realizată de Obada Khamis 2 ani în urmă
785
Glucose
Lesch-Nyhan syndrome arises from a defect in the HGPRT enzyme, leading to increased levels of hypoxanthine and guanine, resulting in elevated uric acid and subsequent gout-like symptoms.
realizată de Obada Khamis 2 ani în urmă
785
Mai multe ca aceasta
Fructose-1-Phosphate Aldolase Deficiency: Progressive hepatomegaly and delayed development.
Symptoms:
Hereditary fructose intolerance!
Favism is the deficiency of G6PD (most common enzyme deficiency?)
Criegler Najjar:
Types:
Deficienies of Heme metabolism enzymes cause Porphyrias
Affects skeletal muscles, the heart. Myoglobin increases in the plasma due to increases muscular effort
Affects liver an causes a decrease in gluconeogenesis
Acetoacertyl CoA
3-Hydroxy-3-Methylglutaryl CoA
Mevaolnate
Mevalonate-5-Phosphate
5 Pyrophosphomevalonate
Isopentylyl Pyrophosphate
Squalene
Squaline 2,3 Epoxide
Lanosterol
Zymosterol
Desmosterol
Cholesterol
High cholesterol concentration:
Hypocholesterolemia:
C14 Acyl-CoA
Deficiency is caused by:
Regulation:
-Inhibitors:
-Activators:
Fructosuria
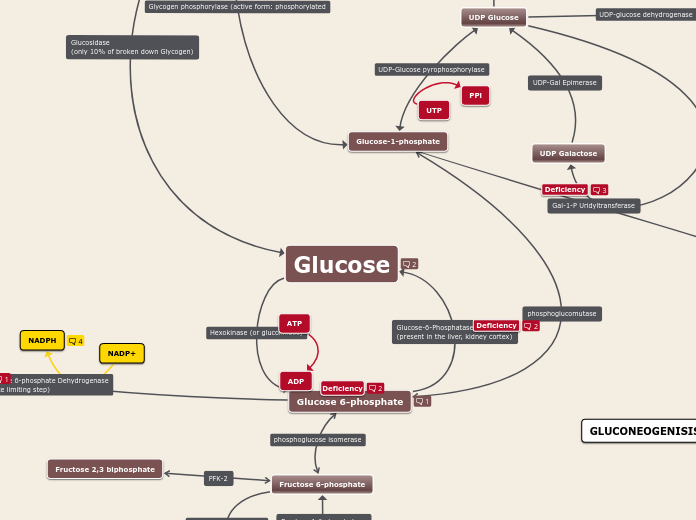
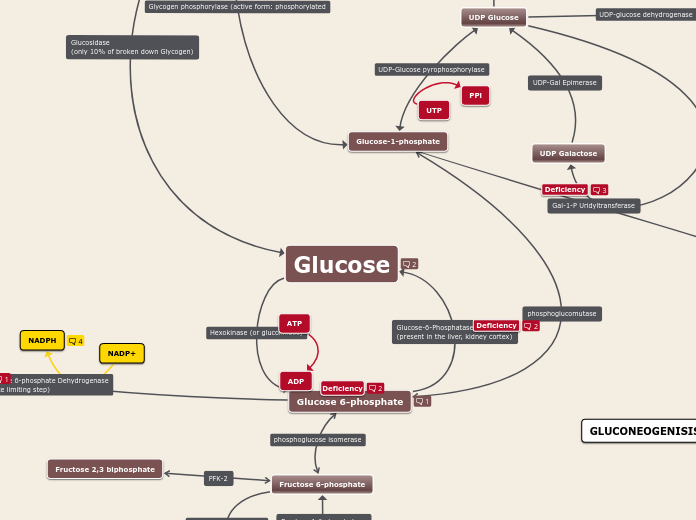
Causes: Type one GSD I (Von Gierke Disease)
Signs:
Treatment: Liver transplants
Causes Galactosemia -> accumulates Gal-1-P
Mortality: 75%
Symtoms: hepatomegaly, cirrhosis, renal failure, cataracts, vomiting, seizures, hypoglycemia, lethargy and ovarian failure
+ Cataracts due to galactitol accumulation
Thymine is an analog of 5-flurouracil (5-FU)
Key step: CPS II (carbamoylphosphate synthase II)
first synthesis UMP
Medical importance:
>Azaserine inhibits CTP synthesis
>Methotrexate inhibits dTMP synthesis
>Arabinosyl Cytosine inhibits dCDP synthesis
dTMP
Methotrexate inhibits the synthesis of dTMP
dTDP
dTTP
Azaserine inhibits the synthesis of CTP
CDP
dCDP
Arabinosyl Cytosing (ara-c) inhibits the synthesis of dCDP
dCMP
dCTP
Regulating enzyme is Aspartate transcarbamoylase
APRT = Adenine phosphoribosyl transferase
Adenine + PRPP >> AMP + PP
Hypoxanthine + PRPP >> IMP + PP
HGPRT = Hypoxanthin-Guanin-Phosphoribosyl tranferase
*Guanine + PRPP >> GMP + PP
LESCH NYHAN SYNDROME
-->increased level of Hypoxanthine + Guanine (also: more uric acid)
-->PRPP accumulates (stimulates Purine production + degradation)
>gout like symptoms, neurological symptoms (spasticity, aggression, selfmutilation)
Excess of uric acid in urine froms crystals in kidney (renal stones)
Excess froms crystals in joints (Gout)
Gout drugs vermindern uric acid production:
a) hemmen Xanthine oxidase = Xanthine oxidase inhibitors
b) binden Xantine Oxidase = Allopurinol treatment
control by feedback mechanism (zu viel GMP hemmt GMP synthesis)
control via feedback mechanism (zu viel AMP hemmt AMP synthesis)
!! Schlüsselenzym = geschwindigkeitsbestimmende Reaktion:
Bildung von 5-Phosphoribosylamin aus PRPP und GLUTAMIN
durch das Enzym GLUTAMIN-PRPP-AMIDOTRANSFERASE
Glutamin-PRPP-Amidotranferase gehemmt durch AMP, GMP, IMP
Key step: PRPP synthetase
first synthesis of IMP
Hemmung durch AMP, GMP, IMP
Competitive Inhibition: other enzymes that decrease cholestrol levels in the blood
Feedback Inhibition: Mevalonate and Cholesterol
Hormones (Covalent Inhibition):
Sterol Regulatory Element Binding Protein: regulates mRNA synthesis of HMG reductase mRNA.
