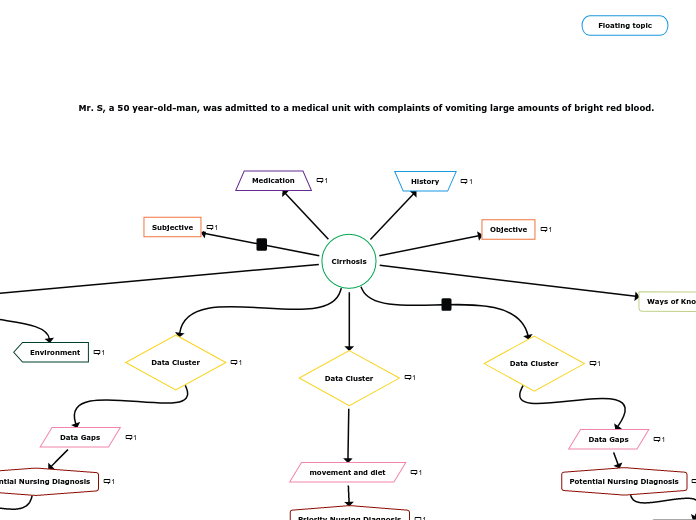
Floating topic
Mr. S, a 50 year-old-man, was admitted to a medical unit with complaints of vomiting large amounts of bright red blood.
Key
Smart Goal
Nursing DIagnosis
Subjective and Objective Data
Medical Diagnsis
Cirrhosis
Ways of Knowing
- Aesthetic knowing considers a holistic approach taking into account physiologic, psychosocial and spiritual needs in arriving to a plan of care. Using aesthetic knowing, I can involve his family with the objective of helping him abstain from alcohol. Patient can also be referred to home health services, local support groups and counselling for patient and family to assist. This would be help manage the patient’s tendency of being prone to alcohol abuse.
Metaparadigm
Nursing
Nursing
This aspect pertains to the care plan assessment and actual knowledge application of the nurse in providing care to the patient. An example would be vital sign gathering and assessment requiring to prompt action as per called by the situation. The nurse should be aware on what to look out for and ensure that primary care provider is up to date with any changes.
Environment
Environment
Focus is to utilize opportunities within the patient’s immediate environment to assist with his recovery. The patient’s condition requires an absolute necessity in avoiding alcohol and other hepatotoxic drugs. In line with this, community-based alcohol treatment programs and support groups like Alcoholics Anonymous can be recommended.
Person
Person
Focus is to treat the patient holistically and view the patient in his wholeness. Main objective is to assist patient to adapt to physiological and psychological changes. This can be achieved by looking for ways to manage fatigue and conserve energy plus strengthen self-esteem and morale of the patient.
Health
Health
The main objective is to achieve the best possible degree of health for the patient and to sustain it as long as possible. This can be achieved by extending health teachings to the patient specific to his condition along with the importance of complying with follow-up health care visits to be able to monitor his condition properly.
Varices due to portal hypertension
-HR 122, BP 86/58 mmHg
-Hemoglobin 70 mmoL/L (normal for males: 140 – 180 mmol/L)
-Hematocrit 0.27 (0.42-0.54)
-vomiting large amounts of bright red blood
-multiple ecchymotic areas on his body
-INR 3 (INR 0.81- 1.2)
movement and diet
Bowel movement
-To know if the patient is constipated. Constipation causes straining with bowel movements and could increase bleeding.
Diet
-Need to identify diets to be avoided such as irritating foods which could increase trauma on mucus membranes due to increased risk of injury as a result of high vascularity. Also, diet rich in vitamins helpful to the patient like vitamin K which could help promote clotting and avoid bleeding complications need to be recommended.
Priority Nursing Diagnosis
Decreased Cardiac Output related to cirrhosis and varices due to portal
hypertension shown by HR 122, BP 86/58 mmHg, Hemoglobin 70 mmoL/L
(normal for males: 140 – 180 mmol/L), Hematocrit 0.27 (0.42-0.54), INR 3 (INR
0.81- 1.2), vomiting large amounts of bright red blood, and multiple ecchymotic
areas on his body.
-Patient to maintain normal vital sign readings within limits within the next 48 hours from admission monitored every 3 hours.
-Patient’s hematocrit and hemoglobin be maintained within normal limits within the next 48 hours from admission monitored through daily lab works.
-Patient will sustain urine output of >30 mL/hr within the next 72 hours monitored every 3 hours.
-Patient will verbalize that their anxiety is reducing during each assessment.
-Nurse to monitor vital signs keeping an eye on tachycardia or hypotension which should be reported once identified. An increased pulse and decreasing blood pressure may indicate hypovolemia due to hemorrhage.
-Nurse to facilitate bleeding precautions such as use of soft toothbrush, avoid blowing nose and prevent constipation. Preventive measures applied can decrease the risk for active bleeding.
