MedChem of MS
Pathology of MS
- Demyelinated areas (plaques/lesions) in the CNS:
- Loss of myelin + oligodendrocytes
- White/grey matter (lesions)
- Brain and spinal cord
- Early MS: axons/neurons preserved
- Ongoing MS: axons/neurons lost
- Brain atrophy + ventricular enlargement
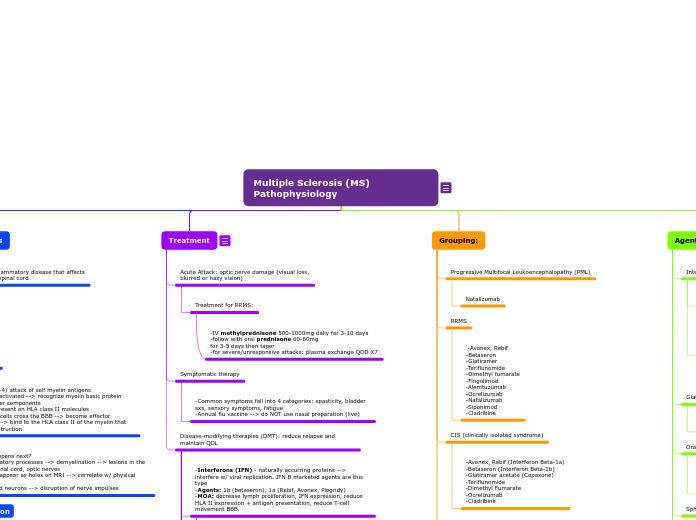
Treatment :D
Symptomatic therapies
-maintain QOL; manage sxs (muscle spasticity, bladder sxs, sensory sxs, fatigue)
Disease modification treatment
Slow disease course, reduce progression
Rituximab was once considered for MS but was suspended.
Daclizumab was approved 2016, removed in 2018. Urgent review after 7 cases of serious inflammatory brain disorders and encephalitis meningoencephalitis.
Other classes:
Fumarates:
Monomethyl fumarate: Relapsing MS, SPMS
Unknown MOA, may decrease blood vessel permeability. Eliminated mainly as CO2.
Diroximel fumarate: Relapsing MS, SPMS
Less likely to cause GI ADEs due to substitution of methanol with inert 2-hydroxyethyl succinamide
Dimethyl fumarate: Relapsing MS, SPMS
Metabolized by esterase in liver and GI tract to active MMF
Cladribine
ADEs:
-Cytotoxic
-Malignancies
-Lymphopenia/hematologic toxicity
-Infections
-Liver injury
-Cardiac failure
-Risk of teratogenicity
MOA:
-Adenosine analog --> inhibits nucleoside metabolism --> toxic to B/T cells --> red lympho counts
Indication: MS, SPMS (used when other txt unacceptable)
Mitoxantrone
ADEs:
-Bone marrow suppression
-Neutropenia
-Menstrual disorder
MOA:
Binds to+ breaks DNA --> reduce lympho proliferation
Indication: SPMS, PRMS, or worsening RRMS (LAST RESORT)
Teriflunomide
ADEs:
-Liver toxicity (CI in hepatic imp)
-Teratogenicity
MOA:
-Reduce inflammation
-Reduce pyrimidine synthesis --> reduce T/B cell proliferation --> reduce lymphocytes in CNS
Glatiramer Acetate (Copaxone)
MOA:
-Mimics myelin basic protein of the myelin sheath --> decoy to T-cell attack
-Mixture of polypeptides containing L-Glu, L-Lys, L-Ala, L-Tyr
S1P Receptor modulators
Ozanimod: MS/SPMS
ADEs:
-somnolence, fatigue, headache, dizziness, bradycardia, HTN, liver injury, N
Siponimod: MS/SPMS
** similar to Fingolimod
Fingolimod: Relapsing MS
ADEs:
-Heart toxicity:
-Bradycardia (1st dose monitor)
-QTc prolongation, other arrhythmias, need heart monitor for 6h after 1st dose
-CI: I/III anti arrhythmic drugs, 2/3 AV block, prolonged QTc, recent cardiac diseases
MOA:
-Sphingosine 1-phosphate receptor modulators
-Bind to S1P1R/S1P5R --> sequesters lymphocytes in lymph nodes/thymus/GI tract --> reduces circ. T cells/macrophages --> reduce CNS infiltration of immune cells
Antibodies
Ofatumumab
ADEs:
-Hepatitis B reactivation
-Progressive PML
MOA:
-IgG, CD20
-Bind to CD20 --> Ab-depnd cytolysis
Indication: Relapsing MS or SPMS
Ocrelizumab
ADEs:
-Infused-related reaction
-Infections
is there a difference b/w infusion related rxn and infusion associated rxn???
