Tissue Repair
Morphology of Granulation tissue
2 patterns
Late form
Fibrous granulation tissue
Inconspicuous capillaries and numerous plump activated fibroblasts
Early form
Vascular granulation tissue
Loose connective tissue matrix
Proliferating fibroblasts
Leukocytes
Occupied by
Macrophages and lymphocytes
Resolving inflammation
Proliferating capillaries and fibroblast
Wound Healing
Former site of tissue damage and active inflammation
2nd intention
Differences compared to 1st Intention healing
Parenchymal regen cannot fully reconstitute original architecture
wound contraction present
Fibroblast with smooth muscle characteristics
mediated by myofibroblast
Much larger amounts of grnulation tissue formed
More intense inflammatory rxn
Occurs in wounds with separated edges
First intention
1st Month
Tensile strength increases gradually thereafter
Dermal appendages destroyed by injury are permanently lost
Scar comprises of connective tissue covered by intact epidermis
Week 2
Leukocyte infiltration, Edema and increased vascularity disappeared
Continued proliferation of fibroblast and accumulation of fibrogen
Day 5
Epidermis recovers normal thickeness
Collagen bridges incision
Incisional space filled with granulation tissue
Day 3
Epithelial proliferation continues
Collagen fibers present at margin but do not bridge incision
Granulation tissue invades incisional space
Replacement of neutrophils by macrophages
24-48Hrs
Continuous thin epithelial layer formed
Fusing in midline beneath surface scab
Spurs of epithelial cells migrate and grow along margins
Epidermis at cut edge thickens due to mitotic activity of basal cells
Immediate response to injury
Acute inflamation occurs with appearance of neutrophils at edge of wound
Dehydration of clot form scab
Wound fills with clotted blood
Healing of clean wounds with opposed edges
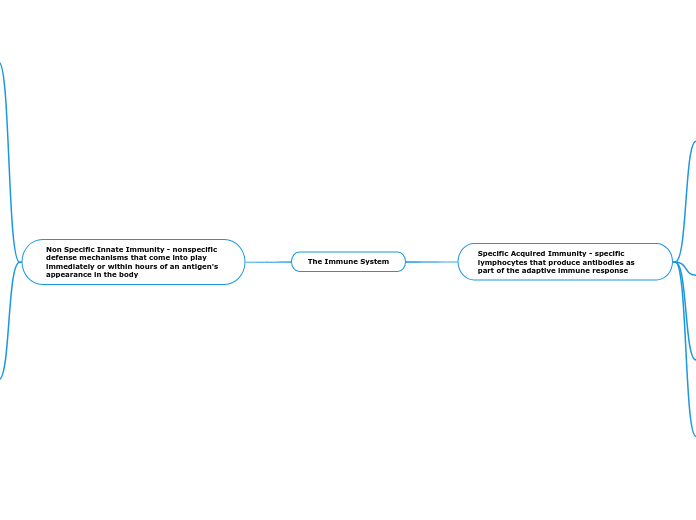
2 Distinct Processes
Fibrosis
Non-dividing cells hence must heal by fibrosis instead
Skeletal muscle
Cardiac muscle
Neurons
Scar formation
Replacement of injured cells by connective tissue
4) Remodelling of Fibrous Tissue
Vascular regression continues as scar matures
Conversion of granulation tissue into scar
Dense collagen
Spindle shaped fibroblasrt
3) Deposition of ECM
Fibroblast proliferation decreases over time while ECM deposition increases
major portion of connective tissue formed by fibrillar collagens
2) Migration + Proliferation of Fibroblasts
Formation of granulation tissue framework
Proliferation triggered by GFs and Cytokines
1) Angiogenesis
d) Recruitment of periendothelial cells
Smooth muscle cells
Pericytes
c) Maturation of Cells
Inhibition and remodeling into capillary tubes
b) Migration and proliferation of Endothelial Cells
To angiogenic stimulus
a) Proteolytic Degradation
BM of parent vessel
Regeneration
Restitution of normal structure
Needs intact basement Membrane
Cells proliferate haphazrdly if BM disrupted
Needed for organized regeneration
Underlying supporting stroma of parenchymal cells
Replacement of injured cells by cells of same type
Stable Cells
Quiescent cells
E.g.
Parenchymal cells of glandular organs
Vascular endothelial cells
Mesenchymal cells
Considered to be G0 but can be stimulated into G1
Capable of rebuilding tissue of origin
Rapid division in response to stimuli
Normally low level or replication
Labile Cells
Stratified sq. cells of skin, columnar epithelium of GI tract
Regen. derived mostly from stem cells with unlimited regen capacity
Continuously dividing cells
Proliferate to replace cells
Follow cell cycle from one mitosis to the next