set of intervention strategies that can improve sleep quality through strengthening the entrainment of the biological clock to the solar light-dark cycle, and includes strategies such as (1) bright light therapy (BLT); (2) physical activity (PA); and (3) good sleep hygiene. Of these strategies, BLT is the most potent and is based on providing individualized timing to entrain circadian rhythms. Thus, a personalized chronotherapy intervention of individually timed BLT and individually tailored PA promotion, in conjunction with general sleep hygiene education may promote older adult sleep quality. We therefore aim to carry out a proof-of-concept randomized controlled trial (RCT) to examine the efficacy of such a personalized chronotherapy intervention to improve sleep quality among older adults with MCI.
Methods/design: This was a 24-week RCT of a personalized chronotherapy intervention aimed to primarily improve sleep quality as measured by the MotionWatch8©. Participants in the personalized chronotherapy group (INT) will receive four once-weekly, general sleep hygiene education classes, followed by 20 weeks of (1) individually timed BLT and (2) bi-weekly, individually tailored PA counseling phone calls in conjunction with receiving a consumer-available PA tracker-the Fitbit® Flex™. Ninety-six adults (aged 65-85 years) classified as having MCI (i.e., Mini-Mental State Exam (MMSE) ≥ 24; Montreal Cognitive Assessment (MoCA) ≤ 26; without dementia or significant functional impairment) will be randomized to either INT or a waitlist control group (CON).
Discussion: The results of this trial will help determine if a personalized chronotherapy intervention that includes individually timed BLT and individually tailored PA promotion, along with general sleep hygiene education can promote sleep quality among older adults at increased risk for dementia. Our results will help inform best practices for promoting sleep quality among older adults with MCI.
Insomnia in the Older Adult
Abstract
Although insomnia is not a normal part of the aging process, its prevalence increases with age. Factors such as medications and medical and psychiatric disorders can increase the risk for insomnia. To diagnose insomnia, it is important for older adults to complete comprehensive sleep and health histories. Cognitive-behavioral therapy for insomnia, which includes stimulus control, sleep restriction, sleep hygiene, and cognitive therapy, is the recommended first-line treatment of insomnia and is more effective than medications for the long-term management of insomnia. Medications, such as benzodiazepines and antidepressants, should be avoided for the treatment of insomnia in older adults.
Sleep in Women Across the Life Span
Abstract
There are many ways in which women experience sleep differently from men. Women contending with distinct sleep challenges respond differently to sleep disorders, as well as sleep deprivation and deficiency, and face particular health outcomes as a result of poor sleep. Idiosyncrasies, including changes that occur with the biological life cycles of menstruation, pregnancy, and menopause, make the understanding of sleep in women an important topic to study. Each phase of a woman's life, from childhood to menopause, increases the risk of sleep disturbance in unique ways that may require distinct management. Indeed, new research is unraveling novel aspects of sleep pathology in women and the fundamental role that sex hormones play in influencing sleep regulation and arousals and possibly outcomes of sleep conditions. Moreover, studies indicate that during times of hormonal change, women are at an increased risk for sleep disturbances such as poor sleep quality and sleep deprivation, as well as sleep disorders such as OSA, restless legs syndrome, and insomnia. This article reviews sleep changes in female subjects from neonatal life to menopause.
Sleep disorders in the elderly: a growing challenge
Abstract
In contrast to newborns, who spend 16-20 h in sleep each day, adults need only about sleep daily. However, many elderly may struggle to obtain those 8 h in one block. In addition to changes in sleep duration, sleep patterns change as age progresses. Like the physical changes that occur during old age, an alteration in sleep pattern is also a part of the normal ageing process. As people age, they tend to have a harder time falling asleep and more trouble staying asleep. Older people spend more time in the lighter stages of sleep than in deep sleep. As the circadian mechanism in older people becomes less efficient, their sleep schedule is shifted forward. Even when they manage to obtain 7 or 8 h sleep, they wake up early, as they have gone to sleep quite early. The prevalence of sleep disorders is higher among older adults. Loud snoring, which is more common in the elderly, can be a symptom of obstructive sleep apnoea, which puts a person at risk for cardiovascular diseases, headaches, memory loss, and depression. Restless legs syndrome and periodic limb movement disorder that disrupt sleep are more prevalent in older persons. Other common medical problems of old age such as hypertension diabetes mellitus, renal failure, respiratory diseases such as asthma, immune disorders, gastroesophageal reflux disease, physical disability, dementia, pain, depression, and anxiety are all associated with sleep disturbances.
Sleep, Noninvasive Brain Stimulation, and the Aging Brain: Challenges and Opportunities
Abstract
As we age, sleep patterns undergo severe modifications of their micro and macrostructure, with an overall lighter and more fragmented sleep structure. In general, interventions targeting sleep represent an excellent opportunity not only to maintain life quality in the healthy aging population, but also to enhance cognitive performance and, when pathology arises, to potentially prevent/slow down conversion from e.g. Mild Cognitive Impairment (MCI) to Alzheimer's Disease (AD). Sleep abnormalities are, in fact, one of the earliest recognizable biomarkers of dementia, being also partially responsible for a cascade of cortical events that worsen dementia pathophysiology, including impaired clearance systems leading to build-up of extracellular amyloid-β (Aβ) peptide and intracellular hyperphosphorylated tau proteins. In this context, Noninvasive Brain Stimulation (NiBS) techniques, such as transcranial electrical stimulation (tES) and transcranial magnetic stimulation (TMS), may help investigate the neural substrates of sleep, identify sleep-related pathology biomarkers, and ultimately help patients and healthy elderly individuals to restore sleep quality and cognitive performance. However, brain stimulation applications during sleep have so far not been fully investigated in healthy elderly cohorts, nor tested in AD patients or other related dementias. The manuscript discusses the role of sleep in normal and pathological aging, reviewing available evidence of NiBS applications during both wakefulness and sleep in healthy elderly individuals as well as in MCI/AD patients. Rationale and details for potential future brain stimulation studies targeting sleep alterations in the aging brain are discussed, including enhancement of cognitive performance, overall quality of life as well as protein clearance.
Understanding the interplay of sleep and aging: Methodological challenges
Abstract
In quest of new avenues to explain, predict, and treat pathophysiological conditions during aging, research on sleep and aging has flourished. Despite the great scientific potential to pinpoint mechanistic pathways between sleep, aging, and pathology, only little attention has been paid to the suitability of analytic procedures applied to study these interrelations. On the basis of electrophysiological sleep and structural brain data of healthy younger and older adults, we identify, illustrate, and resolve methodological core challenges in the study of sleep and aging. We demonstrate potential biases in common analytic approaches when applied to older populations. We argue that uncovering age-dependent alterations in the physiology of sleep requires the development of adjusted and individualized analytic procedures that filter out age-independent interindividual differences. Age-adapted methodological approaches are thus required to foster the development of valid and reliable biomarkers of age-associated cognitive pathologies.
Sleep fragmentation, microglial aging, and cognitive impairment in adults with and without Alzheimer's dementia
Abstract
Sleep disruption is associated with cognitive decline and dementia in older adults; however, the underlying mechanisms are unclear. In rodents, sleep disruption causes microglial activation, inhibition of which improves cognition. However, data from humans are lacking. We studied participants in two cohort studies of older persons-the Rush Memory and Aging Project and the Religious Orders Study. We assessed sleep fragmentation by actigraphy and related this to cognitive function, to neocortical microglial marker gene expression measured by RNA sequencing, and to the neocortical density of microglia assessed by immunohistochemistry. Greater sleep fragmentation was associated with higher neocortical expression of genes characteristic of aged microglia, and a higher proportion of morphologically activated microglia, independent of chronological age- and dementia-related neuropathologies. Furthermore, these were, in turn, associated with worse cognition. This suggests that sleep fragmentation is accompanied by accelerated microglial aging and activation, which may partially underlie its association with cognitive impairment.
Sleep as a Therapeutic Target in the Aging Brain
Abstract
Sleep is a behavioral phenomenon conserved among mammals and some invertebrates, yet the biological functions of sleep are still being elucidated. In humans, sleep time becomes shorter, more fragmented, and of poorer quality with advancing age. Epidemiologically, the development of age-related neurodegenerative diseases such as Alzheimer's and Parkinson's disease is associated with pronounced sleep disruption, whereas emerging mechanistic studies suggest that sleep disruption may be causally linked to neurodegenerative pathology, suggesting that sleep may represent a key therapeutic target in the prevention of these conditions. In this review, we discuss the physiology of sleep, the pathophysiology of neurodegenerative disease, and the current literature supporting the relationship between sleep, aging, and neurodegenerative disease.
Sleep in Normal Aging
Abstract
Sleep patterns change with aging, independent of other factors, and include advanced sleep timing, shortened nocturnal sleep duration, increased frequency of daytime naps, increased number of nocturnal awakenings and time spent awake during the night, and decreased slow wave sleep. Most of these changes seem to occur between young and middle adulthood; sleep parameters remain largely unchanged among healthy older adults. The circadian system and sleep homeostatic mechanisms become less robust with normal aging. The amount and pattern of sleep-related hormone secretion change as well. The causes of sleep disturbances in older adults are multifactorial.
Sleep in the Aging Population
Abstract
There are normal changes to sleep architecture throughout the lifespan. There is not, however, a decreased need for sleep and sleep disturbance is not an inherent part of the aging process. Sleep disturbance is common in older adults because aging is associated with an increasing prevalence of multimorbidity, polypharmacy, psychosocial factors affecting sleep, and certain primary sleep disorders. It is also associated with morbidity and mortality. Because many older adults have several factors from different domains affecting their sleep, these complaints are best approached as a multifactorial geriatric health condition, necessitating a multifaceted treatment approach.
Low-grade inflammation in the relationship between sleep disruption, dysfunctional adiposity, and cognitive decline in aging
Abstract
Aging is characterized by a progressive increase in proinflammatory status. This state, known as inflammaging, has been associated with cognitive decline in normal and pathological aging. However, this relationship has been inconsistently reported, likely because it is conditioned by other factors also affected by the aging process. Sleep and adiposity are two factors in particular that show significant alterations with aging and have been related to both cognitive decline and inflammaging. Given the consequences this state also has for brain integrity and cognition, we discuss here evidence supporting the potential mediating role of chronic low-grade systemic inflammation in the complex relationship between impaired sleep, dysfunctional adiposity, and cognitive decline through the common pathway of neuroinflammation. This review proposes a multi-factor model of aging-related cognitive decline that highlights the reciprocal interactions between sleep, the circadian system, and inflammation on the one hand, and between sleep, adiposity, and hormone resistance on the other. The model identifies sleep and adiposity as modifiable lifestyle factors that can be targeted to maximize cognitive function and quality of life in the elderly.
Sleep Quality, Duration, and Associated Sexual Function at Older Age: Findings from the English Longitudinal Study of Ageing
Abstract
Introduction: One factor that may plausibly be associated with sexual dysfunction is sleep disturbance. Like sexual problems, complaints of sleep disturbance increase with age and are commonly reported by older adults.
Aims: To examine associations between sleep quality, duration, and a range of sexual problems in a large, representative sample of older adults.
Methods: Data were from 2,568 men and 1,376 women (age ≥50 years) participating in Wave 6 of the English Longitudinal Study of Ageing (2012-2013). Sleep quality, duration, and problems with erectile function, sexual arousal, and orgasmic experience were self-reported; associations were examined using logistic regression models. Covariates included age, ethnicity, partner status, wealth, limiting long-standing illness, smoking, alcohol consumption, physical activity, and depressive symptoms.
Main outcome measure: Participants self-reported problems with erectile function, sexual arousal, and orgasmic experience.
Results: In women, moderate (odds ratio [OR] = 1.53, 95% CI 1.09-2.13, P = .013) and low sleep quality (OR = 1.70, 95% CI 1.24-2.32, P = .001) were associated with increased odds of arousal problems relative to high sleep quality. In men, moderate sleep quality was associated with increased odds of erectile difficulties (OR = 1.47, 95% CI 1.16-1.85, P = .001), the difference between low and high sleep quality did not reach statistical significance (OR = 1.24, 95% CI 0.97-1.58, P = .091). Sleep quality was not associated with difficulty achieving an orgasm in men, but in women low sleep quality was associated with increased odds of orgasmic difficulty (OR = 1.63, 95% CI 1.18-2.25, P = .003). No associations between sleep duration and problems with sexual function were observed in women, but, in men, long sleep was associated with higher odds of difficulty achieving orgasm (OR = 1.75, 95% CI 1.04-2.95, P = 0.036) relative to optimal sleep duration.
Clinical implications: Older adults presenting sleep problems should be screened for sexual dysfunction and vice versa.
Strength & limitations: Strengths of this study include the large representative sample of older English adults, the assessment of several aspects of sexual dysfunction and sleep, and the inclusion of potentially important confounding variables into statistical models. However, the study was cross-sectional, meaning we were unable to ascertain the direction of the observed associations.
Conclusion: Sleep problems are associated with sexual dysfunction in older English adults, although some variation is noted between men and women. Smith L, Grabovac I, Veronese N, et al. Sleep Quality, Duration, and Associated Sexual Function at Older Age: Findings From the English Longitudinal Study of Ageing. J Sex Med 2019;16:427-433.
Sleep Counteracts Aging Phenotypes to Survive Starvation-Induced Developmental Arrest in C. elegans
Abstract
Sleep is ancient and fulfills higher brain functions as well as basic vital processes. Little is known about how sleep emerged in evolution and what essential functions it was selected for. Here, we investigated sleep in Caenorhabditis elegans across developmental stages and physiological conditions to find out when and how sleep in a simple animal becomes essential for survival. We found that sleep in worms occurs during most stages and physiological conditions and is typically induced by the sleep-active RIS neuron. Food quality and availability determine sleep amount. Extended starvation, which induces developmental arrest in larvae, presents a major sleep trigger. Conserved nutrient-sensing regulators of longevity and developmental arrest, AMP-activated kinase and FoxO, act in parallel to induce sleep during extended food deprivation. These metabolic factors can act in multiple tissues to signal starvation to RIS. Although sleep does not appear to be essential for a normal adult lifespan, it is crucial for survival of starvation-induced developmental arrest in larvae. Rather than merely saving energy for later use, sleep counteracts the progression of aging phenotypes, perhaps by allocating resources. Thus, sleep presents a protective anti-aging program that is induced by nutrient-sensing longevity pathways to survive starvation-induced developmental arrest. All organisms are threatened with the possibility of experienced famine in their life, which suggests that the molecular coupling of starvation, development, aging, and sleep was selected for early in the evolution of nervous systems and may be conserved in other species, including humans.
Association between Sleep Quality and Body Composition in Sedentary Middle-Aged Adults
Abstract
Background: Ageing is associated with sleep pattern changes and body composition changes, which are related to several diseases. Purpose: This study aimed to analyse the association between sleep quality and an extensive set of body composition parameters (waist-hip ratio, body mass index, bone mineral content, bone mineral density, lean mass, lean mass index, fat mass, fat mass percentage, fat mass index, visceral adipose tissue) and sleep quality in sedentary middle-aged adults. We also aimed to evaluate whether the possible associations accord between subjective and objective measurements of sleep quality. Methods: 74 (39 women) middle-aged sedentary adults (40⁻65 years old) participated in the present study. The sleep quality was assessed using the Pittsburgh sleep quality index (PSQI) scale and accelerometers. A PSQI global score more than 5 indicates poor sleep quality. Weight, height, waist and hip circumferences were measured, and body mass index and waist-hip ratio were also calculated. Body composition was assessed with a dual-energy X-ray absorptiometry scanner. Results: The PSQI global score was negatively associated with bone mineral content, bone mineral density, lean mass, lean mass index and positively associated with fat mass percentage. No association was found between accelerometer parameters and body composition variables. Conclusion: We showed that a subjective poor sleep quality was negatively associated with bone mineral content (BMC), bone mineral density (BMD), lean mass and lean mass index (LMI) whereas was positively associated with fat mass percentage in middle-aged adults. We also observed that these associations did not accord with objective sleep quality measurements.
Sleep Disorders in the Elderly
Abstract
Although some physiologic changes in sleep are a normal part of the aging process, other sleep complaints made by elderly patients can indicate a primary or secondary sleep disorder. It is important to recognize the difference between normal age-related changes and what may require further testing to make an accurate diagnosis. Proper diagnosis and treatment of sleep disorders can improve the quality of life and safety for the elderly and their families.
Does poor sleep quality affect skin ageing?
Abstract
Background: Sleep is important for growth and renewal of multiple physiological systems. The effects of chronic poor sleep quality on human skin function and visible signs of ageing have not been elucidated.
Aim: To evaluate the effect of chronic poor sleep quality on measures of skin health and ageing. Self-perceived satisfaction with appearance was also assessed.
Methods: 60 healthy caucasian women, who were categorized as poor quality sleepers [Pittsburg Sleep Quality Index (PSQI) > 5, sleep duration ≤ 5 h] or good quality sleepers (PSQI ≤ 5, sleep duration 7-9 h). A validated clinical tool, SCINEXA(TM) , was used to assess intrinsic and extrinsic skin ageing. Dark under-eye circles were evaluated using standardized photos. Measurement of in vivo transepidermal water loss (TEWL) was used to assess recovery of the skin barrier after tape stripping. Subjects were exposed to simulated solar ultraviolet light, and recovery from erythema was monitored. Subjects also completed a questionnaire evaluating self-perception of attractiveness.
Results: Good sleepers had significantly lower intrinsic skin ageing scores by SCINEXA(TM) . At baseline, poor sleepers had significantly higher levels of TEWL. At 72 h after tape stripping, good sleepers had 30% greater barrier recovery compared with poor sleepers. At 24 h after exposure to ultraviolet light, good sleepers had significantly better recovery from erythema. Good sleepers also reported a significantly better perception of their appearance and physical attractiveness compared with poor sleepers.
Conclusions: This study indicates that chronic poor sleep quality is associated with increased signs of intrinsic ageing, diminished skin barrier function and lower satisfaction with appearance.
Sleep-dependent memory consolidation in healthy aging and mild cognitive impairment
Abstract
Sleep quality and architecture as well as sleep's homeostatic and circadian controls change with healthy aging. Changes include reductions in slow-wave sleep's (SWS) percent and spectral power in the sleep electroencephalogram (EEG), number and amplitude of sleep spindles, rapid eye movement (REM) density and the amplitude of circadian rhythms, as well as a phase advance (moved earlier in time) of the brain's circadian clock. With mild cognitive impairment (MCI) there are further reductions of sleep quality, SWS, spindles, and percent REM, all of which further diminish, along with a profound disruption of circadian rhythmicity, with the conversion to Alzheimer's disease (AD). Sleep disorders may represent risk factors for dementias (e.g., REM Behavior Disorder presages Parkinson's disease) and sleep disorders are themselves extremely prevalent in neurodegenerative diseases. Working memory , formation of new episodic memories, and processing speed all decline with healthy aging whereas semantic, recognition, and emotional declarative memory are spared. In MCI, episodic and working memory further decline along with declines in semantic memory. In young adults, sleep-dependent memory consolidation (SDC) is widely observed for both declarative and procedural memory tasks. However, with healthy aging, although SDC for declarative memory is preserved, certain procedural tasks, such as motor-sequence learning, do not show SDC. In younger adults, fragmentation of sleep can reduce SDC, and a normative increase in sleep fragmentation may account for reduced SDC with healthy aging. Whereas sleep disorders such as insomnia, obstructive sleep apnea, and narcolepsy can impair SDC in the absence of neurodegenerative changes, the incidence of sleep disorders increases both with normal aging and, further, with neurodegenerative disease. Specific features of sleep architecture, such as sleep spindles and SWS are strongly linked to SDC. Diminution of these features with healthy aging and their further decline with MCI may account for concomitant declines in SDC. Notably these same sleep features further markedly decline, in concert with declining cognitive function, with the progression to AD. Therefore, progressive changes in sleep quality, architecture, and neural regulation may constitute a contributing factor to cognitive decline that is seen both with healthy aging and, to a much greater extent, with neurodegenerative disease.
Subjective and Objective Sleep Quality and Aging in the Sleep Heart Health Study
AbstractOBJECTIVES: To examine the extent to which subjective and objective sleep quality are related to age independent of chronic health conditions.
DESIGN: Cross‐sectional study.
SETTING: The Sleep Heart Health Study (SHHS) is a multicenter study designed to determine the cardiovascular consequences and the natural history of sleep disordered breathing.
PARTICIPANTS: Five thousand four hundred seven community‐dwelling adults who participated in the SHHS (mean age 63, range 45–99; 52% women).
MEASUREMENTS: Unattended home polysomnography (PSG) and sleep questionnaires.
RESULTS: Older age was associated with shorter sleep time, diminished sleep efficiency, and more arousals in men and women. In men, age was independently associated with more Stage 1 and Stage 2 sleep and less slow‐wave (Stage 3 to 4) and rapid eye movement sleep. In women, older age was less strongly associated according to linear trend with sleep stage. Conversely, poor subjective sleep quality was not associated with older age in men, but older women had more trouble falling asleep, and there was a trend toward older women having more problems with waking up during the night and waking up too early. Associations between self‐report and directly measured sleep time and sleep latency were low to moderate across age groups (correlation coefficient=0.06–0.32).
CONCLUSION: Older age was more strongly associated with poorer sleep according to PSG in men than women, yet the subjective report of poor sleep with older age was stronger in women. The higher prevalence of chronic health conditions, including sleep apnea, in older adults did not explain changes of sleep parameters with aging and age–sex differences in these relationships.
Challenging sleep in aging: the effects of 200 mg of caffeine during the evening in young and middle‐aged moderate caffeine consumers
SummaryThe aim of this study was to evaluate the effects of a 200‐mg administration of caffeine on polysomnographic sleep variables and quantitative sleep electroencephalography (EEG) in 12 young (20–30 years) and 12 middle‐aged (40–60 years) moderate caffeine consumers (one to three cups of coffee per day). All subjects were submitted to both a caffeine (200 mg) and placebo (lactose) condition in a double‐blind cross‐over design. The conditions were separated by 1 week. Compared with the placebo condition, the evening ingestion of caffeine lengthened sleep latency, reduced sleep efficiency, and decreased sleep duration and amount of stage 2 sleep in both age groups. Caffeine also reduced spectral power in delta frequencies in frontal, central and parietal brain areas, but not in prefrontal (PF) and occipital regions. Moreover, caffeine increased spectral power in beta frequencies in frontal and central brain areas in both age groups. A suppression of spectral power in the PF area in low delta frequencies (0.5–1.00 Hz) and a rise in spectral power in the parietal region in high alpha (10.00–12.00 Hz) and beta frequencies (17.00–21.00, 23.00–25.00, 27.00–29.00 Hz) occurred solely in middle‐aged subjects. No such changes were noticeable in young subjects. Generally, caffeine produced similar effects in young and middle‐aged subjects. Only a few frequency bins showed more effects of caffeine in middle‐aged subjects compared with young subjects. Furthermore, sleep EEG results do not entirely support the hypothesis that caffeine fully mimics the effects of a reduction of homeostatic sleep propensity when following a normal sleep–wake cycle.
Sleep Latency in Men and Sleep Duration in Women Can Be Frailty Markers in Community-Dwelling Older Adults: The Korean Frailty and Aging Cohort Study (KFACS)
Abstract
Objectives
To test whether sleep disturbances are associated with frailty in older men and women.
Design
Cross-sectional analysis of cohort study data. The participants were 1168 community-dwelling older adults aged 70 to 84 years who took part in the Korean Frailty and Aging Cohort Study and completed both self-reported sleep parameters and assessment of frailty. Univariate and multivariate survey logistic regression models were used to calculate odds ratios (OR) with 95% confidence intervals (CI) for frailty. Frailty was defined using the Fried’s criteria.
Results
Frailty was associated with sleep latency in men. The odds ratio for this association was 3.39 (95% CI 1.31-8.76) after adjusting for age, body mass index (BMI), physical activity, and select comorbidities, and 2.16 (95% CI 0.75-6.23) after further adjusting for depression. Frailty was associated with long sleep duration of more than 8 hours a night in women. The odds ratio for this association was 3.95 (95% CI, 1.27-12.33) after adjusting for age, BMI, physical activity, select comorbidities, and the number of medications.
Conclusion
Prolonged sleep latency (≥60 minutes) in men and long sleep duration (>8hr per night) in women were each independently associated with higher odds of frailty. Long sleep latency in elderly men and long sleep duration in elderly women may suggest they have a high chance of frailty.
Aging-Related Sleep Changes
Normal aging is accompanied by changes in the sleep quality, quantity, and architecture. Specifically, there appears to be a measurable decrease in the ability of the healthy elderly to initiate and maintain sleep, accompanied by a decrease in the proportion of the deeper, more restorative slow-wave sleep and rapid eye movement sleep. There is epidemiologic evidence that this impaired ability to initiate, maintain, and ultimately achieve good quality, optimal sleep may be a marker of increased mortality and neurocognitive dysfunction. Possible mechanisms related to these age-related changes in sleep include age-related changes in circadian modulation, homeostatic factors, cardiopulmonary function , and endocrine function. This article describes the normal changes in sleep physiology in the elderly.
Cellular Aging and Restorative Processes: Subjective Sleep Quality and Duration Moderate the Association between Age and Telomere Length in a Sample of Middle-Aged and Older Adults
Abstract
Study Objectives:
To examine whether subjective sleep quality and sleep duration moderate the association between age and telomere length (TL).
Design:
Participants completed a demographic and sleep quality questionnaire, followed by a blood draw.
Setting:
Social Neuroscience Laboratory.
Participants:
One hundred fifty-four middle-aged to older adults (age 45–77 y) participated. Participants were excluded if they were on immunosuppressive treatment and/or had a disease with a clear immunologic (e.g., cancer) component.
Interventions:
N/A.
Measurements and Results:
Subjective sleep quality and sleep duration were assessed using the Pittsburgh Sleep Quality Index (PSQI) and TL was determined using peripheral blood mononuclear cells (PBMCs). There was a significant first-order negative association between age and TL. Age was also negatively associated with the self-reported sleep quality item and sleep duration component of the PSQI. A significant age × self-reported sleep quality interaction revealed that age was more strongly related to TL among poor sleepers, and that good sleep quality attenuated the association between age and TL. Moreover, adequate subjective sleep duration among older adults (i.e. greater than 7 h per night) was associated with TL comparable to that in middle-aged adults, whereas sleep duration was unrelated to TL for the middle-aged adults in our study.
Conclusions:
The current study provides evidence for an association between sleep quality, sleep duration, and cellular aging. Among older adults, better subjective sleep quality was associated with the extent of cellular aging, suggesting that sleep duration and sleep quality may be added to a growing list of modifiable behaviors associated with the adverse effects of aging.
Association between Sleep Duration and Mortality Is Mediated by Markers of Inflammation and Health in Older Adults: The Health, Aging and Body Composition Study
Abstract
Study Objective:
Inflammation may represent a common physiological pathway linking both short and long sleep duration to mortality. We evaluated inflammatory markers as mediators of the relationship between sleep duration and mortality in community-dwelling older adults.
Design:
Prospective cohort with longitudinal follow-up for mortality outcomes.
Setting:
Pittsburgh, Pennsylvania, and Memphis, Tennessee.
Participants:
Participants in the Health, Aging and Body Composition (Health ABC) Study (mean age 73.6 ± 2.9 years at baseline) were sampled and recruited from Medicare listings.
Measurements and Results:
Baseline measures of subjective sleep duration, markers of inflammation (serum interleukin-6, tumor necrosis factor-α, and C-reactive protein) and health status were evaluated as predictors of all-cause mortality (average follow-up = 8.2 ± 2.3 years). Sleep duration was related to mortality, and age-, sex-, and race-adjusted hazard ratios (HR) were highest for those with the shortest (< 6 h HR: 1.30, CI: 1.05–1.61) and longest (> 8 h HR: 1.49, CI: 1.15–1.93) sleep durations. Adjustment for inflammatory markers and health status attenuated the HR for short (< 6 h) sleepers (HR = 1.06, 95% CI = 0.83–1.34). Age-, sex-, and race-adjusted HRs for the > 8-h sleeper group were less strongly attenuated by adjustment for inflammatory markers than by other health factors associated with poor sleep with adjusted HR = 1.23, 95% CI = 0.93–1.63. Inflammatory markers remained significantly associated with mortality.
Conclusions:
Inflammatory markers, lifestyle, and health status explained mortality risk associated with short sleep, while the mortality risk associated with long sleep was explained predominantly by lifestyle and health status.
Melatonin Regulates Aging and Neurodegeneration through Energy Metabolism, Epigenetics, Autophagy and Circadian Rhythm Pathways
Abstract
Brain aging is linked to certain types of neurodegenerative diseases and identifying new therapeutic targets has become critical. Melatonin, a pineal hormone, associates with molecules and signaling pathways that sense and influence energy metabolism, autophagy, and circadian rhythms, including insulin-like growth factor 1 (IGF-1), Forkhead box O (FoxOs), sirtuins and mammalian target of rapamycin (mTOR) signaling pathways. This review summarizes the current understanding of how melatonin, together with molecular, cellular and systemic energy metabolisms, regulates epigenetic processes in the neurons. This information will lead to a greater understanding of molecular epigenetic aging of the brain and anti-aging mechanisms to increase lifespan under healthy conditions.
Disturbance and strategies for reactivation of the circadian rhythm system in aging and Alzheimer’s disease
Abstract
Circadian rhythm disturbances, such as sleep disorders, are frequently seen in aging and are even more pronounced in Alzheimer’s disease (AD). Alterations in the biological clock, the suprachiasmatic nucleus (SCN), and the pineal gland during aging and AD are considered to be the biological basis for these circadian rhythm disturbances. Recently, our group found that pineal melatonin secretion and pineal clock gene oscillation were disrupted in AD patients, and surprisingly even in non-demented controls with the earliest signs of AD neuropathology (neuropathological Braak stages I–II), in contrast to non-demented controls without AD neuropathology. Furthermore, a functional disruption of the SCN was observed from the earliest AD stages onwards, as shown by decreased vasopressin mRNA, a clock-controlled major output of the SCN. The observed functional disconnection between the SCN and the pineal from the earliest AD stage onwards seems to account for the pineal clock gene and melatonin changes and underlies circadian rhythm disturbances in AD. This paper further discusses potential therapeutic strategies for reactivation of the circadian timing system, including melatonin and bright light therapy. As the presence of melatonin MT1 receptor in the SCN is extremely decreased in late AD patients, supplementary melatonin in the late AD stages may not lead to clear effects on circadian rhythm disorders.
Light-at-Night-Induced Circadian Disruption, Cancer and Aging
Light-at-night has become an increasing and essential part of the modern lifestyle and leads to a number of health problems, including excessive body mass index, cardiovascular diseases, diabetes, and cancer. The International Agency for Research on Cancer (IARC) Working Group concluded that “shift-work that involves circadian disruption is probably carcinogenic to humans” (Group 2A) [1]. According to the circadian disruption hypothesis, light-at-night might disrupt the endogenous circadian rhythm and specifically suppress nocturnal production of the pineal hormone melatonin and its secretion into the blood. We evaluated the effect of various light/dark regimens on the survival, life span, and spontaneous and chemical carcinogenesis in rodents. Exposure to constant illumination was followed by accelerated aging and enhanced spontaneous tumorigenesis in female CBA and transgenic HER-2/neu mice. In male and female rats maintained at various light/dark regimens (standard 12:12 light/dark [LD], the natural light [NL] of northwestern Russia, constant light [LL], and constant darkness [DD]) from the age of 25 days until natural death, it was found that exposure to NL and LL regimens accelerated age-related switch-off of the estrous function (in females), induced development of metabolic syndrome and spontaneous tumorigenesis, and shortened life span both in male and females rats compared to the standard LD regimen. Melatonin given in nocturnal drinking water prevented the adverse effect of the constant illumination (LL) and natural light (NL) regimens on the homeostasis, life span, and tumor development both in mice and rats. The exposure to the LL regimen accelerated colon carcinogenesis induced by 1,2-dimethylhydrazine (DMH) in rats, whereas the treatment with melatonin alleviated the effects of LL. The maintenance of rats at the DD regimen inhibited DMH-induced carcinogenesis. The LL regimen accelerated, whereas the DD regimen inhibited both mammary carcinogenesis induced by N-nitrosomethylurea and transplacental carcinogenesis induced by N-nitrosoethylurea in rats. Treatment with melatonin prevented premature aging and tumorigenesis in rodents. The data found in the literature and our observations suggest that the use of melatonin would be effective for cancer prevention in humans at risk as a result of light pollution.
Circadian disruption induced by light-at-night accelerates aging and promotes tumorigenesis in rats
Abstract
We evaluated the effect of various light/dark regimens on the survival, life span and tumorigenesis in rats. Two hundred eight male and 203 females LIO rats were subdivided into 4 groups and kept at various light/dark regimens: standard 12:12 light/dark (LD); natural lighting of the North-West of Russia (NL); constant light (LL), and constant darkness (DD) since the age of 25 days until natural death. We found that exposure to NL and LL regimens accelerated development of metabolic syndrome and spontaneous tumorigenesis, shortened life span both in male and females rats as compared to the standard LD regimen. We conclude that circadian disruption induced by light-at-night accelerates aging and promotes tumorigenesis in rats. This observation supports the conclusion of the International Agency Research on Cancer that shift-work that involves circadian disruption is probably carcinogenic to humans.
Shift work and cognitive aging: a longitudinal study
Abstract
Objectives The few studies of shift work and late life cognitive functioning have yielded mixed findings. The aim of the present study is to estimate the association between shift-work experience and change in cognitive performance before and after retirement age among older adults who were gainfully employed. Methods Five hundred and ninety five participants with no dementia were followed up for a mean of 17.6 standard deviation (SD) 8.8 years from a Swedish population-based sample. Participants had self-reported information on any type of shift-work experience (ever/never) in 1984 and measures of cognitive performance (verbal, spatial, memory, processing speed, and general cognitive ability) from up to 9 waves of cognitive assessments during 1986–2012. Night work history (ever/never) from 1998–2002 was available from a subsample (N=320). Early adult cognitive test scores were available for 77 men. Results In latent growth curve modeling, there were no main effects of "any-type" or night shift work on the mean scores or rate of change in any of the cognitive domains. An interaction effect between any-type shift work and education on cognitive performance at retirement was noted. Lower-educated shift workers performed better on cognitive tests than lower-educated day workers at retirement. Sensitivity analyses, however, indicated that the interactions appeared to be driven by selection effects. Lower-educated day workers demonstrated poorer cognitive ability in early adulthood than lower-educated shift workers, who may have selected jobs entailing higher cognitive demand. Conclusion There was no difference in late-life cognitive aging between individuals with a history of working shifts compared to those who had typical day work schedules during midlife.
Aging and Shift Work: A Complex Problem to Face
Abstract
The baby boomer generation is well into the 50+ age bracket, making it one of the largest demographic age cohorts. Whereas this cohort would have previously considered retirement, the evidence suggests that it will remain in the workforce for a longer period in response to a number of social and economic drivers. Mandatory retirement has either been abolished or is under consideration. An increased and healthier life expectancy means that people may work longer for financial and/or psychological reasons. In addition, a global shortage of skilled labor will result in efforts to keep employees in the workplace for longer periods. These trends have a number of implications for working time. What are the health implications of an aging workforce? How do we sustain good work ability into the latter years? What do we know about aging and shift work? What actions are required in the workplace to assist aging workers? This paper is not a comprehensive review of the literature but serves to highlight the complexities in understanding the relationship between shift work and aging. We discuss aging and human function and, in particular, the impact of aging on the circadian system. In addition, we outline new policy directions in this area and raise several suggestions to assist the well‐being of aging workers.
Alzheimer's Disease
Development of a dyadic sleep intervention for Alzheimer's disease patients and their caregivers
Abstract
Purpose: This study aimed to refine a behavioral sleep intervention program targeting patients with Alzheimer's disease and their caregivers. Methods: In this case series, key components of the sleep program were built upon previous intervention studies of patients with cognitive impairment/dementia. The intervention consisted of five weekly sessions covering sleep hygiene, sleep compression, stimulus control, daily walking/light exposure, relaxation/mindfulness, and caregiver training to manage patients' behavioral problems. The materials and structure were iteratively refined based on feedback from caregivers and sleep educators. Sleep diaries were used to evaluate sleep outcomes. Results: Five out of six enrolled dyads completed the sessions. Several revisions were made during testing: the last session was changed from telephone to in-person; some components (e.g., sleep scheduling, mindfulness) were rearranged within or across sessions; sleep educator guidelines for sleep scheduling, light exposure, and walking were revised. After the fifth dyad, no additional issues were identified by the caregiver or the sleep educator. Four patients and three caregivers had improved sleep at the last session. Conclusions: The iterative refinement process was successful in finalizing the intervention program, with evidence of sleep improvements. Formal pilot testing of the program will provide further information on feasibility and effectiveness. IMPLICATIONS FOR REHABILITATION Our dyadic behavioral sleep program can be tailored to various types of sleep problems among patients with Alzheimer's disease and their family caregivers, with the goal of improving daytime function by reducing sleep disturbances at night. Caregiver training and participation of both members of the dyad in sleep management may benefit the patients' sleep and other health outcomes, reduce caregiver stress and burden, and ultimately delay or prevent institutionalization of Alzheimer's disease patients.
Sleep, major depressive disorder, and Alzheimer disease: A Mendelian randomization study
Abstract
Objective: To explore the causal relationships between sleep, major depressive disorder (MDD), and Alzheimer disease (AD).
Methods: We conducted bidirectional 2-sample Mendelian randomization analyses. Genetic associations were obtained from the largest genome-wide association studies currently available in UK Biobank (n = 446,118), Psychiatric Genomics Consortium (n = 18,759), and International Genomics of Alzheimer's Project (n = 63,926). We used the inverse variance-weighted Mendelian randomization method to estimate causal effects and weighted median and Mendelian randomization-Egger for sensitivity analyses to test for pleiotropic effects.
Results: We found that higher risk of AD was significantly associated with being a "morning person" (odds ratio [OR] 1.01, p = 0.001), shorter sleep duration (self-reported: β = -0.006, p = 1.9 × 10-4; accelerometer based: β = -0.015, p = 6.9 × 10-5), less likely to report long sleep (β = -0.003, p = 7.3 × 10-7), earlier timing of the least active 5 hours (β = -0.024, p = 1.7 × 10-13), and a smaller number of sleep episodes (β = -0.025, p = 5.7 × 10-14) after adjustment for multiple comparisons. We also found that higher risk of AD was associated with lower risk of insomnia (OR 0.99, p = 7 × 10-13). However, we did not find evidence that these abnormal sleep patterns were causally related to AD or for a significant causal relationship between MDD and risk of AD.
Conclusion: We found that AD may causally influence sleep patterns. However, we did not find evidence supporting a causal role of disturbed sleep patterns for AD or evidence for a causal relationship between MDD and AD.