Causes hemolytic anemia
Symptoms: jaundice and splenomegaly
Treatment: blood transfusion, splenectomy
Causes decreased 2,3-DPG levels (70% of normal), making oxygen release more difficult
Causes Mody II Diabetes Mellitus
Tissues dependent on it:
Autosomal recessive disorder. Causes high arginine levels in urine
Treatment: low nitrogen diet
Recessive autosomal disorder. Causes high argininosuccinate in the urine.
Severity varies.
Treatment: dietary restrictions of nitrogen
Autosomal recessive disorder. Causes Citrulline accumulation in blood and urine
Type I citrullinemia: manifests in the first few days of life
Type II citrullinemia: manifests in adulthood in the nervous system
Treatment: Arginine supplements for protein synthesis
X-linked recessive. Most common urea cycle disorder
Symptoms:
Mental retardationa and developmental delay
Autosomal recessive metabolic disease that causes mental retardation and developmental delay
Hyperammonemia is observed
Treatment:
benzoate and phenylactetate
*Hippurate and phenylacetylglutamine and excreted in urine
Heme
Biliverdin
Unconjugated Bilirubin
Albumin-Bilirubin Complex
Salicylates & sulfonamides can displace unconjugated bilirubin in the blood and cause brain damage
Conjugated Bilirubin (Diglucuronide)
Urobilinogen
Stercobilin
Symptoms: -present in the first 6 months of life followed by death
-cabbage like odor, hypoglycemia and then glycemia
-mild mental retardation
-urine contains tyrosine, p-HPPA and hydroxyphenylacetic acid
-serum contains tryosine
Treatment: restricted diet of tyrosine and phenylalanine
Treatment: vitamin C and a restricted protein diet
Symptoms: Hypertyrosinemia in newborns
Normal Life in early life up to middle age.
Symptoms:
Symptoms: mental retardation, keratosis of the palms. corneal lesions, photophobia
Treatment: low protein diet
I (Classical): total deficiency
II (Variant): Partial deficiency
III (Transient): Delayed maturation of the enzyme
Diagnosis: -blood criteria: >20 mg/dL (normal = 1)
-Gutherie's Test: Bascillus Subtilis culture
-Ferric Chloride Test: a drop is added to urine. A change to blue-green is positive
-DNA analysis
Treatment: A strict phenylalanine free diet
Symptoms: -elevated phenylalanine serum levels, depressed tyrosine levels
-thyroid hormone decrease
-catecholamine and tryptophan decrease
-hypopigmentation
-musty smelling urine and swear
80 micrograms produced by the Thryoid
5 micrograms produced by thyroid + 25 due to peripheral monodeiodination
Norepinephrine
Epinephrine
Excess = Pheochromocytoma.
Symtoms:
Melanin
4-Maleylacetoacetate
4-Fumarylacetoacetate
Cytosolic
In the liver
Fructose metabolism only occurs in the liver
Formed after 3 days of starvation
Essential in the synthesis of fatty acids, cholesterol and steroid hormones
Maintains glutathion in its reduced forms in red blood cells which is essential for membrane intergrity against oxidizing agents
Keeps iron in its reduced from (F2+)
Needed for Nitric oxide synthesis, which is a vasodilator and platelet aggregation inhibitor.
The C1 of the UDP glucose forms a glycosidic bond with the C4 of an already existing glycogen chain
Adrenaline and Glucagon inhibit Glycogen Synthase; Insulin stimulates it
Phosphorylase Kinase stimulates Glycogen phosphorylase
Diacylglyerol and Ca2+ inhibit glycogen production by activating phophorylase kinase (which phosphorylates Glycogen synthase and consequently deactivates it).