-Nurse to encourage verbalization of fears and concerns, answer questions honestly and correct any false notions about the disease treatment, process or prognosis.
History
-Diagnosed with cirrhosis
-Cirrhotic liver has never fully recovered from 25 years of heavy drinking
-He has not been compliant with follow-up visits to his health care provider
-Admitted to the hospital four times in the past 24 months, with a diagnosis of G.I. bleed
-He has a 30-year history of smoking
-CEO of a large real estate company
-Lives with his wife (upscale suburban neighborhood outside of Toronto)
-Job is very stressful
-Drinking 2 or 3 bottles of beer, and several glasses of wine each evening
-Has business lunches where several alcoholic drinks may be consumed
-Never appears to be impaired during business hours
-Lifestyle does not allow him to fully abstain from drinking
Ascites
-abdomen firm and distended
-abdominal discomfort
-breath sounds diminished to bases, complaining of shortness of breath (dyspnea)
-feels fatigued & lethargic
Weight and Abdominal girth
-Monitor to determine if the patient is retaining fluids
Paracentesis
-Procedure details to drain excess fluid from abdomen so proper care can be given if required. Monitor for infection, hypovolemia and bleeding.
Diet
-If there is fluid restriction(H2O and Na+) avoid fluid buildup.
Excess fluid volume related to cirrhosis and ascites shown by abdomen firm and distended, abdominal discomfort, breath sounds diminished to bases, complaining of shortness of breath, feels fatigued & lethargic.
SMART Goal
-Patient’s fluid balance is kept by monitoring intake and output within a 24-hour period making sure that body weight is stable and absence of ascites and peripheral edema every shift.
-Nurse to recommend low-sodium diet within 500-2000 mg/day and control fluids within suggested volumes. Increased sodium and fluids can result to higher water retention, increasing fluid volume, ascites, and portal hypertension.
Medication
Medications
-Packed RBCs to be infused 2Units over 2 hours each
-PIV insertion
-Octreotide
- IV fluid 0.9 Nacl at 25mls/hr
-Albumin 25% 5g to be infused after RBCs completed
-Oxygen was administered at 3 liters per minute by nasal cannula.
-Beta adrenergic blocker
-Spironolactone
-Lactulose
-Sclerotherapy for bleeding varices
Objective
Objective:
-50-year old man
-awake, alert, orientated to time, but not to place, initially irritable and confused.
-Epistaxis noted; Yellow sclera
-lung lobes clear bilaterally, breath sounds diminished to bases, complaining of shortness of breath
-normal S1 S2, no S3 or S4. Heart rhythm regular, HR 122. BP 86/58 mmHg, feels fatigued & lethargic
-abdomen firm and distended, bowel sounds hyperactive to 4 quadrants, abdominal discomfort, vomiting large amounts of bright red blood
-normal urinary output, gynecomastia
-some mild tremors in both hands
-pale, jaundiced, multiple ecchymotic areas on his body, site for the maintenance IV has fresh bloodstains noted on the dressing
-observe a large amount of blood all over his gown and bed linen
-Hemoglobin 70 mmoL/L (normal for males: 140 – 180 mmol/L) Low
-Hematocrit 0.27 (0.42-0.54) Low
-AST 260 u/L (normal: 0 – 35 u/L) High
-Ammonia level of 117 mcmol/L, (normal: 6 – 47 mcmol/L) High
-INR 3 (INR 0.81- 1.2) High
-SpO2 94 room air
Subjective
Subjective:
-“He states he has been coughing on and off for the past several days”
-“bright red blood”
-“he was quite irritable and refused to come to the hospital”
-“he began vomiting large amounts of bright red blood”
-“I feel nauseated and dizzy”
Data Cluster
Portal systemic encephalopathy
-Orientated to time, but not to place, initially irritable and confused
-feels fatigued & lethargic
-Ammonia level of 117 mcmol/L, (normal: 6 – 47 mcmol/L)
-some mild tremors in both hands (Asterixis – “liver flap”)
-Lactulose
Data Gaps
Effects of Lactulose
How is the patient tolerating the effect of lactulose? Maintain 2-5 loose bowel movements per day.
Diet
Patient should have protein restriction, high calorie (3000kcal/d), high carb, moderate to low fat and Na+
Potential Nursing Diagnosis
Risk for Acute confusion related to cirrhosis and portal systemic encephalopathy shown by Ammonia level of 117 mcmol/L, (normal: 6 – 47 mcmol/L), some mild tremors in both hands, awake, alert, orientated to time, but not to place, initially irritable and confused feels fatigued & lethargic.
SMARTGoal
-Patient to demonstrate cognitive orientation by an accurate identification of self, significant other, current location, date and time, recollection of recent significant events to be evaluated every shift during assessment.
Nursing Intervention
-Nurse to monitor bowel function preventing constipation and promoting regular movement.