Sleep and Dementia
Abstract
Neurocognitive and sleep problems are common, underdiagnosed, and frequently co-morbid. Sleep disruption, and fatigue, predict cognitive impairment. Cognitive impairment, in turn, can worsen sleep hygiene. In dementia patients, sleep disorders are common, and dementia medications affect sleep. Emerging insights on the brain's glymphatic system suggests that sleep may drive clearance of Aβ peptide to affect Alzheimer pathophysiology. Parkinsonian dementias are linked with REM behavior disorder, a highly treatable problem that predicts future conversion into dementia.
Sleep, Cognitive impairment, and Alzheimer's disease: A Systematic Review and Meta-Analysis
Abstract
Study objectives: Mounting evidence implicates disturbed sleep or lack of sleep as one of the risk factors for Alzheimer's disease (AD), but the extent of the risk is uncertain. We conducted a broad systematic review and meta-analysis to quantify the effect of sleep problems/disorders on cognitive impairment and AD.
Methods: Original published literature assessing any association of sleep problems or disorders with cognitive impairment or AD was identified by searching PubMed, Embase, Web of Science, and the Cochrane library. Effect estimates of individual studies were pooled and relative risks (RR) and 95% confidence intervals (CI) were calculated using random effects models. We also estimated the population attributable risk.
Results: Twenty-seven observational studies (n = 69216 participants) that provided 52 RR estimates were included in the meta-analysis. Individuals with sleep problems had a 1.55 (95% CI: 1.25-1.93), 1.65 (95% CI: 1.45-1.86), and 3.78 (95% CI: 2.27-6.30) times higher risk of AD, cognitive impairment, and preclinical AD than individuals without sleep problems, respectively. The overall meta-analysis revealed that individuals with sleep problems had a 1.68 (95% CI: 1.51-1.87) times higher risk for the combined outcome of cognitive impairment and/or AD. Approximately 15% of AD in the population may be attributed to sleep problems.
Conclusion: This meta-analysis confirmed the association between sleep and cognitive impairment or AD and, for the first time, consolidated the evidence to provide an "average" magnitude of effect. As sleep problems are of a growing concern in the population, these findings are of interest for potential prevention of AD.
Keywords: Alzheimer’s disease; cognitive decline; dementia.; sleep disorders; sleep parameters; sleep problems.
Alzheimer's disease: Neurotransmitters of the sleep-wake cycle
The Relationship between Obstructive Sleep Apnea and Alzheimer's Disease
Abstract
Obstructive sleep apnea (OSA) and Alzheimer's disease (AD) are highly prevalent conditions with growing impact on our aging society. While the causes of OSA are now better characterized, the mechanisms underlying AD are still largely unknown, challenging the development of effective treatments. Cognitive impairment, especially affecting attention and executive functions, is a recognized clinical consequence of OSA. A deeper contribution of OSA to AD pathogenesis is now gaining support from several lines of research. OSA is intrinsically associated with disruptions of sleep architecture, intermittent hypoxia and oxidative stress, intrathoracic and hemodynamic changes as well as cardiovascular comorbidities. All of these could increase the risk for AD, rendering OSA as a potential modifiable target for AD prevention. Evidence supporting the relevance of each of these mechanisms for AD risk, as well as a possible effect of AD in OSA expression, will be explored in this review.
Alzheimer's Disease and Sleep-Wake Disturbances: Amyloid, Astrocytes, and Animal Models
Abstract
Sleep-wake abnormalities are common in patients with Alzheimer's disease, and can be a major reason for institutionalization. However, an emerging concept is that these sleep-wake disturbances are part of the causal pathway accelerating the neurodegenerative process. Recently, new findings have provided intriguing evidence for a positive feedback loop between sleep-wake dysfunction and β-amyloid (Aβ) aggregation. Studies in both humans and animal models have shown that extended periods of wakefulness increase Aβ levels and aggregation, and accumulation of Aβ causes fragmentation of sleep. This perspective is aimed at presenting evidence supporting causal links between sleep-wake dysfunction and aggregation of Aβ peptide in Alzheimer's disease, and explores the role of astrocytes, a specialized type of glial cell, in this context underlying Alzheimer's disease pathology. The utility of current animal models and the unexplored potential of alternative animal models for testing mechanisms involved in the reciprocal relationship between sleep disruption and Aβ are also discussed.
Sleep and Attention in Alzheimer's Disease
Abstract
Individuals with Alzheimer's disease (AD) present with a wide variety of symptoms, including sleep disruption and sleep disorders. Conversely, disordered sleep has been associated with an increased risk of developing AD. Both conditions individually have adverse effects on attention, which can be further divided into selective, sustained, divided, and alternating attention. The neural mechanisms underpinning sleep problems in AD involve the disruption of the circadian system. This review comprehensively discusses the types of attention impairments, the relationship between AD pathology and sleep disruption, and the effect of sleep issues on attention in AD. Recommendations for future research include addressing the lack of consistency among study designs and outcomes, and the need to continue exploring the biology of sleep and attention in AD.
Bidirectional relationship between sleep and Alzheimer's disease: role of amyloid, tau, and other factors
Abstract
As we age, we experience changes in our nighttime sleep and daytime wakefulness. Individuals afflicted with Alzheimer's disease (AD) can develop sleep problems even before memory and other cognitive deficits are reported. As the disease progresses and cognitive changes ensue, sleep disturbances become even more debilitating. Thus, it is imperative to gain a better understanding of the relationship between sleep and AD pathogenesis. We postulate a bidirectional relationship between sleep and the neuropathological hallmarks of AD; in particular, the accumulation of amyloid-β (Aβ) and tau. Our research group has shown that extracellular levels of both Aβ and tau fluctuate during the normal sleep-wake cycle. Disturbed sleep and increased wakefulness acutely lead to increased Aβ production and decreased Aβ clearance, whereas Aβ aggregation and deposition is enhanced by chronic increased wakefulness in animal models. Once Aβ accumulates, there is evidence in both mice and humans that this results in disturbed sleep. New findings from our group reveal that acute sleep deprivation increases levels of tau in mouse brain interstitial fluid (ISF) and human cerebrospinal fluid (CSF) and chronic sleep deprivation accelerates the spread of tau protein aggregates in neural networks. Finally, recent evidence also suggests that accumulation of tau aggregates in the brain correlates with decreased nonrapid eye movement (NREM) sleep slow wave activity. In this review, we first provide a brief overview of the AD and sleep literature and then highlight recent advances in the understanding of the relationship between sleep and AD pathogenesis. Importantly, the effects of the bidirectional relationship between the sleep-wake cycle and tau have not been previously discussed in other reviews on this topic. Lastly, we provide possible directions for future studies on the role of sleep in AD.
Circadian and sleep dysfunction in Alzheimer's disease
Abstract
Alzheimer's disease (AD) is a devastating and irreversible cognitive impairment and the most common type of dementia. Along with progressive cognitive impairment, dysfunction of the circadian rhythms also plays a pivotal role in the progression of AD. A mutual relationship among circadian rhythms, sleep, and AD has been well-recommended. The etiopathogenesis of the disturbances of the circadian system and AD share some general features that also unlock the outlook of observing them as a mutually dependent pathway. Indeed, the burden of amyloid β (Aβ), neurofibrillary tangles (NFTs), neuroinflammation, oxidative stress, and dysfunction of circadian rhythms may lead to AD. Aging can alter both sleep timings and quality that can be strongly disrupted in AD. Increased production of Aβ and reduced Aβ clearance are caused by a close interplay of Aβ, sleep disturbance and raised wakefulness. Besides Aβ, the impact of tau pathology is possibly noteworthy to the sleep deprivation found in AD. Hence, this review is focused on the primary mechanistic complexities linked to disruption of circadian rhythms, sleep deprivation, and AD. Furthermore, this review also highlights the potential therapeutic strategies to abate AD pathogenesis.
Implications of sleep disturbance and inflammation for Alzheimer's disease dementia
Abstract
Nearly half of all adults older than 60 years of age report sleep disturbance, as characterised either by reports of insomnia complaints with daytime consequences, dissatisfaction with sleep quality or quantity, or the diagnosis of insomnia disorder. Accumulating evidence shows that sleep disturbance contributes to cognitive decline and might also increase the risk of Alzheimer's disease dementia by increasing β-amyloid burden. That sleep disturbance would be a candidate risk factor for Alzheimer's disease might seem surprising, given that disturbed sleep is usually considered a consequence of Alzheimer's disease. However, a bidirectional relationship between sleep and Alzheimer's disease is supported by advances in our understanding of sleep disturbance-induced increases in systemic inflammation, which can be viewed as an early event in the course of Alzheimer's disease. Inflammation increases β-amyloid burden and is thought to drive Alzheimer's disease pathogenesis. Improved understanding of the mechanisms linking sleep disturbance and Alzheimer's disease risk could facilitate the identification of targets for prevention, given that both sleep disturbance and inflammatory activation might be modifiable risk factors for Alzheimer's disease.
Alzheimer's disease and sleep disturbances: a review
Abstract
The association between Alzheimer's disease (AD) and sleep disturbances has received increasing scientific attention in the last decades. However, little is known about the impact of sleep and its disturbances on the development of preclinical AD stages, such as mild cognitive impairment. This review describes the evolution of knowledge about the potential bidirectional relationships between AD and sleep disturbances exploring recent large prospective studies and meta-analyses and studies of the possible mechanisms through which sleep and the neurodegenerative process could be associated. The review also makes a comprehensive exploration of the sleep characteristics of older people, ranging from cognitively normal individuals, through patients with mild cognitive impairment, up to the those with dementia with AD.
β-Amyloid accumulation in the human brain after one night of sleep deprivation
Abstract
The effects of acute sleep deprivation on β-amyloid (Aβ) clearance in the human brain have not been documented. Here we used PET and 18F-florbetaben to measure brain Aβ burden (ABB) in 20 healthy controls tested after a night of rested sleep (baseline) and after a night of sleep deprivation. We show that one night of sleep deprivation, relative to baseline, resulted in a significant increase in Aβ burden in the right hippocampus and thalamus. These increases were associated with mood worsening following sleep deprivation, but were not related to the genetic risk (APOE genotype) for Alzheimer's disease. Additionally, baseline ABB in a range of subcortical regions and the precuneus was inversely associated with reported night sleep hours. APOE genotyping was also linked to subcortical ABB, suggesting that different Alzheimer's disease risk factors might independently affect ABB in nearby brain regions. In summary, our findings show adverse effects of one-night sleep deprivation on brain ABB and expand on prior findings of higher Aβ accumulation with chronic less sleep.
Alzheimer’s disease: Neurotransmitters of the sleep-wake cycle
Abstract
With aging, our sleeping pattern alters. Elderly often wake unrested because their sleep time and sleep efficacy is reduced. In Alzheimer's disease (AD) patients, these alterations are even more pronounced and may further aggravate cognitive decline. Therefore, sleep disturbances greatly impact self-care ability, caregiver exhaustion and institutionalization rate. Reestablishing an effective sleep-wake cycle in these patients still remains an unresolved challenge, partly because sleep physiology is quite complex and multiple neurotransmitter systems contribute to a single process. Gaining a better understanding of sleep physiology will be crucial for further research. Conjointly, animal models, along with a multidisciplinary approach, will be of great value to establish a common ground between AD and sleep disturbances and work towards a potential therapeutic application.
Chronic sleep fragmentation exacerbates amyloid β deposition in Alzheimer’s disease model mice
Abstract
Sleep fragmentation due to intermittent nocturnal arousal resulting in a reduction of total sleep time and sleep efficiency is a common symptom among people with Alzheimer’s disease (AD) and elderly people with normal cognitive function. Although epidemiological studies have indicated an association between sleep fragmentation and elevated risk of AD, a relevant disease model to elucidate the underlying mechanisms was lacking owing to technical limitations. Here we successfully induced chronic sleep fragmentation in AD model mice using a recently developed running-wheel-based device and demonstrate that chronic sleep fragmentation increases amyloid β deposition. Notably, the severity of amyloid β deposition exhibited a significant positive correlation with the extent of sleep fragmentation. These findings provide a useful contribution to the development of novel treatments that decelerate the disease course of AD in the patients, or decrease the risk of developing AD in healthy elderly people through the improvement of sleep quality.
Sleep disturbance: an emerging opportunity for Alzheimer's disease prevention?
Abstract
As the older segment of our population grows, cognitive decline and dementia will increase in prevalence, with Alzheimer's disease (AD) as the cause in most cases. Until a cure exists, prevention through the identification and manipulation of modifiable risk factors for dementia, in general, or AD, in particular, will be our only means of reducing dementia prevalence or delaying its onset. Furthermore, it is likely that eventual treatments for AD, when available, will depend on the ability to identify individuals at greatest risk for developing AD. Sleep disturbances are common in later life - roughly half of older adults experience regular insomnia (Ohayon, 2002) and about as many have some degree of sleep-disordered breathing (SDB) (Ancoli-Israel et al., 1991) - and accumulating evidence suggests they may contribute to cognitive decline, at least in part, by promoting the development of AD pathology (Spira et al., 2014). Because they are treatable, sleep disturbances are an important potential target for ongoing study in AD prevention. Moreover, understanding the mechanisms underlying an effect of sleep on subsequent cognitive decline and AD would allow for better identification of opportunities and optimal timing for treatment of sleep disorders, and ultimately perhaps, AD prevention.
Bidirectional relationship between sleep and Alzheimer’s disease: role of amyloid, tau, and other factors
Abstract
As we age, we experience changes in our nighttime sleep and daytime wakefulness. Individuals afflicted with Alzheimer’s disease (AD) can develop sleep problems even before memory and other cognitive deficits are reported. As the disease progresses and cognitive changes ensue, sleep disturbances become even more debilitating. Thus, it is imperative to gain a better understanding of the relationship between sleep and AD pathogenesis. We postulate a bidirectional relationship between sleep and the neuropathological hallmarks of AD; in particular, the accumulation of amyloid-β (Aβ) and tau. Our research group has shown that extracellular levels of both Aβ and tau fluctuate during the normal sleep−wake cycle. Disturbed sleep and increased wakefulness acutely lead to increased Aβ production and decreased Aβ clearance, whereas Aβ aggregation and deposition is enhanced by chronic increased wakefulness in animal models. Once Aβ accumulates, there is evidence in both mice and humans that this results in disturbed sleep. New findings from our group reveal that acute sleep deprivation increases levels of tau in mouse brain interstitial fluid (ISF) and human cerebrospinal fluid (CSF) and chronic sleep deprivation accelerates the spread of tau protein aggregates in neural networks. Finally, recent evidence also suggests that accumulation of tau aggregates in the brain correlates with decreased nonrapid eye movement (NREM) sleep slow wave activity. In this review, we first provide a brief overview of the AD and sleep literature and then highlight recent advances in the understanding of the relationship between sleep and AD pathogenesis. Importantly, the effects of the bidirectional relationship between the sleep−wake cycle and tau have not been previously discussed in other reviews on this topic. Lastly, we provide possible directions for future studies on the role of sleep in AD.
Sleep deprivation accelerates the progression of alzheimer’s disease by influencing Aβ-related metabolism
Abstract
Sleep disorders have previously been connected with the neurodegenerative pathology of Alzheimer’s disease (AD) due to the aggregation of β-amyloid(Aβ)peptides and tau proteinsinduced by sleep deprivation (SD). However, the underlying mechanisms remain unclear. Therefore, this study was performed to clarify how Aβ-related metabolism is regulated after SD. Three-month-old Sprague-Dawley rats (250–300 g) were randomly divided into 5 groups: two SD groups(i.e.,SD-2d and SD-4d), two platform control groups(i.e.,PC-2d and PC-4d) and a home cage control group (CC). For the two SD groups, themodified multiple platform method (MMPM) was used to induce SD.Our experiments confirmed that SD impaired cognitive function and increased the levels of Aβ peptides, a hallmark of AD. Additionally, we found that SD significantly increasedthe levels of the β-site amyloid precursor protein (APP)-cleaving enzyme 1(BACE1, β-secretase), but had little impacton the levels of Aβ-degradationenzymes.This resultmay be the main cause of the over-expression of Aβ1-42 and Aβ1-40. Our results suggested that SD accelerates the progression of AD bymodulating Aβ-related metabolism. This findinghasimportant implications for the diagnosis and prevention of AD.
The role of sleep deprivation and circadian rhythm disruption as risk factors of Alzheimer’s disease
Abstract
Emerging evidence suggests that sleep deprivation (SD) and circadian rhythm disruption (CRD) may interact and increase the risk for the development of Alzheimer's disease (AD). This review inspects different pathophysiological aspects of SD and CRD, and shows that the two may impair the glymphatic-vascular-lymphatic clearance of brain macromolecules (e.g., β-amyloid and microtubule associated protein tau), increase local brain oxidative stress and diminish circulatory melatonin levels. Lastly, this review looks into the potential association between sleep and circadian rhythm with stress granule formation, which might be a new mechanism along the AD pathogenic pathway. In summary, SD and CRD is likely to be associated with a positive risk in developing Alzheimer's disease in humans.
Sleep deprivation and cerebrospinal fluid biomarkers for Alzheimer’s disease
Abstract
Study objectives: To investigate the cumulative effect of five consecutive nights of partial sleep deprivation (PSD) on a panel of cerebrospinal fluid (CSF) biomarkers in healthy adults.
Methods: A randomized, cross-over study conducted at the University of Gothenburg. The participants (N = 13) were healthy adults (20-40 years of age) with a normal sleeping pattern. The participants underwent a baseline sleep period consisting of five nights with 8 hr spent in bed. A subsequent period with PSD consisted of five nights of maximum 4 hr of sleep per night. Four participants were also subjected to a prolonged period of PSD consisting of eight nights with 4 hr of sleep per night. Sleep was monitored by means of observation, actigraphy, and continuous polysomnographic recordings. CSF samples were collected by routine lumbar puncture after each period. CSF biomarkers included the 38, 40, and 42 amino acid-long Aβ isoforms, total-τ, phospho-τ, orexin, monoamine metabolites (3-methoxy-4-hydroxyphenylglycol, homovanillinic acid, and 5-hydroxyindoleacetic acid), neuron-derived biomarkers (neurofilament light, neuron-specific enolase, and fatty acid-binding protein), and astro- and microglia-derived biomarkers (glial fibrillary acidic protein, S-100B, and YKL-40).
Results: PSD was associated with a 27 per cent increase in CSF orexin concentrations (p = 0.001). No PSD-related changes in CSF biomarkers for amyloid build-up in the brain, Alzheimer's disease (AD)-type neurodegeneration, or astroglial activation were observed. PSD led to a shortening of time spent in all sleep stages except slow-wave sleep (SWS).
Conclusion: Five to eight consecutive nights of PSD, with preserved SWS, increased CSF orexin but had no effect on CSF biomarkers for amyloid deposition, neuronal injury, and astroglial activation.
What is the impact of shift work on the psychological functioning and resilience of nurses? An integrative review
AbstractAim
To synthesize existing research to determine if nurses who work shifts have poorer psychological functioning and resilience than nurses who do not work shifts.
Background
Research exploring the impact of shift work on the psychological functioning and resilience of nurses is limited compared with research investigating the impact of shifts on physical outcomes.
Design
Integrative literature review.
Data Sources
Relevant databases were searched from January 1995–August 2016 using the combination of keywords: nurse, shift work; rotating roster; night shift; resilient; hardiness; coping; well‐being; burnout; mental health; occupational stress; compassion fatigue; compassion satisfaction; stress; anxiety; depression.
Review Methods
Two authors independently performed the integrative review processes proposed by Whittemore and Knafl and a quality assessment using the mixed‐methods appraisal tool by Pluye et al.
Results
A total of 37 articles were included in the review (32 quantitative, 4 qualitative and 1 mixed‐methods). Approximately half of the studies directly compared nurse shift workers with non‐shift workers. Findings were grouped according to the following main outcomes: (1) general psychological well‐being/quality of life; (2) Job satisfaction/burnout; (3) Depression, anxiety and stress; and (4) Resilience/coping. We did not find definitive evidence that shift work is associated with poorer psychological functioning in nurses. Overall, the findings suggest that the impact of shift work on nurse psychological functioning is dependent on several contextual and individual factors.
Conclusion
More studies are required which directly compare the psychological outcomes and resilience of nurse shift workers with non‐shift workers.
Poor sleep quality impairs cognitive performance in older adults
Abstract
The prevalence of insomnia increases with age. Short sleep duration is associated with deficits in cognitive performance. We hypothesized that short sleep duration and sleep quality influence cognitive performance in older adults. The study included 78 adults aged 60 years and over (72.2 ± 5.9 years). Total sleep time and sleep efficiency (total sleep time/time in bed × 100) were calculated using actigraphy. We evaluated cognitive performance with the continuous performance test-identical pairs and the number-back test. Sleep apnea was evaluated overnight with a portable home monitoring system. The accuracy of the 0-back test significantly decreased in participants with total sleep time less than 5 h compared with those with total sleep time greater than 7 h, but there was no significant difference in continuous performance test-identical pairs between the two groups. Participants with sleep efficiency <85% showed a significant decrease in 0- and 1-back test accuracy compared with those with sleep efficiency ≥85%. There were no significant differences in the accuracy of number-back tests and continuous performance test-identical pairs between apnea-hypopnea index ≥15 h(-1) and apnea-hypopnea index <15 h(-1) groups, or among lowest SpO2 ≥ 90%, lowest 80-90%, and lowest SpO2 < 80% groups. Age, total sleep time and sleep efficiency were significantly correlated with accuracy on the 0-back test. Age and sleep efficiency were significantly correlated with accuracy on the 1-back test. Multiple regression analysis revealed that total sleep time was independently correlated with accuracy on the 0-back test, while age was independently correlated with accuracy on the 1-back test. Our findings suggest that sleep duration and sleep quality may play a role in cognitive performance in older adults.
Circadian rhythms in cognitive performance: implications for neuropsychological assessment
Abstract: Circadian variations have been found in human performance, including the efficiency to execute many tasks, such as sensory, motor, reaction time, time estimation, memory, verbal, arithmetic calculations, and simulated driving tasks. Performance increases during the day and decreases during the night. Circadian rhythms have been found in three basic neuropsychological processes (attention, working memory, and executive functions), which may explain oscillations in the performance of many tasks. The time course of circadian rhythms in cognitive performance may be modified significantly in patients with brain disorders, due to chronotype, age, alterations of the circadian rhythm, sleep deprivation, type of disorder, and medication. This review analyzes the recent results on circadian rhythms in cognitive performance, as well as the implications of these rhythms for the neuropsychological assessment of patients with brain disorders such as traumatic head injury, stroke, dementia, developmental disorders, and psychiatric disorders.
Role of sleep continuity and total sleep time in executive function across the adult lifespan.
Abstract
The importance of sleep for cognition in young adults is well established, but the role of habitual sleep behavior in cognition across the adult lifespan remains unknown. We examined the relationship between sleep continuity and total sleep time assessed with a sleep detection device and cognitive performance using a battery of tasks in young (n = 59, mean age = 23.05) and older (n = 53, mean age = 62.68) adults. Across age groups, higher sleep continuity was associated with better cognitive performance. In the younger group, higher sleep continuity was associated with better working memory and inhibitory control. In the older group, higher sleep continuity was associated with better inhibitory control, memory recall, and verbal fluency. Very short and very long total sleep time was associated with poorer working memory and verbal fluency, specifically in the younger group. Total sleep time was not associated with cognitive performance in any domains for the older group. These findings reveal that sleep continuity is important for executive function in both young and older adults, but total sleep time may be more important for cognition in young adults.
Behavioral Sleep Problems and their Potential Impact on Developing Executive Function in Children
Abstract
Bedtime resistance and night waking are common sleep problems throughout childhood, especially in the early years. These sleep problems may lead to difficulties in neurobehavioral functioning, but most research into childhood sleep problems has not emphasized the importance of the developmental context in which disruptions in neurobehavioral and daytime functioning occur. We review the development of sleep as well as executive functioning (EF) in childhood and suggest that EF may be particularly vulnerable to the effects of these common childhood sleep problems because of its prolonged course of maturation. Behavioral problems associated with common sleep problems suggest poor self-regulation in the context of sleep loss, and developing EF skills play important roles in self-regulation. A research agenda that considers a developmental approach to sleep and sleep problems in the context of childhood EF performance is outlined to promote future research in this area.
Sleep Well, Think Well: Sleep-Wake Disturbance in Mild Cognitive Impairment
Abstract
While literature suggests that sleep is important for cognition and mood, and that sleep disturbance is a prominent feature of neurodegenerative and neuropsychiatric disorders, these relationships have not yet been examined in older people ''at risk" of dementia. In this study, 15 older people with the nonamnestic subtype of mild cognitive impairment ([MCI] mean age = 66.7 years, SD = 8.7) underwent psychiatric and neuropsychological assessment. Participants completed sleep diaries, questionnaires, and 2 weeks of actigraphy. Key outcome data during the rest interval were time spent ''awake" or wake after sleep onset (WASO) and the number of arousals/wake bouts. Results showed that even after controlling for age, greater WASO was associated with reduced attention and executive functioning and increased arousals were related to poorer nonverbal learning and problem solving. This preliminary data suggests that sleep-wake disturbance in nonamnestic forms of MCI is related to cognitive functioning and may be indicative of shared neurobiological underpinnings.
Cognitive deficits in chronic fatigue syndrome and their relationship to psychological status, symptomatology, and everyday functioning.
Abstract
Objective: To examine cognitive deficits in people with chronic fatigue syndrome (CFS) and their relationship to psychological status, CFS symptoms, and everyday functioning.
Method: The current study compared the cognitive performance (reaction time, attention, memory, motor functioning, verbal abilities, and visuospatial abilities) of a sample with CFS (n = 50) with that of a sample of healthy controls (n = 50), all of whom had demonstrated high levels of effort and an intention to perform well, and examined the extent to which psychological status, CFS symptoms, and everyday functioning were related to cognitive performance.
Results: The CFS group showed impaired information processing speed (reaction time), relative to the controls, but comparable performance on tests of attention, memory, motor functioning, verbal ability, and visuospatial ability. Moreover, information processing speed was not related to psychiatric status, depression, anxiety, the number or severity of CFS symptoms, fatigue, sleep quality, or everyday functioning.
Conclusion: A slowing in information processing speed appears to be the main cognitive deficit seen in persons with CFS whose performance on effort tests is not compromised. Importantly, this slowing does not appear to be the consequence of other CFS-related variables, such as depression and fatigue, or motor speed.
Poor sleep is associated with CSF biomarkers of amyloid pathology in cognitively normal adults
Abstract
Objective: To determine the relationship between sleep quality and CSF markers of Alzheimer disease (AD) pathology in late midlife.
Methods: We investigated the relationship between sleep quality and CSF AD biomarkers in a cohort enriched for parental history of sporadic AD, the Wisconsin Registry for Alzheimer's Prevention. A total of 101 participants (mean age 62.9 ± 6.2 years, 65.3% female) completed sleep assessments and CSF collection and were cognitively normal. Sleep quality was measured with the Medical Outcomes Study Sleep Scale. CSF was assayed for biomarkers of amyloid metabolism and plaques (β-amyloid 42 [Aβ42]), tau pathology (phosphorylated tau [p-tau] 181), neuronal/axonal degeneration (total tau [t-tau], neurofilament light [NFL]), neuroinflammation/astroglial activation (monocyte chemoattractant protein-1 [MCP-1], chitinase-3-like protein 1 [YKL-40]), and synaptic dysfunction/degeneration (neurogranin). To adjust for individual differences in total amyloid production, Aβ42 was expressed relative to Aβ40. To assess cumulative pathology, CSF biomarkers were expressed in ratio to Aβ42. Relationships among sleep scores and CSF biomarkers were assessed with multiple regression, controlling for age, sex, time between sleep and CSF measurements, and CSF assay batch.
Results: Worse subjective sleep quality, more sleep problems, and daytime somnolence were associated with greater AD pathology, indicated by lower CSF Aβ42/Aβ40 and higher t-tau/Aβ42, p-tau/Aβ42, MCP-1/Aβ42, and YKL-40/Aβ42. There were no significant associations between sleep and NFL or neurogranin.
Conclusions: Self-report of poor sleep was associated with greater AD-related pathology in cognitively healthy adults at risk for AD. Effective strategies exist for improving sleep; therefore sleep health may be a tractable target for early intervention to attenuate AD pathogenesis.
Sleep, cognition, and behavioral problems in school-age children: A century of research meta-analyzed.
Abstract
Clear associations of sleep, cognitive performance, and behavioral problems have been demonstrated in meta-analyses of studies in adults. This meta-analysis is the first to systematically summarize all relevant studies reporting on sleep, cognition, and behavioral problems in healthy school-age children (5-12 years old) and incorporates 86 studies on 35,936 children. Sleep duration shows a significant positive relation with cognitive performance (r = .08, confidence interval [CI] [.06, .10]). Subsequent analyses on cognitive subdomains indicate specific associations of sleep duration with executive functioning (r = .07, CI [.02, .13]), with performance on tasks that address multiple cognitive domains (r = .10, CI = [.05, .16]), and with school performance (r = .09, CI [.06, .12]), but not with intelligence. Quite unlike typical findings in adults, sleep duration was not associated with sustained attention and memory. Methodological issues and brain developmental immaturities are proposed to underlie the marked differences. Shorter sleep duration is associated with more behavioral problems (r = .09, CI [.07, .11]). Subsequent analyses on subdomains of behavioral problems showed that the relation holds for both internalizing (r = .09, CI [.06, .12]) and externalizing behavioral problems (r = .08, CI [.06, .11]). Ancillary moderator analyses identified practices recommended to increase sensitivity of assessments and designs in future studies. In practical terms, the findings suggest that insufficient sleep in children is associated with deficits in higher-order and complex cognitive functions and an increase in behavioral problems. This is particularly relevant given society's tendency towards sleep curtailment.
Greater Cognitive Deficits with Sleep-disordered Breathing among Individuals with Genetic Susceptibility to Alzheimer Disease. The Multi-Ethnic Study of Atherosclerosis
Abstract
Rationale: There are conflicting findings regarding the link between sleep apnea and cognitive dysfunction.
Objectives: Investigate associations between indicators of sleep-disordered breathing (SDB) and cognitive function in the Multi-Ethnic Study of Atherosclerosis and assess effect modification by the apolipoprotein ε-4 (APOE-ε4) allele.
Methods: A diverse population (N = 1,752) underwent type 2 in-home polysomnography, which included measurement of percentage sleep time less than 90% oxyhemoglobin saturation (%Sat < 90%) and apnea-hypopnea index (AHI). Epworth Sleepiness Scale score (ESS) and sleep apnea syndrome (SAS; AHI ≥ 5 and ESS > 10) were also analyzed. Cognitive outcomes included the Cognitive Abilities Screening Instrument; Digit Symbol Coding (DSC) test; and Digit Span Tests (DST) Forward and Backward.
Results: Participants were 45.4% men, aged 68.1 years (SD, 9.1 yr) with a median AHI of 9.0 and mean ESS of 6.0. Approximately 9.7% had SAS, and 26.8% had at least one copy of the APOE-ε4 allele. In adjusted analyses, a 1-SD increase in %Sat < 90% and ESS score were associated with a poorer attention and memory assessed by the DST Forward score (β = -0.12 [SE, 0.06] and β = -0.13 [SE, 0.06], respectively; P ≤ 0.05). SAS and higher ESS scores were also associated with poorer attention and processing speed as measured by the DSC (β = -0.69 [SE, 0.35] and β = -1.42 [SE, 0.35], respectively; P < 0.05). The presence of APOE-ε4 allele modified the associations of %Sat < 90% with DST forward and of ESS with DSC (Pinteraction ≤ 0.05).
Conclusions: Overnight hypoxemia and sleepiness were associated with cognition. The average effect estimates were small, similar to effect estimates for several other individual dementia risk factors. Associations were strongest in APOE-ε4 risk allele carriers. Our results (1) suggest that SDB be considered among a group of modifiable dementia risk factors, and (2) highlight the potential vulnerability of APOE-ε4 risk allele carriers with SDB.
Pain Mitigation
Sleep Disturbances in Chronic Pain: Neurobiology, Assessment, and Treatment in Physical Therapist Practice
Abstract
Among people with chronic pain, insomnia is highly prevalent, closely related to the mechanism of central sensitization, characterized by low-grade neuroinflammation, and commonly associated with stress or anxiety; in addition, it often does not respond effectively to drug treatments. This review article applies the current understanding of insomnia to clinical practice, including assessment and conservative treatment of insomnia in people with chronic pain. Cognitive-behavioral therapy for insomnia can be efficacious for improvements in sleep initiation, sleep maintenance, perceived sleep quality, and pain interference with daily functioning in people with chronic pain. A recent systematic review concluded that with additional training, physical therapist-led cognitive-behavioral interventions are efficacious for low back pain, allowing their implementation within the field. Cognitive-behavioral therapy for insomnia, as provided to people with chronic pain, typically includes education, sleep restriction measures, stimulus control instructions, sleep hygiene, and cognitive therapy.
Total sleep deprivation increases pain sensitivity, impairs conditioned pain modulation and facilitates temporal summation of pain in healthy participants
Abstract
Chronic pain patients often suffer from insomnia or impaired sleep which has been associated with increased pain sensitivity, but a limited amount of studies have investigated the effects of total sleep deprivation on central pain mechanisms. Therefore, the aim of this study was to determine the effects of total sleep deprivation on temporal summation, conditioned pain modulation, thermal and pressure pain sensitivity in healthy participants. Twenty-four healthy participants took part in this two-session trial. The measurements were conducted after a night of habitual sleep (baseline) and following 24 hours of total sleep deprivation. Detection thresholds for cold and warmth and pain thresholds for cold and heat were assessed. Cuff induced pressure pain detection and tolerance thresholds, temporal summation and conditioned pain modulation were assessed with user-independent, computer-controlled cuff algometry. Conditioned pain modulation was significantly impaired, temporal summation was significantly facilitated and pain sensitivity to pressure and cold pain were significantly increased at follow-up compared with baseline. In conclusion, this study found that one night of total sleep deprivation impaired descending pain pathways, facilitated spinal excitability and sensitized peripheral pathways to cold and pressure pain. Future studies are encouraged to investigate if sleep therapy might normalize pain sensitivity in sleep-deprived chronic pain patients.
Influence of Itch and Pain on Sleep Quality in Atopic Dermatitis and Psoriasis
Abstract
Subjective symptoms accompanying atopic dermatitis and psoriasis can negatively influence patients' well-being. This study assessed the impact of itch and pain on sleep quality among 100 patients with atopic dermatitis and 100 patients with psoriasis, compared with 50 controls. The Athens Insomnia Scale (AIS) and Pittsburgh Sleep Quality Index (PSQI) were used to evaluate a spectrum of sleep disturbances. Co-existence of insomnia was indicated in the majority of patients; atopic dermatitis; 82%, psoriasis; 62%. PSQI total scores for patients with atopic dermatitis (8.3 ± 4.2 points) and those with psoriasis (8.1 ± 4.8 points) qualified them, in 80% of cases, as poor sleepers and were significantly higher compared with controls (3.1 ± 1.9 points). However, subjects with atopic dermatitis experienced more problems with insomnia and sleep quality than did those with psoriasis. Atopic dermatitis and psoriasis-related itch, but not pain, has a substantial association with insomnia and sleep quality in these patients, and is a crucial subjective symptom in these chronic, inflammatory skin diseases.
Neurobiological mechanisms underlying the sleep-pain relationship in adolescence: A review
Abstract
Adolescence characterizes a period of significant change in brain structure and function, causing the neural circuitry to be particularly susceptible to the environment and various other experiences. Chronic pain and sleep deprivation represent major health issues that plague adolescence. A bidirectional relationship exists between sleep and pain; however, emerging evidence suggests that sleep disturbances have a stronger influence on subsequent pain than vice versa. The neurobiological underpinnings of this relationship, particularly during adolescence, are poorly understood. This review examines the current literature regarding sleep and pain in adolescence, with a particular focus on the neurobiological mechanisms underlying pain, sleep problems, and the neural circuitry that potentially links the two. Finally, a research agenda is outlined to stimulate future research on this topic. Given the high prevalence of these health issues during adolescence and the debilitating effects they inflict on nearly every domain of development, it is crucial that we determine the neurobiological mechanisms fundamental to this relationship and identify potential therapeutic strategies.
Improvement in clinical outcomes after dry needling versus myofascial release on pain pressure thresholds, quality of life, fatigue, pain intensity, quality of sleep, anxiety, and depression in patients with fibromyalgia syndrome
Abstract
Purpose: To compare the effectiveness of dry needling versus myofascial release on myofascial trigger points pain in cervical muscles, quality of life, impact of symptoms pain, quality of sleep, anxiety, depression, and fatigue in patients with fibromyalgia syndrome.
Method: A single-blind randomized controlled trial was conducted. Sixty-four subjects with fibromyalgia were randomly assigned to a dry needling group or a myofascial release group. Pain pressure thresholds of myofascial trigger points were evaluated in the cervical muscles. In addition, quality of life, impact of fibromyalgia symptoms, quality of sleep, intensity of pain, anxiety and depression symptoms, impact of fatigue at baseline and post treatment after four weeks of intervention were evaluated.
Results: Significant improvement was found in most pain pressure thresholds of the myofascial trigger points in cervical muscles in the dry needling group compared to myofascial release (p < 0.05). Similarly, these differences between groups were found for the components of quality of life of physical function (F = 12.74, p = 0.001), physical role (F = 11.24, p = 0.001), body pain (F =30.26, p < 0.001), general health (F = 15.83, p < 0.001), vitality (F = 13.51, p = 0.001), social function (F = 4.73, p = 0.034), emotional role (F = 8.01, p = 0.006), and mental health (F = 4.95, p = 0.030). Similar results were achieved for total impact of FMS symptoms (F = 42.91, p < 0.001), quality of sleep (F = 11.96, p = 0.001), state anxiety (F = 7.40, p = 0.009), and trait anxiety (F = -14.63, p < 0.001), hospital anxiety and depression (F = 20.60, p < 0.001), general pain intensity (F = 29.59, p < 0.001), and fatigue (F = -25.73, p < 0.001).
Conclusion: The dry needling therapy showed higher improvements in comparison with myofascial release therapy for pain pressure thresholds, the components of quality of life of physical role, body pain, vitality and social function, as well as the total impact of FMS symptoms, quality of sleep, state and trait anxiety, hospital anxiety-depression, general pain intensity and fatigue. Implications for rehabilitation Dry needling therapy reduces myofascial trigger point pain in the short term in patients with fibromyalgia syndrome. This therapeutic approach improves anxiety, depression, fatigue symptoms, quality of life, and sleep after treatment. Dry needling and myofascial release therapies decrease intensity of pain, and the impact of fibromyalgia symptoms in this population. These intervention approaches should be considered in an independent manner as complementary therapies within a multidisciplinary setting.
