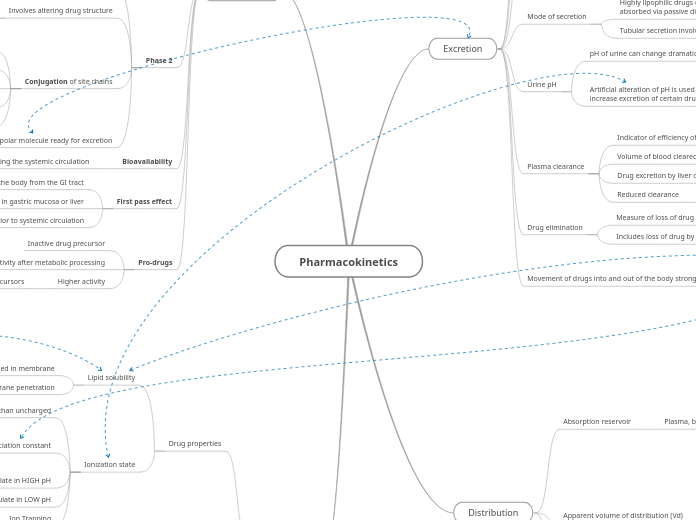
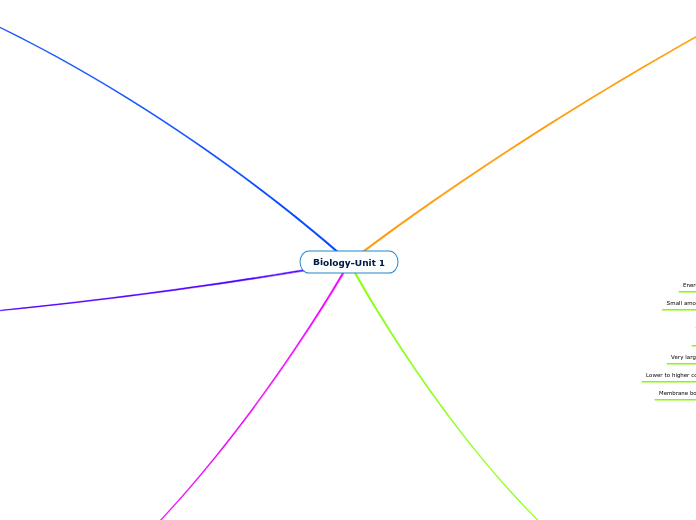
Pharmacokinetics
Absorption
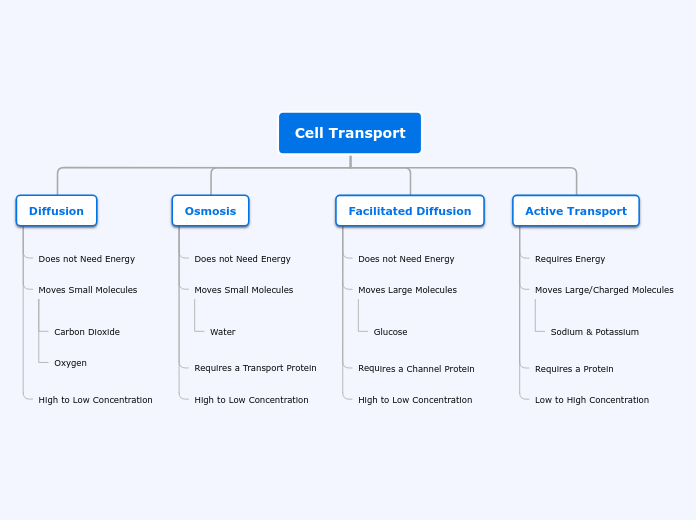
Passive movement
Solute carrier
E.g. Organic cation transporters
Mediate the movement of dopamine and choline
Facilitates transport single species IN THE DIRECTION of its electrochemical gradient
Aquaporins
Diffusion is the mechanism used by most drugs
Facilitated diffusion is passive with no energy
Active transport
Pinocytosis
Specific carriers
ABC transporters
Mediate removal of drugs from cells
E.g. P‐glycoprotein transporters
Primary group of ABC transporters
Transport AGAINST concentration gradients
Specialized membrane proteins
Drug properties
Ionization state
Ion Trapping
Drug's ionization preference and retention
Basic drug will accumulate in LOW pH
Acidic drug will accumulate in HIGH pH
Dissociation constant
Negative value = greater proportion
of non-ionized drug
Greater lipid solubility
Ratio between dissociated ions and drug
Ionized dissolve aqueous fluids than uncharged
Lipid solubility
High soluble = higher membrane penetration
Too lipid-soluble = retained in membrane
Metabolism
Pro-drugs
Higher activity
Different absorption or distribution properties than precursors
Gain full drug activity after metabolic processing
Inactive drug precursor
First pass effect
Reduces bioavailability prior to systemic circulation
Occur in gastric mucosa or liver
Almost all drugs entering the body from the GI tract
Bioavailability
Amount of drug reaching the systemic circulation
Phase 2
Produces polar molecule ready for excretion
Conjugation of site chains
Glycine or water addition
Methylation
Glutathione addition
Sulphation
Glucuronidation
Involves altering drug structure
Normally results in inactive product (some exceptions)
Reduce intrinsic efficacy for excretion
Mainly in the liver
Can also occur in other tissues like lungs and kidneys
Phase 1
Metabolic enzymes generally alter drugs to activate them and make them more water soluble
Cytochrome system
P450 enzyme levels regulated by external factors
E.g. grapefruit juice and Brussels sprouts
Genetic variations exist
Primary cause of patient response variation
Net effect of cytochrome p450 cycle
is addition of oxygen or hydroxyl
3 main CYP gene families
CYP3
CYP2
CYP1
Nonpolar drugs go through phase 1 more than polar
Need to cross cell membrane to reach cytochrome systems
Mainly in liver
Can also occur in other tissues or plasma
Hepatic cytoplasmic microsomal enzymes
E.g. cytochrome systems
Most common residue is hydroxyl