Roles:
-Conjugation of bilirubin
-Synthesis of vitamin C (in plants)
-Synthesis of glycosaminoglycans (repetitive disaccharide (sugar-amino sugar))
D Glucoronic Acid
L-Xylulose
Glycoaminoglycans
N-acetylglutamate (NAG) is the postive allosteric regulator of CPS I
An increase in arginine increases NAG
NAG deficiency causes urea cycle failure and death if not detected
immediately after birth. Hyperammonemia and general hyperaminoacidemia
are signs.
Argininosuccinate
Arginine
Guanidoacetate
Creatine
H2O
Creatinine
Urine
Peeeeeeeeeee
Creatine phosphate
P
Urea
Ornithine
Glycerol-3-Phosphate
Glucose-6-phosphatase is active in the phosphorylated form!!
Na independent diffusion transport:
Na dependent co-transport:
Hexokinase/Glucokinase is inhibited by glucose-6-phoshate and ATP excess
NADPH is a strong competitive inhibitor of G6PD. When the NADPH/NADP+ ratio decreased, this pathway is opened due to the lack of inhibition of the enzyme.
PFK-I is
Inhibited by:
Stimulated by:
Glyceraldehyde 3-phosphate x2
1,3-biphosphoglycerate x2
2,3-Diphosphoglycerate
Subjects with hexokinase deficiency have decreased levels of 2,3 DPG (70% of normal), so the affinity of Hb to oxygen is greater than normal, which makes oxygen release towards tissues more difficult.
◦Subjects with pyruvate kinase deficiency increase in 2,3 DPG and the affinity of hemoglobin to oxygen is less than normal.
3-phosphoglycerate x2
2-phosphoglycerate x2
phospho-enol-pyruvate x2
Pyruvate x2
Pyruvate Kinase is inhibited by ATP excess
-phosphorylated = active
-dephosphorylated = inactive
Oxaloacetate
Pryuvate Carboxylase requires Biotin, ATP and acetyl CoA
Malate
Fumarate
Succinate
Succinyl CoA
Ketoglutarate Dehydrogenase is inhibited by succinyl CoA, ATP and NADH
CoA and Glycine (?)
δ-AminoLevulinic Acid
Limiting step.
-Regulated genetically by synthesis of ALA synthase.
-Erythrocytes regulate it through iron availability
Porphobilinogen
Porphobilinogen Synthase is inhibited by Lead
High ALA is thought to cause some of the neurological
effects of lead poisoning, although Pb ++
also may directly affect the nervous system.
ALA is toxic to the brain, perhaps due to:
• Similar ALA & neurotransmitter GABA
(g-aminobutyric acid) structures.
• ALA autoxidation generates reactive oxygen
species (oxygen radicals).
α-ketoglutarate
Isocitrate Deydrogenase is stimulated by ADP. It's inhibited by ATP and NADH
Glutamate Glutamine Arginine Histidine Proline
Isocitrate
Citrate
Citrate Synthetase is inhibited by ATP, FFA and succinyl CoA
Acteyl-CoA
Fatty Acid Synthase
Has two subunits
Condensation
Reduction
Dehydration
NADPH
Palmitic Acid C16
Preseved by: Carnitine-Acetylcarnitine I
Inhibited by: malonyl CoA
Regulation:
-Insulin:
-Glucagon:
Fatty Acid
Glycolipids
Cerebrosides: White matter + Myelin Sheath
Gangliosides: Grey matter
Fatty Acid-Acyl CoA
2x COASH
Phosphatidic Acid
Phosphate
Diglyceride
Diacylglyceride (DAG)-CDP (Lecithin or sphingosine)
Lecithin: Framework of cells and nuclear membrane
Cepahlin: Blood clotting and coagulation role
Sphingophospholipids: Cell membranes and myelin sheath
Catabolism
Phospholipase C (mammals and bacteria)
Phospholipase D (plants)
Phospholipase A1 (mammals)
Phospholipase A2 (mammals)
CoA
Acylcarnitine
Rate Limiting Step
Malonyl CoA
Acetyl CoA Carboxylase requires Biotin as a coenzyme
Reglated by citrate (activates) and palmitoyl CoA (inhibits) allosterically
Ocaloacetate
Ethanol (not in humans)
Alanine
Transaminase require pyidoxal phosphate
Acetyl CoA
Pyruvate Dehydrogenase is inhibited by Arsenic and vitamin B1 deficiency
Pyruvate Dehydrogenase also requires:
-thiamine pyrophosphate
-lipoic acid
-COASH (from pantathonic acid)
-FAD (Flavin Adenine Dinucleotide) from B2
-NAD (from niacin)
Activated by: PDH Phosphatase, which is stimulated by Mg2+, Ca2+ and insulin
Deactivated by: PDH Kinase, which is stimulated by acetyl CoA, NADH and ATP excess. Inhibited by: pyruvate
Acetoacetyl CoA
3-Hydroxy-methylglutaryl CoA
Acetoacetate
3-Hydroxybutyrate
CO2
Acetone
Acetyl CoA x2
Lactate
Cori's Cycle