[Sleep disorders in chronic pain syndromes]
Abstract
Sleep disorders and pain syndromes are widespread in the general population. This review presents data on comorbidity of these phenomena and possibility of their mutual influence on each other including data based on long-term prospective studies. Studies of pain syndromes and sleep disorders dynamics are analyzed in detail. Anatomical basis of sleep-pain interactions is described, and results of the emotional influence on sleep and pain associations are presented. Non-pharmacological and drug-based approaches to treatment with detailed description of the biochemical basis of their action are considered. The authors conclude that pain syndromes and sleep disorders have reciprocal relations; the improvement of sleep quality helps in various pain syndromes; sleep normalization could play a preventive role with regard to pain.
Sleep, chronic pain, and opioid risk for apnea
Abstract
Pain is an unwelcome sleep partner. Pain tends to erode sleep quality and alter the sleep restorative process in vulnerable patients. It can contribute to next-day sleepiness and fatigue, affecting cognitive function. Chronic pain and the use of opioid medications can also complicate the management of sleep disorders such as insomnia (difficulty falling and/or staying asleep) and sleep-disordered breathing (sleep apnea). Sleep problems can be related to various types of pain, including sleep headache (hypnic headache, cluster headache, migraine) and morning headache (transient tension type secondary to sleep apnea or to sleep bruxism or tooth grinding) as well as periodic limb movements (leg and arm dysesthesia with pain). Pain and sleep management strategies should be personalized to reflect the patient's history and ongoing complaints. Understanding the pain-sleep interaction requires assessments of: i) sleep quality, ii) potential contributions to fatigue, mood, and/or wake time functioning; iii) potential concomitant sleep-disordered breathing (SDB); and more importantly; iv) opioid use, as central apnea may occur in at-risk patients. Treatments include sleep hygiene advice, cognitive behavioral therapy, physical therapy, breathing devices (continuous positive airway pressure - CPAP, or oral appliance) and medications (sleep facilitators, e.g., zolpidem; or antidepressants, e.g., trazodone, duloxetine, or neuroleptics, e.g., pregabalin). In the presence of opioid-exacerbated SDB, if the dose cannot be reduced and normal breathing restored, servo-ventilation is a promising avenue that nevertheless requires close medical supervision.
Sleep and Pain: A Systematic Review of Studies of Mediation
Abstract
Objectives: A relationship between sleep and pain is well established. A better understanding of the mechanisms that link sleep and pain intensity is urgently needed to optimize pain management interventions. The objective of this systematic review was to identify, synthesize, and critically appraise studies that have investigated putative mediators on the path between sleep and pain intensity.
Methods: A systematic search of 5 electronic bibliographic databases (EMBASE, MEDLINE, CINAHL, PsycINFO, and the Cochrane Central Register of Controlled Trials) was conducted. Eligible studies had to apply a formal test of mediation to variables on the path between a sleep variable and pain intensity or vice versa. All searches, data extraction and quality assessment were conducted by at least 2 independent reviewers.
Results: The search yielded 2839 unique articles, 9 of which were eligible. Of 13 mediation analyses, 11 investigated pathways from a sleep variable to pain intensity. Putative mediators included affect/mood, depression and/or anxiety, attention to pain, pain helplessness, stress, fatigue, and physical activity. Two analyses investigated pathways from pain intensity to a sleep variable, examining the potentially mediating role of depressive symptoms and mood. Although evidence supported a mediating role for psychological and physiological aspects of emotional experiences and attentional processes, methodological limitations were common, including use of cross-sectional data and minimal adjustment for potential confounders.
Discussion: A growing body of research is applying mediation analysis to elucidate mechanistic pathways between sleep and pain intensity. Currently sparse evidence would be illuminated by more intensively collected longitudinal data and improvements in analysis.
The association between pain and sleep in fibromyalgia
Abstract
To clarify the association between pain and sleep in fibromyalgia. Methods: Electronic databases, including PsycINFO, the Cochrane database for systematic reviews, PubMed, EMBASE, and Ovid were searched to identify eligible articles. Databases independently screened and the quality of evidence using a reliable and valid quality assessment tool was assessed. Results: In total, 16 quantitative studies fulfilled the inclusion criteria. According to the results, increased pain in fibromyalgia was associated with reduced sleep quality, efficiency, and duration and increased sleep disturbance and onset latency and total wake time. Remarkably, depressive symptoms were also related to both pain and sleep in patients with fibromyalgia. Conclusion: Management strategies should be developed to decrease pain while increasing sleep quality in patients with fibromyalgia. Future studies should also consider mood disorders and emotional dysfunction, as comorbid conditions could occur with both pain and sleep disorder in fibromyalgia.
Pain and sleep : A bidirectional relationship
Abstract
Disturbed sleep and persistent pain are common in old people. Persistent pain has a well proven impact on sleep but the relationship between both phenomena is bidirectional since disturbed sleep affects pain perception by lowering the pain threshold. An optimal disease management takes both phenomena into account.
Sleep deficiency and chronic pain: potential underlying mechanisms and clinical implications
Abstract
Pain can be both a cause and a consequence of sleep deficiency. This bidirectional relationship between sleep and pain has important implications for clinical management of patients, but also for chronic pain prevention and public health more broadly. The review that follows will provide an overview of the neurobiological evidence of mechanisms thought to be involved in the modulation of pain by sleep deficiency, including the opioid, monoaminergic, orexinergic, immune, melatonin, and endocannabinoid systems; the hypothalamus-pituitary-adrenal axis; and adenosine and nitric oxide signaling. In addition, it will provide a broad overview of pharmacological and non-pharmacological approaches for the management of chronic pain comorbid with sleep disturbances and for the management of postoperative pain, as well as discuss the effects of sleep-disturbing medications on pain amplification.
Sleep and Orofacial Pain
Abstract
Sleep and pain share a bidirectional relationship. Therefore, it is important for practitioners managing patients experiencing either sleep and/or pain issues to recognize and understand this complex association from a neurobiological perspective involving neuroanatomic and neurochemical processes. Accounting for the influence of pain on the various aspects of sleep and understanding its impact on various orofacial pain disorders assists in developing a prudent management approach. Screening for sleep disorders benefits practitioners in identifying these individuals. Instituting evidence-based multidisciplinary management strategies using both behavioral and pharmacologic strategies enhances the delivery of appropriate care.
The Effects of Pain, Gender, and Age on Sleep/Wake and Circadian Rhythm Parameters in Oncology Patients at the Initiation of Radiation Therapy
Abstract
To date, no studies have evaluated for differences in subjective and objective measures of sleep disturbance in oncology outpatients with and without pain. This descriptive study, recruited 182 patients from 2 radiation therapy (RT) departments at the time of the patient's simulation visit. Approximately 38% of the sample reported moderate to severe pain (ie, worst pain intensity of 6.2 ± 2.4). After controlling for age, patients in pain reported worse sleep quality and more sleep disturbance using the Pittsburgh Sleep Quality Index. With the General Sleep Disturbance Scale, patients in pain reported poorer sleep quality, increased use of sleep medications, and more daytime sleepiness. In addition using an objective measure of sleep disturbance (ie, actigraphy), significant gender × pain interactions were found for sleep onset latency, percentage of time awake at night, wake duration, total sleep time, and sleep efficiency. While no differences were found in female patients, males in pain had worse scores than males without pain. Findings from this study suggest that pain and sleep disturbance are prevalent in oncology outpatients and that a patient's age and gender need to be considered in any evaluation of the relationship between pain and sleep.
Massage therapy in cortisol circadian rhythm, pain intensity, perceived stress index and quality of life of fibromyalgia syndrome patients
Abstract
We investigate the effects of a massage therapy program (MTP) in cortisol concentration (CC), intensity of pain, quality of life and perceived stress index of fibromyalgia patients. Volunteers (n = 24, aged 26-55 years) were treated with MT, twice a week for three months. They answered the Fibromyalgia Impact Questionnaire (FIQ), Perceived Stress Questionnaire (PSQ) and McGill Pain Questionnaire (MPQ-Br), and collected saliva to evaluate CC before and after the end of each month. The MT had improvement in quality of life, according to the FIQ results, and promoted reduction in PSQ values after the second (PSQ2-0.62 ± 0.04vsPSQ0-0.71 ± 0.04) and third month (PSQ3-0.64 ± 0.04vsPSQ0-0.71 ± 0.04). The MTP also promoted reduction in pain after the third month (MQP-Br1-44.50 ± 2.15vsMQP-Br4-35.38 ± 3.71). Despite PSQ reduction, the CC were not affected by the program. This pilot suggests that this treatment improved quality of life, reduced perceived stress index and pain in these volunteers.
The Effects of Shift Work and Interaction Between Shift Work and Overweight/Obesity on Low Back Pain in Nurses: Results From a Longitudinal Study
Abstract
OBJECTIVE: To examine whether shift work is a risk factor for low back pain (LBP) and the interaction effects of shift work and overweight/obesity on LBP over time among nurses. METHODS: A longitudinal study over 2 years. Measurements included reported LBP, shift work status, and selected potential confounders. RESULTS: Among 928 LBP-free nurses at baseline, 319 (34.4%) developed LBP over 2 years. After adjusting for confounders, shift workers were 1.15 times more likely to develop LBP (adjusted odds ratio [aOR], 1.15; 95% confidence interval, 1.05 to 1.40; P = 0.03). The interaction analysis showed that overweight/obese shift workers were more likely to develop LBP than day workers (overweight: aOR, 1.23 vs aOR, 1.03, respectively; obesity: aOR, 1.34 vs aOR, 1.10, respectively). CONCLUSIONS: Our findings suggest that shift workers are at a higher risk of developing LBP over time, especially those who are overweight/obese.
Night-shift work is associated with increased pain perception
Abstract
Objectives The aim of the present study was to determine whether shift workers exhibit increased perception of experimentally induced pain after working night shifts. Methods The study was a paired cross-over design with two sleep conditions, after at least two nights of habitual sleep and after two consecutive night shifts at work. Fifty-three nurses in rotating shift work participated. The sensitivity to electrically induced pain, heat pain, cold pain, pressure pain and pain inhibition was determined experimentally in each sleep condition. Sleepiness and vigilance were also assessed. Results Night-shift work (NSW) increased the sensitivity to electrically induced pain and heat pain (P≤0.001). Relative to habitual sleep, electrically induced pain increased by 22.3% and heat pain increased by 26.5%. The sensitivity to cold and pressure pain did not change, changes relative to habitual sleep was <5% (P>0.5). Pain inhibition was 66.9% stronger after NSW versus after habitual sleep (P<0.001). Sleepiness (measured with the Karolinska Sleepiness Scale) increased from 4.1 after habitual sleep to 6.9 after NSW (P<0.001). Vigilance decreased after NSW, measured as a 0.03-second decrease in reaction time (P<0.005). Conclusions Changes in pain sensitivity after NSW is measurable with clinically relevant effect sizes and may be an important marker for studies comparing the physiological effects of different shift work schedules. Explanations for the differential effect on different pain modalities should be a focus for future studies.
Determining the association between low back pain and occupational stress in nurses
Abstract:
Introduction: The reported 12 months prevalence of low back pain in nurses ranges from 43% to 76%. In most researches physical factors were only a part of high prevalence of low back pain in nurses. This study was conducted to determine the association between occupational stress and low back pain in nurses.
Materials and Methods: In this case-control study, 80 nurses as case group and 80 nurses as control group were selected via convenience sampling. Case group were defined as those subjects who had experienced low back pain in the last 12 months. Control group were defined as those subjects who had not experienced low back pain in the last 12 months. A questionnaire was used for data collection which consisted of 3 sections: demographic information, history of low back pain and occupational stress. Data was analyzed using paired T, Mann-Whitney, and Chi-square tests, correlation coefficient and one way ANOVA.
Results: Results indicated that, there was an association between low back pain and occupational stress (p<0/01).Also an association existed between low back pain and working hours per month (p<0/05). Statistical tests showed no significant difference between the two groups in terms of age, gender, marital status, number of childbirth, number of pregnancy, smoking, sport, work shift, number of years spent in the hospital (nursing experience).
Conclusion: Results indicated that occupational stress in case group was more than control group. Since there was not any significant difference between other factors and low back pain, it can be concluded that there is an association between low back pain and occupational stress.
Perceived work stress, overcommitment, and self-reported musculoskeletal pain: Across-sectional investigation
Abstract
The objective of this study was to analyze associations of three indicators of perceived work stress (physical job demand, low control at work, and an imbalance between effort and reward), and of overcommitment, a personal pattern of coping with work demands, with musculoskeletal pain. A standardized questionnaire measuring these conditions in addition to self-reported musculoskeletal pain at different locations was administered to a group of 316 male and female employees of a public transport enterprise. After we adjusted for confounding effects of age, sex, socioeconomic status, shift work, and negative affectivity, we observed elevated prevalence odds ratios in employees who scored high on overcommitment, who were exposed to physical job demand, and, to a lesser extent, who reported psychosocial work stress. Results have implications for a more comprehensive approach to primary and secondary prevention of musculoskeletal pain.
The effects of total and REM sleep deprivation on laser-evoked potential threshold and pain perception
Abstract
We investigated the effects of total and rapid eye movement (REM) sleep deprivation on the thermal nociceptive threshold and pain perception using the objective laser-evoked potential (LEP) and the subjective visual analogue scale (VAS). Twenty-eight male adult volunteers were assigned into Control (CTRL), Total (T-SD), and REM (REM-SD) Sleep Deprivation groups. The T-SD and REM-SD volunteers were totally or selectively deprived of sleep for 2 and 4 consecutive nights, respectively. Pain parameters were measured daily during the experimental period. Volunteers were stimulated on the back of the hand by blocks of 50 diode laser pulses. Intensities increased between successive blocks, ranging from nonnoxious to noxious levels, and the LEP threshold was identified based on the evoked-response onset. Both the LEP threshold and VAS ratings were significantly increased after the second night of T-SD. No significant variations were observed in the REM-SD group, suggesting a predominant role for slow wave sleep rather than selective REM-SD in pain perception. Also, for both sleep-deprived groups, the mean values of the LEP threshold and VAS ratings showed a gradual increase that was proportional to the SD deprivation time, followed by a decrease after 1 night of sleep restoration. These findings demonstrate a hyperalgesic modification to pain perception (as reflected by the augmented VAS) and a concomitant increase in the LEP threshold following T-SD, an apparently contradictory effect that can be explained by differences in the ways that attention affects these pain measurements.
Induction of neurasthenic musculoskeletal pain syndrome by selective sleep stage deprivation.
Abstract
Two groups of young, healthy, nonathletic volunteers were subjected to selective sleep stage deprivation. Six subjects were deprived of stage 4 sleep and seven subjects of REM sleep. The stage 4 deprived group reported more musculoskeletal symptoms during the deprivation condition than did the REM deprived group. The stage 4 deprived group also showed a significant increase in muscle tenderness between the baseline and deprivation conditions and an altered pattern of overnight change in muscle tenderness in response to deprivation. The REM deprived group did not show either of these changes. These results are discussed in the light of the previously postulated relationship between NREM sleep disturbance and muscoloskeletal pain in patients with so-called "Fibrositis syndrome."
Decreased alertness due to sleep loss increases pain sensitivity in mice
Abstract
Extended daytime and nighttime activities are major contributors to the growing sleep deficiency epidemic, as is the high prevalence of sleep disorders like insomnia. The consequences of chronic insufficient sleep for health remain uncertain. Sleep quality and duration predict presence of pain the next day in healthy subjects, suggesting that sleep disturbances alone may worsen pain, and experimental sleep deprivation in humans supports this claim. We demonstrate that sleep loss, but not sleep fragmentation, in healthy mice increases sensitivity to noxious stimuli (referred to as 'pain') without general sensory hyper-responsiveness. Moderate daily repeated sleep loss leads to a progressive accumulation of sleep debt and also to exaggerated pain responses, both of which are rescued after restoration of normal sleep. Caffeine and modafinil, two wake-promoting agents that have no analgesic activity in rested mice, immediately normalize pain sensitivity in sleep-deprived animals, without affecting sleep debt. The reversibility of mild sleep-loss-induced pain by wake-promoting agents reveals an unsuspected role for alertness in setting pain sensitivity. Clinically, insufficient or poor-quality sleep may worsen pain and this enhanced pain may be reduced not by analgesics, whose effectiveness is reduced, but by increasing alertness or providing better sleep.
Sleep duration mediates abdominal and lower-extremity pain after night work in nurses
Abstract and Figures
Objectives The aim of this study was to investigate the association between different working shifts (i.e. morning, evening, night shifts) and headache, musculoskeletal and abdominal pain, and the extent to which reduced sleep duration could account for these associations. Methods Nurses (N = 679, 649 female, aged 22–53 years) were followed up for a period of 28 consecutive days, responding to a diary about sleep, shift type and pain complaints (measured on a Likert-type scale ranging from 0 to 3). Generalised structural equation modelling mediation analysis (GSEM) was performed to test whether shift type was associated with higher incidence or higher intensity of pain (headache, pain in neck/shoulders/upper back, upper extremity, low back, lower extremity and abdominal pain), and if this effect was mediated by sleep duration (continuous variable), after controlling for age, work and lifestyle factors. Results Pain scores in lower extremities were decreased following night shifts in general. However, when night shifts were followed by short sleep duration, the risk of pain in the lower extremities and abdominal pain were increased. Headache and pain in the upper extremity were increased after night shifts, but were not associated with sleep duration. Pain in the neck/shoulder/upper back and lower back was not related to shift work. Conclusions Among nurses in a three-shift rotating schedule, night shifts increased the risk of pain in several regions, but only pain in the lower extremities and abdomen was related to reduced sleep duration.
Association between sleep duration and musculoskeletal pain: The Korea National Health and Nutrition Examination Survey 2010-2015
Abstract
Both extremely long and short sleep durations have been associated with increased risk of numerous health problems. This study examined the association between self-reported sleep duration and reporting of musculoskeletal pain in the adult Korean population.
This study included data from 17,108 adults aged ≥50 years, obtained from the Korea National Health and Nutrition Examination Survey 2010–2012 and 2013–2015. Self-reported daily hours slept and the presence of musculoskeletal pain in knee joint, hip joint, or low back were examined. Patients were stratified into 5 groups by their sleep duration: ≤5, 6, 7, 8, or ≥9 h. Multivariate logistic regression analysis was performed, adjusting for covariates including age, sex, marital status, smoking, alcohol use, family income level, education, physical exercise, body mass index (BMI), and stress level.
A U-shaped relationship was observed between the length of sleep duration and the presence of musculoskeletal pain. After adjusting for covariates, sleep duration of ≤5 h or ≥9 h was significantly associated with musculoskeletal pain experienced for more than 30 days over a 3-month period. We also found that the presence of multi-site musculoskeletal pain was significantly higher among those who slept for ≤5 h or ≥9 h than in those who slept for 7 h.
These findings suggest that either short or long sleep duration is associated with musculoskeletal pain among Korean adults.
Effects of mindfulness-based stress reduction combined with music therapy on pain, anxiety, and sleep quality in patients with osteosarcoma
Abstract
Objectives: To evaluate the effects of mindfulness-based stress reduction (MBSR) combined with music therapy (MT) on clinical symptoms in patients with osteosarcoma.
Methods: Patients diagnosed with osteosarcoma were assessed for eligibility. A total of 101 patients were ultimately randomized into the intervention and control groups. Both groups received routine care. Eight sessions of MBSR and MT psychotherapy were conducted in the intervention group, while the control group received no psychological intervention. Patients were assessed regarding pain, anxiety, and sleep quality at two distinct stages: before and after the intervention.
Results: There were no significant differences in sociodemographic and clinical parameters between the intervention and control groups at baseline. The intervention program significantly alleviated psychological and physiological complications in patients with osteosarcoma. Specifically, the study revealed that 8 weeks of the combined MBSR/MT intervention effectively reduced pain and anxiety scores and improved the quality of sleep in patients.
Conclusion: MBSR combined with MT significantly alleviated clinical symptoms, and could be considered a new, effective psychotherapeutic intervention for patients with osteosarcoma.
Preoperative sleep quality affects postoperative pain and function after total joint arthroplasty: a prospective cohort study
Abstract
Background: The relationship between preoperative sleep quality and postoperative clinical outcomes after total joint arthroplasty (TJA) is unclear. We performed a prospective cohort study to determine whether preoperative sleep quality was correlated with postoperative outcomes after TJA.
Methods: In this prospective cohort study, 994 patients underwent TJA. Preoperative sleep measures included scores on the Pittsburgh Sleep Quality Index (PSQI), the Epworth Sleepiness Scale (ESS), and a ten-point sleep quality scale. The primary study outcome measured was the visual analog scale (VAS) pain score to 12 weeks postoperation. The consumption of analgesic rescue drugs (oxycodone and parecoxib) and postoperative length of stay (LOS) were recorded. We also measured functional parameters, including range of motion (ROM), Knee Society Score (KSS), and Harris hip score (HHS).
Results: The mean age for total knee and hip arthroplasties was 64.28 and 54.85 years, respectively. The PSQI scores were significantly correlated with nocturnal and active pain scores and ROM and functional scores from postoperative day 1 (POD1) to POD3. In addition, significant correlation was noted between the correlation between the active pain scores and ESS scores in the TKA group at postoperative 3 months. The consumption of analgesics after joint arthroplasty was significantly correlated with the PSQI scores. Moreover, significant correlations were noted between the sleep parameters and postoperative length of hospital stay (LOS).
Conclusion: Preoperative sleep parameters were correlated with clinical outcomes (i.e., pain, ROM, function, and LOS) after TJA. Clinicians should assess the sleep quality and improve it before TJA.
Pain, sleep patterns and health-related quality of life in paediatric patients with cancer
Abstract
Purpose: To compare sleep and health-related quality of life (HRQOL) in children and adolescents with cancer who had pain, with those who had no pain during hospitalisation.
Method: A prospective comparative study was used to collect data from paediatric oncology units in three countries (Portugal, Brazil, USA). Participants (n = 118; 8-18 years) completed the Quality of Life Inventory (PedsQL) Cancer module, which includes a pain subscale, and wore a wrist actigraph for at least 72 hr.
Results: Almost half of the participants (48.3%) reported having pain. Sleep patterns were not affected by pain. Girls, adolescents and patients diagnosed with leukaemia/lymphoma who reported pain, had significantly lower HRQOL scores. Low sleep duration and HRQOL were found, irrespectively of pain status.
Conclusions: The low sleep duration and HRQOL score in children and adolescents with cancer highlight the importance of physical and psychosocial nursing interventions during hospitalisation. The mediating effect of gender, age and diagnoses on the relation between pain and HRQOL needs to be further understood.
Pain Extent, Pain Intensity, and Sleep Quality in Adolescents and Young Adults
Objectives. Pain has been shown to be associated with poor sleep quality. The aim of this study was to better understand the role that pain intensity and pain extent (number of painful areas) may play in the sleep quality of young people with acute and chronic pain.
Design. Cross-sectional survey.
Setting and Patients. A convenience sample of adolescents and young adults with acute or chronic pain; 414 individuals ages 12 to 24 (44% with chronic pain).
Methods. We performed a hierarchical regression analysis with sleep as the dependent variable and pain intensity, extent, age and pain chronicity as predictors.
Results. Pain extent and pain intensity made significant and independent contributions to the prediction of sleep quality (βs = 0.23 [P < 0.001] and 0.14 [P < 0.01]). Young adults reported poorer sleep than adolescents (β = 0.13, P < 0.01). Two significant interactions emerged: age × intensity (β = 0.39, P < 0.05) and chronicity × intensity (β = 0.88, P < 0.001).
Conclusions. Sleep quality in young people could be improved by teaching them strategies to better manage pain intensity and pain extent. Clinical trials to evaluate the efficacy of (and best timing for) pain interventions to improve sleep quality are warranted.
Relationships Between Sleep Quality and Pain-Related Factors for People with Chronic Low Back Pain: Tests of Reciprocal and Time of Day Effects
Abstract
Background: Poor sleep quality among people with chronic low back pain appears to be related to worse pain, affect, poor physical function, and pain catastrophizing. The causal direction between poor sleep and pain remains an open question, however, as does whether sleep quality exerts effects on low back pain differently across the course of the day.
Purpose: This daily diary study examined lagged temporal associations between prior night sleep quality and subsequent day pain, affect, physical function and pain catastrophizing, the reverse lagged temporal associations between prior day pain-related factors and subsequent night sleep quality, and whether the time of day during which an assessment was made moderated these temporal associations.
Methods: Chronic low back pain patients (n = 105) completed structured electronic diary assessments five times per day for 14 days. Items included patient ratings of their pain, affect, physical function, and pain catastrophizing.
Results: Collapsed across all observations, poorer sleep quality was significantly related to higher pain ratings, higher negative affect, lower positive affect, poorer physical function, and higher pain catastrophizing. Lagged analyses averaged across the day revealed that poorer prior night sleep quality significantly predicted greater next day patient ratings of pain, and poorer physical function and higher pain catastrophizing. Prior poorer night sleep quality significantly predicted greater reports of pain, and poorer physical function, and higher pain catastrophizing, especially during the early part of the day. Sleep quality × time of day interactions showed that poor sleepers reported high pain, and negative mood and low function uniformly across the day, whereas good sleepers reported relatively good mornings, but showed pain, affect and function levels comparable to poor sleepers by the end of the day. Analyses of the reverse causal pathway were mostly nonsignificant.
Conclusions: Sleep quality appears related not only to pain intensity but also to a wide range of patient mood and function factors. A good night's sleep also appears to offer only temporary respite, suggesting that comprehensive interventions for chronic low back pain not only should include attention to sleep problems but also focus on problems with pain appraisals and coping.
A Systematic Review and Meta-Analysis of Mindfulness-Based (Baduanjin) Exercise for Alleviating Musculoskeletal Pain and Improving Sleep Quality in People with Chronic Diseases
Abstract
Objective: we performed the first systematic review with meta-analyses of the existing studies that examined mindfulness-based Baduanjin exercise for its therapeutic effects for individuals with musculoskeletal pain or insomnia.
Methods: Both English- (PubMed, Web of Science, Elsevier, and Google Scholar) and Chinese-language (CNKI and Wangfang) electronic databases were used to search relevant articles. We used a modified PEDro scale to evaluate risk of bias across studies selected. All eligible RCTS were considered for meta-analysis. The standardized mean difference was calculated for the pooled effects to determine the magnitude of the Baduanjin intervention effect. For the moderator analysis, we performed subgroup meta-analysis for categorical variables and meta-regression for continuous variables.
Results: The aggregated result has shown a significant benefit in favour of Baduanjin at alleviating musculoskeletal pain (SMD = -0.88, 95% CI -1.02 to -0.74, p < 0.001, I² = 10.29%) and improving overall sleep quality (SMD = -0.48, 95% CI -0.95 to -0.01, p = 004, I² = 84.42%).
Conclusions: Mindfulness-based Baduanjin exercise may be effective for alleviating musculoskeletal pain and improving overall sleep quality in people with chronic illness. Large, well-designed RCTs are needed to confirm these findings.
Sleep quality in subjects suffering from chronic pain
Abstract
Background: Sleeping problems are very common in patients with chronic pain. The aim of the study was to investigate the association between different dimensions of chronic pain and sleep quality in chronic pain patients.
Methods: In this cross-sectional interview-based questionnaire study, patients from 3 different pain treatment centers in Vienna aged 18-65 years, with pain lasting 3 months or longer were asked to participate. The association between the short-form McGill pain questionnaire (SF-MPQ) and sleep quality (sleep onset latency, interrupted sleep due to pain, sleep duration and recovering effect of sleep) was assessed.
Results: In this study 121 patients (male 32, female 89, mean age 49 ± 9 years) could be analyzed. Of the patients 38.8% needed more than 30 min for falling asleep, 63.6% reported sleep fragmentation, 30.6% slept less than 5 h and 60.3% reported no recovering effect of sleep. The strongest associations between pain characteristics and sleep quality were found for pain intensity and affective pain aspects. Logistic regression analyses revealed that one point more in the total score of SF-MPQ increased the odds of needing more than 30 min for falling asleep, waking up more than 3 times due to pain, sleeping less than 5 h, and perceiving the sleep as non-recovering, by 6%. Adjusting for physical and psychological quality of life lowered the odds ratios and the association was no longer significant.
Conclusion: The results underline the importance of paying attention to sleep quality in patients with chronic pain. The results also indicate that psychological factors might mediate the association between pain and sleep quality.
Dental Health
Bruxism defined and graded: an international consensus
Abstract
To date, there is no consensus about the definition and diagnostic grading of bruxism. A written consensus discussion was held among an international group of bruxism experts as to formulate a definition of bruxism and to suggest a grading system for its operationalisation. The expert group defined bruxism as a repetitive jaw-muscle activity characterised by clenching or grinding of the teeth and/or by bracing or thrusting of the mandible. Bruxism has two distinct circadian manifestations: it can occur during sleep (indicated as sleep bruxism) or during wakefulness (indicated as awake bruxism). For the operationalisation of this definition, the expert group proposes a diagnostic grading system of 'possible', 'probable' and 'definite' sleep or awake bruxism. The proposed definition and grading system are suggested for clinical and research purposes in all relevant dental and medical domains.
[Sleep bruxism in children and adolescents]
Abstract
Bruxism is a rhythmic masticatory muscle activity, characterized by teeth grinding and clenching. This is a phenomenon mainly regulated by the central nervous system and peripherally influenced. It has two circadian manifestations, during sleep (sleep bruxism) and awake states (awake bruxism). Bruxism is much more than just tooth wearing. It is currently linked to orofacial pain; headaches; sleep disorders; sleep breathing disorders, such as apnea and hypopnea sleep syndrome; behavior disorders, or those associated with the use of medications. It is also influenced by psycho-social and behavior factors, which means that oromandibular parafunctional activities, temporomandibular disorders, malocclusion, high levels of anxiety and stress, among others, may precipitate the occurrence of bruxism. Nowadays, its etiology is multifactorial. The dentist and the pediatrician are responsible for its early detection, diagnosis, management, and prevention of its possible consequences on the patients. The aim of this review is to update the concepts of this disease and to make health professionals aware of its early detection and its timely management.
Associations between tooth wear and dental sleep disorders: A narrative overview
Abstract
Objectives: Tooth wear is a common finding in adult patients with dental sleep disorders. The aim of this paper was to review the literature on the possible associations between tooth wear and the following dental sleep disorders: sleep-related oro-facial pain, oral moistening disorders, gastroesophageal reflux disease (GERD), obstructive sleep apnoea syndrome (OSAS) and sleep bruxism.
Methods: A PubMed search was performed on 1 June 2018 using MeSH terms in the following query: Tooth Wear AND (Facial Pain OR Temporomandibular Joint Disorders OR Xerostomia OR Sialorrhea OR Gastroesophageal Reflux OR Sleep Apnea Syndrome OR Sleep Bruxism).
Results: The query yielded 706 reports on tooth wear and the mentioned dental sleep disorders. Several associations between tooth wear and the dental sleep disorders were suggested in the literature. It could be concluded that: (a) tooth wear is associated with dental pain and/or hypersensitivity; (b) oral dryness is associated with tooth wear, oro-facial pain and sleep bruxism; (c) GERD is associated with tooth wear, oro-facial pain, oral dryness, OSAS and sleep bruxism; (d) OSAS is associated with oral dryness, GERD and sleep bruxism; and (e) sleep bruxism is associated with tooth wear.
Conclusions: Tooth wear is associated with the dental sleep disorders oro-facial pain, oral dryness, GERD and sleep bruxism. The dental sleep disorders are interlinked with each other, which leads to indirect associations as well, and makes the consequences of each single condition difficult to disentangle. Knowledge of these associations is clinically relevant, but more research is needed to confirm their validity.
Oral health in children with sleep-disordered breathing: a cross-sectional study
Abstract
Sleep-disordered breathing (SDB) is associated with a wide range of oral manifestations, including adeno-tonsillar hypertrophy, narrow dentoalveolar width, increased overjet, reduced overbite, and malocclusion. There are no studies about the relationship between SDB and poor oral health in the pediatric population. The aim of this study was to investigate oral health status and oral health-related quality of life (OHRQoL) in children at risk of SDB (SDB+), compared with a control group, not at risk for SDB (SDB). The current cross-sectional study recruited consecutive children, aged between 8 and 17 years, from a university-based dental clinic. Caregivers completed the Pediatric Sleep Questionnaire (PSQ) to stratify risk of SDB. Both children and caregivers completed the Child Oral Health Impact Profile (COHIP) to measure the OHRQoL. A dental exam was conducted to evaluate dental caries, periodontal status, oropharyngeal characteristics, and dental occlusion. DMFS (decay-missing-filled for permanent teeth), dmfs (for primary teeth), PPD (pocket probing depth), parent COHIP score, child COHIP score, and BOP (bleeding on probing) were compared between children SDB+ and SDB-. In this study, 122 children were enrolled and divided into two equal subgroups (61 each). There was a significant association between SDB and all six outcomes (all p < 0.05) with higher values in SDB+ children. SDB+ was associated with a poorer OHRQoL, and a greater COHIP score for both parents and children. In conclusion, the current study suggests that the impact of SDB on oral health and OHRQoL in children is relevant and far-reaching. Therefore, it is necessary to closely monitor the oral health of SDB+ children, and, if appropriate, to use gentle non-pharmacological treatments able to reduce nasal congestion.
Impact of Sleep Bruxism on Oral Health-Related Quality of Life
Abstract
Purpose: To determine the prevalence of possible tooth grinding (TG) and possible sleep bruxism (SB) and to examine their impacts on oral health-related quality of life (OHRQoL) among Asian adults.
Materials and methods: A total of 3,072 subjects (18 to 65 years of age) from 12 dental centers were invited to complete a self-administered questionnaire on TG/SB and OHRQoL, and 2,417 were included in the study. Participants were subsequently categorized into three groups (no TG/SB, possible TG, and possible SB) based on the International Classification of Sleep Disorders. The 14-item Oral Health Impact Profile (OHIP-14) severity, extent, and prevalence scores were subsequently computed and compared. Data were examined using Kruskal-Wallis and Mann-Whitney U tests, Spearman correlation, and univariate regression analysis (P < .05).
Results: Of the 2,417 subjects (mean age 24.79 ± 7.49 years), 42.82% reported either possible TG (n = 921; 38.11%) or possible SB (n = 114; 4.72%). Significant differences in global and domain OHIP-14 scores were found between the groups, except for the extent scores in functional limitation and physical disability. Mean global severity scores of the possible SB group (9.36 ± 9.45) were 1.5- and 2.2-fold larger than the possible TG (6.39 ± 7.61) and no TG/SB (4.22 ± 6.15) groups, respectively. A significant but weak correlation (r = 0.14 to 0.19) was found between the number of positive responses for TG/SB and OHIP-14 severity scores.
Conclusions: A high prevalence of possible TG and SB was found among the Asian cohort studied. Possible TG and SB were significantly associated with poorer OHRQoL. The physical pain, psychologic discomfort, and psychologic disability domains were most influenced by TG/SB. More epidemiologic studies on the functional, physical, and psychosocial influences of SB are required.
Obstructive sleep apnea and orthodontics: An American Association of Orthodontists White Paper
Abstract
The Board of Trustees of the American Association of Orthodontists asked a panel of medical and dental experts in sleep medicine and dental sleep medicine to create a document designed to offer guidance to practicing orthodontists on the suggested role of the specialty of orthodontics in the management of obstructive sleep apnea. This White Paper presents a summary of the Task Force's findings and recommendations.
Poor sleep quality and oral health among older Brazilian adults
Abstract
Objectives: This study evaluates the association between normative and subjective oral health measures and poor self-reported sleep quality among community-dwelling older adults in Brazil.
Methods: This was a cross-sectional study with data from the Brazilian Longitudinal Study of Aging. The dependent variable was the poor sleep quality. Independent variables of interest included number of teeth and self-reported impact of oral health on eating/chewing and on maintaining emotional stability.
Results: Poor sleep quality was reported by 17.8 (95% CI 16.6; 19.2) of the participants, 29% of the participants were edentulous, and 30% had 20 or more teeth. Impacts of oral health on eating and maintaining emotional stability was found among 33.3% and 20% of the older adults, respectively. After adjusting for all oral health measures and covariates, the magnitude of the associations between the number of teeth and sleep quality was attenuated. Sleep quality was related to oral health impacts on eating (OR 1.19 [95% CI 1.00; 1.41]) and on emotional stability (OR 1.51 [95% CI 1.21; 1.87]).
Conclusions: This study found an association between oral health and sleep quality emphasizing the importance of oral health to general health.
Recognizing Poor Sleep Quality Factors During Oral Health Evaluations
Abstract
Oral health practitioners routinely perform oral health assessments for the dental patient to determine if oral disease is present. Systemic health is often a contributor to oral health concerns. One area in particular that has a direct effect on oral structures and oral health is poor sleep quality and open mouth breathing. Sleep is a fundamental process of the human body, which regulates core biological functions. Sleep quality reflects a person's ability to fall asleep, stay asleep, and enter into the various rejuvenating sleep cycles for the full duration. A person who does not obtain quality sleep can exhibit a wide range of oral, systemic, and cognitive health problems. Obstructive sleep apnea, which historically has been considered an adult male disease, is being recognized more often in women children. Research suggests various oral malformations found in newborns and young children can manifest as obstructive sleep apnea in adults. Oral health professionals are in a position to recognize the relationship between sleep and health, identify sleep quality concerns in relation to oral health assessments, administer sleep quality assessments, and determine appropriate referrals for further sleep quality evaluation.
Sleep bruxism and oral health-related quality of life in children: A systematic review
Abstract
Sleep bruxism (SB) is a masticatory muscle activity during sleep that can cause several consequences to the stomatognathic system. This systematic review investigated the impact of SB on oral health-related quality of life (OHRQoL) of 0- to 6-year-old children. Literature search was undertaken through PubMed/MEDLINE, LILACS, Scopus, TRIP, Livivo databases, and grey literature. The search was conducted with no publication year or language limits. Two reviewers independently selected the studies, extracted the data and assessed the risk of bias. The quality of evidence was assessed using GRADE. From 185 potentially eligible studies, three were included in the review. All studies were conducted in Brazil, published between 2015 and 2017, and used the B-ECOHIS instrument to evaluate OHRQoL. Two studies found no association between SB and OHRQoL, whereas one showed a significant negative impact of SB on the OHRQoL of children. SB was associated with respiratory problems, presence of tooth wear, dental caries, malocclusion as well as income and pacifier use. Risk of bias ranged from moderate to high, and the quality of evidence was judged as very low. The evidence is currently insufficient for definitive conclusions about the impact of SB on OHRQoL of children.