Mediated by cytochrome system associated with ER
Oxidation (also reduction and hydrolysis)
Distribution
Endothelial cells
Blood brain barrier
Diffusion is PRIMARY for drugs crossing BBB
Active transport by carriers
AA, glucose, amines and purines
Highly lipophilic drugs able to readily pass through
Molecule must pass through at least 2 membranes
Fenestrations
Gaps that allow solute diffusion
Apparent volume of distribution (Vd)
Large Vd drug likely to enter body compartment
Drug with very low Vd likely to still be in circulation
Gives estimate where drug is (tissues or circulation)
Dose divided by measured plasma concentration
Absorption reservoir
Plasma, body fat and interstitial water
Fat ~20%
Intracellular water ~35%
Interstitial water ~16%
Plasma water ~5%
Transcellular water ~2%
Comprises CSF, intraocular, peritoneal, pleural and synovial fluids and digestive secretions
Excretion
Movement of drugs into and out of the body strongly influenced by:
pH of the compartment
Drug pKa
Drug lipid solubility
Drug elimination
Includes loss of drug by metabolism and any other excretory routes
Measure of loss of drug mass from the circulation per unit of time
Plasma clearance
Reduced clearance
Indicative of function impairment of excretory organ
Drug excretion by liver or kidneys is best described by clearance
Volume of blood cleared of a drug through an organ per time
Indicator of efficiency of drug removal from plasma
Clearance is a constant for any given drug
Urine pH
Artificial alteration of pH is used to
increase excretion of certain drugs
Alkaline urine increases acidic drug excretion
Acidic urine increases basic drug excretion
Ion trapping to increase drug retention in urine
pH of urine can change dramatically
Due to diet or drug intake
Mode of secretion
Tubular secretion involve specific transporter proteins
Highly lipophilic drugs or non-ionized
absorbed via passive diffusion
Glomerular ultrafiltration
Unbound fraction exhibits pharmacologic effects
Small molecules readily pass and are cleared
Drugs with high affinity protein slower excretion
Less free drug for filtration and diffusion
Level of plasma protein binding to drug
Plasma proteins too large to
pass renal luminal barrier
Retained in circulation
Enterohepatic circulation
Drugs may be excreted in the bile after transport by the solute carriers and ABC transporters
Results in prolonged drug action
Account up to 20% of total drug in the body
Most excretion occurs in kidneys
Most drugs excreted in urine or bile (lesser extent)
Drug clearance rate via renal greatly differ