MOA:
-IgG monoclonal antibody
-Target CD20 on surface of B cells
-Induce B cell self-destruction
Indication: MS or PPMS
Natalizumab
ADEs:
-IAR
-Risk of PML (progressive multifocal leukoencephalopathy) due to human polyomavirus (check pts)
-risk of immune reconstitution inflammation syndrome (IRIS) when D/C due to PML
-depression, infection, fatigue
Human Polyomavirus (John Cunningham (JC) Virus):
- infected by inhalation
- resides in bone marrow/kidneys
- reactivated by immunosuppression
- Enters CNS --> attacks oligodendrocytes --> causes PML
MOA:
-Humanized IgG monoclonal antibody
-binds to interns, reduces lymphocyte entry through BBB
Indication: Relapsing MS
Alemtuzumab
ADEs:
-Infusion Associated Rxn (IAR) in 90% of pts
-Mild-mod: headache, rash, pyrexia, N, resp/urinary tract infections
-Increased herpes infection risk (prophylactic acyclovir txt)
-secondary autoimmune disease mainly changing thyroid func (30-40% of pts)
MOA:
-CD52 monoclonal antibody
-depletes T+B cells
Indication: High efficacy for relapsing MS
-Use after inadeq response to 2 other drugs
Interferon-B1a/B1b
ADEs:
-Flu-like sxs
-depression
-Caution: dev. of neutralizing antibodies (NABs) --> dec efficacy overtime
Agents:
B1a (glycosylated):
-Avonex, Rebif
B1b (non-glycol):
-Betaseron, Extavia
Pegylated-IFNB1a:
-Plegridy
Glycosylation improves activity and has a stabilizing influence
MOA:
-Immunomodulation
-reduces inflammatory response
Indication: Relapsing MS
-Reduce MRI lesion activity
-reduce brain atrophy
-inc time to reach clinic def MS
-decrease relapse rate
-reduce risk of sustained disability progression
Treatment of exacerbations (early RRMS):
-shorten duration/reduce severity
-IV high dose corticosteroid
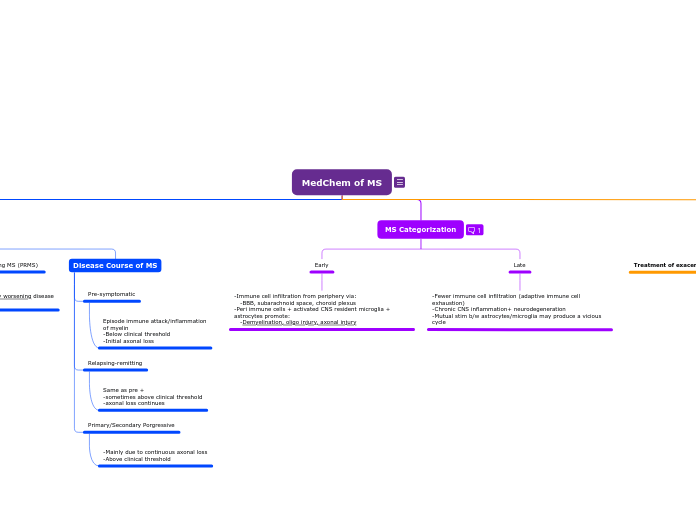
MS Categorization
Inflammation is present at ALL stages
Late
-Fewer immune cell infiltration (adaptive immune cell exhaustion)
-Chronic CNS inflammation+ neurodegeneration
-Mutual stim b/w astrocytes/microglia may produce a vicious cycle
Early
-Immune cell infiltration from periphery via:
-BBB, subarachnoid space, choroid plexus
-Peri immune cells + activated CNS resident microglia + astrocytes promote:
-Demyelination, oligo injury, axonal injury
Clinical Course Categories of MS
Disease Course of MS
Primary/Secondary Porgressive
-Mainly due to continuous axonal loss
-Above clinical threshold
Relapsing-remitting
Same as pre +
-sometimes above clinical threshold
-axonal loss continues
Pre-symptomatic
Episode immune attack/inflammation
of myelin
-Below clinical threshold
-Initial axonal loss
Progressive Relapsing MS (PRMS)
Rare form of MS, steadily worsening disease
state from the onset
Primary progressive MS (PPMS)
Uncommon, slowly worsening sxs from the onset w NO relapses or remissions
Secondary Progressive MS (SPMS)
Sxs worsen more steadily over time w/wo the
occurrence of relapses and remissions
-most ppl who are diagnosed w/ RRMS will --> SPMS
Relapsing-Remitting MS (RRMS)
The most common form, characterized by temporary
periods of relapses and remissions