Stroke
[Sleep disorders and stroke: data of the esse-rf study]
Abstract
Aim: To assess the association between stroke and self-reported sleep disorders in the epidemiological studies of cardiovascular diseases in various regions of Russia (ESSE-RF).
Material and methods: A questionnaire survey included unorganized male and female population, aged 25 to 64 years, from 13 regions of the Russian Federation. In the analysis, answers to the question related to history of stroke: 'Did the doctor ever tell you that you had / had the following diseases?' (the 'Diseases' module) were included. The authors also evaluated answers about sleep duration, insomnia complaints, and sleepiness (the 'Sleep assessment' module).
Results and conclusion: Of 20 357 respondents, 422 (2%) confirmed the history of stroke. Both short and long sleep duration were not associated with stroke. Complaints of sleep disorders (snoring, sleep apnea, difficulty falling and maintaining sleep, as well as their combinations) were more frequently correlated with stroke. After adjustment for gender, age, body mass index, office blood pressure, the regression analysis showed that odds ratio was not significant for all complaints, except the combination of sleep apnea with frequent daytime sleepiness (1.7 (95% CI 1.04-2.8) (p=0.034). Therefore, symptoms of sleep-disordered breathing and insomnia are more common in respondents with the history of stroke. The combination of sleep apnea and frequent sleepiness complaints may indicate more severe sleep disorders in post-stroke patients.
Stroke during sleep and obstructive sleep apnea: there is a link
Abstract
Objectives: The onset of ischemic stroke symptoms has been established to have a diurnal variation, with a sizeable proportion (8-28%) occurring during sleep. Obstructive sleep apnea (OSA) has been established as an important risk factor for ischemic stroke. However, data on the relationship between OSA and wake-up stroke (WUS) has been scarce. The aim of our study is to determine the relationship between OSA and WUS.
Methods: This is a case-control study conducted on acute stroke patients who presented to one of two major medical centers in Riyadh of Saudi Arabia. Those who woke up with the symptoms were labeled as WUS, and those whose stroke occurred while awake were labeled as non wake-up stroke (NWUS). The Berlin Questionnaire, which was submitted to either the patient or his/her partner, was used to determine the frequency of OSA in the two groups.
Results: One hundred seven patients (60% males) with acute stroke were admitted between March 2016 and March 2017. Of the 40 patients with WUS, 29 (72.5%) had underlying OSA based on the Berlin Questionnaire, whereas only 30 (45%) of the 67 patients with NWUS have underlying OSA. Logistic regression analysis showed OSA is highly prevalent in the patients with WUS (OR = 3.25; 95% CI = 1.397-8.38; p = 0.0053).
Conclusion: OSA is an important risk factor for ischemic stroke during sleep. Health care providers must be vigilant in inquiring about symptoms suggestive of OSA in every ischemic stroke patient, especially the patient whose stroke occurred during sleep.
Slow Waves Promote Sleep-Dependent Plasticity and Functional Recovery after Stroke
Abstract
Functional recovery after stroke is associated with a remapping of neural circuits. This reorganization is often associated with low-frequency, high-amplitude oscillations in the peri-infarct zone in both rodents and humans. These oscillations are reminiscent of sleep slow waves (SW) and suggestive of a role for sleep in brain plasticity that occur during stroke recovery; however, direct evidence is missing. Using a stroke model in male mice, we showed that stroke was followed by a transient increase in NREM sleep accompanied by reduced amplitude and slope of ipsilateral NREM sleep SW. We next used 5 ms optical activation of Channelrhodopsin 2-expressing pyramidal neurons, or 200 ms silencing of Archeorhodopsin T-expressing pyramidal neurons, to generate local cortical UP, or DOWN, states, respectively, both sharing similarities with spontaneous NREM SW in freely moving mice. Importantly, we found that single optogenetically evoked SW (SWopto) in the peri-infarct zone, randomly distributed during sleep, significantly improved fine motor movements of the limb corresponding to the sensorimotor stroke lesion site compared with spontaneous recovery and control conditions, while motor strength remained unchanged. In contrast, SWopto during wakefulness had no effect. Furthermore, chronic SWopto during sleep were associated with local axonal sprouting as revealed by the increase of anatomic presynaptic and postsynaptic markers in the peri-infarct zone and corresponding contralesional areas to cortical circuit reorganization during stroke recovery. These results support a role for sleep SW in cortical circuit plasticity and sensorimotor recovery after stroke and provide a clinically relevant framework for rehabilitation strategies using neuromodulation during sleep.SIGNIFICANCE STATEMENT Brain stroke is one of the leading causes of death and major disabilities in the elderly worldwide. A better understanding of the pathophysiological mechanisms underlying spontaneous brain plasticity after stroke, together with an optimization of rehabilitative strategies, are essential to improve stroke treatments. Here, we investigate the role of optogenetically induced sleep slow waves in an animal model of ischemic stroke and identify sleep as a window for poststroke intervention that promotes neuroplasticity and facilitates sensorimotor recovery.
Wake-up stroke: From pathophysiology to management
Abstract
Wake-up strokes (WUS) are strokes with unknown exact time of onset as they are noted on awakening by the patients. They represent 20% of all ischemic strokes. The chronobiological pattern of ischemic stroke onset, with higher frequency in the first morning hours, is likely to be associated with circadian fluctuations in blood pressure, heart rate, hemostatic processes, and the occurrence of atrial fibrillation episodes. The modulation of stroke onset time also involves the sleep-wake cycle as there is an increased risk associated with rapid-eye-movement sleep. Furthermore, sleep may have an impact on the expression and perception of stroke symptoms by patients, but also on brain tissue ischemia processes via a neuroprotective effect. Obstructive sleep apnea syndrome is particularly prevalent in WUS patients. Until recently, WUS was considered as a contra-indication to reperfusion therapy because of the unknown onset time and the potential cerebral bleeding risk associated with thrombolytic treatment. A renewed interest in WUS has been observed over the past few years related to an improved radiological evaluation of WUS patients and the recent demonstration of the clinical efficacy of reperfusion in selected patients when the presence of salvageable brain tissue on advanced cerebral imaging is demonstrated.
Sleep Apnea Is a Risk Factor for Stroke and Vascular Dementia
Abstract
Purpose of review: In this article, we review the cerebrovascular complications of sleep apnea (SA). SA is the major sleep disorder associated with stroke and vascular dementia.
Recent findings: Sleep apnea syndrome of moderate to severe intensity affects 17% of 50-70-year-old men and 9% of 50-70-year-old women, making SA a notorious and prevalent disorder. SA increases the risk of hypertension, stroke, myocardial infarction, and atrial fibrillation (AF) and is closely linked to vascular dementia. In addition, SA may worsen the neurologic outcome in acute stroke patients and interferes with rehabilitation after stroke. Proper management of SA may decrease the clinical impact of stroke risk factors, improve neurologic outcome after stroke, and lessen the progression of subcortical ischemic vascular disease. In this article, we will cover the most salient pathologies that associate SA and cerebrovascular pathology.
Sleep and cognitive function in chronic stroke: a comparative cross-sectional study
Abstract
Poor sleep is common following stroke, limits stroke recovery, and can contribute to further cognitive decline post-stroke. However, it is unclear what aspects of sleep are different in older adults with stroke compared with those without, and whether the relationship between sleep and cognitive function differs by stroke history. We investigated whether older adults with stroke experience poorer sleep quality than older adults without stroke, and whether poor sleep quality attenuates cognitive performance among older adults with a history of stroke. Thirty-five age- and sex-matched older adults with stroke (age: 69.86 ± 1.13 years; 51.43% female) and without stroke (age: 69.83 ± 1.12; 51.43% female) were compared with respect to sleep quality using the MotionWatch8 (MW8) and Pittsburgh Sleep Quality Index (PSQI). Cognitive performance was indexed using the Alzheimer's Disease Assessment Scale Plus (ADAS-Cog Plus). Additionally, we examined whether poor sleep quality is associated with poorer cognitive performance among older adults with stroke. Older adults with stroke had longer MW8 measured sleep duration (27.82 ± 12.17 min; p = 0.03) and greater fragmentation (6.44 ± 2.24; p < 0.01), but did not differ in PSQI from their nonstroke peers. There was a significant group x sleep quality interaction for fragmentation (β = 0.02; p < 0.01) and efficiency (β = -0.03; p = 0.02) on ADAS-Cog Plus performance, whereby differences in cognitive performance between older adults with and without stroke were accentuated in the presence of poor sleep quality. Older adults with stroke have poorer sleep quality than their nonstroke counterparts, and older adults with stroke and poor sleep quality experience larger deficits in cognitive performance. Clinical Trial Registration: Vitality: Promoting Cognitive Function in Older Adults With Chronic Stroke (Vitality); https://clinicaltrials.gov/ct2/show/NCT01916486;
NCT01916486
.
Role of sleep-disordered breathing and sleep-wake disturbances for stroke and stroke recovery
Abstract
Background: Sleep-disordered breathing (SDB) and sleep-wake disturbances (SWD) are highly prevalent in stroke patients. Recent studies suggest that they represent both a risk factor and a consequence of stroke and affect stroke recovery, outcome, and recurrence.
Methods: Review of literature.
Results: Several studies have proven SDB to represent an independent risk factor for stroke. Sleep studies in TIA and stroke patients are recommended in view of the very high prevalence (>50%) of SDB (Class IIb, level of evidence B). Treatment of obstructive SDB with continuous positive airway pressure is recommended given the strength of the increasing evidence in support of a positive effect on outcome (Class IIb, level of evidence B). Oxygen, biphasic positive airway pressure, and adaptive servoventilation may be considered in patients with central SDB. Recently, both reduced and increased sleep duration, as well as hypersomnia, insomnia, and restless legs syndrome (RLS), were also suggested to increase stroke risk. Mainly experimental studies found that SWD may in addition impair neuroplasticity processes and functional stroke recovery. Treatment of SWD with hypnotics and sedative antidepressants (insomnia), activating antidepressants or stimulants (hypersomnia), dopaminergic drugs (RLS), and clonazepam (parasomnias) are based on single case observations and should be used with caution.
Conclusions: SDB and SWD increase the risk of stroke in the general population and affect short- and long-term stroke recovery and outcome. Current knowledge supports the systematic implementation of clinical procedures for the diagnosis and treatment of poststroke SDB and SWD on stroke units.
Sleep duration, midday napping, and sleep quality and incident stroke: The Dongfeng-Tongji cohort
Abstract
Objective: To investigate the associations of sleep duration, midday napping, sleep quality, and change in sleep duration with risk of incident stroke and stroke subtypes.
Methods: Among 31,750 participants aged 61.7 years on average at baseline from the Dongfeng-Tongji cohort, we used Cox regression models to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for incident stroke.
Results: Compared with sleeping 7 to <8 hours/night, those reporting longer sleep duration (≥9 hours/night) had a greater risk of total stroke (hazard ratio [HR] 1.23; 95% confidence interval [CI] 1.07-1.41), while shorter sleep (<6 hours/night) had no significant effect on stroke risk. The HR (95% CI) of total stroke was 1.25 (1.03-1.53) for midday napping >90 minutes vs 1-30 minutes. The results were similar for ischemic stroke. Compared with good sleep quality, those with poor sleep quality showed a 29%, 28%, and 56% higher risk of total, ischemic, and hemorrhagic stroke, respectively. Moreover, we observed significant joint effects of sleeping ≥9 hours/night and midday napping >90 minutes (HR 1.85; 95% CI 1.28-2.66), and sleeping ≥9 hours/night and poor sleep quality (HR 1.82; 95% CI 1.33-2.48) on risk of total stroke. Furthermore, compared with persistently sleeping 7-9 hours/night, those who persistently slept ≥9 hours/night or switched from 7 to 9 hours to ≥9 hours/night had a higher risk of total stroke.
Conclusions: Long sleep duration, long midday napping, and poor sleep quality were independently and jointly associated with higher risks of incident stroke. Persistently long sleep duration or switch from average to long sleep duration increased the risk of stroke.
Sleep Medicine: Stroke and Sleep
Abstract
Cerebrovascular disease encompassing both ischemic and hemorrhagic strokes are among the leading causes of disability and mortality globally. The current evidence strongly suggests that identifying and addressing sleep disorders should be a part of both primary and secondary stroke prevention. Stroke and sleep are 'bedfellows' since sleep disorders, including sleep-disordered breathing, parasomnias, sleep-related movement disorders, insomnia, and hypersomnia are intimately intertwined with co-morbid cardiovascular conditions and increase stroke risk. Post-stroke sleep disorders also impact stroke rehabilitation, quality of life, and if left untreated can contribute to stroke recurrence.
Fatigue after stroke: manifestations and strategies
Abstract
Purpose: To describe how fatigue is experienced by stroke survivors, how they understand and deal with fatigue and how fatigue impacts their daily life. Method: A qualitative interview study was carried out as part of a larger longitudinal study investigating the prevalence, characteristics and contributing factors to post-stroke fatigue. Thirty-two participants (15 men and 17 women) were strategically sampled to explore the experiences of fatigue. Participants were interviewed at 6 months, 1 year and 2 years post-stroke. Data were analysed applying a Grounded theory approach. Results: Patients clearly described and differentiated their experience between: (1) tiredness as an ordinary life event and (2) fatigue as a post-stroke life condition. Three fatigue-transforming strategies were identified, being on a mission, settling for less and stalling. Stalling seemed to put the stroke survivors in a particularly vulnerable situation. Over time, some participants moved between these two tiredness/fatigue manifestations and their range of strategies. Conclusions: Post-stroke fatigue is a new life experience different from ordinary tiredness and seems to be a significant problem in the stroke survivors’ struggle to regain a new normalcy. Intervention studies are needed to reduce the impact of post-stroke fatigue on coping and recovery.
Cognitive and Graded Activity Training Can Alleviate Persistent Fatigue After Stroke
Abstract
Background and Purpose—
Fatigue is a common, persistent consequence of stroke, and no evidence-based treatments are currently available to alleviate fatigue. A new treatment combining cognitive therapy (CO) with graded activity training (GRAT), called COGRAT, was developed to alleviate fatigue and fatigue-related symptoms. This study compared the effectiveness of the COGRAT intervention with a CO-only intervention after a 3-month qualification period without intervention.
Methods—
This randomized, controlled, assessor-blind clinical trial was conducted in 8 rehabilitation centers. Eighty-three stroke patients (>4 months after stroke) were randomly assigned to 12 weeks of CO or COGRAT after qualification. Seventy-three patients completed treatment and 68 were available at follow-up. Primary outcomes (Checklist Individual Strength–subscale Fatigue (CIS-f); self-observation list–fatigue (SOL-f)) and secondary outcomes (Hospital Anxiety and Depression Scale, Stroke-Adapted Sickness Impact Profile, SOL-pain, SOL-sleep-D, 6-minute walk test) were collected at baseline (before and after qualification period) and after treatment (immediate and 6-month follow-up).
Results—
The qualification period showed stable outcome measures. Both treatments showed significant beneficial effects on fatigue (CIS-f: ηp2=0.48, P<0.001) and other outcomes (except pain and anxiety) with intention-to-treat analyses. Gains for the COGRAT group exceeded those in the CO group on number of individuals showing clinical improvement on the CIS-f (≥8 points: 58% versus 24%) and on physical endurance (ηp2=0.20, P<0.001).
Conclusions—
A 12-week cognitive therapy program can alleviate persistent fatigue after stroke. The best results are obtained when cognitive therapy is augmented with graded activity training.
Model of Understanding Fatigue After Stroke
Fatigue is ubiquitous but it is more common and more severe in patients with acute and chronic conditions, including stroke. The reported proportion of people with fatigue after stroke ranges from 23% to 75%.1
The variation in proportion between studies reflects the heterogeneity in the studied populations, time since stroke, and assessment methods for fatigue. Fatigue is common immediately after stroke, and it tends to persist in most but not all patients. It contributes to lower quality of life and a higher risk of death.
How to manage and prevent fatigue is ranked by stroke survivors and health professionals among the top 10 research priorities relating to life after stroke.4
However, there is no effective treatment, which is partly because of our lack of knowledge of its mechanisms.
Fatigue after stroke may share some common underlying mechanisms with other conditions. For example, Zedlitz and colleagues found that the psychosocial profiles of stroke patients with fatigue were similar to those reported in patients with cancer, multiple sclerosis, and chronic fatigue syndrome.5
Several fatigue models have been developed for patients with other conditions; a myriad of biological, psychosocial, and behavioral factors, as well as other symptoms, such as pain and sleep problems, are involved. In this review, we explored whether these factors contribute to fatigue after stroke.
We systematically reviewed studies of post-stroke fatigue (PSF) and discussed the definition of PSF, its natural history, and its associations. By drawing on literature of fatigue in other conditions alongside evidence from stroke studies, we propose a conceptual model of PSF. This model is potentially useful in understanding the mechanisms of PSF and informing the development of its treatment.
Physical impairment, depressive symptoms and pre-stroke fatigue are related to fatigue in the acute phase after stroke
Abstract
Purpose. The aim of this study was to describe prevalence of fatigue and its relationship with demographic and clinical variables during the first 2 weeks (acute phase) following a stroke.
Method. Data were collected in a cross-sectional correlational study from face-to-face interviews using structured questionnaires and patient's medical records. The sample consists of 115 patients with first-ever stroke admitted to two hospitals in Norway in 2007 and 2008. Post-stroke fatigue was measured with the Fatigue Severity Scale (FSS). The FSS measure was applied in the analysis as a continuous variable, and also used to categorise patients into three groups of fatigue intensity: no fatigue (mean FSS-score <4), moderate fatigue (mean FSS-score = 4–4.9) and severe fatigue (mean FSS-score ≥5). Patients who reported fatigue lasting longer than 3 months before the stroke were defined as having prestroke fatigue.
Results. Pre-stroke fatigue was reported by 34 patients (30%). After stroke, 24% had severe fatigue, and fatigue was more common for women (57%). Controlling for sex and prestroke fatigue, the multivariate analysis showed that prestroke fatigue, lower physical function and depressive symptoms were related to post-stroke fatigue.
Conclusion. Pre-stroke fatigue and fatigue during the acute phase needs to be assessed in relation to physical functioning and depression during recovery and the rehabilitation process.
Interventions for post‐stroke fatigue
Background
Fatigue after stroke is common and distressing to patients. The best way to treat this fatigue is uncertain. Theoretically, several different interventions may be of benefit.
Objectives
To determine whether any treatment for fatigue after stroke reduces the proportion of patients with fatigue, or fatigue severity, or both, and to determine the effect of treatment on health‐related quality of life, disability, dependency and death, and whether such treatments are cost effective.
Search methods
We searched the Cochrane Stroke Group Trials Register (last searched January 2008), the Cochrane Central Register of Controlled Trials (The Cochrane Library Issue 1, 2008), MEDLINE (1950 to February 2008), EMBASE (1980 to February 2008), CINAHL (1982 to February 2008), AMED (1985 to February 2008), PsycINFO (1967 to February 2008), Digital Dissertations (1861 to March 2008), PsycBITE (searched March 2008), PEDro (searched March 2008), and British Nursing Index (1985 to March 2008). We also searched four trials registries, scanned reference lists, performed citation tracking of included trials, and contacted experts.
Selection criteria
The review author who performed the searches scrutinised all titles and abstracts, excluded irrelevant references, and obtained references for potentially relevant studies. A second review author independently scrutinised potentially relevant studies to determine whether they fulfilled inclusion criteria. We included randomised controlled trials of any intervention in patients with stroke where fatigue was a primary or secondary endpoint.
Data collection and analysis
The two review authors who scrutinised references independently extracted data. We performed a narrative review; we had intended to perform a meta‐analysis but this was not possible as the interventions were too diverse for data to be combined.
Main results
We identified three trials. One randomised 83 patients with emotional disturbance after stroke to fluoxetine or placebo. After correcting for differences in fatigue severity at baseline, there was no significant difference in fatigue between groups at follow up. The second trial randomised 31 women with subarachnoid haemorrhage to tirilazad or placebo, of whom 18 were available for follow up. There was no difference in fatigue between the two groups. The third trial investigated a chronic disease self‐management programme in 1150 patients with chronic diseases, of whom 125 had had a stroke. There was no difference in fatigue at follow up between the treatment and control in the subgroup with stroke.
Authors' conclusions
There is insufficient evidence available to guide the management of fatigue after stroke. Further trials are required.
Abstract
Objective To synthesise the association of shift work with major vascular events as reported in the literature.
Data sources Systematic searches of major bibliographic databases, contact with experts in the field, and review of reference lists of primary articles, review papers, and guidelines.
Study selection Observational studies that reported risk ratios for vascular morbidity, vascular mortality, or all cause mortality in relation to shift work were included; control groups could be non-shift (“day”) workers or the general population.
Data extraction Study quality was assessed with the Downs and Black scale for observational studies. The three primary outcomes were myocardial infarction, ischaemic stroke, and any coronary event. Heterogeneity was measured with the I2 statistic and computed random effects models.
Results 34 studies in 2 011 935 people were identified. Shift work was associated with myocardial infarction (risk ratio 1.23, 95% confidence interval 1.15 to 1.31; I2=0) and ischaemic stroke (1.05, 1.01 to 1.09; I2=0). Coronary events were also increased (risk ratio 1.24, 1.10 to 1.39), albeit with significant heterogeneity across studies (I2=85%). Pooled risk ratios were significant for both unadjusted analyses and analyses adjusted for risk factors. All shift work schedules with the exception of evening shifts were associated with a statistically higher risk of coronary events. Shift work was not associated with increased rates of mortality (whether vascular cause specific or overall). Presence or absence of adjustment for smoking and socioeconomic status was not a source of heterogeneity in the primary studies. 6598 myocardial infarctions, 17 359 coronary events, and 1854 ischaemic strokes occurred. On the basis of the Canadian prevalence of shift work of 32.8%, the population attributable risks related to shift work were 7.0% for myocardial infarction, 7.3% for all coronary events, and 1.6% for ischaemic stroke.
Conclusions Shift work is associated with vascular events, which may have implications for public policy and occupational medicine.
Sleep disorders and the risk of stroke
Abstract
Stroke is a major cause of disability and death in the United States and across the world, and the incidence and prevalence of stroke are expected to rise significantly due to an aging population. Obstructive sleep apnea, an established independent risk factor for stroke, is a highly prevalent disease that is estimated to double the risk of stroke. It remains uncertain whether non-apnea sleep disorders increase the risk of stroke. Areas covered: This paper reviews the literature describing the association between incident stroke and sleep apnea, rapid eye movement sleep behavior disorder, restless legs syndrome, periodic limb movements of sleep, insomnia, and shift work. Expert commentary: Trials of continuous positive airway pressure for stroke prevention in sleep apnea patients have been largely disappointing, but additional trials that target populations not yet optimally studied are needed. Self-reported short and long sleep duration may be associated with incident stroke. However, abnormal sleep duration may be a marker of chronic disease, which may itself be associated with incident stroke. The relationship between non-apnea sleep disorders and incident stroke deserves further attention. Identification of specific non-apnea sleep disorders or sleep problems that convey an increased risk for stroke may provide novel targets for stroke prevention.
Sleep duration versus sleep insufficiency as predictors of cardiometabolic health outcomes
Abstract
Objective: The objective of the present study was to investigate the relationship between sleep insufficiency and sleep duration, particularly regarding negative cardiometabolic health outcomes already considered to be affected by reduced sleep time.
Methods: A total of N=30,934 participants from the 2009 Behavioural Risk Factor Surveillance System (BRFSS) answered questions about their sleep duration as well as subjective feelings of sleep insufficiency. Outcomes included body mass index (BMI), obesity (BMI ≥ 30kgm(-2)) and history of hypertension, diabetes, hypercholesterolaemia, heart attack and stroke. Linear and logistic regression models examined whether cardiometabolic outcomes were associated with (1) sleep duration alone, (2) sleep insufficiency alone and (3) the combined effect of sleep duration and sleep insufficiency.
Results: Results indicated that, when examined alone, sleep duration <5h (versus 7h) was related to BMI (B=2.716, p<0.01), obesity (B=2.080, p<0.000001), diabetes (B=3.162, p<0.000001), hypertension (B=2.703, p<0.000001), hypercholesterolaemia (B=1.922, p<0.00001), heart attack (B=4.704, p<0.000001) and stroke (B=4.558, p<0.000001), and sleep insufficiency (days per week, continuous) was related to BMI (B=0.181, p<0.01), obesity (B=1.061, p<0.000001) and hypercholesterolaemia (B=1.025, p<0.01). All of these relationships remained significant after adjustment for covariates, except for diabetes and sleep duration. Also, after adjustment, a significant relationship between insufficient sleep and hypertension emerged (B=1.039, p<0.001). When evaluated together, after adjustment for covariates, significant relationships remained between sleep duration <5h (versus 7h) and BMI (B=1.266, p<0.05), obesity (B=1.389, p<0.05), hypertension (B=1.555, p<0.01), heart attack (B=2.513, p<0.01) and stroke (B=1.807, p<0.05). It should be noted that relationships between sleep duration >9h (versus 7h) were seen for heart attack (B=1.863, p<0.001) and stroke (B=1.816, p<0.01). In these models, sleep insufficiency was associated with hypercholesterolaemia (B=1.031, p<0.01) and hypertension (B=1.027, p<0.05).
Conclusions: These analyses show that both sleep duration and insufficiency are related to cardiometabolic health outcomes, and that when evaluated together, both variables demonstrate unique effects.
Time-of-Day Dependent Neuronal Injury After Ischemic Stroke: Implication of Circadian Clock Transcriptional Factor Bmal1 and Survival Kinase AKT
Abstract
Occurrence of stroke cases displays a time-of-day variation in human. However, the mechanism linking circadian rhythm to the internal response mechanisms against pathophysiological events after ischemic stroke remained largely unknown. To this end, temporal changes in the susceptibility to ischemia/reperfusion (I/R) injury were investigated in mice in which the ischemic stroke induced at four different Zeitgeber time points with 6-h intervals (ZT0, ZT6, ZT12, and ZT18). Besides infarct volume and brain swelling, neuronal survival, apoptosis, ischemia, and circadian rhythm related proteins were examined using immunohistochemistry, Western blot, planar surface immune assay, and liquid chromatography-mass spectrometry tools. Here, we present evidence that midnight (ZT18; 24:00) I/R injury in mice resulted in significantly improved infarct volume, brain swelling, neurological deficit score, neuronal survival, and decreased apoptotic cell death compared with ischemia induced at other time points, which were associated with increased expressions of circadian proteins Bmal1, PerI, and Clock proteins and survival kinases AKT and Erk-1/2. Moreover, ribosomal protein S6, mTOR, and Bad were also significantly increased, while the levels of PRAS40, negative regulator of AKT and mTOR, and phosphorylated p53 were decreased at this time point compared to ZT0 (06:00). Furthermore, detailed proteomic analysis revealed significantly decreased CSKP, HBB-1/2, and HBA levels, while increased GNAZ, NEGR1, IMPCT, and PDE1B at midnight as compared with early morning. Our results indicate that nighttime I/R injury results in less severe neuronal damage, with increased neuronal survival, increased levels of survival kinases and circadian clock proteins, and also alters the circadian-related proteins.
Time to Target Stroke: Examining the Circadian System in Stroke
Abstract
Stroke is the 5th leading cause of death in the United States and a leading cause of long-term disability. Ischemic strokes account for 87 percent of total stroke cases, yet the only FDA-approved treatments involve disruption of the blood clot to restore blood flow. New treatments aimed at saving or protecting neural tissue have largely failed in clinical trials and so new methodology or targets must be found. The occurrence of strokes significantly increases between 6 AM and 12 PM, implicating the circadian system in the onset of this debilitating brain injury. But it is not known whether or how the circadian system may regulate the response to and recovery from stroke. New strategies to identify treatments for stroke are beginning to look at cell types other than neurons as therapeutic targets, including astrocytes. In this review, we present links between the astrocyte circadian clock, the molecular response to stroke, and the damage caused by ischemia. We highlight aspects of astrocyte circadian function that could dictate new methodologies for stroke treatment, including the potential of chronotherapy.
Shift work and vascular events: systematic review and meta-analysis
Abstract
Objective: To synthesise the association of shift work with major vascular events as reported in the literature.
Data sources: Systematic searches of major bibliographic databases, contact with experts in the field, and review of reference lists of primary articles, review papers, and guidelines.
Study selection: Observational studies that reported risk ratios for vascular morbidity, vascular mortality, or all cause mortality in relation to shift work were included; control groups could be non-shift ("day") workers or the general population.
Data extraction: Study quality was assessed with the Downs and Black scale for observational studies. The three primary outcomes were myocardial infarction, ischaemic stroke, and any coronary event. Heterogeneity was measured with the I(2) statistic and computed random effects models.
Results: 34 studies in 2,011,935 people were identified. Shift work was associated with myocardial infarction (risk ratio 1.23, 95% confidence interval 1.15 to 1.31; I(2)=0) and ischaemic stroke (1.05, 1.01 to 1.09; I(2)=0). Coronary events were also increased (risk ratio 1.24, 1.10 to 1.39), albeit with significant heterogeneity across studies (I(2)=85%). Pooled risk ratios were significant for both unadjusted analyses and analyses adjusted for risk factors. All shift work schedules with the exception of evening shifts were associated with a statistically higher risk of coronary events. Shift work was not associated with increased rates of mortality (whether vascular cause specific or overall). Presence or absence of adjustment for smoking and socioeconomic status was not a source of heterogeneity in the primary studies. 6598 myocardial infarctions, 17,359 coronary events, and 1854 ischaemic strokes occurred. On the basis of the Canadian prevalence of shift work of 32.8%, the population attributable risks related to shift work were 7.0% for myocardial infarction, 7.3% for all coronary events, and 1.6% for ischaemic stroke.
Conclusions: Shift work is associated with vascular events, which may have implications for public policy and occupational medicine.
Predictive factors of subjective sleep quality and insomnia complaint in patients with stroke: implications for clinical practice
Abstract
The complaints regarding sleep problems have not been well identified after a stroke. The aim of this study was to investigate the predictive factors of sleep quality and insomnia complaints in patients with stroke. A total of 70 subjects, 40 patients (57 ± 7 years) and 30 healthy controls (52 ± 6 years) assessed by the Pittsburgh Sleep Quality Index (PSQI) and the Sleep Habits Questionnaire took part in the study. The data were analyzed using the chi-square test, the Student's t-test and logistic regression analysis. On average, the patients showed poor sleep quality (patients: 6.3 ± 3.5; controls: 3.9 ± 2.2; p= 0.002) and insomnia complaint was the most prevalent (patients: 37.5%; controls: 6.7%; p= 0.007). The absence of insomnia complaint (OR= 0.120; 95%CI= 0.017-0.873; p= 0.036) and the decreased latency of sleep (OR= 0.120; 95%CI= 0.017-0.873; p= 0.036) were the protective factors of sleep quality. Female sex (OR= 11.098; 95%CI= 1.167-105.559; p= 0.036) and fragmented sleep (OR= 32.040; 95%CI= 3.236-317.261; p= 0.003) were the risk factors for insomnia complaint. We suggest that complaints of poor sleep quality and insomnia should be given priority assessment during clinical diagnosis of sleep disorders in stroke.
Subjective sleep quality in relation to objective sleep estimates: comparison, gender differences and changes between the acute phase and the six-month follow-up after stroke
Abstract
Aims: To describe sleep experiences after stroke using subjective and objective indicators and identify possible gender differences in sleep in the acute phase and at 6-month follow-up.
Background: Sleep disturbances after stoke are recognized, but poorly described. Gender differences in sleep exist in other populations, but have not been reported after stroke.
Design: A longitudinal cohort study.
Method: Subjective sleep quality was measured with the Pittsburgh Sleep Quality Index and objective sleep was estimated with actigraphy in 100 patients in the acute phase and six months after stroke, from April 2007-March 2009.
Findings: Subjective sleep quality was better and objective wake percentage was lower at follow-up than in the acute phase after stroke. Actigraphy estimated low sleep efficiency and many awakenings at both time points. Subjective and objective measures were correlated at the 6-month follow-up, but not in the acute phase. Women's subjective sleep efficiency and total score on the Pittsburgh Sleep Quality Index were worse than men's in the acute phase, but actigraphy estimated that women slept more than men in the course of a day. Women's subjective sleep quality was better at follow-up than in the acute phase. Men reported worse subjective sleep quality, but better subjective sleep efficiency at follow-up than in the acute phase, and also had lower objective wake percentage at follow-up.
Conclusions: Subjective sleep quality was poor and actigraphy indicated disturbed sleep-wake patterns in the acute phase and at 6-month follow-up. Gender differences existed in subjective and objective sleep in the acute phase, but not at follow-up.
Circadian and homeostatic changes of sleep-wake and quality of life in stroke: implications for neurorehabilitation
Abstract
The present study aimed to assess changes in the circadian and homeostatic control of the sleep-wake pattern in stroke patients and correlations with quality of life. Participants were 22 patients (55 ± 12 years) and 24 healthy subjects (57 ± 11 years). Instruments used were: the Pittsburgh Sleep Quality Index, SF-36 Questionnaire and Actigraphy. Data were analyzed by Mann-Whitney test and Spearman's correlation. Results identified a significant difference in sleep quality and quality of life between patients and healthy subjects, with patients on average exhibiting poor sleep quality (patients: 8.4 ± 3.4; healthy subjects: 6.2 ± 2.5; p = 0.0001) and low quality of life scores (p < 0.001). Correlation analysis detected an association between circadian variables (total activity, start and finish times of activity) and quality of life (p < 0.001). Associations between homeostatic variables (sleep duration, latency and efficiency) and quality of life were also significant (p < 0.001). In conclusion, results in this study showed compromised sleep quality and quality of life in the patients evaluated, associated with circadian and homeostatic alterations. This suggests that complaints regarding poor sleep quality be taken into consideration when planning the rehabilitation of stroke patients.
Sleep quality and adverse outcomes for patients with acute myocardial infarction
Abstract
Aims and objectives: This study aimed to analyse the relationship between the worsening of clinical outcomes (cardiovascular death, recurrent cardiovascular ischaemic events and stroke) and sleep quality, daytime sleepiness and risk for obstructive sleep apnoea syndrome in patients admitted to cardiac care units due to an acute myocardial infarction.
Background: There is evidence that sleep disorders can contribute to the worsening of cardiovascular diseases.
Design: This is a descriptive study with follow-up.
Methods: Data collection was conducted in a large university hospital in Brazil from October 2013 to March 2014. Patients admitted with acute myocardial infarction provided data about sleep quality, daytime sleepiness and risk factors for obstructive sleep apnoea syndrome by answering specific questionnaires. Clinical data were obtained from medical charts. Data were analysed with descriptive statistics and multiple logistic regression models.
Results: The worsening of clinical outcome occurred in 12·4% of patients and was independently associated to poor sleep quality.
Conclusion: Poor sleep quality, excessive daytime sleepiness and high risk for obstructive sleep apnoea syndrome were frequent in hospitalised patients with acute myocardial infarction and affect negatively the process of recovery.
Relevance to clinical practice: It is important to evaluate sleep quality and sleep disorders, aiming at preventing and reducing unfavourable outcomes of cardiovascular disease, particularly for acute myocardial infarction patients.
Relationship between Sleep Duration and Risk Factors for Stroke
Abstract
Stroke is a leading cause of death and disability worldwide. While various risk factors have been identified, sleep has only been considered a risk factor more recently. Various epidemiologic studies have associated stroke with sleep such as sleep duration, and laboratory and clinical studies have proposed various underlying mechanisms. The pathophysiology is multifactorial, especially considering sleep affects many common risk factors for stroke. This review aims to provide an outline of the effect of sleep duration on common stroke risk factors. Appropriate sleep duration, especially in patients who have stroke risk factors, and increasing awareness and screening for sleep quality may contribute to primary prevention of stroke.
The influence of sleep quality and circadian preferences on upper extremity rehabilitation in stroke patients after constraint-induced movement therapy
Abstract
Our aim was to explore the influence of sleep and circadian preference on upper extremity (UE) rehabilitation in stroke patients after constraint-induced movement therapy (CIMT) in a cross-sectional retrospective observational study. Forty-three patients were selected to complete questionnaires on circadian preference, sleep quality, excessive daytime sleepiness, and risk of obstructive sleep apnea. They had undergone a 10-day standard CIMT program without medical complications and with normal to minimal cognitive dysfunction. All pre- and postrehabilitation scores (patient perception of the quantity and quality of use of the affected UE and self-quantification of motor ability) were analyzed retrospectively. All patients had improved perception of the quantity and quality of use of the affected UE and self-quantified motor ability. Patients with an evening-type chronotype demonstrated less improvement than those with morning and intermediate types. In addition, patients with poor sleep quality showed less improvement in functional ability than those with good sleep quality. Circadian preferences and sleep quality impacted the improvements in motor performance of patients with stroke after CIMT rehabilitation. This is the first study to suggest that rehabilitation sessions must respect the circadian preferences of patients and that sleep quality can affect outcomes. Future studies should investigate the relationship and mechanisms between circadian preference and poor sleep quality and rehabilitation outcomes on a larger scale.
Sleep Duration, Sedentary Behavior, Physical Activity, and Quality of Life after Inpatient Stroke Rehabilitation
Abstract
Objective: The aim of this study was to describe accelerometer-derived sleep duration, sedentary behavior, physical activity, and quality of life and their association with demographic and clinical factors within the first month after inpatient stroke rehabilitation.
Materials and methods: Thirty people with stroke (mean ± standard deviation, age: 63.8 ± 12.3 years, time since stroke: 3.6 ± 1.1 months) wore an activPAL3 Micro accelerometer (PAL Technologies, Glasgow, Scotland) continuously for 7 days to measure whole-day activity behavior. The Stroke Impact Scale and the Functional Independence Measure were used to assess quality of life and function, respectively.
Results: Sleep duration ranged from 6.6 to 11.6 hours/day. Fifteen participants engaged in long sleep greater than 9 hours/day. Participants spent 74.8% of waking hours in sedentary behavior, 17.9% standing, and 7.3% stepping. Of stepping time, only a median of 1.1 (interquartile range: .3-5.8) minutes were spent walking at a moderate-to-vigorous intensity (≥100 steps/minute). The time spent sedentary, the stepping time, and the number of steps differed significantly by the hemiparetic side (P < .05), but not by sex or the type of stroke. There were moderate to strong correlations between the stepping time and the number of steps with gait speed (Spearman r = .49 and .61 respectively, P < .01). Correlations between accelerometer-derived variables and age, time since stroke, and cognition were not significant.
Conclusions: People with stroke sleep for longer than the normal duration, spend about three quarters of their waking hours in sedentary behaviors, and engage in minimal walking following stroke rehabilitation. Our findings provide a rationale for the development of behavior change strategies after stroke.
Poor Sleep Quality I Related to Impaired Functional Status Following Stroke
Abstract
Introduction: Sleep disorders are more prevalent in patients with previous stroke compared to healthy individuals. The main objective of the present study was to investigate the impact of sleep quality on the functional status of patients with a history of stroke, upon admission to inpatient rehabilitation.
Methods: Fifty patients (mean age: 69 ± 11 years) with previous stroke were consecutively included in this single center cross-sectional observational study upon admission to inpatient rehabilitation. Pittsburgh Sleep Questionnaire Index (PSQI) was calculated for all patients and patients were divided into 2 groups according to PSQI scores (PSQI ≤ 5 as good sleepers and PSQI > 5 as poor sleepers). A specialist evaluated the level of muscle spasticity and disability, walking capability, and overall performance of daily activity of all enrolled patients using the functional ambulation scale (FAS) score, modified Brunnstrom Classification, Modified Ashworth scale, and Beck Depression Inventory.
Results: The FAS score (3.4 ± 1.3 versus 1.8 ± 1.7, P = .004) and Brunnstrom scores of upper limb (3.8 ± 1.1 versus 2.5 ± 1.6, P = .005), lower limb (4.3 ± 1.4 versus 3.1 ± 1.7, P = .013) and hand (3.6 ± 1.5 versus 2.3 ± 1.6, P = .006) were significantly higher in good sleepers than poor sleepers. Linear regression analysis revealed that PSQI score (coefficient β = -.360, 95% CI: -.212-.032, P = .009) and age (coefficient β = -.291, 95% CI: .100-.245, P = .032) were independently associated with FAS score.
Conclusion: Results of the present study indicate that presence of poor sleep quality is associated with poor functional status which might further impair the outcomes of the rehabilitation and accordingly the health-related quality of life in patients admitted for stroke rehabilitation.
Arthritis
Circadian rhythms and rheumatoid arthritis
Abstract
Circadian rhythms (Nobel prize for Medicine 2017) regulate, under action of biological clocks located both at the level of central nervous system and inside peripheral cells, several daily activities, embracing sleep, feeding times, energy metabolism, endocrine and immune functions with related pathological conditions, including rheumatoid arthritis (RA). In RA the circadian rhythms impact on cellular functions, involving night synthesis and release of pro-inflammatory cytokines and chemokines, cell migration to inflamed tissues, phagocytosis, proliferative cell response and all are peaking at late night. In chronic inflammatory conditions such as RA, the amplitude of the circadian rhythm of the anti-inflammatory endogenous cortisol availability is not increased as expected and requested, which indicate a reduced night cortisol secretion under the adrenal chronic stress induced by the disease. Therefore, the prevention/treatment of the immune cell night hyperactivity, with related flare of cytokine synthesis and morning RA clinical symptoms, has been shown more effective when the availability of the exogenous glucocorticoids is obtained in the middle of the night (night release). The impressive positive results observed in RA patients treated with modified-night release prednisone with a low-dose chronotherapy, seem applicable even for other agents such as conventional NSAIDs and DMARDs, including the positive experimental and clinical results obtained by the night time daily administration of methotrexate. Interestingly, a very recent study showed that methotrexate upregulates important cell circadian genes, resulting in induction of apoptosis in synovial fibroblasts. The link between the circadian rhythms of the disease and the chronotherapy of RA is promising.
Management of Fatigue in Rheumatoid Arthritis
Abstract
Fatigue in rheumatoid arthritis is highly prevalent. It is correlated only weakly with disease activity but more so with pain, mood, personality features, poor sleep, obesity and comorbidities. Fatigue can be measured by many standardised questionnaires and more easily with a Visual Analogue Scale or numeric rating scale. Most patients with RA have some fatigue, and at least one in six have severe fatigue. Chronic pain and depressed mood are also common in RA patients with significant fatigue. It affects function and quality of life and is worse on average in women. Evidence-based treatment for fatigue includes treatment of underlying disease activity (with on average modest improvement of fatigue), exercise programmes and supervised self-management programmes with cognitive-behavioural therapy, mindfulness and reinforcement (such as reminders). The specific programmes for exercise and behavioural interventions are not standardised. Some medications cause fatigue such as methotrexate. More research is needed to understand fatigue and how to treat this common complex symptom in RA that can be the worst symptom for some patients.
Sleep disorders and vascular responsiveness in patients with rheumatoid arthritis
Abstract
Background: Rheumatoid arthritis (RA) is the most common systemic autoimmune disease characterized by chronic systemic inflammation. Half of the deaths of patients with RA are due to cardiovascular diseases (CVD), considered to be 1.5 to -2.0-fold that in the general population. Patients with RA also experience poor sleep, which by itself is associated with endothelial dysfunction, CVD events and sudden death. Our aim was to study the mechanistic pathways and the correlations between sleep efficiency and vascular reactivity of patients with RA.
Methods and results: A prospective study that evaluated quality of sleep using ACTi Graphs, vascular inflammation and endothelial function of 18 patients with RA. Inflammation was studied by levels of E-selectin, intercellular adhesion molecule 1 (ICAM-1) and NO in serum. Endothelial function was studied using the brachial artery plethysmography method. Eighteen RA patients (aged 57.56 ± 13.55 years; 16 women) with a long-standing active RA: Eight patients had impaired sleep efficiency and 10 had a good sleep efficiency. Those who had an impaired sleep had larger baseline diameters of the brachial artery (0.39 ± 0.08 cm vs. 0.32 ± 0.04 cm; P = 0.02). Negative correlations were found between baseline brachial artery diameter and sleep efficiency (P = 0.01), and with NO level (P = 0.04). Stepwise regression found that brachial artery diameter at baseline and NO level could predict sleep efficiency (r2 = 0.543, P = 0.01).
Conclusion: Vascular reactivity could predict quality of sleep in patients with RA. Quality of sleep may serve as an independent CVD risk factor in patients with RA.
Dose-response Relationship between Sleep and Rheumatoid Arthritis
Abstract
Objectives: In this study, we explored the association between sleep quality, duration and prevalence of rheumatoid arthritis (RA) among low-income adults in rural areas of China.
Methods: Face-to-face investigation were conducted in 2017, and completed questionnaires were obtained from 16,648 individuals. Sleep quality and duration were evaluated using the standard Pittsburgh Sleep Quality Index. RA was based on self-reported physician diagnosis. Logistic regression analysis and restricted cubic spline models were performed.
Results: Sleep duration shorter than 7 hours was associated with increased odds of RA, with an odds ratio (OR) of 1.49 for 6-<7 hours and 1.70 for <6 hours. Poor sleep quality was associated with RA, with an OR of 1.68. The combination category of poor sleep quality and any group of sleep duration was associated with a significantly increased risk of developing RA. Combined groups of good sleep quality with short sleep duration (<7 hours) were also found to be related to prevalence of RA. There was a non-linear relationship between sleep quality, duration and the odds of RA.
Conclusions: Poor sleep quality and short sleep duration may be trigger or risk factors for RA.
Similar articles
Yoga for the management of pain and sleep in rheumatoid arthritis: a pilot randomized controlled trial
Abstract
Objective: The aim of the present study was to determine the feasibility of a relaxation-based yoga intervention for rheumatoid arthritis, designed and reported in accordance with Delphi recommendations for yoga interventions for musculoskeletal conditions.
Methods: Participants were recruited from a hospital database, and randomized to either eight weekly 75-min yoga classes or a usual care control. Feasibility was determined by recruitment rates, retention, protocol adherence, participant satisfaction and adverse events. Secondary physical and psychosocial outcomes were assessed using self-reported questionnaires at baseline (week 0), week 9 (primary time point) and week 12 (follow-up).
Results: Over a 3-month period, 26 participants with mild pain, mild to moderate functional disability and moderate disease activity were recruited into the study (25% recruitment rate). Retention rates were 100% for yoga participants and 92% for usual care participants at both weeks 9 and 12. Protocol adherence and participant satisfaction were high. Yoga participants attended a median of seven classes; additionally, seven of the yoga participants (54%) reported continuing yoga at home during the follow-up period. No serious adverse events were related to the study. Secondary outcomes showed no group effects of yoga compared with usual care.
Conclusions: A relaxation-based yoga programme was found to be feasible and safe for participants with rheumatoid arthritis-related pain and functional disability. Adverse events were minor, and not unexpected from an intervention including physical components. This pilot provides a framework for larger intervention studies, and supports further exploration of yoga as a complex intervention to assist with the management of rheumatoid arthritis.
Fatigue, Sleep, and Autoimmune and Related Disorders
Abstract
Profound and debilitating fatigue is the most common complaint reported among individuals with autoimmune disease, such as systemic lupus erythematosus, multiple sclerosis, type 1 diabetes, celiac disease, chronic fatigue syndrome, and rheumatoid arthritis. Fatigue is multi-faceted and broadly defined, which makes understanding the cause of its manifestations especially difficult in conditions with diverse pathology including autoimmune diseases. In general, fatigue is defined by debilitating periods of exhaustion that interfere with normal activities. The severity and duration of fatigue episodes vary, but fatigue can cause difficulty for even simple tasks like climbing stairs or crossing the room. The exact mechanisms of fatigue are not well-understood, perhaps due to its broad definition. Nevertheless, physiological processes known to play a role in fatigue include oxygen/nutrient supply, metabolism, mood, motivation, and sleepiness-all which are affected by inflammation. Additionally, an important contributing element to fatigue is the central nervous system-a region impacted either directly or indirectly in numerous autoimmune and related disorders. This review describes how inflammation and the central nervous system contribute to fatigue and suggests potential mechanisms involved in fatigue that are likely exhibited in autoimmune and related diseases.
Arthritis, Sleep Health, and Systemic Inflammation in Older Men
Abstract
Objective: To examine the associations of prevalent arthritis with systemic inflammation in older men and to test whether sleep health mediates the associations.
Methods: Cross-sectional data came from 2,562 community-dwelling older men (all were age 65 years or older; mean age 76 years) in the Osteoporotic Fractures in Men Study who participated in a sleep ancillary study in 2003-2005. Participants were classified as having osteoarthritis (OA) (24%) or rheumatoid arthritis (RA) (0.7%) based on self-reported diagnoses and medication use. We constructed a composite score of multidimensional sleep health (i.e., perceived sleep quality, sleepiness, frequency of daytime napping, wake after sleep onset, and sleep duration) measured by both self-report and actigraphy. We also created binary indicators of elevated inflammation using C-reactive protein (CRP) (>3 mg/liter) and interleukin-6 (IL-6) (>1.08 pg/ml) levels. Analyses controlled for age, diagnosed sleep disorders, body mass index, smoking status, relevant medication use, and comorbidities.
Results: Older men with OA did not have higher risk of elevated CRP or IL-6 levels. However, indirect associations of OA through sleep health were found. OA was associated with poorer sleep health, which was further associated with 16% higher odds of elevated CRP (P < 0.001) and 12% higher odds of elevated IL-6 (P < 0.01) levels after controlling for OA. Older men with RA had higher odds of elevated CRP and IL-6 levels, but the associations were not mediated by sleep health.
Conclusion: Findings suggest that promoting sleep health may help reduce the risk of systemic inflammation in older men with OA.
Causes and consequences of fatigue in rheumatoid arthritis
Abstract
Purpose of review: To review current information on the causes, treatments, and consequences of fatigue in rheumatoid arthritis.
Recent findings: Disease activity (inflammation, pain, joint symptoms) is associated with greater fatigue. However, disease activity per se accounts for only a small portion of fatigue, and rheumatoid arthritis medications that reduce disease activity have small effects on fatigue. Instead, factors outside the direct effects of rheumatoid arthritis, such as obesity, physical inactivity, sleep disturbance, and depression, explain the majority of variation in fatigue. Some of these factors may be indirect effects of disease (e.g. pain can lead to sleep disturbance). Rheumatoid arthritis has significant effects on the quality of life of individuals with rheumatoid arthritis. The most effective approaches to reducing rheumatoid arthritis fatigue appear to be behavioral, such as increasing physical activity, or cognitive, such as cognitive behavioral interventions.
Summary: Fatigue in rheumatoid arthritis appears to be largely because of factors outside the direct effects of the disease, such as behavioral and psychological factors. In spite of the tremendous impact of fatigue on patient health and quality of life, effective treatments remain elusive, but existing data show that behavioral and cognitive approaches may be most effective.
Circadian Disruption and Vascular Variability Disorders (VVD): Mechanisms Linking Aging, Disease State and Arctic Shift-Work: Applications for Chronotherapy
Abstract A fast growing body of evidence indicates that the circadian system is important for health. In turn, desynchrony has been associated with the development of numerous agerelated diseases and the aging process. Alterations of the circadian variation occurring within the physiological range provide warning signs that, if acted upon, lead to truly primary prevention not across the board but targeted to the individual person. This is the case for instance for Vascular Variability Disorders. Particular attention is given to blood pressure and heart rate recorded in the elderly, in shiftworkers in the Arctic, and to a personalized chronotherapeutic approach.
Relationship between shift work and the onset of rheumatoid arthritis
Abstract
Background Environmental factors play a prominent role in rheumatoid arthritis (RA) aetiology. Shift work has previously been associated with increased RA risk in females. The aim of this study was to investigate the potential association, including a dose–response association, between permanent night shift work, rotating shift work and day-oriented shift work and risk of developing anticitrullinated peptide antibodies (ACPA)-positive and ACPA-negative RA.
Methods The present report is based on a population-based, case–control study with incident cases of RA (1951 cases and 2225 controls matched by age, gender and residential area). Using logistic regression, occurrence of RA among subjects who have been exposed to different kinds of shift work was compared with that among those who have never been exposed by calculating the OR with a 95% CI.
Results Rotating shift work and day-oriented shift work increased the risk of developing ACPA-positive RA (OR 1.3, 95% CI 1.0 to 1.7 and OR 1.3, 95% CI 1.0 to 1.6), but not ACPA-negative RA. Permanent night shift work appeared to be a protective factor both against ACPA-positive RA (OR 0.7, 95% CI 0.6 to 0.9) and ACPA-negative RA (OR 0.8, 95% CI 0.6 to 1.0). For both subsets of RA, significant trends showed a lower risk of developing RA with increasing duration of permanent night shift work (p value for trend 0.002 vs 0.04).
Conclusions Sleep restriction as a consequence of shift work is associated with several biological effects among which changes in melatonin production may be involved. The present epidemiological findings of a complex relationship between sleep patterns and different forms of RA may be of importance for increasing the understanding of the pathophysiology of RA.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial.
Is shift work a risk factor for rheumatoid arthritis? The Finnish Public Sector study
Rheumatoid arthritis (RA) is a chronic inflammatory disease with both environmental and genetic determinants.1 Shift work, defined here as working outside regular day shifts, has been found to induce changes in the biomarkers of systemic inflammation such as leucocyte count2 3 and T cell responses.4 5 We examined whether shift work also predicts development of RA.
Sleep Loss Exacerbates Fatigue, Depression, and Pain in Rheumatoid Arthritis
Abstract
Study Objectives:
Disturbances of sleep are hypothesized to contribute to pain. However, experimental data are limited to healthy pain-free individuals. This study evaluated the effect of sleep loss during part of the night on daytime mood symptoms and pain perceptions in patients with rheumatoid arthritis in comparison with control subjects.
Design:
A between-groups laboratory study with assessment of mood symptoms and pain perception before and after partial night sleep deprivation (PSD; awake 23:00 hr to 03:00 hr).
Setting:
General clinical research center.
Participants:
Patients with rheumatoid arthritis (n = 27) and volunteer comparison control subjects (n = 27).
Measurements:
Subjective reports of sleep, mood symptoms and pain, polysomnographic assessment of sleep continuity, and subjective and objective assessment of rheumatoid arthritis-specific joint pain.
Results:
PSD induced differential increases in self-reported fatigue (P < 0.09), depression (P < 0.04), anxiety (P < 0.04), and pain (P < 0.01) in patients with rheumatoid arthritis compared with responses in control subjects, in whom differential increases of self-reported pain were independent of changes in mood symptoms, subjective sleep quality, and objective measures of sleep fragmentation. In the patients with rheumatoid arthritis, PSD also induced increases in disease-specific activity as indexed by self-reported pain severity (P < 0.01) and number of painful joints (P < 0.02) as well as clinician-rated joint counts (P < 0.03).
Conclusion:
This study provides the first evidence of an exaggerated increase in symptoms of mood and pain in patients with rheumatoid arthritis after sleep loss, along with an activation of rheumatoid arthritis-related joint pain. Given the reciprocal relationship between sleep disturbances and pain, clinical management of pain in patients with rheumatoid arthritis should include an increased focus on the prevention and treatment of sleep disturbance in this clinical population.
Relationship between Sleep Disorders, Pain and Quality of Life in Patients with Rheumatoid Arthritis
Abstract
Introduction: Rheumatoid arthritis as one of the most common autoimmune diseases is known to be one of the leading causes of disability. Sleep disorders have direct influence on patient’s life. According to studies, sleep problems are known to have negative impact on well-being and functioning, but the exact nature of relationship between sleep disorders and Rheumatoid arthritis is not completely understood. This study aimed to investigate the relationship between sleep disorders, pain and quality of life in patients with rheumatoid arthritis patients.
Methods: In a descriptive -correlative study, 210 patients with rheumatoid arthritis referred to Tabriz medical university clinics selected by convenience sampling and were assessed by Sleep Disorders Questionnaire (SDQ), Epworth Sleepiness Scale (ESS), SF-36 Quality of Life Questionnaire and Visual Analog Scale (VAS). Data were analyzed using SPSS-13 by descriptive statistics such as frequency, mean (SD) and inferential statistics including Spearman correlation analysis, linear regression, χ2,t-test and ANOVA.
Results: The mean age of participants was 48.41(12.92) years in which most of them (74%) were female. The mean (SD) quality of life was 40.51(22.94), sleepiness 13.14 (5.6) and pain 6.09 (2.14). There was significant negative relationship between some sleep disorders such as (naps, apnea, asphyxia,…) and pain with quality of life but pain severity had more effect on QOL compared to sleep problems. Furthermore, participants had low quality of life with more restriction in physical (mean=34.71) and general health (mean=34.42).
Conclusion: Sleep problems and pain were associated with poor quality of life in Rheumatoid Arthritis patients.
Improved Sleep May Reduce Arthritis Pain
Abstract
Studies indicate that pain interferes with sleep and, in turn, sleep disturbances increase pain. Statistics show that up to 60% of those with arthritis experience pain during the night. But despite these findings, sleep is not generally addressed as a major treatment concern among this population. This article reviews the relationship between pain and sleep; sleep issues as they relate to 3 common types of arthritis—osteoarthritis, rheumatoid arthritis, and fibromyalgia; and holistic approaches that may be used by the patient in the self-management of pain and sleep.
Delta sleep instability in children with chronic arthritis
Abstract

The objective of the present study was to evaluate the expression of a cyclic alternating pattern (CAP) in slow wave sleep (SWS) in children with the well-defined chronic syndrome juvenile idiopathic arthritis (JIA). Twelve patients (9-17 years of age), 7 girls, with JIA were compared to matched controls by age, pubertal stage and gender. After one night of habituation in the sleep laboratory, sleep measurements were obtained by standard polysomnography with conventional sleep scoring and additional CAP analyses. The sleep parameters of the JIA and control groups were similar for sleep efficiency (91.1 ± 6.7 vs 95.8 ± 4.0), sleep stage in minutes: stage 1 (16.8 ± 8.5 vs 17.8 ± 4.0), stage 2 (251.9 ± 41 vs 262.8 ± 38.1), stage 3 (17.0 ± 6.0 vs 15.1 ± 5.7), stage 4 (61.0 ± 21.7 vs 77.1 ± 20.4), and rapid eye movement sleep (82.0 ± 27.6 vs 99.0 ± 23.9), respectively. JIA patients presented nocturnal disrupted sleep, with an increase in short awakenings, but CAP analyses showed that sleep disruption was present even during SWS, showing an increase in the overall CAP rate (P < 0.01). Overall CAP rate during non-rapid eye movement sleep was significantly higher in pediatric patients who were in chronic pain. This is the first study of CAP in pediatric patients with chronic arthritis showing that CAP analyses can be a powerful tool for the investigation of disturbance of SWS in children, based on sleep EEG visual analysis.
Sleep problems in fibromyalgia and rheumatoid arthritis compared with the general population
Abstract Objective Our aim was to evaluate how frequently problems of quality and quantity of sleep and depression occur in patients with fibromyalgia (FM), and compare these findings with those occurring in patients with rheumatoid arthritis (RA) and in the general population. Materials and methods The patients were recruited from rehabilitation courses in the Rheumatism Foundation Hospital, Finland. There were 37 patients with FM and 31 patients with RA participating in the study. For comparison, we used the results from a general population study of 1284 adult subjects. The data had been collected earlier in a longitudinal cohort study for the Finnish Social Insurance Institution. Results The patients with FM and RA slept fewer hours a day than the population sample. The FM patients reported more insomnia, less contentment with sleep and more lack of deep and restful sleep in comparison to the RA patients and the participants of the population study. The FM patients also reported significantly more depression and pain than the RA patients (p<0.01). It was still shown in a logistic regression analysis that insomnia was almost five times more frequent in FM patients than in RA patients, even when depression and pain were adjusted. Conclusions The FM patients reported more insomnia-related symptoms than either RA patients or the population sample. The higher prevalence of insomnia-related symptoms among FM patients was not explained by depression or pain. Both patient groups reported somewhat shorter nocturnal sleep than the general population.
Reciprocal Relationship between Sleep Macrostructure and Evening- and Morning Cellular Inflammation in Rheumatoid Arthritis
Abstract
Objective
This study examines the reciprocal associations between sleep macrostructure and levels of cellular inflammation in rheumatoid arthritis (RA) patients and controls.
Methods
RA patients (n=24) and matched controls (n=48) underwent all-night polysomnography (PSG), along with assessment of spontaneous- and Toll-like receptor (TLR)-4 stimulated monocytic production of tumor necrosis factor-α (TNF) and interleukin (IL)-6 at 23:00 and 8:00.
Results
As compared to controls, RA patients showed lower levels of sleep efficiency (mean ± SD, 88.1 ±6.1 vs. 83.8 ± 7.0), a higher percentage Stage 3 sleep (9.3 ± 6.4 vs. 13.1 ± 6.9), and higher levels of percentage of monocytes either spontaneously expressing TNF at 23:00 (log transformed, 1.07 ± 0.28 vs. 1.22 ± 0.17), and higher TLR4 stimulated production of IL6 at 8:00 (log transformed, 3.45 ± 0.80 vs. 3.83 ± 0.39). Higher levels of stimulated production of TNF at 23:00 were associated with higher sleep efficiency (.74). In turn, sleep efficiency had a countervailing relationship on TNF production at 8:00 (. 64). Higher levels of spontaneous and stimulated production of IL6 at 23:00 were associated with more Stage 3 (.39), 4 (.43), and slow wave sleep (.49), with evidence that Stage 4 had a countervailing relationship on IL6 production at 8:00 (.60).
Conclusion
RA patients show evidence of sleep fragmentation, greater sleep depth, and higher levels of cellular inflammation. Sleep maintenance and sleep depth show countervailing relationships with evening- and morning levels of monocytic production of TNF and IL-6, respectively, which support the hypothesis of a feedback loop between sleep maintenance, slow wave sleep and cellular inflammation that is cytokine specific.
Nocturnal sleep, daytime sleepiness and fatigue in fibromyalgia patients compared to rheumatoid arthritis patients and healthy controls: A preliminary study
Abstract
Objective
Fibromyalgia (FM) and rheumatoid arthritis (RA) are pain disorders, both of which are associated with complaints of sleep disturbance, non-refreshing sleep, and daytime sleepiness and fatigue. Given the putative differential central versus peripheral nervous system involvement in these disorders, subjective and objective measures of nocturnal sleep, daytime sleepiness, fatigue and pain were compared between patient groups and to healthy controls (HC).
Methods
Fifty women (18 with FM, 16 with RA, and 16 HC) completed an 8 h nocturnal polysomnogram (NPSG), Multiple Sleep Latency Test (MSLT) the following day, and self-reports of sleepiness, fatigue, and pain.
Results
FM and RA patients were similar to each other and had less total sleep time than HC, primarily due to more wake after sleep onset. In an analysis of sleep and wake bouts, both patient groups had longer duration of wake bouts than HC. Nocturnal sleep was judged to be non-restorative for both patient groups. Although reporting the greatest subjective sleepiness and fatigue, FM patients had less objective (MSLT) daytime sleepiness than HC, whereas RA patients were intermediate in objective sleepiness. Unlike the RA and HC, FM patients also showed no association between their subjective and objective sleepiness.
Conclusions
Women with FM have similar nocturnal sleep disturbance as those with RA, but FM patients report greater self-rated daytime sleepiness and fatigue than RA and HC, which did not correspond to the relatively low level of objectively determined daytime sleepiness of FM patients. These findings suggest a generalized hyperarousal state in FM.
Effect of acute gouty arthritis on sleep patterns: A preclinical study
Abstract
Background
It has been demonstrated that the interrelation between pain and sleep produces changes in sleep patterns and
pain perception
. Although some evidences suggest that sleep and pain may interact in a complex way, polysomnographic studies in animals with acute nociception are limited in number.
Aims
This study was carried out in order to evaluate the effect of intra-articular knee injection of
uric acid
on sleep-wake patterns.
Methods
Surgical
electrode implantation
was performed in seven anesthetized
Wistar rats
to carry out 10 h polysomnographic recordings. Acute nociception was induced by the
intra-articular administration
of 30% uric acid crystals into the knee joint of the right
hind limb
. Two recordings before and after intra-articular drug administration were obtained. Sleep-wake parameters were classified as (i) wakefulness (W), (ii)
slow wave sleep
(SWS), and (iii)
rapid eye movement
(REM) sleep. Frequency and duration from each parameter were evaluated under the two above-mentioned conditions.
Results
Intra-articular administration of uric acid induced: (i) an increased duration of wakefulness (p = 0.014), (ii) a decrement in the duration (p = 0.001) and number of events (p = 0.027) in REM sleep, and (iii) a decrement in the total sleep time (p = 0.001). SWS did not present statistical differences between groups.
Conclusions
These data suggest that a nociceptive stimulus, induced by the intra-articular administration of uric acid, alters the sleep-wake equilibrium with REM sleep being particularly altered. However, further research concerning pain–sleep interaction is needed.
Nightmare disorder and REM sleep behavior disorder in inflammatory arthritis: Possibility beyond neurodegeneration
Abstract
Objectives: To investigate the prevalence of REM sleep behavior disorder (RBD) in patients with inflammatory arthritis (IA) to ascertain if RBD could be an internal red flag signaling a fluctuating state of inflammation based on the theory of "protoconsciousness".
Materials & methods: One hundred and three patients with a confirmed diagnosis of IA were consecutively recruited. The patients underwent general (IA activity, functional status, laboratory tests) and neurological evaluations. A neurologist investigated RBD and REM sleep parasomnias in a semi-structured interview. Sleep quality was assessed with the Pittsburgh Sleep Quality Index, while the risk of obstructive sleep apnea syndrome (OSAS) was evaluated with the Berlin questionnaire. Beck Depression Inventory II and State-Trait Anxiety Inventory investigated depression and anxiety.
Results: Patients had a mean age of 53.7 ± 14.6 years, 65% were women; 57.3% were in a clinically active phase of IA. Two women fulfilled ICSD-3 criteria for RBD appearing 11 years after and 20 years before IA onset respectively. 31 patients scored positive for nightmare disorder (ND), 8 for recurrent isolated sleep paralysis. 65 (63.1%) patients reported poor sleep quality and 25 (24.3%) resulted at high risk for OSAS. 32 (31.0%) patients scored positively for depression or anxiety.
Conclusions: The prevalence of RBD in patients with IA did not differ from that in the general population, whereas ND presented a 2-fold increased prevalence. Whether RBD can be considered a red flag signaling an internal danger remains an open question, while ND may be a new player in this intriguing relation.
Sleep disorders in patients with psoriatic arthritis and psoriasis
Abstract
Objectives: To assess and measure occurrence of sleep disorders in patients with psoriatic arthritis (PsA) and psoriasis (Ps).
Material and methods: The study included 62 patients with psoriatic arthritis and 52 patients with psoriasis. The measurement of sleep quality was conducted using the Pittsburgh Sleep Quality Index (PSQI), the evaluation of fatigue by the fatigue subscale of the FACIT-F questionnaire and the patient's quality of life by the Health Assessment Questionnaire (HAQ). The psoriasis severity was determined using the Psoriasis Area Severity Index (PASI) and the activity of arthritis by the disease activity score of 28 joints (DAS 28). The Visual Analogue Scale (VAS) was used to assess the severity of pain.
Results: Poor sleep quality was found in 67.7% of PsA patients, 57.7% in Ps patients and 14.6% within the control group. Sleeping disorders in patients with PsA and Ps were related to worse quality of life and intense fatigue. Methotrexate treatment was not related to sleeping disorders, but an improvement in sleep quality was observed in both PsA and Ps patients who were treated with anti TNF-α antibodies (p < 0.001 and p = 0.032 respectively). Following the use of the linear regression model, the following factors worsen the sleep quality in PsA: pain (R2 = 0.462, p < 0.001), tender joint count (R2 = 0.434, p < 0.001), C-reactive protein (CRP) concentration (R2 = 0.391, p < 0.001), patient's age (R2 = 0.284, p = 0.003) and duration of psoriasis (R2 = 0.166, p = 0.006). In Ps patients the factors were: severity of skin lesions (R2 = 0.329, p < 0.001), duration of psoriasis (R2 = 0.290, p = 0.004) and patient's age (R2 = 0.282, p = 0.019).
Conclusions: Poor sleep quality in patients with PsA or Ps is a common symptom. Sleep disorders are more frequent in patients with PsA than in those with psoriasis.
Fatigue in Rheumatoid Arthritis Patients: Association With Sleep Quality, Mood Status, and Disease Activity
Abstract
Objectives: Rheumatoid arthritis (RA) is a chronic inflammatory disease, characterized by polyarthritis and systemic manifestations. RA-fatigue is a significant problem and adds on disease burden. Sleep disturbance, depression, and disease activity are suggested contributing factors to RA-fatigue; however, their combined role did not examine before among Egyptian RA patients. The objective of the study was to investigate the presence of fatigue, sleep and mood disturbances in RA patients. Also, to evaluate the possible association of poor sleep, depression, and disease activity with RA-fatigue.
Methods: This cross-sectional study included 115 RA patients diagnosed according to the 2010 ACR-EULAR criteria and 46 age and sex matched controls. Fatigue using the Multidimensional Assessment of Fatigue-Global Fatigue Index, sleep using the Pittsburgh Sleep Quality Index and mood status using Beck Depression Inventory were assessed for all participants. RA disease activity was evaluated using disease activity score-28 joints.
Results: RA patients had higher mean fatigue, sleep disturbance, and depression scores (27.2±8.9, 6.4±3.6, and 12.8±7.3; respectively) than controls (22.7±7, 4.8±3, 7.8±5.9; respectively) (P<.05). Poor sleep, depression and higher disease activity were significantly correlated with fatigue (r=0.4, r=0.65, r=0.55; respectively) (P<.001). The three variables may explain up to 49.1% of the variation in fatigue on multiple regression analysis.
Conclusion: Fatigue, poor sleep, and depression are more common in Egyptian patients with RA. A remarkably higher fatigue was associated with poor sleep, depression, and high disease activity, thus monitoring these silent comorbidities in clinical practice is required.
Sleep impairment: an obstacle to achieve optimal quality of life in rheumatoid arthritis
Abstract
Sleep impairment is a common clinical condition in patients with rheumatoid arthritis. There are several confounding factors for poor sleep quality including inflammation, pain, comorbidities, and medications. Consequences of impaired sleep vary within a wide spectrum, as well. These include exacerbated inflammation and inflammation-related symptoms, mental and physical fatigue, mood disorders, daytime sleepiness, and poor quality of life. Sleep impairment in rheumatoid arthritis and its association with disease-related variables including health-related quality of life have been studied several times in the literature. Therefore, it would be of value to review the existing data on the crosstalk between sleep and rheumatoid arthritis. In the present article, the mechanism, confounders, and consequences of this association will be reviewed in detail. The evaluation of sleep impairment in rheumatoid arthritis along with the potential management strategies will be discussed.
Rheumatoid arthritis and sleep quality
Abstract
Background: Sleep disturbances are common in rheumatoid arthritis (RA) patients and contribute to loss of life quality.
Objective: To study associations of sleep quality with pain, depression and disease activity in RA.
Methods: This is a transversal observational study of 112 RA patients submitted to measurement of DAS-28, Epworth scale for daily sleepiness, index of sleep quality by Pittsburg index, risk of sleep apnea by the Berlin questionnaire and degree of depression by the CES-D (Center for Epidemiologic Studies Depression scale) questionnaire. We also collected epidemiological, clinical, serological and treatment data.
Results: Only 18.5% of RA patients had sleep of good quality. In univariate analysis a bad sleep measured by Pittsburg index was associated with daily doses of prednisone (p=0.03), DAS-28 (p=0.01), CES-D (p=0.0005) and showed a tendency to be associated with Berlin sleep apnea questionnaire (p=0.06). In multivariate analysis only depression (p=0.008) and Berlin sleep apnea questionnaire (p=0.004) kept this association.
Conclusions: Most of RA patients do not have a good sleep quality. Depression and risk of sleep apnea are independently associated with sleep impairment.
Fatigue and sleep quality in rheumatoid arthritis patients during hospital admission
Abstract
Objectives: Rheumatoid arthritis (RA) is a systemic disease of connective tissue characterised by chronic course with periods of exacerbation and remission. Even in the early stages of the disease patients report the occurrence of fatigue and sleep disorders. Reduced sleep quality and chronic fatigue are common among patients with rheumatoid arthritis. The aim of the research was to evaluate the severity of fatigue and sleep quality assessment among patients hospitalised with rheumatoid arthritis and to determine the relation between the level of symptoms of fatigue and sleep quality and variables such as: age, gender, disease duration, marital status, applied pharmacological treatment, and pain intensity.
Materials and methods: The study involved 38 patients (12 men and 26 women) hospitalised in the Rheumatologic Ward of the Orthopaedics and Rehabilitation Hospital of the University of Medical Sciences. The average age of the entire group was 56.26 years. Fatigue was evaluated with use of Polish version of Functional Assessment of Chronic Illness Therapy-Fatigue (FACIT-F), while in order to evaluate sleep quality within the examined group of patients the Pittsburgh Sleep Quality Index (PSQI) was used.
Results: Patients with rheumatoid arthritis in the analysed group have lower sleep quality, and within subjects with such a diagnosis the fatigue is present. The relation was found between fatigue and such variables as: age, illness duration, marital status, applied pharmacological treatment, and severity of pain. Sleep quality within patients with RA is correlated by such variables as: age, gender, applied pharmaceutical treatment, and severity of pain. It was identified that patients with lower sleep quality experience increased levels of fatigue.
Conclusions: There is a need to clarify which factors determine the level of fatigue and sleep quality in patients suffering from RA in future population-based research and to indicate to doctors, nurses, psychologists, and physiotherapists the significance and importance of the problem, which requires specialised and holistic care.
Sleep Quality in Patients with Rheumatoid Arthritis and Associations with Pain, Disability, Disease Duration, and Activity
Abstract
We aimed to assess the subjective sleep quality in patients with rheumatoid arthritis (RA) and its correlation with disease activity, pain, inflammatory parameters, and functional disability. In a cross-sectional study, patients with confirmed RA diagnosis responded to a questionnaire (consisting of socio-demographic data, the Health Assessment Questionnaire Disability Index, and the Medical Outcome Study Sleep Scale). Disease activity was assessed with the Clinical Disease Activity Index, and pain levels using the visual analogue scale. In addition, inflammatory markers (C-reactive protein, interleukin-6, and tumor necrosis factor alpha) were analyzed. Ninety-five patients were analyzed, predominantly female, with an average age of 50.59 (9.61) years. Fifty-seven percent reported non-optimal sleep duration, where functional disability (92.7% vs. 69.8%; p = 0.006) and higher median pain levels (3.75 (2.3⁻6.0) vs. 2.5 (2.0⁻3.5); p = 0.003) were also more prevalent. No differences in sociodemographic variables, disease duration or activity, inflammatory parameters, or use of biological and corticosteroid therapy were observed. The multivariate regression analysis showed that more intense pain was associated with a lower likelihood of optimal sleep (odds ratio (OR) = 0.68, 95% confidence interval (CI) 0.47⁻0.98, p = 0.038). Patients with RA report a high prevalence of non-optimal sleep, which is linked to pain level. Clinicians need to be aware of this issue and the potential effects on health and functional status.
Fatigue and sleep in children and adolescents with juvenile idiopathic arthritis:a cross-sectional study
Abstract
Background/aim: The aims of this study were to primarily investigate fatigue and sleep and to secondarily examine possible relationships between disease activity, pain, and functional ability in children and adolescents with juvenile idiopathic arthritis (JIA).
Materials and methods: Ninety-six patients were enrolled in the study. Disease activity, functional ability, fatigue symptoms, fatigue severity, and sleep quality were assessed with the Juvenile Arthritis Disease Activity Score (JADAS), Childhood Health Assessment Questionnaire (CHAQ), Pediatric Quality of Life Inventory-Multidimensional Fatigue Scale (PedsQL-F), visual analog scale (VAS), and Pittsburgh Sleep Quality Index (PSQI), respectively.
Results: Fatigue severity was moderate to high in 75% of patients with JIA and sleep quality was poor in 40% of them. VAS-fatigue was correlated with VAS-pain, VAS-wellbeing, PSQI, and sleep duration (P < 0.001). Significant relationships were found between the PedsQL-F and all other parameters except JADAS (P < 0.05). VAS-fatigue, CHAQ, and PSQI were identified as significant predictors of PedsQL-F (P < 0.05). Sleep quality, pain, and sleep duration were also significant predictors of fatigue severity (P < 0.05).
Conclusion: This study suggests that fatigue and sleep problems are common problems in JIA. If underlying factors of fatigue and sleep are understood, strategies for improving sleep/fatigue paradox may develop in JIA.
Sex Differences in Sleep Duration among Older Adults with Self-Reported Diagnosis of Arthritis: National Health and Nutrition Examination Survey, 2009-2012
Abstract
Objective: Sleep is restorative, essential, and beneficial to health. Prevalences of some diseases have been associated with sleep duration. There are few studies in the literature on the relationship of sleep duration and arthritis stratified by sex in older adults. The purpose of this research is to investigate sleep duration among older adults in the United States who have self-reported diagnosis of arthritis.
Methods: A cross-sectional study design was used. The data source was the National Health and Nutrition Examination 2009-2010 and 2011-2012. Self-reported diagnosis of arthritis and sleep duration were the variables of interest.
Results: There were 4,888 participants, aged 50 years and above, of whom 41.6% self-reported having a diagnosis of arthritis, and 60.6% were female. Of the people who had a self-reported diagnosis of arthritis, 15.2% reported sleeping 2-5 hours as compared with 10.9% of the people who did not have a self-reported diagnosis of arthritis (P = .0004). In bivariate analysis of self-reported diagnosis of arthritis and sleep stratified by sex, there were significantly more people with self-reported diagnosis of arthritis who slept 2-5 hours for both women (P = 0.0192) and men (P = 0.0231). The overall relationship remained significant in adjusted overall logistic regression comparing for self-reported diagnosis of arthritis for 2-5 hours of sleep (with 6-7 hours of sleep as the reference) (odds ratio: 1.35 [95% CI: 1.08, 1.70; P = 0.0103]); however, when the data were stratified by sex, the association failed to reach significance.
Conclusion: In this analysis of noninstitutionalized older adults in the United States, the prevalence of a self-reported diagnosis of arthritis was associated with shorter sleep duration in the overall analyses, but the association failed to reach significance when stratified by sex.
Association of sleep duration with rheumatoid arthritis in Korean adults: analysis of seven years of aggregated data from the Korea National Health and Nutrition Examination Survey (KNHANES)
Abstract
Objectives: To investigate the association between rheumatoid arthritis (RA) and self-reported sleep duration.
Setting: The present study analysed 7 years of aggregated cross-sectional data (2007-2013) from the Korea National Health and Nutrition Examination Surveys (KNHANES).
Participants: A total of 37 979 individuals were selected for the analyses.
Interventions: RA.
Primary and secondary outcome measures: Sleep duration.
Results: After adjusting for confounding factors, the odds of short-duration sleepers (≤6 hours/day) and long-duration sleepers (≥9 hours/day) for RA were 1.23-fold (95% CI 1.101 to 1.51) and 1.27-fold (95% CI 0.85 to 1.88) higher, respectively, than those for persons with sleep duration of 7-8 hours/day. A subgroup analysis according to the extent of pain in RA revealed that the strong relationship between RA and sleep disturbances was observed in those with high pain from RA (OR: 1.28 CI 1.04 to 1.58).
Conclusions: Individuals with RA may be at a higher risk for sleep disturbances compared with individuals without RA. Therefore, the provision of comprehensive care for patients with RA by healthcare professionals should include assessments of sleep duration and patients with RA should be encouraged to report sleep problems.
Depression
Treating insomnia improves depression, maladaptive thinking, and hyperarousal in postmenopausal women: comparing cognitive-behavioral therapy for insomnia (CBTI), sleep restriction therapy, and sleep hygiene education
Abstract
Introduction: Depression increases during menopause, and subclinical depressive symptoms increase risk for major depression. Insomnia is common among postmenopausal women and increases depression-risk in this already-vulnerable population. Recent evidence supports the efficacy of cognitive-behavioral therapy for insomnia (CBTI) to treat menopausal insomnia, but it remains unclear whether treating insomnia also alleviates co-occurring depressive symptoms and depressogenic features. This trial tested whether CBTI improves depressive symptoms, maladaptive thinking, and somatic hyperarousal in postmenopausal women with insomnia; as well as whether sleep restriction therapy (SRT)-a single component of CBTI-is equally efficacious.
Materials and methods: Single-site, randomized controlled trial. 117 postmenopausal women (56.34 ± 5.41 years) with peri-or-postmenopausal onset of chronic insomnia were randomized to three treatment conditions: sleep hygiene education control (SHE), SRT, and CBTI. Blinded assessments were performed at baseline, posttreatment, and six-month follow-up.
Results: CBTI produced moderate-to-large reductions in depressive symptoms, whereas SRT produced moderate reductions but not until six months posttreatment. Treatment effects on maladaptive thinking were mixed. CBTI and SRT both produced large improvements in dysfunctional beliefs about sleep, but weaker influences on presleep cognitive arousal, rumination, and worry. Presleep somatic arousal greatly improved in the CBTI group and moderately improved in the SRT group. Improvements in depression, maladaptive thinking, and hyperarousal were linked to improved sleep. SHE produced no durable treatment effects.
Conclusions: CBTI and SRT reduce depressive symptoms, dysfunctional beliefs about sleep, and presleep somatic hyperarousal in postmenopausal women, with CBTI producing superior results. Despite its cognitive emphasis, cognitive arousal did not respond strongly or durably to CBTI. NAME: Behavioral Treatment of Menopausal Insomnia: Sleep and Daytime Outcomes. URL: clinicaltrials.gov.
Chronic paradoxical sleep deprivation-induced depression-like behavior, energy metabolism and microbial changes in rats
Abstract
Aims: Given the lasting impact of chronic paradoxical sleep deprivation (PSD) on behavior and organism metabolic alternations, along with the role of the microbiome in neurobehavioral development and metabolism, we sought to examine the relationship between the microbiota and chronic PSD-induced behavioral and metabolic changes.
Materials and methods: Psychological status of 7-day PSD (7d-PSD) male rats was tested by behavioral method, serum inflammatory cytokines and hypothalamic-pituitary-adrenal (HPA) axis-related hormones. In addition, GC-MS based urine metabolomics and 16S rRNA gene sequencing approaches were applied to estimate the influences of chronic PSD on host metabolism and gut-microbiota. Furtherly, microbial functional prediction and Spearman's correlation analysis were implemented to manifest the relations between the differential urinary metabolites and gut microbiota.
Key findings: 7d-PSD rats displayed depression-like behavior, metabolic and microbial changes. By integrating differential gut bacteria with indicators of depression and differential metabolites, we found that the alterations of Akkermansia, Oscillospira, Ruminococcus, Parabacteroides, Aggregatibacter and Phascolarctobacterium were closely related to abnormalities of depression symptoms and inflammatory cytokines. These bacteria also had close connections with host energy metabolism concerning arginine and proline metabolism, glycine, serine and threonine metabolism, and glyoxylate and dicarboxylate metabolism, pyruvate metabolism, which overlapped with the results of 16S rRNA gene function annotation.
Significance: These data suggest that a specific situation of circadian disturbance, chronic PSD-induced alterations in gut microbiota and related host changes in metabolism may be the pathogenesis of depression.
Systematic review and meta-analysis of the relationship between sleep disorders and suicidal behaviour in patients with depression
Abstract
Background: The potential link between sleep disorders and suicidal behaviour has been the subject of several reviews. We performed this meta-analysis to estimate the overall association between sleep disorders and suicidal behaviour and to identify a more specific relationship in patients with depression.
Methods: A systematic search strategy was developed across the electronic databases PubMed, EMBASE and the Cochrane Library from inception to January 1, 2019 for studies that reported a relationship between sleep disorders and suicidal behaviour in depressed patients. The odds ratio (OR) and corresponding 95% confidence interval (CI) were used to measure the outcomes. Heterogeneity was evaluated by Cochran's Q test and the I2 statistic. The Newcastle-Ottawa Scale (NOS) was adopted to evaluate the methodological quality of each of the included studies, and the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach was used to assess the quality of the evidence. We calculated the overall association between sleep disorders and suicidal behaviour and estimated more specific categories, including insomnia, nightmares, hypersomnia, suicidal ideation, suicide attempt, and completed suicide.
Results: A total of 18 studies were included in this study. Overall, sleep disorders were closely related to suicidal behaviour in patients with depression (OR = 2.45 95% CI: 1.33 4.52). The relatively increased risks of sleep disorders with suicidal ideation, suicide attempt and completed suicide ranged from 1.24 (95% CI: 1.00 1.53) to 2.41 (95% CI: 1.45 4.02). Nightmares were found to be highly correlated with the risk of suicidal behaviour (OR = 4.47 95% CI: 2.00 9.97), followed by insomnia (OR = 2.29 95% CI: 1.69 3.10). The certainty of the evidence was rated as very low for the overall outcome and the major depression subgroup and was rated as low for the depression subgroup.
Conclusions: This meta-analysis supports the finding that sleep disorders, particularly nightmares and insomnia, increase the risk of suicidal behaviour in depressed patients. Considering that all included studies were observational, the quality of the evidence is rated as very low. More well-designed studies are needed to confirm our findings and to better explain the mechanisms by which sleep disorders aggravate suicidal behaviour in depressed patients.
The effect of non-pharmacological sleep interventions on depression symptoms: A meta-analysis of randomised controlled trials
Abstract
Poor sleep is a significant risk factor for depression across the lifespan and sleep problems have been hypothesised to contribute to the onset and maintenance of depression symptoms. However, sleep problems are usually not a direct target of interventions for depression. A range of non-pharmacological treatments can reduce sleep problems but it is unclear whether these interventions also reduce other depression symptoms. The aim of this review was to examine whether non-pharmacological interventions for sleep problems are effective in reducing symptoms of depression. We carried out a systematic search for randomised controlled trials of non-pharmacological sleep interventions that measured depression symptoms as an outcome. Forty-nine trials (n = 5908) were included in a random effects meta-analysis. The pooled standardised mean difference for depression symptoms after treatment for sleep problems was -0.45 (95% CI: -0.55,-0.36). The size of the effect on depression symptoms was moderated by the size of the effect on subjective sleep quality. In studies of participants with mental health problems, sleep interventions had a large effect on depression symptoms (d = -0.81, 95% CI: -1.13,-0.49). The findings indicate that non-pharmacological sleep interventions are effective in reducing the severity of depression, particularly in clinical populations. This suggests that non-pharmacological sleep interventions could be offered as a treatment for depression, potentially improving access to treatment.
Clarifying the role of sleep in depression: A narrative review
Abstract
It has been established that 4.4 to 20% of the general population suffers from a major depressive disorder (MDD), which is frequently associated with a dysregulation of normal sleep-wake mechanisms. Disturbances of circadian rhythms are a cardinal feature of psychiatric dysfunctions, including MDD, which tends to indicate that biological clocks may play a role in their pathophysiology. Thus, episodes of depression and mania or hypomania can arise as a consequence of the disruption of zeitgebers (time cues). In addition, the habit of sleeping at a time that is out of phase with the body's other biological rhythms is a common finding in depressed patients. In this review, we have covered a vast area, emerging from human and animal studies, which supports the link between sleep and depression. In doing so, this paper covers a broad range of distinct mechanisms that may underlie the link between sleep and depression. This review further highlights the mechanisms that may underlie such link (e.g. circadian rhythm alterations, melatonin, and neuroinflammatory dysregulation), as well as evidence for a link between sleep and depression (e.g. objective findings of sleep during depressive episodes, effects of pharmacotherapy, chronotherapy, comorbidity of obstructive sleep apnea and depression), are presented.
Connecting insomnia, sleep apnoea and depression
Poor sleep quality increases symptoms of depression and anxiety in postpartum women
Abstract
This study evaluated the relationship between sleep quality and symptoms of depression and anxiety in women studied in pregnancy and postpartum. Scores on standardized measures of sleep (PSQI) at 6 months postpartum, and symptoms of anxiety and depression (OASIS, the PHQ9, and EPDS) were assessed by structured interviews in 116 women in pregnancy and/or postpartum. Poor sleep quality was significantly associated with greater symptoms of depression and anxiety. Women who had significantly higher OASIS (anxiety) scores (β = .530, p < .001), PHQ9 (depression) scores (β = .496, p < .001), and EPDS (postpartum depression and anxiety) scores (β = .585, p < .001) also had elevated total PSQI scores after adjustment for covariates, including prenatal depression and anxiety scores. Though inferences about causality are not feasible, these results support emerging research showing sleep quality is a risk factor for negative maternal affect in the postpartum period. Assessment of maternal sleep hygiene is worth consideration as a component of identifying women at risk for postpartum depression and anxiety.
Sleep correlates of depression and anxiety in an elderly Asian population
Abstract
Background: Research looking at the association between sleep and psychiatric symptoms in elderly Asian populations is lacking. The present study examines the sleep correlates of depression and anxiety in a sample of cognitively healthy older adults.
Methods: The Geriatric Depression Scale, Geriatric Anxiety Inventory, and the Pittsburgh Sleep Quality Index were administered to a community sample of elderly participants (n = 107; 81 women; Mage = 71.3 years, SD = 5.7) RESULTS: Geriatric Depression Scale and Geriatric Anxiety Inventory scores are both significantly correlated with sleep disturbance. Geriatric Depression Scale scores are uniquely associated with daytime dysfunction, and Geriatric Anxiety Inventory scores are uniquely associated with perceived sleep quality, sleep latency, and global Pittsburgh Sleep Quality Index scores.
Conclusions: Depression and anxiety in a cohort of elderly Asian subjects are associated with a number of sleep-related issues; both are related to a somewhat different profile of sleep problems.
Keywords: Asia; anxiety; depression; elderly population; sleep problems.
Depression in sleep disturbance: A review on a bidirectional relationship, mechanisms and treatment
Abstract
Sleep disturbance is the most prominent symptom in depressive patients and was formerly regarded as a main secondary manifestation of depression. However, many longitudinal studies have identified insomnia as an independent risk factor for the development of emerging or recurrent depression among young, middle-aged and older adults. This bidirectional association between sleep disturbance and depression has created a new perspective that sleep problems are no longer an epiphenomenon of depression but a predictive prodromal symptom. In this review, we highlight the treatment of sleep disturbance before, during and after depression, which probably plays an important role in improving outcomes and preventing the recurrence of depression. In clinical practice, pharmacological therapies, including hypnotics and antidepressants, and non-pharmacological therapies are typically applied. A better understanding of the pathophysiological mechanisms between sleep disturbance and depression can help psychiatrists better manage this comorbidity.
Depression and obstructive sleep apnea
Abstract
Objective: Obstructive sleep apnea (OSA), is described as intermittent interruptions or reductions in airflow which are initiated by an incomplete or complete collapse of the upper airways despite respiratory effort. When left untreated, OSA is connected with comorbid conditions, such as cardiovascular and metabolic illnesses.
Method: The PubMed database was used to examine papers published until April 2017 using the subsequent terms: "obstructive sleep apnea" or "obstructive sleep apnoea" and "depression" in successive combination with "CPAP (continuous positive airway pressure)", "therapy", "pharmacotherapy", "psychotherapy", "cognitive behavioral therapy" or "quality of life".
Results: After assessment for the suitability, 126 articles were chosen. The numerous evidence of a connection between OSA and depressive symptoms, as well as depressive disorder, were found. This connection may be directly or indirectly linked due to the participation of some OSA mediators consequences such as obesity, hypertension, and the decreased quality of life. Patients with the comorbid major depression and OSA reported more severe and longer episodes of depression. Nevertheless, the information on the effect of the treatment of OSA using CPAP on the depressive symptoms was limited. Still, the current state of the art suggests that this treatment decreases the severity of the comorbid depressive symptoms.
Conclusions: It is important to evaluate the symptoms of depression in the patients with OSA. On the other side, a psychiatrist should not just treat the depression, as it is also important to screen individuals at high risk of OSA when assessing patients for depressive disorder, especially those with depression resistant to treatment.
Sleep, insomnia, and depression
Abstract
Since ancient times it is known that melancholia and sleep disturbances co-occur. The introduction of polysomnography into psychiatric research confirmed a disturbance of sleep continuity in patients with depression, revealing not only a decrease in Slow Wave Sleep, but also a disinhibition of REM (rapid eye movement) sleep, demonstrated as a shortening of REM latency, an increase of REM density, as well as total REM sleep time. Initial hopes that these abnormalities of REM sleep may serve as differential-diagnostic markers for subtypes of depression were not fulfilled. Almost all antidepressant agents suppress REM sleep and a time-and-dose-response relationship between total REM sleep suppression and therapeutic response to treatment seemed apparent. The so-called Cholinergic REM Induction Test revealed that REM sleep abnormalities can be mimicked by administration of cholinomimetic agents. Another important research avenue is the study of chrono-medical timing of sleep deprivation and light exposure for their positive effects on mood in depression. Present day research takes the view on insomnia, i.e., prolonged sleep latency, problems to maintain sleep, and early morning awakening, as a transdiagnostic symptom for many mental disorders, being most closely related to depression. Studying insomnia from different angles as a transdiagnostic phenotype has opened many new perspectives for research into mechanisms but also for clinical practice. Thus, the question is: can the early and adequate treatment of insomnia prevent depression? This article will link current understanding about sleep regulatory mechanisms with knowledge about changes in physiology due to depression. The review aims to draw the attention to current and future strategies in research and clinical practice to the benefits of sleep and depression therapeutics.
Adolescents' electronic media use at night, sleep disturbance, and depressive symptoms in the smartphone age
Abstract
Adolescence is a time of increasing vulnerability for poor mental health, including depression. Sleep disturbance is an important risk factor for the development of depression during adolescence. Excessive electronic media use at night is a risk factor for both adolescents' sleep disturbance and depression. To better understand the interplay between sleep, depressive symptoms, and electronic media use at night, this study examined changes in adolescents' electronic media use at night and sleep associated with smartphone ownership. Also examined was whether sleep disturbance mediated the relationship between electronic media use at night and depressive symptoms. 362 adolescents (12-17 year olds, M = 14.8, SD = 1.3; 44.8% female) were included and completed questionnaires assessing sleep disturbance (short sleep duration and sleep difficulties) and depressive symptoms. Further, participants reported on their electronic media use in bed before sleep such as frequency of watching TV or movies, playing video games, talking or text messaging on the mobile phone, and spending time online. Smartphone ownership was related to more electronic media use in bed before sleep, particularly calling/sending messages and spending time online compared to adolescents with a conventional mobile phone. Smartphone ownership was also related to later bedtimes while it was unrelated to sleep disturbance and symptoms of depression. Sleep disturbance partially mediated the relationship between electronic media use in bed before sleep and symptoms of depression. Electronic media use was negatively related with sleep duration and positively with sleep difficulties, which in turn were related to depressive symptoms. Sleep difficulties were the more important mediator than sleep duration. The results of this study suggest that adolescents might benefit from education regarding sleep hygiene and the risks of electronic media use at night.
Sleep Disturbance and Short Sleep as Risk Factors for Depression and Perceived Medical Errors in First-Year Residents
Abstract
Study objectives: While short and poor quality sleep among training physicians has long been recognized as problematic, the longitudinal relationships among sleep, work hours, mood, and work performance are not well understood. Here, we prospectively characterize the risk of depression and medical errors based on preinternship sleep disturbance, internship-related sleep duration, and duty hours.
Methods: Survey data from 1215 nondepressed interns were collected at preinternship baseline, then 3 and 6 months into internship. We examined how preinternship sleep quality and internship sleep and work hours affected risk of depression at 3 months, per the Patient Health Questionnaire 9. We then examined the impact of sleep loss and work hours on depression persistence from 3 to 6 months. Finally, we compared self-reported errors among interns based on nightly sleep duration (≤6 hr vs. >6 hr), weekly work hours (<70 hr vs. ≥70 hr), and depression (non- vs. acutely vs. chronically depressed).
Results: Poorly sleeping trainees obtained less sleep and were at elevated risk of depression in the first months of internship. Short sleep (≤6 hr nightly) during internship mediated the relationship between sleep disturbance and depression risk, and sleep loss led to a chronic course for depression. Depression rates were highest among interns with both sleep disturbance and short sleep. Elevated medical error rates were reported by physicians sleeping ≤6 hr per night, working ≥ 70 weekly hours, and who were acutely or chronically depressed.
Conclusions: Sleep disturbance and internship-enforced short sleep increase risk of depression development and chronicity and medical errors. Interventions targeting sleep problems prior to and during residency hold promise for curbing depression rates and improving patient care.
Depression and sleep duration: findings from middle-aged and elderly people in China
Abstract
Objective: This study aims to investigate whether depression is associated with subsequent sleep duration among middle-aged and elderly people in China.
Study design: Cross-sectional study.
Methods: Data were obtained from the China Health and Retirement Longitudinal Study (CHARLS). Depression was evaluated from the 2011 baseline survey data using the Chinese version of the Center for Epidemiologic Studies Depression scale (CES-D). All other data were extracted from CHARLS 2013 survey data. Sleep duration was assessed according to the American National Sleep Foundation. Participants were divided into subgroups based on their gender (male or female) and age (45-59 years [middle-aged] or ≥60 years [elderly people]). The relative risk ratios (RRRs) were calculated using the multinomial logistic regression analysis method.
Results: No significant associations were found between depression and subsequent long sleep duration among middle-aged and elderly people in China; in addition, no association was found during subgroup analysis. The adjusted RRR (RRR = 1.71; 95% confidence interval [CI] = 1.56-1.88) shows there is a significant association between depression and subsequent short sleep duration among subgroups. The RRR of the male, female, middle-aged, and elderly people were 1.64 (95% CI=1.38-1.95), 1.74 (95% CI=1.56-1.95), 1.68 (95% CI = 1.47-1.92), 1.74 (95% CI = 1.52-1.99), respectively, which revealed that this association was still significant in subgroups.
Conclusions: Findings from this study suggest that there is a complex association between depression and subsequent alternations in sleep duration among middle-aged and elderly people in China.
Synaptic plasticity model of therapeutic sleep deprivation in major depression
Abstract
Therapeutic sleep deprivation (SD) is a rapid acting treatment for major depressive disorder (MDD). Within hours, SD leads to a dramatic decrease in depressive symptoms in 50-60% of patients with MDD. Scientifically, therapeutic SD presents a unique paradigm to study the neurobiology of MDD. Yet, up to now, the neurobiological basis of the antidepressant effect, which is most likely different from today's first-line treatments, is not sufficiently understood. This article puts the idea forward that sleep/wake-dependent shifts in synaptic plasticity, i.e., the neural basis of adaptive network function and behavior, represent a critical mechanism of therapeutic SD in MDD. Particularly, this article centers on two major hypotheses of MDD and sleep, the synaptic plasticity hypothesis of MDD and the synaptic homeostasis hypothesis of sleep-wake regulation, and on how they can be integrated into a novel synaptic plasticity model of therapeutic SD in MDD. As a major component, the model proposes that therapeutic SD, by homeostatically enhancing cortical synaptic strength, shifts the initially deficient inducibility of associative synaptic long-term potentiation (LTP) in patients with MDD in a more favorable window of associative plasticity. Research on the molecular effects of SD in animals and humans, including observations in the neurotrophic, adenosinergic, monoaminergic, and glutamatergic system, provides some support for the hypothesis of associative synaptic plasticity facilitation after therapeutic SD in MDD. The model proposes a novel framework for a mechanism of action of therapeutic SD that can be further tested in humans based on non-invasive indices and in animals based on direct studies of synaptic plasticity. Further determining the mechanisms of action of SD might contribute to the development of novel fast acting treatments for MDD, one of the major health problems worldwide.
#Sleepyteens: Social media use in adolescence is associated with poor sleep quality, anxiety, depression and low self-esteem
Abstract
This study examined how social media use related to sleep quality, self-esteem, anxiety and depression in 467 Scottish adolescents. We measured overall social media use, nighttime-specific social media use, emotional investment in social media, sleep quality, self-esteem and levels of anxiety and depression. Adolescents who used social media more - both overall and at night - and those who were more emotionally invested in social media experienced poorer sleep quality, lower self-esteem and higher levels of anxiety and depression. Nighttime-specific social media use predicted poorer sleep quality after controlling for anxiety, depression and self-esteem. These findings contribute to the growing body of evidence that social media use is related to various aspects of wellbeing in adolescents. In addition, our results indicate that nighttime-specific social media use and emotional investment in social media are two important factors that merit further investigation in relation to adolescent sleep and wellbeing.
Effects of Antidepressants on Sleep
Abstract
Purpose of review: The aim of this review article was to summarize recent publications on effects of antidepressants on sleep and to show that these effects not only depend on the kind of antidepressant drugs but are also related to the dose, the time of drug administration, and the duration of the treatment.
Recent findings: Complaints of disrupted sleep are very common in patients suffering from depression, and they are listed among diagnostic criteria for this disorder. Moreover, midnocturnal insomnia is the most frequent residual symptom of depression. Thus, all antidepressants should normalize sleep. However, at least in short-term treatment, many antidepressants with so-called activating effects (e.g. fluoxetine, venlafaxine) may disrupt sleep, while others with sedative properties (e.g., doxepin, mirtazapine, trazodone) rapidly improve sleep, but may cause problems in long-term treatment due to oversedation.For sleep-promoting action, the best effects can frequently be achieved with a very low dose, administered early enough before bedtime and importantly, always as a part of more complex interventions based on the cognitive-behavioral protocol to treat insomnia (CBT-I). For successful treatment of depression, it is necessary to understand the effects of antidepressants on sleep. Each physician should also be aware that some antidepressants may worsen or induce primary sleep disorders like restless legs syndrome, sleep bruxism, REM sleep behavior disorder, nightmares, and sleep apnea, which may result from an antidepressant-induced weight gain.
REM sleep dysregulation in depression: state of the art
Abstract
Disturbances of sleep are typical for most depressed patients and belong to the core symptoms of the disorder. Since the 1960s polysomnographic sleep research has demonstrated that besides disturbances of sleep continuity, depression is associated with altered sleep architecture, i.e., a decrease in slow wave sleep (SWS) production and disturbed rapid eye movement (REM) sleep regulation. Shortened REM latency (i.e., the interval between sleep onset and the occurrence of the first REM period), increased REM sleep duration and increased REM density (i.e., the frequency of rapid eye movements per REM period) have been considered as biological markers of depression which might predict relapse and recurrence. High risk studies including healthy relatives of patients with depression demonstrate that REM sleep alterations may precede the clinical expression of depression and may thus be useful in identifying subjects at high risk for the illness. Several models have been developed to explain REM sleep abnormalities in depression, like the cholinergic-aminergic imbalance model or chronobiologically inspired theories, which are reviewed in this overview. Moreover, REM sleep alterations have been recently considered not only as biological "scars" but as true endophenotypes of depression. This review discusses the genetic, neurochemical and neurobiological factors that have been implicated to play a role in the complex relationships between REM sleep and depression. We hypothesize on the one hand that REM sleep dysregulation in depression may be linked to a genetic predisposition/vulnerability to develop the illness; on the other hand it is conceivable that REM sleep disinhibition in itself is a part of a maladaptive stress reaction with increased allostatic load. We also discuss whether the REM sleep changes in depression may contribute themselves to the development of central symptoms of depression such as cognitive distortions including negative self-esteem and the overnight consolidation of negatively toned emotional memories.
SLEEP DURATION AND DEPRESSION AMONG ADULTS: A META-ANALYSIS OF PROSPECTIVE STUDIES
Abstract
Background: Results from longitudinal studies on sleep duration and incidence of depression remain controversial.
Methods: PubMed and Web of Science updated on October 22, 2014 were searched for eligible publications. Pooled relative risks (RRs) with 95% confidence interval (CI) were calculated using a random-effects model.
Results: Seven prospective studies were included, involving 25,271 participants for short sleep duration and 23,663 participants for long sleep duration. Compared with the normal sleep duration, the pooled RR for depression was 1.31 (95% CI, 1.04-1.64; I(2) = 0%) for the short sleep duration overall. For long sleep duration, the pooled RR was 1.42 (95% CI, 1.04-1.92; I(2) = 0%). The associations between short or long sleep duration and risk of depression did not substantially change in sensitivity and subgroup analyses. No evidence of publication bias was found.
Conclusion: This meta-analysis indicates that short and long sleep duration was significantly associated with increased risk of depression in adults.
Shift Work and Poor Mental Health: A Meta-Analysis of Longitudinal Studies
Abstract
Background. Shift work is characterized by employees working outside the standard hours of 7:00 am to 6:00 pm. Because shift work includes night work, the normal sleep-wake cycle (circadian rhythm) is disrupted, with potential consequences for shift workers' physical and mental health.Objectives. To assess the pooled effects of shift work on mental health and to evaluate whether these differ in men and women.Search Methods. We searched PubMed, Scopus, and Web of Science databases for peer-reviewed or government reports published up to August 2018Selection Criteria. To be included, studies had to be longitudinal or case-control studies of shift work exposure associated with adverse mental health outcomes. For subanalyses, we grouped these outcomes as anxiety symptoms, depressive symptoms, or general poor mental health symptoms.Data Collection and Analysis. We followed the Meta-Analysis of Observational Studies in Epidemiology Group guidelines. We extracted adjusted risk estimates for each study to calculate pooled effect sizes (ESs) using random effect models and metaregression analysis to explore sources of heterogeneity.Main Results. We included 7 longitudinal studies, with 28 431 unique participants. Shift work was associated with increased overall risk of adverse mental health outcomes combined (ES = 1.28; 95% confidence interval [CI] = 1.02, 1.62; I2 = 70.6%) and specifically for depressive symptoms (ES = 1.33; 95% CI = 1.02, 1.74; I2 = 31.5%). Gender differences explained more than 90% of heterogeneity, with female shift workers more likely to experience depressive symptoms than female non-shift workers (odds ratio = 1.73; 95% CI = 1.39, 2.14).Authors' Conclusions. To our knowledge, this is the first meta-analysis to investigate the pooled effects of shift work on the risk of poor mental health, including subanalyses by type of poor mental health and gender. Shift workers, particularly women, are at increased risk for poor mental health, particularly depressive symptoms.Public Health Implications. Depression accounts for 4.3% of the global burden of disease and incidence, with mental disorders worldwide predicted to cost US $16.3 million by 2030. With 1 in 5 people in the United States and Europe doing shift work, and the increased risk of poor mental health among shift workers, shift work industries are a priority context for reducing this burden. Workplace health promotion programs and policies are needed to minimize shift workers' risk of poor mental health.
Night Shift Work and Risk of Depression: Meta-analysis of Observational Studies
Abstract
This study aimed to assess whether night shift work is associated with the risk of depression by using a meta-analysis of observational studies. We searched PubMed and EMBASE in August, 2016 to locate eligible studies and investigated the association between night shift work and the risk of depression, reporting outcome measures with adjusted odds ratios (ORs) or relative risks (RRs) and 95% confidence intervals (CIs). In the meta-analysis of a total of 11 observational studies with 9 cross-sectional study, 1 longitudinal study, and 1 cohort study, night shift work was significantly associated with an increased risk of depression (OR/RR, 1.43; 95% CI, 1.24-1.64; I² = 78.0%). Also, subgroup meta-analyses by gender, night shift work duration, type of occupation, continent, and type of publication showed that night shift work was consistently associated with the increased risk of depression. The current meta-analysis suggests that night shift work is associated with the increased risk of depression. However, further large prospective cohort studies are needed to confirm this association.
Sleep and Antidepressant Treatment
The aim of this review was to describe the sleep anomalies in depression, the effects of antidepressants on sleep, the usefulness of antidepressants in the treatment of primary insomnia and insomnia in other psychiatric disorders.
Depression is associated with abnormalities in the sleep pattern that include disturbances of sleep continuity, diminished slow-wave sleep (SWS) and altered rapid eye movement (REM) sleep parameters. Although none of the reported changes in sleep are specific to depression, many of them, for example increased REM density and reduced amount of SWS in the first sleep cycle, are used as biological markers for research on depression and in the development of antidepressant drugs.
An antidepressant should reverse abnormalities in the sleep pattern. However, many antidepressants can worsen sleep. Because of the activating effects of some drugs, for example imipramine, desipramine, fluoxetine, paroxetine, venlafaxine, reboxetine and bupropion, many patients who take them have to be co-prescribed with sleep-promoting agents to improve sleep. Even in maintenance treatment with activating antidepressants as many as 30-40%; of patients may still suffer from insomnia. Antidepressants with sleep-promoting effects include sedative antidepressants, for example doxepin, mirtazapine, trazodone, trimipramine, and agomelatine which promotes sleep not through a sedative action but through resynchronization of the circadian rhythm. Sedative antidepressants are frequently used in the treatment of primary insomnia, although not many double-blind studies have been provided to support such an approach to insomnia treatment. One exception is doxepin, which has been approved for the treatment of insomnia characterized by difficulties in maintaining sleep.
A review of lifestyle factors that contribute to important pathways associated with major depression: Diet, sleep and exercise
Abstract
Research on major depression has confirmed that it is caused by an array of biopsychosocial and lifestyle factors. Diet, exercise and sleep are three such influences that play a significant mediating role in the development, progression and treatment of this condition. This review summarises animal- and human-based studies on the relationship between these three lifestyle factors and major depressive disorder, and their influence on dysregulated pathways associated with depression: namely neurotransmitter processes, immuno-inflammatory pathways, hypothalamic–pituitary–adrenal (HPA) axis disturbances, oxidative stress and antioxidant defence systems, neuroprogression, and mitochondrial disturbances. Increased attention in future clinical studies on the influence of diet, sleep and exercise on major depressive disorder and investigations of their effect on physiological processes will help to expand our understanding and treatment of major depressive disorder. Mental health interventions, taking into account the bidirectional relationship between these lifestyle factors and major depression are also likely to enhance the efficacy of interventions associated with this disorder.
A Systematic Review Assessing Bidirectionality between Sleep Disturbances, Anxiety, and Depression
Abstract
Study Objectives:
To investigate whether sleep disturbances are bidirectionally related to anxiety and depression, and thus identify potential risk factors for each problem.
Design:
A systematic review was conducted on 9 studies (8 longitudinal, 1 retrospective) that assessed bidirectionality between a sleep disturbance, and anxiety or depression. Treatment studies were excluded, along with those solely based on clinical samples or cohorts at high risk of suffering from a sleep disturbance, anxiety and depression. Eligible studies were identified by searching PubMed, PsychINFO, Embase, and Scopus databases, and reference lists of eligible studies. Publication dates ranged from the beginning of each database to December 2011.
Measurements and Results:
Syntheses of longitudinal studies suggested insomnia and sleep quality were bidirectionally related to anxiety and depression, and depression/anxiety, respectively. Childhood sleep problems significantly predicted higher levels of depression and a combined depression/anxiety variable, but not vice-versa. A one-way relationship was found where anxiety predicted excessive daytime sleepiness, but excessive daytime sleepiness was not associated with depression.
Conclusions:
Definitive conclusions regarding bidirectionality cannot be made for most sleep disturbances due to the small number and heterogeneity of cohort samples used across studies. Nevertheless, best available evidence suggests insomnia is bidirectionally related to anxiety and depression. Clinical and theoretical implications are discussed.
Cytokine-induced depression during IFN-α treatment: The role of IL-6 and sleep quality
Abstract
Depressive symptoms, poor sleep quality, and systemic markers of inflammation (e.g.,
interleukin
(IL)-6) are frequently associated.
Interferon-alpha
(IFN-α) therapy results in Major Depressive Disorder (MDD) in some people, offering the possibility to elucidate the relationship of MDD to sleep and inflammation during treatment. In particular, delineating the temporal relations among these factors could help inform their causal relationships. To this end, a cohort of 95 non-depressed hepatitis C patients was followed prospectively for four consecutive months during IFN-α therapy. We found that higher pre-treatment levels of circulating IL-6 predicted incidence of MDD (X2(1) = 7.7; p < 0.05). Time-lagged mixed-effect analyses supported uni-directional associations in which IL-6 predicted next month’s PSQI scores (F(47, 11.6) = 78.4; p < 0.0005), and PSQI scores predicted next month’s depressive Beck Depression Inventory-II (BDI) scores (F(16, 22.6) = 3.4; p < 0.005). In addition, on any given month of treatment, IL-6 levels predicted BDI symptoms the following month (F(16, 97.5) = 7.3; p < 0.0005), and conversely BDI predicted next month’s IL-6 (F(14, 7.4) = 5.2; p < 0.05) – providing evidence for a positive feedback relationship between depressive symptoms and
systemic inflammation
. These data provide further evidence that high levels of inflammation and poor sleep quality may be risk factors for IFN-α induced depression. Furthermore, these findings highlight the complex temporal relationships that exist among sleep, depression, and inflammation, and support the need for further prospective investigations to elucidate the dynamics that underlie depression during IFN-α treatment.
Depression and sleep: pathophysiology and treatment
Abstract
This review examines the relationship between sleep and depression. Most depressive disorders are characterized by subjective sleep disturbances, and the regulation of sleep is intricately linked to the same mechanisms that are implicated in the pathophysiology of depression. After briefly reviewing the physiology and topography of normal sleep, the disturbances revealed in studies of sleep in depression using polysomnographic recordings and neuroimaging assessments are discussed. Next, treatment implications of the disturbances are reviewed at both clinical and neuro-biologic levels. Most antidepressant medications suppress rapid eye movement (REM) sleep, although this effect is neither necessary nor sufficient for clinical efficacy. Effects on patients' difficulties initiating and maintaining sleep are more specific to particular types of antidepressants. Ideally, an effective antidepressant will result in normalization of disturbed sleep in concert with resolution of the depressive syndrome, although few interventions actually restore decreased slow-wave sleep. Antidepressants that block central histamine 1 and serotonin 2 tend to have stronger effects on sleep maintenance, but are also prone to elicit complaints of daytime sedation. Adjunctive treatment with sedative hypnotic medications-primarily potent, shorter-acting benzodiazepine and γ-aminobutyric acid (GABA A)-selective compounds such as zolpidem-are often used to treat associated insomnia more rapidly. Cognitive behavioral therapy and other nonpharmacologic strategies are also helpful.
Inflammation and Behavioral Symptoms After Breast Cancer Treatment: Do Fatigue, Depression, and Sleep Disturbance Share a Common Underlying Mechanism?
Abstract
Purpose
Fatigue, depression, and sleep disturbance are common adverse effects of cancer treatment and frequently co-occur. However, the possibility that inflammatory processes may underlie this constellation of symptoms has not been examined.
Patients and Methods
Women (N = 103) who had recently finished primary treatment (ie, surgery, radiation, chemotherapy) for early-stage breast cancer completed self-report scales and provided blood samples for determination of plasma levels of inflammatory markers: soluble tumor necrosis factor (TNF) receptor II (sTNF-RII), interleukin-1 receptor antagonist, and C-reactive protein.
Results
Symptoms were elevated at the end of treatment; greater than 60% of participants reported clinically significant problems with fatigue and sleep, and 25% reported elevated depressive symptoms. Women treated with chemotherapy endorsed higher levels of all symptoms and also had higher plasma levels of sTNF-RII than women who did not receive chemotherapy (all P < .05). Fatigue was positively associated with sTNF-RII, particularly in the chemotherapy-treated group (P < .05). Depressive symptoms and sleep problems were correlated with fatigue but not with inflammatory markers.
Conclusion
This study confirms high rates of behavioral symptoms in breast cancer survivors, particularly those treated with chemotherapy, and indicates a role for TNF-α signaling as a contributor to postchemotherapy fatigue. Results also suggest that fatigue, sleep disturbance, and depression may stem from distinct biologic processes in post-treatment survivors, with inflammatory signaling contributing relatively specifically to fatigue.
Relationship between Obstructive Sleep Apnea Severity and Sleep, Depression and Anxiety Symptoms in Newly-Diagnosed Patients
Abstract
Obstructive sleep apnea (OSA) occurs in at least 10% of the population, and leads to higher morbidity and mortality; however, relationships between OSA severity and sleep or psychological symptoms are unclear. Existing studies include samples with wide-ranging comorbidities, so we assessed relationships between severity of OSA and common sleep and psychological disturbances in recently diagnosed OSA patients with minimal co-morbidities. We studied 49 newly diagnosed, untreated OSA patients without major co-morbidities such as mental illness, cardiovascular disease, or stroke; subjects were not using psychoactive medications or tobacco (mean ± std age: 46.8±9.1 years; apnea/hyponea index [AHI]: 32.1±20.5 events/hour; female/male: 12/37; weight <125 kg). We evaluated relationships between the AHI and daytime sleepiness (Epworth Sleepiness Scale; ESS), sleep quality (Pittsburg Sleep Quality Index; PSQI), depressive symptoms (Beck Depression Inventory-II; BDI), and anxiety symptoms (Beck Anxiety Inventory; BAI), as well as sex and body mass index (BMI). AHI was similar in females and males. Mean levels of all symptoms were above normal thresholds, but AHI was not correlated with age, ESS, PSQI, BDI, or BAI; only BMI was correlated with OSA severity. No differences in mean AHI appeared when subjects were grouped by normal versus elevated values of ESS, PSQI, BDI, or BAI. Consistent with other studies, a strong link between OSA severity and psychological symptoms did not appear in these newly diagnosed patients, suggesting that mechanisms additional to the number and frequency of hypoxic events and arousals occurring with apneas contribute to adverse health effects in OSA. OSA patients presenting with mild or moderate severity, and no major co-morbidities will not necessarily have low levels of sleep or psychological disturbances.
The Prospective Association between Sleep Deprivation and Depression among Adolescents
Abstract
Study Objectives:
To examine the prospective, reciprocal association between sleep deprivation and depression among adolescents.
Design:
A community-based two-wave cohort study.
Setting:
A metropolitan area with a population of over 4 million.
Participants:
4,175 youths 11-17 at baseline, and 3,134 of these followed up a year later.
Measurements:
Depression is measured using both symptoms of depression and DSM-IV major depression. Sleep deprivation is defined as ≤ 6 h of sleep per night.
Results:
Sleep deprivation at baseline predicted both measures of depression at follow-up, controlling for depression at baseline. Examining the reciprocal association, major depression at baseline, but not symptoms predicted sleep deprivation at follow-up.
Conclusion:
These results are the first to document reciprocal effects for major depression and sleep deprivation among adolescents using prospective data. The data suggest reduced quantity of sleep increases risk for major depression, which in turn increases risk for decreased sleep.
REM sleep dysregulation in depression: State of the art
Summary
Disturbances of sleep are typical for most depressed patients and belong to the core symptoms of the disorder. Since the 1960s polysomnographic sleep research has demonstrated that besides disturbances of sleep continuity, depression is associated with altered sleep architecture, i.e., a decrease in
slow wave sleep
(SWS) production and disturbed
rapid eye movement
(REM) sleep regulation. Shortened REM latency (i.e., the interval between sleep onset and the occurrence of the first REM period), increased REM sleep duration and increased REM density (i.e., the frequency of rapid eye movements per REM period) have been considered as biological markers of depression which might predict relapse and recurrence. High risk studies including healthy relatives of
patients with depression
demonstrate that REM sleep alterations may precede the clinical expression of depression and may thus be useful in identifying subjects at high risk for the illness. Several models have been developed to explain REM sleep abnormalities in depression, like the cholinergic–aminergic imbalance model or chronobiologically inspired theories, which are reviewed in this overview. Moreover, REM sleep alterations have been recently considered not only as biological “scars” but as true
endophenotypes
of depression. This review discusses the genetic, neurochemical and neurobiological factors that have been implicated to play a role in the complex relationships between REM sleep and depression. We hypothesize on the one hand that REM sleep dysregulation in depression may be linked to a genetic predisposition/vulnerability to develop the illness; on the other hand it is conceivable that REM sleep disinhibition in itself is a part of a maladaptive stress reaction with increased
allostatic load
. We also discuss whether the REM sleep changes in depression may contribute themselves to the development of central symptoms of depression such as cognitive distortions including negative self-esteem and the overnight consolidation of negatively toned emotional memories.
Diabetes
Sleep disturbance in people with diabetes: A concept analysis
Abstract
Aims and objectives: To clarify the meaning of sleep disturbance in people with diabetes and examine its antecedents, attributes and consequences through concept analysis.
Background: Sleep is crucial for health, and people with diabetes are frequently beset with disturbances in their sleep. The concept of sleep disturbance in people with diabetes has not been clearly defined. The inconsistent use of sleep disturbance has created confusion and impeded our understanding of the sleep in people with diabetes. This analysis will provide a conceptual foundation of sleep disturbance in diabetes, thereby facilitating more effective means for assessment and treatment.
Design: Concept analysis.
Methods: A systematic search without time restriction on the publication year was carried out using PubMed, CINAHL, PsycINFO, Web of Science and ProQuest Dissertations and Theses. Rodgers's method of evolutionary concept analysis guided the analysis. Inductive thematic analysis was conducted to identify the attributes, antecedents and consequences.
Results: Based on the 26 eligible studies, two major attributes are that sleep disturbance is a symptom and is characterised by impaired sleep quality and/or abnormal sleep duration. Two antecedents are diabetes-related physiological change and psychological well-being. Sleep disturbance can result in impaired daytime functioning, glucose regulation and quality of life.
Conclusions: Defining the concept of sleep disturbance in people with diabetes facilitates consistent use and effective communication in both practice and research. Sleep disturbance in people with diabetes is a complex symptom that includes impaired sleep quality and/or abnormal sleep duration. This paper contributes to the current knowledge of sleep in people with diabetes. Future research on antecedents and consequences of sleep disturbance is necessary for further clarifications.
Abstract
Background: Associations between sleep duration and type 2 diabetes (T2D) risk markers in childhood have been little studied. We examined associations between self-reported sleep duration and T2D risk markers in children.
Methods: Cross-sectional study of 4525 multiethnic UK children aged 9 to 10 years. Sleep time was calculated from self-reported usual time of going to bed and getting up on a school day, validated in a subset using accelerometers. Fasting blood samples provided levels of serum lipids and insulin, plasma glucose, and HbA1c. Physical measures included height, weight, bioimpedance, and blood pressure. Multilevel linear regression models of anthropometric, T2D, and cardiovascular risk markers with sleep duration were adjusted for sex, age, month, ethnicity, socioeconomic position, observer (physical measures only), and random effect of school.
Results: On average, children slept 10.5 hours per night (95% range 8.0-12.0 hours). There were strong inverse graded relationships between sleep duration, adiposity, and diabetes risk markers. In adjusted models, a 1-hour-longer sleep duration was associated with 0.19 lower BMI (95% confidence interval [CI] 0.09 to 0.28), 0.03 kg/m5 lower fat mass index (95% CI 0.00 to 0.05 kg/m5), 2.9% lower homeostasis model assessment insulin resistance (95% CI 1.2% to 4.4%), and 0.24% lower fasting glucose (95% CI 0.03% to 0.44%); there was no association with HbA1c or cardiovascular risk. Associations with insulin and glucose remained after an additional adjustment for adiposity markers.
Conclusions: The finding of an inverse association between sleep duration and T2D risk markers in childhood is novel. Intervention studies are needed to establish the causality of these associations, which could provide a simple strategy for early T2D prevention.
Sleep characteristics in young adults with type 1 diabetes
Abstract
Only 14% of young adults with Type 1 Diabetes (T1D) achieve targets for glycemic control (HbA1C < 7.0%), with deterioration over time. Complex cognitive processes required to manage glycemia are vulnerable to sleep deficiency. Using Whittemore and Knafl's approach, we conducted an integrative review of research literature on sleep characteristics and glycemia in these young adults. Quality was assessed using the Mixed Methods Appraisal Tool (v. 2011). Multiple databases were searched for articles published in English in peer-reviewed journals from 2003 to 2018, using search terms 'sleep' and 'T1D' with age limiters 18-40. Of 218 studies initially retrieved, 17 original studies met the inclusion criteria. The following themes were identified in young adults with T1D: (1) They had poorer objective and subjective sleep quality, more variability, and impaired awakening response to hypoglycemia compared with controls; (2) They had poorer glycemic control that was associated with shorter sleep duration, poorer sleep quality, and less time in deep sleep; and (3) Hypoglycemia negatively impacted diabetes management, sleep quality, and next day functioning. Sleep deficiency, as indicated by short sleep duration is associated with a range of negative health outcomes for people with T1D; therefore, optimizing sleep should be a priority in practice and research.
Abstract
Sleep disturbances [short (<6 h) and long (>8 h) sleeping time, insomnia (initiating or maintaining sleep), obstructive sleep apnea (OSA) and abnormal sleep timing] have been associated with increased diabetes risk but the effect size relative to that of traditional risk factors is unknown. We conducted a systematic review and meta-analysis to compare the risk associated with sleep disturbances to traditional risk factors. Studies were identified from Medline and Scopus. Cohort studies measuring the association between sleep disturbances and incident diabetes were eligible. For traditional risk factors (i.e., overweight, family history, and physical inactivity), systematic reviews with or without meta-analysis were included. Thirty-six studies (1,061,555 participants) were included. Pooled relative risks (RRs) of sleep variables were estimated using a random-effect model. Pooled RRs of sleeping ≤5 h, 6 h, and ≥9 h/d were respectively 1.48 (95%CI:1.25,1.76), 1.18 (1.10,1.26) and 1.36 (1.12,1.65). Poor sleep quality, OSA and shift work were associated with diabetes with a pooled RR of 1.40 (1.21,1.63), 2.02 (1.57, 2.61) and 1.40 (1.18,1.66), respectively. The pooled RRs of being overweight, having a family history of diabetes, and being physically inactive were 2.99 (2.42,3.72), 2.33 (1.79,2.79), and 1.20 (1.11,1.32), respectively. In conclusion, the risk of developing diabetes associated with sleep disturbances is comparable to that of traditional risk factors. Sleep disturbances should be considered in clinical guidelines for type 2 diabetes screening.
Disturbed sleep and diabetes: A potential nexus of dementia risk
Abstract
Type 2 diabetes (T2D) and sleep disturbance (e.g., insomnia, sleep-disordered breathing) are prevalent conditions among older adults that are associated with cognitive decline and dementia, including Alzheimer's disease (AD). Importantly, disturbed sleep is associated with alterations in insulin sensitivity and glucose metabolism, and may increase the risk of T2D, and T2D-related complications (e.g., pain, nocturia) can negatively affect sleep. Despite these associations, little is known about how interactions between T2D and sleep disturbance might alter cognitive trajectories or the pathological changes that underlie dementia. Here, we review links among T2D, sleep disturbance, cognitive decline and dementia-including preclinical and clinical AD-and identify gaps in the literature, that if addressed, could have significant implications for the prevention of poor cognitive outcomes.
[Obstructive sleep apnea-hypopnea and stroke]
Abstract
Stroke, one of the main causes of disability and death worldwide, is frequently associated to the obstructive sleep apnea-hypopnea syndrome. This sleep disorder has been demonstrated to be an independent risk factor for stroke, and therefore its investigation and treatment has been recommended for patients with stroke. Mechanisms relating these two clinical disorders include: oxidative stress, cerebral blood flow alterations, autonomic dysfunction, and hypercoagulability, as well as patent foramen ovale, blood pressure, and heart rhythm disorders. Increasing amount of evidence supports continuous airway positive pressure therapy in patients with stroke, but further randomized clinical trials are needed to obtain solid conclusions. This work reviews the literature on epidemiology, pathophysiology, clinical assessment, and treatment of apnea-hypopnea syndrome in patients with stroke.
Sleep apnea and stroke
Abstract
Purpose of review: Stroke and sleep apnea are highly prevalent conditions with a physiologically plausible bidirectional relationship. This review addresses prestroke sleep apnea, wake-up stroke and sleep apnea, and poststroke sleep apnea, with an attempt to highlight research published in the last 18 months.
Recent findings: Sleep apnea is highly prevalent poststroke. Poststroke sleep apnea is associated with worse poststroke functional and cognitive outcomes and a higher risk of recurrent stroke. Physiologic tests are needed to diagnose sleep apnea in poststroke patients as sleep apnea questionnaires do not perform well in this population. The role of CPAP in poststroke management is not yet well established.
Summary: Sleep apnea is a well established independent risk factor for stroke that confers an approximately two-fold increased risk of incident stroke. Sleep apnea is highly prevalent poststroke and is associated with worse outcomes after stroke. Sleep apnea is an attractive target for research addressing secondary stroke prevention and recovery.
Sleep apnea and type 2 diabetes
Abstract
The aim of the present review was to clarify the association between obstructive sleep apnea (OSA) and type 2 diabetes, and discuss the therapeutic role of continuous positive airway pressure (CPAP) in type 2 diabetes. OSA patients are more likely than non-OSA populations to develop type 2 diabetes, while more than half of type 2 diabetes patients suffer from OSA. Similar to Western countries, in the East Asian population, the association between these two disorders has also been reported. CPAP is the primary treatment for OSA, but the effect of CPAP on comorbid diabetes has not been established. CPAP improved glucose metabolism determined by the oral glucose tolerance test in OSA patients, and several studies have shown that CPAP improves insulin resistance, particularly in obese populations undergoing long-term CPAP. Diabetes is associated with other sleep-related manifestations as well, such as snoring and excessive daytime sleepiness. Snoring is associated with the development of diabetes, and excessive daytime sleepiness appears to modify insulin resistance. Well-designed studies are required to clarify the therapeutic effect of CPAP on diabetes. As both diabetes and OSA lead to cardiovascular disease, clinicians and healthcare professionals should be aware of the association between diabetes and OSA, and should take CPAP and health-related behaviors into consideration when treating patients with diabetes and/or OSA.
The Epidemiology of Sleep and Diabetes
Abstract
Purpose of review: To provide an overview of the mechanistic and epidemiologic evidence linking sleep-related exposures, such as short sleep duration, obstructive sleep apnea, shift work, and insomnia, with type 2 diabetes risk in adults.
Recent findings: Both poor sleep habits and sleep disorders are highly prevalent among adults with type 2 diabetes. In observational studies, short sleep duration, obstructive sleep apnea, shift work, and insomnia are all associated with higher risk of incident type 2 diabetes and may predict worse outcomes in those with existing diabetes. However, interventional studies addressing sleep abnormalities in populations with or at high risk for type 2 diabetes are scarce. Although common sleep abnormalities are associated with risk of incident type 2 diabetes and worse prognosis in those with established diabetes, there are few randomized trials evaluating the impact of sleep-focused interventions on diabetes, making it difficult to determine whether the relationship is causal.
Shift work and diabetes--a systematic review
Abstract
Diabetes mellitus is a chronic disease, which has an increasing trend all over the world. Type 2 diabetes constitutes 90% of all diabetes. It is associated with weight gain and insulin resistance. Research during recent years has suggested that shift work could be a risk factor of type 2 diabetes. Since shift work is becoming more common, it could contribute to the increasing trend of diabetes. In this systematic review, we have studied the potential association between shift work and type 2 diabetes. We have also reviewed studies on control of diabetes in relation to shift work.
Untimely oxidative stress in β-cells leads to diabetes - Role of circadian clock in β-cell function
Abstract
Diabetes results from a loss of β-cell function. With the number of people with diabetes reaching epidemic proportions globally, understanding mechanisms that are contributing to this increasing prevalence is critical. One such factor has been circadian disruption, with shift-work, light pollution, jet-lag, increased screen time, all acting as potential contributory factors. Though circadian disruption has been epidemiologically associated with diabetes and other metabolic disorders for many decades, it is only recently that there has been a better understanding of the underlying molecular mechanisms. Experimental circadian disruption, via manipulation of environmental or genetic factors using gene-deletion mouse models, has demonstrated the importance of circadian rhythms in whole body metabolism. Genetic disruption of core clock genes, specifically in the β-cells in mice, have, now demonstrated the importance of the intrinsic β-cell clock in regulating function. Recent work has also shown the interaction of the circadian clock and enhancers in β-cells, indicating a highly integrated regulation of transcription and cellular function by the circadian clock. Disruption of either the whole body or only the β-cell clock leads to significant impairment of mitochondrial function, uncoupling, impaired vesicular transport, oxidative stress in β-cells and finally impaired glucose-stimulated insulin secretion and diabetes. In this review, we explore the role of the circadian clock in mitigating oxidative stress and preserving β-cell function.
Metabolic consequences of sleep and circadian disorders
Abstract
Sleep and circadian rhythms modulate or control daily physiological patterns with importance for normal metabolic health. Sleep deficiencies associated with insufficient sleep schedules, insomnia with short-sleep duration, sleep apnea, narcolepsy, circadian misalignment, shift work, night eating syndrome, and sleep-related eating disorder may all contribute to metabolic dysregulation. Sleep deficiencies and circadian disruption associated with metabolic dysregulation may contribute to weight gain, obesity, and type 2 diabetes potentially by altering timing and amount of food intake, disrupting energy balance, inflammation, impairing glucose tolerance, and insulin sensitivity. Given the rapidly increasing prevalence of metabolic diseases, it is important to recognize the role of sleep and circadian disruption in the development, progression, and morbidity of metabolic disease. Some findings indicate sleep treatments and countermeasures improve metabolic health, but future clinical research investigating prevention and treatment of chronic metabolic disorders through treatment of sleep and circadian disruption is needed.
Circadian System and Glucose Metabolism: Implications for Physiology and Disease
Abstract
The circadian system serves one of the most fundamental properties present in nearly all organisms: it generates 24-h rhythms in behavioral and physiological processes and enables anticipating and adapting to daily environmental changes. Recent studies indicate that the circadian system is important in regulating the daily rhythm in glucose metabolism. Disturbance of this circadian control or of its coordination relative to the environmental/behavioral cycle, such as in shift work, eating late, or due to genetic changes, results in disturbed glucose control and increased type 2 diabetes risk. Therefore, an in-depth understanding of the mechanisms underlying glucose regulation by the circadian system and its disturbance may help in the development of therapeutic interventions against the deleterious health consequences of circadian disruption.
Blood pressure circadian rhythms and adverse outcomes in type 2 diabetes patients diagnosed with orthostatic hypotension
Abstract
Aims/introduction: Patients with diabetes frequently develop orthostatic hypotension (OH). The present study was designed to examine the relationship of blood pressure (BP) circadian rhythms and outcomes in diabetes with OH.
Materials and methods: In the present study, 173 inpatients with type 2 diabetes were enrolled. Patients were divided into an OH group and a non-OH group according to the BP changes detected in the supine and standing position. Then, 24-h ambulatory BP was monitored. Patients were followed up for an average of 45 ± 10 months post-discharge. Outcomes - death and major adverse cardiac and cerebrovascular events, including heart failure, myocardial infarction and stroke - were recorded.
Results: There were 61 patients (35.26%) in the OH group and 112 patients (64.74%) in the non-OH group. In the OH group, the night-time systolic BP and night-time diastolic BP were higher, the blood BP rhythms were predominantly of the riser type (67.21%). OH was as an independent marker of riser type circadian rhythm (adjusted odds ratio 4.532, 95% confidence interval 2.579-7.966). In the OH group, the incidence rates of mortality, and major adverse cardiac and cerebrovascular events were increased significantly compared with those in the non-OH group (11.48 vs 2.68%, P = 0.014; 37.70 vs 8.93%, P < 0.01).
Conclusions: In patients who had type 2 diabetes diagnosed with OH, the BP circadian rhythm usually showed riser patterns, and they had increased rates of mortality, and major adverse cardiac and cerebrovascular events.
Rotating night shift work and adherence to unhealthy lifestyle in predicting risk of type 2 diabetes: results from two large US cohorts of female nurses
Abstract
Objectives: To prospectively evaluate the joint association of duration of rotating night shift work and lifestyle factors with risk of type 2 diabetes risk, and to quantitatively decompose this joint association to rotating night shift work only, to lifestyle only, and to their interaction.
Design: Prospective cohort study.
Setting: Nurses' Health Study (1988-2012) and Nurses' Health Study II (1991-2013).
Participants: 143 410 women without type 2 diabetes, cardiovascular disease, or cancer at baseline.
Exposures: Rotating night shift work was defined as at least three night shifts per month in addition to day and evening shifts in that month. Unhealthy lifestyles included current smoking, physical activity levels below 30 minutes per day at moderate to vigorous intensity, diet in the bottom three fifths of the Alternate Healthy Eating Index score, and body mass index of 25 or above.
Main outcome measures: Incident cases of type 2 diabetes were identified through self report and validated by a supplementary questionnaire.
Results: During 22-24 years of follow-up, 10 915 cases of incident type 2 diabetes occurred. The multivariable adjusted hazard ratios for type 2 diabetes were 1.31 (95% confidence interval 1.19 to 1.44) per five year increment of duration of rotating night shift work and 2.30 (1.88 to 2.83) per unhealthy lifestyle factor (ever smoking, low diet quality, low physical activity, and overweight or obesity). For the joint association of per five year increment rotating night shift work and per unhealthy lifestyle factor with type 2 diabetes, the hazard ratio was 2.83 (2.15 to 3.73) with a significant additive interaction (P for interaction <0.001). The proportions of the joint association were 17.1% (14.0% to 20.8%) for rotating night shift work alone, 71.2% (66.9% to 75.8%) for unhealthy lifestyle alone, and 11.3% (7.3% to 17.3%) for their additive interaction.
Conclusions: Among female nurses, both rotating night shift work and unhealthy lifestyle were associated with a higher risk of type 2 diabetes. The excess risk of rotating night shift work combined with unhealthy lifestyle was higher than the addition of risk associated with each individual factor. These findings suggest that most cases of type 2 diabetes could be prevented by adhering to a healthy lifestyle, and the benefits could be greater in rotating night shift workers.
Inadequate sleep as a contributor to type 2 diabetes in children and adolescents
Abstract
Lack of sleep is a modifiable risk factor for adverse health in humans. Short sleep duration and poor sleep quality are common in the pediatric population; the largest decline in sleep duration over the past decades has been seen in children and adolescents. The objective of the present narrative review was to provide for the first time an overview of the literature on sleep and its association with type 2 diabetes mellitus (T2D) biomarkers in children and adolescents. For this narrative review, 23 studies were retained (21 observational and 2 experimental studies). Notwithstanding the conflicting results found in these studies and despite being attenuated by adiposity level, maturity, sex and age, there is still some compelling evidence for an association between sleep duration (for both objective or subjective measurements of duration) and architecture with one or more T2D biomarkers in children and adolescents. The majority of the studies reviewed did focus on sleep duration and one or more T2D biomarkers in children and adolescents, but sleep architecture, more precisely the suppression of slow wave sleep and rapid eye movement sleep, has also been shown to be associated with insulin resistance. Only two studies looked at sleep quality, and the association between sleep quality and insulin resistance was not independent of level of adiposity. Future experimental studies will help to better understand the mechanisms linking insufficient sleep with T2D. Work also needs to be carried out on finding novel and effective strategies aimed at improving sleep hygiene and health outcomes of children and adolescents.
Sleep Quality and Nocturnal Sleep Duration in Pregnancy and Risk of Gestational Diabetes Mellitus
Abstract
Study objectives: To examine the influence of maternal sleep quality and nocturnal sleep duration on risk of gestational diabetes mellitus (GDM) in a multiethnic Asian population.
Methods: A cohort of 686 women (376 Chinese, 186 Malay, and 124 Indian) with a singleton pregnancy attended a clinic visit at 26-28 weeks of gestation as part of the Growing Up in Singapore Towards healthy Outcomes mother-offspring cohort study. Self-reported sleep quality and sleep duration were assessed using the Pittsburgh Sleep Quality Index (PSQI). GDM was diagnosed based on a 75-g oral glucose tolerance test administered after an overnight fast (1999 WHO criteria). Multiple logistic regression was used to model separately the associations of poor sleep quality (PSQI score > 5) and short nocturnal sleep duration (<6 h) with GDM, adjusting for age, ethnicity, maternal education, body mass index, previous history of GDM, and anxiety (State-Trait Anxiety Inventory score).
Results: In the cohort 296 women (43.1%) had poor sleep quality and 77 women (11.2%) were categorized as short sleepers; 131 women (19.1%) were diagnosed with GDM. Poor sleep quality and short nocturnal sleep duration were independently associated with increased risk of GDM (poor sleep, adjusted odds ratio [OR] = 1.75, 95% confidence interval [CI] 1.11 to 2.76; short sleep, adjusted OR = 1.96, 95% CI 1.05 to 3.66).
Conclusions: During pregnancy, Asian women with poor sleep quality or short nocturnal sleep duration exhibited abnormal glucose regulation. Treating sleep problems and improving sleep behavior in pregnancy could potentially reduce the risk and burden of GDM.
Abstract
Purpose of review: To highlight the adverse metabolic effects of sleep disruption and to open ground for research aimed at preventive measures. This area of research is especially relevant given the increasing prevalence of voluntary sleep curtailment, sleep disorders, diabetes, and obesity.
Recent findings: Epidemiological studies have established an association between decreased self-reported sleep duration and an increased incidence of type 2 diabetes (T2D), obesity, and cardiovascular disease. Experimental laboratory studies have demonstrated that decreasing either the amount or quality of sleep decreases insulin sensitivity and decreases glucose tolerance. Experimental sleep restriction also causes physiological and behavioral changes that promote a positive energy balance. Although sleep restriction increases energy expenditure because of increased wakefulness, it can lead to a disproportionate increase in food intake, decrease in physical activity, and weight gain.
Summary: Sleep disruption has detrimental effects on metabolic health. These insights may help in the development of new preventive and therapeutic approaches against obesity and T2D based on increasing the quality and/or quantity of sleep.
The impact of sleep amount and sleep quality on glycemic control in type 2 diabetes: A systematic review and meta-analysis
Abstract
Recent epidemiological studies have suggested that there is an association between glycemic control and sleep disturbances in patients with type 2 diabetes, but the extent is unclear. A systematic literature search was performed in nine electronic databases from inception until August 2015 without any language restriction. The search identified 20 studies (eight studies reporting duration of sleep and 15 studies evaluating sleep quality), and 15 were included in the meta-analysis. Short and long sleep durations were associated with an increased hemoglobin A1c (HbA1c) (weighted mean difference (WMD): 0.23% [0.10-0.36], short sleep; WMD: 0.13% [0.02-0.25], long sleep) compared to normal sleep, suggesting a U-shaped dose-response relationship. Similarly, poor sleep quality was associated with an increased HbA1c (WMD: 0.35% [0.12-0.58]). Results of this study suggest that amount of sleep as well as quality of sleep is important in the metabolic function of type 2 diabetes patients. Further studies are needed to identify for the potential causal role between sleep and altered glucose metabolism.
Sleep habits and diabetes
Abstract
Sleep duration has been constantly decreasing over the past 50 years. Short sleep duration, sleep quality and, recently, long sleep duration have all been linked to poor health outcomes, increasing the risk of developing metabolic diseases and cardiovascular events. Beyond the duration of sleep, the timing of sleep may also have consequences. Having a tendency to go early to bed (early chronotype) compared with the habit of going to bed later (late chronotype) can interfere considerably with social schedules (school, work). Eventually, a misalignment arises in sleep timing between work days and free days that has been described as 'social jet lag'. The present review looks at how different sleep habits can interfere with diabetes, excluding sleep breathing disorders, and successively looks at the effects of sleep duration, chronotype and social jet lag on the risk of developing diabetes as well as on the metabolic control of both type 1 and type 2 diabetes. Finally, this review addresses the current state of knowledge of physiological mechanisms that could be linking sleep habits and metabolic health.
Short Sleep Duration and Poor Sleep Quality Increase the Risk of Diabetes in Japanese Workers With No Family History of Diabetes
Abstract
OBJECTIVE To investigate whether a difference in the risk for diabetes exists in Japanese workers with regard to sleep duration/quality and the presence or absence of a family history of diabetes (FHD).
RESEARCH DESIGN AND METHODS The researchers conducted a prospective, occupational-based study of local government employees in Sapporo, Japan. Between April 2003 and March 2004, 3,570 nondiabetic participants, aged 35–55 years, underwent annual health checkups and completed a self-administered questionnaire that included information on sleep duration/quality and FHD at baseline. Having diabetes was defined as taking medication for diabetes or a fasting plasma glucose level of ≥126 mg/dL at follow-up (2007–2008).
RESULTS A total of 121 (3.4%) new cases of diabetes were reported. In multivariate logistic regression models of workers without an FHD, and after adjustment for potential confounding factors, the odds ratio (95% CI) for developing diabetes was 5.37 (1.38–20.91) in those with a sleep duration of ≤5 h compared with those with a sleep duration of >7 h. Other risk factors were awakening during the night (5.03 [1.43–17.64]), self-perceived insufficient sleep duration (6.76 [2.09–21.87]), and unsatisfactory overall quality of sleep (3.71 [1.37–10.07]). In subjects with an FHD, these associations were either absent or weaker.
CONCLUSIONS The current study shows that poor sleep is associated with a higher risk of developing diabetes in workers without an FHD. Promoting healthy sleeping habits may be effective for preventing the development of diabetes in people without an FHD.
Metabolic effects of sleep disruption, links to obesity and diabetes
Abstract
Purpose of the review
To highlight the adverse metabolic effects of sleep disruption and to open ground for research aimed at preventive measures. This area of research is especially relevant given the increasing prevalence of voluntary sleep curtailment, sleep disorders, diabetes, and obesity.
Resent findings
Epidemiological studies have established an association between decreased self-reported sleep duration and an increased incidence of type 2 diabetes (T2D), obesity, and cardiovascular disease. Experimental laboratory studies have demonstrated that decreasing either the amount or quality of sleep decreases insulin sensitivity and decreases glucose tolerance. Experimental sleep restriction also causes physiological and behavioral changes that promote a positive energy balance. While sleep restriction increases energy expenditure due to increased wakefulness, it can lead to a disproportionate increase in food intake, decrease in physical activity, and weight gain.
Summary
Sleep disruption has detrimental effects on metabolic health. These insights may help in the development of new preventative and therapeutic approaches against obesity and T2D based on increasing the quality and/or quantity of sleep.
Sleep disturbances compared to traditional risk factors for diabetes development: Systematic review and meta-analysis
Summary
Sleep disturbances [short (<6 h) and long (>8 h) sleeping time, insomnia (initiating or maintaining sleep),
obstructive sleep apnea
(OSA) and abnormal sleep timing] have been associated with increased diabetes risk but the effect size relative to that of traditional risk factors is unknown. We conducted a systematic review and meta-analysis to compare the risk associated with sleep disturbances to traditional risk factors. Studies were identified from Medline and Scopus.
Cohort studies
measuring the association between sleep disturbances and incident diabetes were eligible. For traditional risk factors (i.e., overweight, family history, and physical inactivity), systematic reviews with or without meta-analysis were included. Thirty-six studies (1,061,555 participants) were included. Pooled relative risks (RRs) of sleep variables were estimated using a random-effect model. Pooled RRs of sleeping ≤5 h, 6 h, and ≥9 h/d were respectively 1.48 (95%CI:1.25,1.76), 1.18 (1.10,1.26) and 1.36 (1.12,1.65). Poor sleep quality, OSA and shift work were associated with diabetes with a pooled RR of 1.40 (1.21,1.63), 2.02 (1.57, 2.61) and 1.40 (1.18,1.66), respectively. The pooled RRs of being overweight, having a family history of diabetes, and being physically inactive were 2.99 (2.42,3.72), 2.33 (1.79,2.79), and 1.20 (1.11,1.32), respectively. In conclusion, the risk of developing diabetes associated with sleep disturbances is comparable to that of traditional risk factors. Sleep disturbances should be considered in clinical guidelines for type 2 diabetes screening.
Sleep in adolescents and young adults with type 1 diabetes: associations with diabetes management and glycemic control
ABSTRACT
Objective: To describe sleep in adolescents and young adults with type 1 diabetes (T1D) and explore the association between sleep disturbances, diabetes management and glycemic control. Methods: Adolescents with T1D (n = 159, mean age = 16.4, 43% female, 69% white, mean hemoglobin A1c = 9.3%) completed the Pittsburgh Sleep Quality Index to assess sleep quantity and quality and sleep disturbances. Frequency of blood glucose monitoring (meter downloads) was used as a measure of diabetes management. Results: Average sleep duration was 7.4 hours, below the recommended duration for this age. Adolescents using insulin pumps reported fewer sleep disturbances and longer sleep duration than those on injections, and older adolescents reported less sleep than younger adolescents. Poorer sleep duration was related to poorer diabetes management, and better self-reported sleep quality was associated with better glycemic control for males but not for females. Conclusions: Assessing for and treating sleep disturbances in adolescents may improve diabetes management.
Quantity and Quality of Sleep and Incidence of Type 2 Diabetes
OBJECTIVE To assess the relationship between habitual sleep disturbances and the incidence of type 2 diabetes and to obtain an estimate of the risk.
RESEARCH DESIGN AND METHODS We conducted a systematic search of publications using MEDLINE (1955–April 2009), EMBASE, and the Cochrane Library and manual searches without language restrictions. We included studies if they were prospective with follow-up >3 years and had an assessment of sleep disturbances at baseline and incidence of type 2 diabetes. We recorded several characteristics for each study. We extracted quantity and quality of sleep, how they were assessed, and incident cases defined with different validated methods. We extracted relative risks (RRs) and 95% CI and pooled them using random-effects models. We performed sensitivity analysis and assessed heterogeneity and publication bias.
RESULTS We included 10 studies (13 independent cohort samples; 107,756 male and female participants, follow-up range 4.2–32 years, and 3,586 incident cases of type 2 diabetes). In pooled analyses, quantity and quality of sleep predicted the risk of development of type 2 diabetes. For short duration of sleep (≤5–6 h/night), the RR was 1.28 (95% CI 1.03–1.60, P = 0.024, heterogeneity P = 0.015); for long duration of sleep (>8–9 h/night), the RR was 1.48 (1.13–1.96, P = 0.005); for difficulty in initiating sleep, the RR was 1.57 (1.25–1.97, P < 0.0001); and for difficulty in maintaining sleep, the RR was 1.84 (1.39–2.43, P < 0.0001).
CONCLUSIONS Quantity and quality of sleep consistently and significantly predict the risk of the development of type 2 diabetes. The mechanisms underlying this relation may differ between short and long sleepers.
Sleep and Diabetes
Abstract
Sleep apnea is clinically recognized as a heterogeneous group of disorders characterized by recurrent apnea and/or hypopnea. Its prevalence ranges from 4% to 24%. It has been implicated as an independent risk factor for several conditions such as hypertension, stroke, arrhythmia, and myocardial infarction. Recently data has been emerging which suggests an independent association of obstructive sleep apnea with several components of the metabolic syndrome, particularly insulin resistance and abnormalities in lipid metabolism. We hereby review the salient features of the association between sleep and diabetes.
Sleep Duration as a Risk Factor for Incident Type 2 Diabetes in a Multiethnic Cohort
Purpose
We evaluated the association between sleep duration and type 2 diabetes in a multiethnic cohort, considering
insulin sensitivity
(SI) and secretion (acute
insulin response
[AIR]), two important diabetes risk factors.
Methods
Among 900 diabetes-free persons, 146 developed incident type 2 diabetes. At baseline, sleep duration was assessed by self-report and SI and AIR by a frequently sampled
intravenous glucose tolerance test
.
Results
Among non-Hispanic whites and Hispanics, short sleep (≤7 hours: odds ratio [OR] 2.36; 95% confidence interval [CI] 1.21–3.79 compared to 8 hours) was associated with increased odds of diabetes, adjusting for age, sex,
glucose tolerance
, clinical site, hypertension, family history of diabetes, smoking, education, and
body mass index
. Adjustment for SI and AIR did not affect short sleep (2.36; 1.11–5.00), but further attenuated the already non-significant association with long sleep (2.15; 0.50–9.30). In African Americans, an opposing pattern was observed, but none of the associations reached statistical significance.
Conclusion
Our study supports the role of short sleep as an independent risk factor for type 2 diabetes in whites and Hispanics. While
insulin sensitivity and secretion
may explain previously reported associations of long sleep duration with diabetes risk, they do not seem to mediate the effects of short sleep on diabetes.
Does lack of sleep cause diabetes?
Abstract
Several lines of evidence indicate that chronic lack of sleep may contribute to the risk of type 2 diabetes mellitus. Adequate sleep and good sleep hygiene should be included among the goals of a healthy lifestyle, especially for patients with diabetes. We urge clinicians to recommend at least 7 hours of uninterrupted sleep per night as part of a healthy lifestyle.
Night Shift Work, Genetic Risk, and Type 2 Diabetes in the UK Biobank
Abstract
OBJECTIVE To examine the effects of past and current night shift work and genetic type 2 diabetes vulnerability on type 2 diabetes odds.
RESEARCH DESIGN AND METHODS In the UK Biobank, we examined associations of current (N = 272,214) and lifetime (N = 70,480) night shift work exposure with type 2 diabetes risk (6,770 and 1,191 prevalent cases, respectively). For 180,704 and 44,141 unrelated participants of European ancestry (4,002 and 726 cases, respectively) with genetic data, we assessed whether shift work exposure modified the relationship between a genetic risk score (comprising 110 single-nucleotide polymorphisms) for type 2 diabetes and prevalent diabetes.
RESULTS Compared with day workers, all current night shift workers were at higher multivariable-adjusted odds for type 2 diabetes (none or rare night shifts: odds ratio [OR] 1.15 [95% CI 1.05–1.26]; some nights: OR 1.18 [95% CI 1.05–1.32]; and usual nights: OR 1.44 [95% CI 1.19–1.73]), except current permanent night shift workers (OR 1.09 [95% CI 0.93–1.27]). Considering a person’s lifetime work schedule and compared with never shift workers, working more night shifts per month was associated with higher type 2 diabetes odds (<3/month: OR 1.24 [95% CI 0.90–1.68]; 3–8/month: OR 1.11 [95% CI 0.90–1.37]; and >8/month: OR 1.36 [95% CI 1.14–1.62]; Ptrend = 0.001). The association between genetic type 2 diabetes predisposition and type 2 diabetes odds was not modified by shift work exposure.
CONCLUSIONS Our findings show that night shift work, especially rotating shift work including night shifts, is associated with higher type 2 diabetes odds and that the number of night shifts worked per month appears most relevant for type 2 diabetes odds. Also, shift work exposure does not modify genetic risk for type 2 diabetes, a novel finding that warrants replication.
Sleep Duration and Risk of Type 2 Diabetes
Abstract
BACKGROUND: Associations between sleep duration and type 2 diabetes (T2D) risk markers in childhood have been little studied. We examined associations between self-reported sleep duration and T2D risk markers in children.
METHODS: Cross-sectional study of 4525 multiethnic UK children aged 9 to 10 years. Sleep time was calculated from self-reported usual time of going to bed and getting up on a school day, validated in a subset using accelerometers. Fasting blood samples provided levels of serum lipids and insulin, plasma glucose, and HbA1c. Physical measures included height, weight, bioimpedance, and blood pressure. Multilevel linear regression models of anthropometric, T2D, and cardiovascular risk markers with sleep duration were adjusted for sex, age, month, ethnicity, socioeconomic position, observer (physical measures only), and random effect of school.
RESULTS: On average, children slept 10.5 hours per night (95% range 8.0–12.0 hours). There were strong inverse graded relationships between sleep duration, adiposity, and diabetes risk markers. In adjusted models, a 1-hour-longer sleep duration was associated with 0.19 lower BMI (95% confidence interval [CI] 0.09 to 0.28), 0.03 kg/m5 lower fat mass index (95% CI 0.00 to 0.05 kg/m5), 2.9% lower homeostasis model assessment insulin resistance (95% CI 1.2% to 4.4%), and 0.24% lower fasting glucose (95% CI 0.03% to 0.44%); there was no association with HbA1c or cardiovascular risk. Associations with insulin and glucose remained after an additional adjustment for adiposity markers.
CONCLUSIONS: The finding of an inverse association between sleep duration and T2D risk markers in childhood is novel. Intervention studies are needed to establish the causality of these associations, which could provide a simple strategy for early T2D prevention.
Cardiovascular Disease
Role of the circadian system in cardiovascular disease
Abstract
All species organize behaviors to optimally match daily changes in the environment, leading to pronounced activity/rest cycles that track the light/dark cycle. Endogenous, approximately 24-hour circadian rhythms in the brain, autonomic nervous system, heart, and vasculature prepare the cardiovascular system for optimal function during these anticipated behavioral cycles. Cardiovascular circadian rhythms, however, may be a double-edged sword. The normal amplified responses in the morning may aid the transition from sleep to activity, but such exaggerated responses are potentially perilous in individuals susceptible to adverse cardiovascular events. Indeed, the occurrence of stroke, myocardial infarction, and sudden cardiac death all have daily patterns, striking most frequently in the morning. Furthermore, chronic disruptions of the circadian clock, as with night-shift work, contribute to increased cardiovascular risk. Here we highlight the importance of the circadian system to normal cardiovascular function and to cardiovascular disease, and identify opportunities for optimizing timing of medications in cardiovascular disease.
Self-Reported Sleep Duration and Quality and Cardiovascular Disease and Mortality: A Dose-Response Meta-Analysis
Abstract
Background There is growing evidence that sleep duration and quality may be associated with cardiovascular harm and mortality. Methods and Results We conducted a systematic review, meta-analysis, and spline analysis of prospective cohort studies that evaluate the association between sleep duration and quality and cardiovascular outcomes. We searched MEDLINE and EMBASE for these studies and extracted data from identified studies. We utilized linear and nonlinear dose-response meta-analysis models and used DerSimonian-Laird random-effects meta-analysis models of risk ratios, with inverse variance weighting, and the I2 statistic to quantify heterogeneity. Seventy-four studies including 3 340 684 participants with 242 240 deaths among 2 564 029 participants who reported death events were reviewed. Findings were broadly similar across both linear and nonlinear dose-response models in 30 studies with >1 000 000 participants, and we report results from the linear model. Self-reported duration of sleep >8 hours was associated with a moderate increased risk of all-cause mortality, with risk ratio , 1.14 (1.05-1.25) for 9 hours, risk ratio, 1.30 (1.19-1.42) for 10 hours, and risk ratio, 1.47 (1.33-1.64) for 11 hours. No significant difference was identified for periods of self-reported sleep <7 hours, whereas similar patterns were observed for stroke and cardiovascular disease mortality. Subjective poor sleep quality was associated with coronary heart disease (risk ratio , 1.44; 95% confidence interval, 1.09-1.90), but no difference in mortality and other outcomes. Conclusions Divergence from the recommended 7 to 8 hours of sleep is associated with a higher risk of mortality and cardiovascular events. Longer duration of sleep may be more associated with adverse outcomes compared with shorter sleep durations.
Obstructive Sleep Apnea during REM Sleep and Cardiovascular Disease
Abstract
Rationale: Obstructive sleep apnea (OSA) during REM sleep is a common disorder. Data on whether OSA that occurs predominantly during REM sleep is associated with health outcomes are limited.
Objectives: The present study examined the association between OSA during REM sleep and a composite cardiovascular endpoint in a community sample with and without prevalent cardiovascular disease.
Methods: Full-montage home polysomnography was conducted as part of the Sleep Heart Health Study. The study cohort was followed for an average of 9.5 years, during which time cardiovascular events were assessed. Only participants with a non-REM apnea-hypopnea index (AHI) of less than 5 events/h were included. A composite cardiovascular endpoint was determined as the occurrence of nonfatal or fatal events, including myocardial infarction, coronary artery revascularization, congestive heart failure, and stroke. Proportional hazards regression was used to derive the adjusted hazards ratios for the composite cardiovascular endpoint.
Measurements and main results: The sample consisted of 3,265 subjects with a non-REM AHI of less than 5.0 events/h. Using a REM AHI of less than 5.0 events/h as the reference group (n = 1,758), the adjusted hazards ratios for the composite cardiovascular endpoint in those with severe REM OSA (≥30 events/h; n = 180) was 1.35 (95% confidence interval, 0.98-1.85). Stratified analyses demonstrated that the association was most notable in those with prevalent cardiovascular disease and severe OSA during REM sleep with an adjusted hazards ratio of 2.56 (95% confidence interval, 1.46-4.47).
Conclusions: Severe OSA that occurs primarily during REM sleep is associated with higher incidence of a composite cardiovascular endpoint, but in only those with prevalent cardiovascular disease.
The Effects of Insomnia and Sleep Loss on Cardiovascular Disease
Abstract
Sleep loss has negative impacts on quality of life, mood, cognitive function, and heath. Insomnia is linked to poor mood, increased use of health care resources, decreased quality of life, and possibly cardiovascular risk factors and disease. Studies have shown increase in cortisol levels, decreased immunity, and increased markers of sympathetic activity in sleep-deprived healthy subjects and those with chronic insomnia. The literature shows subjective complaints consistent with chronic insomnia and shortened sleep can be associated with development of diabetes, hypertension, and cardiovascular disease. This article explores the relationship between insufficient sleep and insomnia with these health conditions.
Sleep Apnea and Cardiovascular Disease: Lessons From Recent Trials and Need for Team Science
Abstract
Emerging research highlights the complex interrelationships between sleep-disordered breathing and cardiovascular disease, presenting clinical and research opportunities as well as challenges. Patients presenting to cardiology clinics have a high prevalence of obstructive and central sleep apnea associated with Cheyne-Stokes respiration. Multiple mechanisms have been identified by which sleep disturbances adversely affect cardiovascular structure and function. Epidemiological research indicates that obstructive sleep apnea is associated with increases in the incidence and progression of coronary heart disease, heart failure, stroke, and atrial fibrillation. Central sleep apnea associated with Cheyne-Stokes respiration predicts incident heart failure and atrial fibrillation; among patients with heart failure, it strongly predicts mortality. Thus, a strong literature provides the mechanistic and empirical bases for considering obstructive sleep apnea and central sleep apnea associated with Cheyne-Stokes respiration as potentially modifiable risk factors for cardiovascular disease. Data from small trials provide evidence that treatment of obstructive sleep apnea with continuous positive airway pressure improves not only patient-reported outcomes such as sleepiness, quality of life, and mood but also intermediate cardiovascular end points such as blood pressure, cardiac ejection fraction, vascular parameters, and arrhythmias. However, data from large-scale randomized controlled trials do not currently support a role for positive pressure therapies for reducing cardiovascular mortality. The results of 2 recent large randomized controlled trials, published in 2015 and 2016, raise questions about the effectiveness of pressure therapies in reducing clinical end points, although 1 trial supported the beneficial effect of continuous positive airway pressure on quality of life, mood, and work absenteeism. This review provides a contextual framework for interpreting the results of recent studies, key clinical messages, and suggestions for future sleep and cardiovascular research, which include further consideration of individual risk factors, use of existing and new multimodality therapies that also address adherence, and implementation of trials that are sufficiently powered to target end points and to support subgroup analyses. These goals may best be addressed through strengthening collaboration among the cardiology, sleep medicine, and clinical trial communities.
Sleep, sleep deprivation, autonomic nervous system and cardiovascular diseases
Abstract
Sleep deprivation (SD) has become a relevant health problem in modern societies. We can be sleep deprived due to lifestyle habits or due to sleep disorders, such as insomnia, obstructive sleep apnea (OSA) and neurological disorders. One of the common element of sleep disorders is the condition of chronic SD, which has complex biological consequences. SD is capable of inducing different biological effects, such as neural autonomic control changes, increased oxidative stress, altered inflammatory and coagulatory responses and accelerated atherosclerosis. All these mechanisms links SD and cardiovascular and metabolic disorders. Epidemiological studies have shown that short sleep duration is associated with increased incidence of cardiovascular diseases, such as coronary artery disease, hypertension, arrhythmias, diabetes and obesity, after adjustment for socioeconomic and demographic risk factors and comorbidities. Thus, an early assessment of a condition of SD and its treatment is clinically relevant to prevent the harmful consequences of a very common condition in adult population.
Roles of sleep deprivation in cardiovascular dysfunctions
Abstract
It is widely recognized that inadequate sleep is associated with multiple acute and chronic diseases and results in increased mortality and morbidity for cardiovascular diseases. In recent years, there has been increasing interest in sleep related investigations. Emerging evidence indicates that sleep deprivation changes the biological phenotypes of DNA, RNA and protein levels, but the underlying mechanisms are not clear. We summarized the current research on the detrimental roles of sleep deprivation on the heart and elucidated the underlying mechanisms of sleep deficiency to improve our understanding of sleep deprivation and the emerging strategies to target this process for therapeutic benefit.
Evidence of reduced parasympathetic autonomic regulation in inflammatory joint disease: A meta-analyses study
Abstract
Background: Rheumatoid arthritis (RA) and spondyloarthritis (SpA) are inflammatory joint disorders (IJD) with increased risk of cardiovascular disease (CVD). Autonomic dysfunction (AD) is a risk factor for CVD, and parasympathetic AD is linked to key features of IJD such as inflammation, physical inactivity and pain. Heart-rate variability (HRV) is a marker of cardiac AD. The study objective was to compare parasympathetic cardiac AD, measured by HRV, between patients with IJD and healthy controls, using meta-analysis methodology, and to examine the impact of inflammation, physical inactivity and pain on HRV in IJD.
Methods: Medline, Embase and Amed were searched. Inclusion criteria were adult case-control studies published in English or a Scandinavian language, presenting HRV data in IJD. Two measures of HRV and 3 from the Ewing protocol were selected: square root of mean squared difference of successive R-R intervals (RMSSD), high frequency (HF), Ewing protocol; standing (E-S), breathing (E-B) and Valsalva (E-V). Patients with RA, SpA and healthy controls were compared separately using random-effects meta-analyses of standardized mean differences (SMD).
Results: In all, 35 papers were eligible for inclusion. For RMSSD the pooled SMD (95% CI) RA vs. controls was -0.90 (-1.35 to -0.44), for SpA vs. controls; -0.34 (-0.73 to 0.06). For HF pooled SMD RA vs. controls was -0.78 (-0.99 to -0.57), for SpA vs. controls; -0.04 (-0.22 to 0.13). All Ewing parameters were significantly lower in cases, except for E-V which was comparable between cases and controls in patients with RA.
Conclusion: Patients with IJD have cardiac parasympathetic AD which is related to inflammation.
Insomnia with objective short sleep duration and risk of incident cardiovascular disease and all-cause mortality: Sleep Heart Health Study
Abstract
Study objectives: To quantify the association between insomnia or poor sleep with objective short sleep duration and incident cardiovascular disease (CVD) and mortality in the general population.
Methods: We conducted a time-to-event analysis of Sleep Heart Health Study data. Questionnaires and at-home polysomnography (PSG) were performed between 1994 and 1998. Participants were followed for a median of 11.4 years (Q1-Q3, 8.8-12.4 years) until death or last contact. The primary exposure was insomnia or poor sleep with short sleep defined as follows: difficulty falling asleep, difficulty returning to sleep, early morning awakenings, or sleeping pill use, 16-30 nights per month; and total sleep of <6 hr on PSG. We used proportional hazard models to estimate the association between insomnia or poor sleep with short sleep and CVD, as well as all-cause mortality.
Results: Among 4994 participants (mean age: 64.0 ± 11.1 years), 14.1 per cent reported insomnia or poor sleep, of which 50.3 per cent slept <6 hr. Among 4437 CVD-free participants at baseline, we observed 818 incident CVD events. After propensity adjustment, there was a 29 per cent higher risk of incident CVD in the insomnia or poor sleep with short sleep group compared with the reference group (HR: 1.29, 95% CI: 1.00, 1.66), but neither the insomnia or poor sleep only nor short sleep only groups were associated with higher incident CVD. Insomnia or poor sleep with objective short sleep was not associated with all-cause mortality (HR: 1.07, 95% CI: 0.86, 1.33).
Sleep Disordered Breathing and Cardiovascular Diseases
Abstract
Sleep disordered breathing (SDB), which causes sleep deprivation, intermittent hypoxia, and negative intrathoracic pressure swings, can be accompanied by other harmful pathophysiologies relating to cardiovascular diseases (CVD), including sudden death, atrial fibrillation, stroke, and coronary artery disease leading to heart failure. Continuous positive airway pressure (CPAP) therapy for SDB has been reported to provide favorable effects such as lowered systemic blood pressure and improved endothelial function. However, in recent randomized controlled trials, CPAP has failed to demonstrate its beneficial prognostic impact on the primary or secondary setting of CVD. In this review article, we describe the characteristics of SDB complicated with CVD, the prognostic impacts of SDB in CVD, and the beneficial effects of CPAP on CVD.
The contribution of sleep to social inequalities in cardiovascular disorders: a multi-cohort study
Abstract
Aims: Sleep disturbances exhibit a strong social patterning, and inadequate sleep has been associated with adverse health outcomes, including cardiovascular disorders (CVD). However, the contribution of sleep to socioeconomic inequalities in CVD is unclear. This study pools data from eight European cohorts to investigate the role of sleep duration in the association between life-course socioeconomic status (SES) and CVD.
Methods and results: We used cross-sectional data from eight European cohorts, totalling 111 205 participants. Life-course SES was assessed using father's and adult occupational position. Self-reported sleep duration was categorized into recommended (6-8.5 h/night), long (>8.5 h/night), and short (<6 h/night). We examined two cardiovascular outcomes: coronary heart disease (CHD) and stroke. Main analyses were conducted using pooled data and examined the association between life-course SES and CVD, and the contribution of sleep duration to this gradient using counterfactual mediation. Low father's occupational position was associated with an increased risk of CHD (men: OR = 1.19, 95% CI [1.04; 1.37]; women: OR = 1.25, 95% CI [1.02; 1.54]), with marginal decrease of the gradient after accounting for adult occupational position (men: OR = 1.17, 95% CI [1.02; 1.35]; women: OR = 1.22, 95% CI [0.99; 1.52]), and no mediating effect by short sleep duration. Low adult occupational position was associated with an increased risk of CHD in both men and women (men: OR = 1.48, 95% CI [1.14; 1.92]; women: OR = 1.53, 95% CI [1.04; 2.21]). Short sleep duration meaningfully contributed to the association between adult occupational position and CHD in men, with 13.4% mediation. Stroke did not exhibit a social patterning with any of the variables examined.
Conclusion: This study suggests that inadequate sleep accounts to a meaningful proportion of the association between adult occupational position and CHD, at least in men. With sleep increasingly being considered an important cardiovascular risk factor in its own terms, our study additionally points to its potential role in social inequalities in cardiovascular disease.
Epidemiology of Sleep Disturbances and Cardiovascular Consequences
Abstract
It is increasingly recognized that disruption of sleep and reduced amounts of sleep can have significant adverse cardiovascular consequences. For example, obstructive sleep apnea (OSA) is a common underdiagnosed disorder characterized by recurrent nocturnal asphyxia resulting from repetitive collapse of the upper airway; this leads to repetitive episodes of nocturnal hypoxemia and arousal from sleep. Risk factors for disease include obesity, increased age, male sex, and family history. In epidemiologic studies, OSA appears to be an independent risk factor for cardiovascular disease (CVD), and treatment is associated with better outcomes. Habitual short sleep duration is common in today's society. In epidemiologic studies, short sleep duration is associated with a number of adverse health effects, including all-cause mortality, weight gain, and incident CVD. Given the links between sleep disorders and adverse health outcomes, obtaining adequate quality and amounts of sleep should be considered a component of a healthy lifestyle, similar to good diet and exercise.
Benefits of Community-Based Approaches in Assessing and Addressing Sleep Health and Sleep-Related Cardiovascular Disease Risk: a Precision and Personalized Population Health Approach
Abstract
Purpose of review: In this current review, we describe the benefits of community-based and "precision and personalized population health" (P3H) approaches to assessing and addressing sleep health problems and sleep-related cardiovascular diseases (CVD) among vulnerable populations such as racial/ethnic minorities, the elderly, and the socioeconomically disadvantaged.
Recent findings: Very few sleep health programs utilize a community-based or P3H approach, which may account for low estimates of sleep health problems, related CVD outcomes, and inadequate healthcare infrastructure to address sleep-related health outcomes at the community and population level. We describe community-based and P3H approaches and programs as solutions to accurately capture estimates of sleep health and reduce burden of sleep health problems and corollary CVD outcomes at the level of the community and population. Specifically, we describe seven critical steps needed to successfully implement a community-based and P3H approach to address sleep health problems. Community-based and P3H approaches are effective strategies to assessing and addressing sleep health problems and related health conditions.
Association of sleep characteristics with cardiovascular health among women and differences by race/ethnicity and menopausal status: findings from the American Heart Association Go Red for Women Strategically Focused Research Network
Abstract
Background and objective: Sleep is an emerging risk factor for cardiovascular disease (CVD) that is not currently included as a cardiovascular health (CVH) metric in the American Heart Association's Life's Simple 7 (AHA LS7). Our objective was to evaluate the association of sleep with CVH in women and examine differences by menopausal status and race/ethnicity.
Methods: Baseline data from the Columbia University AHA Go Red for Women Strategically Focused Research Network were examined. Sleep habits were self-reported using validated questionnaires. A CVH score was computed using AHA LS7 criteria for smoking, diet, physical activity, BMI, blood pressure(BP), total cholesterol, and fasting glucose. Women received a score of 2 (ideal), 1 (intermediate), or 0 (poor) based on their level of meeting each AHA LS7 metric. Multivariable-adjusted regression models were used to evaluate associations of sleep with meeting overall and individual CVH metrics.
Results: The analytical sample consisted of n = 507 women (62% minority/Hispanic, mean age:37 y). Participants with adequate sleep duration (≥7 h), good sleep quality, no insomnia nor snoring, and low risk for OSA were more likely to meet >4 of the AHA LS7 metrics (P < .01). Poorer sleep quality (β = -0.08, P = .002), higher insomnia severity (β = -0.05, P = .002), snoring (β = -0.77, P = .0001), and higher risk for OSA (β = -1.63, P < .0001) were associated with poorer CVH. Insomnia, snoring, and high OSA risk were associated with 69% to >300% higher odds of having poor CVH (P ≤ .03). Associations were stronger in post-menopausal and racial/ethnic minority women.
Conclusions: Better sleep habits were associated with more favorable CVH among women, suggesting that there may be benefit in incorporating sleep assessment into CVD risk screening.
Mechanisms of cardiovascular disease in obstructive sleep apnoea
Abstract
Obstructive sleep apnoea (OSA) is recognized as a major public health burden conveying a significant risk of cardiovascular diseases (CVD) and mortality. Continuous positive airway pressure (CPAP) is the treatment of choice for the majority of patients with OSA but the benefit of CPAP on CVD is uncertain. Thus, a greater understanding of the mechanisms by which OSA leads to CVD might identify novel therapeutic approaches. Intermittent hypoxia (IH), a hallmark feature of OSA, plays a key role in the pathogenesis and experimental studies using animal and cell culture studies suggest that IH mediates CVD through activation of multiple mechanistic pathways such as sympathetic excitation, inflammation, oxidative stress or metabolic dysregulation. Recurrent arousals, intrathoracic pressure swings and concomitant obesity likely play important additive roles in this process. In this review, the available evidence of the pathophysiological mechanisms of CVD in OSA is explored with a specific emphasis on IH, recurrent arousals and intrathoracic pressure swings as the main pathophysiological triggers.
Sleep disorders, nocturnal blood pressure, and cardiovascular risk: A translational perspective
Abstract
Cardiovascular disease (CVD) represents the first cause of death globally. The nighttime is generally a period of relative protection from CVD events such as myocardial infarction, sudden cardiac death, and stroke, at least compared to the early morning period. The nighttime also generally entails lower values of arterial blood pressure (ABP) and heart rate (HR) and higher cardiac parasympathetic modulation. These day-night cardiovascular rhythms are ultimately driven by circadian molecular oscillators in the hypothalamic suprachiasmatic nucleus and in peripheral cells, including those in the heart, blood vessels, and kidneys. The wake-sleep states are intermediate mechanisms of circadian cardiovascular regulation, with non-REM sleep decreasing ABP and HR and increasing cardiac parasympathetic modulation at the beginning of the night. Obstructive sleep apnea, insomnia, and the restless legs syndrome have high prevalence in the general population and may increase nighttime cardiovascular activity and CVD risk. CVD risk is better predicted by ABP values during nighttime sleep than during daytime wakefulness. Higher nighttime values of ABP and HR increase cardiac work and vessel wall stress. During the night, circadian rhythms may enhance cardiac responses to hypertrophic stimuli, increase vascular smooth muscle Rho kinase activity and contractility, decrease endothelial nitric oxide production and vascular responses to vasodilators, and increase circulating monocytes with the potential to infiltrate atherosclerotic plaques. Together, these factors configure a "perfect storm" scenario that may make increased cardiovascular activity during the night a final common mechanism linking sleep disorders to CVD risk.
Reallocating Time to Sleep, Sedentary Behaviors, or Active Behaviors: Associations With Cardiovascular Disease Risk Biomarkers, NHANES 2005–2006
Abstract
Sleep and sedentary and active behaviors are linked to cardiovascular disease risk biomarkers, and across a 24-hour day, increasing time in 1 behavior requires decreasing time in another. We explored associations of reallocating time to sleep, sedentary behavior, or active behaviors with biomarkers. Data (n = 2,185 full sample; n = 923 fasting subanalyses) from the cross-sectional 2005–2006 US National Health and Nutrition Examination Survey were analyzed. The amounts of time spent in sedentary behavior, light-intensity activity, and moderate-to-vigorous physical activity (MVPA) were derived from ActiGraph accelerometry (ActiGraph LLC, Pensacola, Florida), and respondents reported their sleep duration. Isotemporal substitution modeling indicated that, independent of potential confounders and time spent in other activities, beneficial associations (P < 0.05) with cardiovascular disease risk biomarkers were associated with the reallocation of 30 minutes/day of sedentary time with equal time of either sleep (2.2% lower insulin and 2.0% lower homeostasis model assessment of β-cell function), light-intensity activity (1.9% lower triglycerides, 2.4% lower insulin, and 2.2% lower homeostasis model assessment of β-cell function), or MVPA (2.4% smaller waist circumference, 4.4% higher high-density lipoprotein cholesterol, 8.5% lower triglycerides, 1.7% lower glucose, 10.7% lower insulin, and 9.7% higher homeostasis model assessment of insulin sensitivity. These findings provide evidence that MVPA may be the most potent health-enhancing, time-dependent behavior, with additional benefit conferred from light-intensity activities and sleep duration when reallocated from sedentary time.
Sleep Duration and Quality: Impact on Lifestyle Behaviors and Cardiometabolic Health: A Scientific Statement From the American Heart Association
Insomnia and Risk of Cardiovascular Disease
Insomnia is the most prevalent sleep disorder in the United States and has high comorbidity with a number of cardiovascular diseases (CVDs). In the past decade, a number of observational studies have demonstrated an association between insomnia and incident cardiovascular disease (CVD) morbidity and mortality, including hypertension (HTN),
coronary heart disease
(CHD), and heart failure (HF). Despite some inconsistencies in the literature, likely due to variations in how insomnia is defined and measured, the existing data suggest that insomnia, especially when accompanied by short sleep duration, is associated with increased risk for HTN, CHD and recurrent
acute coronary syndrome
, and HF. Purported mechanisms likely relate to dysregulation of the
hypothalamic-pituitary axis
, increased
sympathetic nervous system
activity, and increased inflammation. This paper reviews the most recent studies of insomnia and CVD and the potential pathophysiological mechanisms underlying this relationship and highlights the need for randomized trials to further elucidate the nature of the relationship between insomnia and CVD.
Sleep Duration and Total and Cause-Specific Mortality in a Large US Cohort: Interrelationships With Physical Activity, Sedentary Behavior, and Body Mass Index
Both short and long durations of sleep are associated with higher mortality, but little is known about the interrelationship between sleep and other modifiable factors in relation to mortality. In the National Institutes of Health-AARP Diet and Health Study (1995–1996), we examined associations between sleep duration and total, cardiovascular disease (CVD), and cancer mortality among 239,896 US men and women aged 51–72 years who were free of cancer, CVD, and respiratory disease. We evaluated the influence of moderate-to-vigorous physical activity, television viewing, and body mass index (BMI; weight (kg)/height (m)2) on the sleep-mortality association and assessed their combined association with mortality. During an average of 14 years of follow-up, we identified 44,100 deaths. Compared with 7–8 hours of sleep per day, both shorter and longer sleep durations were associated with higher total and CVD mortality. We found a greater elevation in CVD mortality associated with shorter sleep among overweight and obese people, suggesting a synergistic interaction between sleep and BMI. People in the unhealthy categories of all 4 risk factors (sleep <7 hours/day, moderate-to-vigorous physical activity ≤1 hour/week, television viewing ≥3 hours/day, and BMI ≥25) had significantly higher all-cause (relative risk (RR) = 1.42, 95% confidence interval (CI): 1.34, 1.52), CVD (RR = 1.90, 95% CI: 1.67, 2.17), and cancer (RR = 1.21, 95% CI: 1.09, 1.34) mortality. Short sleep duration may predict higher mortality, particularly CVD mortality, among overweight and obese people.
Cardiovascular Disease in Women Across the Lifespan: The Importance of Sleep
Abstract
Cardiovascular disease (CVD) and sleep disturbances are both common and associated with significant morbidity and mortality. Compared with men, women are more likely to report insufficient sleep. During the 2018 Research Conference on Sleep and the Health of Women sponsored by the National Heart, Lung, and Blood Institute, researchers in cardiology, integrative physiology and sleep medicine reviewed the current understanding of how sleep and sleep disturbances influence CVD in women across the lifespan. Women may be particularly vulnerable to the negative effects of sleep disturbances at important stages of their life, including during pregnancy and after menopause. The proposed pathways linking sleep disturbances and adverse cardiovascular outcomes in women are numerous and the complex interaction between them is not well understood. Future research focused on understanding the scope of sleep disorders in women, defining the underlying mechanisms, and testing interventions to improve sleep are critical for improving the cardiovascular health of all women.
REM Sleep Imposes a Vascular Load in COPD Patients Independent of Sleep Apnea
Abstract
Arterial stiffness, a marker for cardiovascular risk, is increased in patients with Chronic Obstructive Pulmonary Disease (COPD) and Obstructive Sleep Apnea (OSA). The specific influence of both on arterial stiffness during sleep is unknown. Nocturnal arterial stiffness (Pulse Propagation Time (PPT) of the finger pulse wave) was calculated in 142 individuals evaluated for sleep apnea: 27 COPD patients (64.7 ± 11y, 31.2 ± 8 kg/m2), 72 patients with cardiovascular disease (CVD group, 58.7 ± 13y, 33.6 ± 6 kg/m2) and 43 healthy controls (HC group 49.3 ± 12y, 27.6 ± 3 kg/m2). Sleep stage related PPT changes were assessed in a subsample of COPD patients and matched controls (n = 12/12). Arterial stiffness during sleep was increased in COPD patients (i.e. shortened PPT) compared to healthy controls (158.2 ± 31 vs. 173.2 ± 38 ms, p = 0.075) and to patients with CVD (161.4 ± 41 ms). Arterial stiffening was particular strong during REM sleep (145.9 ± 28 vs. 172.4 ± 43 ms, COPD vs. HC, p = 0.003). In COPD, time SaO2 < 90% was associated with reduced arterial stiffness (Beta +1.7 ms (1.1-2.3)/10 min, p < 0.001). Sleep apnea did not affect PPT. In COPD, but not in matched controls, arterial stiffness increased from wakefulness to REM-sleep (ΔPPT-8.9 ± 10% in COPD and 3.7 ± 12% in matched controls, p = 0.021). Moreover, REM-sleep related arterial stiffening was correlated with elevated daytime blood pressure (r = -0.92, p < 0.001) and increased myocardial oxygen consumption (r = -0.88, p < 0.01). Hypoxia and REM sleep modulate arterial stiffness. In contrast to healthy controls, REM sleep imposes a vascular load in COPD patients independent of sleep apnea indices, intermittent and sustained hypoxia. The link between REM-sleep, vascular stiffness and daytime cardiovascular function suggests that REM-sleep plays a role for increased cardiovascular morbidity of COPD patients.
Sleep Disturbance, Sleep Duration, and Inflammation: A Systematic Review and Meta-Analysis of Cohort Studies and Experimental Sleep Deprivation
Abstract
Background
Sleep disturbance is associated with
inflammatory disease
risk and all-cause mortality. Here, we assess global evidence linking sleep disturbance, sleep duration, and inflammation in adult humans.
Methods
A systematic search of English language publications was performed, with inclusion of primary research articles that characterized sleep disturbance and/or sleep duration or performed experimental sleep deprivation and assessed inflammation by levels of circulating markers. Effect sizes (ES) and 95% confidence intervals (CI) were extracted and pooled using a random effect model.
Results
A total of 72 studies (n > 50,000) were analyzed with assessment of
C-reactive protein
(CRP), interleukin-6 (IL-6), and
tumor necrosis factor α
(TNFα). Sleep disturbance was associated with higher levels of CRP (ES .12; 95% CI = .05–.19) and IL-6 (ES .20; 95% CI = .08–.31). Shorter sleep duration, but not the extreme of short sleep, was associated with higher levels of CRP (ES .09; 95% CI = .01–.17) but not IL-6 (ES .03; 95% CI: −.09 to .14). The extreme of long sleep duration was associated with higher levels of CRP (ES .17; 95% CI = .01–.34) and IL-6 (ES .11; 95% CI = .02–20). Neither sleep disturbances nor sleep duration was associated with TNFα. Neither experimental sleep deprivation nor sleep restriction was associated with CRP, IL-6, or TNFα. Some heterogeneity among studies was found, but there was no evidence of publication bias.
Conclusions
Sleep disturbance and long sleep duration, but not short sleep duration, are associated with increases in markers of systemic inflammation.
Sufficient sleep duration contributes to lower cardiovascular disease risk in addition to four traditional lifestyle factors: the MORGEN study
Abstract
Background
The contribution of sufficient sleep duration to lower CVD risk in addition to sufficient physical activity, a healthy diet, (moderate) alcohol consumption, and non-smoking has not been investigated yet.
Design
The MORGEN study is a prospective cohort study including 8128 men and 9759 women aged 20–65 years, free of CVD at baseline.
Methods
Sufficient physical activity (≥3.5 h/week cycling or sports), a healthy diet (Mediterranean Diet Score ≥5), (moderate) alcohol consumption (≥1 beverage/month), non-smoking, and sufficient sleep duration (≥7 hours) were assessed by self-administered questionnaires between 1994 and 1997. Cardiovascular morbidity and mortality were ascertained through linkage with national registers. Hazard ratios and preventable proportions were calculated adjusted for age, sex, and educational level.
Results
During 10–14 years of follow up, 607 composite CVD events (fatal CVD, nonfatal myocardial infarction and stroke) occurred, of which 129 were fatal. Those with the four traditional healthy lifestyle factors had a 57% lower risk of composite CVD (HR 0.43, 95% CI 0.31–0.59) and a 67% lower risk of fatal CVD (HR 0.33, 95% CI 0.16–0.68) compared with those with none or one healthy lifestyle factor. Sleeping sufficiently in addition to the four traditional lifestyle factors resulted in a 65% lower risk of composite CVD (HR 0.35, 95% CI 0.23–0.52), and an 83% lower risk of fatal CVD (HR 0.17, 95% CI 0.07–0.43).
Conclusions
Sufficient sleep and adherence to all four traditional healthy lifestyle factors was associated with lower CVD risk. When sufficient sleep duration was added to the traditional lifestyle factors, the risk of CVD was further reduced.
Biomarkers of cardiovascular risk in sleep-deprived people
Abstract
The global increase in both coronary heart disease (CHD) and cardiovascular disease (CVD) and the associated increase in undetected subclinical cardiovascular pathology highlight the continuing need for improved risk prediction. Traditional risk factors fail to identify all ‘at-risk’ individuals. Although new risk factors, associated with endothelial function, inflammatory and oxidative stress pathways, for example, have been identified, studies have often observed only minimal improved risk classification when such markers are added. We examine the emerging evidence that short sleep may be a risk factor for obesity, type 2 diabetes and hypertension, and an independent predictor of stroke, CHD and CVD. We examine the underlying mechanisms and the evidence to suggest that short sleep may modulate the association between established factors and CVD. We consider whether the levels of markers of obesity and appetite control, energy metabolism, glucose homoeostasis, inflammation, thrombosis and haemostasis, which are affected by short duration of sleep, might be useful predictors of the risk of developing CVD. Finally, the usefulness of such markers for disease detection, management and prevention is considered.
Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies
Abstract
Aims
To assess the relationship between duration of sleep and morbidity and mortality from coronary heart disease (CHD), stroke, and total cardiovascular disease (CVD).
Methods and results
We performed a systematic search of publications using MEDLINE (1966–2009), EMBASE (from 1980), the Cochrane Library, and manual searches without language restrictions. Studies were included if they were prospective, follow-up >3 years, had duration of sleep at baseline, and incident cases of CHD, stroke, or CVD. Relative risks (RR) and 95% confidence interval (CI) were pooled using a random-effect model. Overall, 15 studies (24 cohort samples) included 474 684 male and female participants (follow-up 6.9–25 years), and 16 067 events (4169 for CHD, 3478 for stroke, and 8420 for total CVD). Sleep duration was assessed by questionnaire and incident cases through certification and event registers. Short duration of sleep was associated with a greater risk of developing or dying of CHD (RR 1.48, 95% CI 1.22–1.80, P < 0.0001), stroke (1.15, 1.00–1.31, P = 0.047), but not total CVD (1.03, 0.93–1.15, P = 0.52) with no evidence of publication bias (P = 0.95, P = 0.30, and P = 0.46, respectively). Long duration of sleep was also associated with a greater risk of CHD (1.38, 1.15–1.66, P = 0.0005), stroke (1.65, 1.45–1.87, P < 0.0001), and total CVD (1.41, 1.19–1.68, P < 0.0001) with no evidence of publication bias (P = 0.92, P = 0.96, and P = 0.79, respectively).
Conclusion
Both short and long duration of sleep are predictors, or markers, of cardiovascular outcomes.
Sleep Duration and Sleep Quality in Relation to 12-Year Cardiovascular Disease Incidence: The MORGEN Study
Abstract
Study Objectives:
We studied sleep duration and sleep quality in relation to cardiovascular disease (CVD) incidence.
Design/Setting:
Dutch population-based cohort study.
Participants:
20,432 men and women aged 20-65 y with no history of CVD.
Interventions:
N/A
Measurements:
Sleep duration and sleep quality were assessed by a self-administered questionnaire. Morbidity data, vital status, and causes of death were obtained through linkage with several national registries. Hazard ratios (HRs) and 95% confidence intervals (95% CIs) were calculated using Cox proportional hazards models.
Results:
During 10-15 years of follow-up, 1,486 CVD and 1,148 coronary heart disease (CHD) events occurred. Short sleepers (≤ 6 h) had a 15% higher risk of total CVD (HR: 1.15; 95%CI: 1.00-1.32) and a 23% higher risk of CHD (HR: 1.23 [1.04-1.45]) compared to normal sleepers (7 h) after adjustment for all confounders. Additional adjustment for intermediate biological risk factors attenuated these relative risks to 1.11 (0.97-1.27) for total CVD and to 1.19 (1.00-1.40) for CHD. Short sleepers with poor sleep quality had a 63% higher risk of CVD (HR: 1.63 [1.21-2.19]) and a 79% higher risk of CHD incidence (HR: 1.79 [1.24-2.58]) compared to normal sleepers with good sleep quality, after adjustments for all confounders. We observed no associations between long sleep duration (≥ 9 h) and CVD or CHD incidence.
Conclusions:
Short sleepers, especially those with poor sleep quality, have an increased risk of total CVD and CHD incidence. Future investigations should not only focus on sleep duration, but should also take sleep quality into account.
Sleep Duration and Cardiovascular Disease: Results from the National Health Interview Survey
Abstract
Background:
Previous studies have shown that both short and long sleep durations are related to increased likelihood of diabetes and hypertension. However, the relation between sleep duration and cardiovascular disease (CVD) is not clear. We examined the hypothesis that compared with sleep duration of 7 hours, shorter and longer sleep durations are independently related to CVD.
Methods:
We conducted a cross-sectional study of 30,397 National Health Interview Survey 2005 participants ≥ 18 years of age (57.1% women). Sleep duration was categorized as ≤ 5 hours, 6 hours, 7 hours, 8 hours, and ≥ 9 hours. The main outcome of interest was the presence of any CVD (n = 2146), including myocardial infarction, angina, and stroke.
Results:
We found both short and long sleep durations to be independently associated with CVD, independent of age, sex, race-ethnicity, smoking, alcohol intake, body mass index, physical activity, diabetes mellitus, hypertension, and depression. Compared with a sleep duration of 7 h (referent), the multivariate odds ratio (95% confidence interval) of CVD was 2.20 (1.78, 2.71), 1.33 (1.13, 1.57), 1.23 (1.06, 1.41), and 1.57 (1.31, 1.89) for sleep duration ≤ 5 h, 6 h, 8 h, and ≥ 9 h. This association persisted in subgroup analyses by gender, race-ethnicity, and body mass index categories. Also, similar associations were observed when we examined myocardial infarction and stroke separately.
Conclusion:
Compared with sleep duration of 7 h, there was a positive association between both shorter and longer sleep durations and CVD in a representative sample of US adults. These results suggest that sleep duration may be an important marker of CVD.