realizată de Phil Garner 5 ani în urmă
152
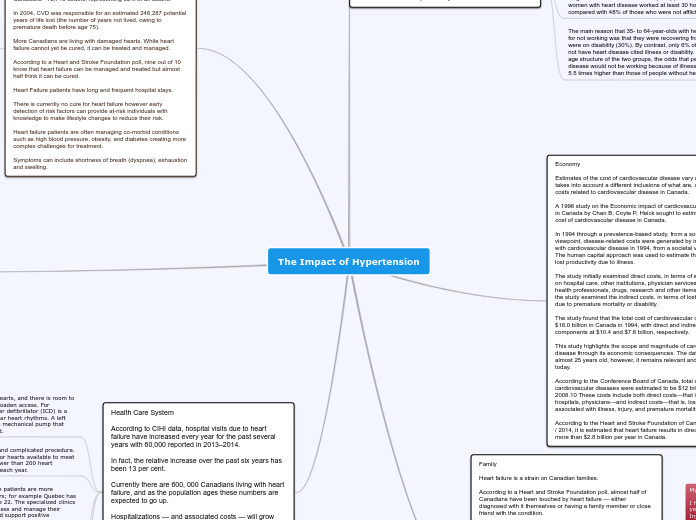
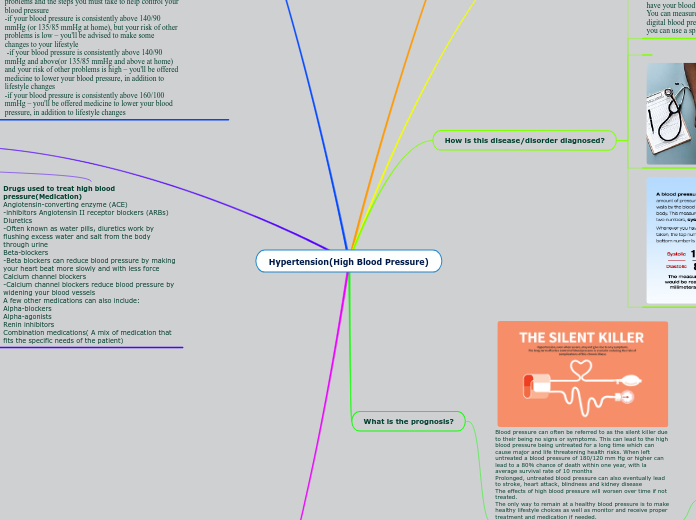
The impact of Hypertension
Hypertension significantly affects individuals and society, prompting extensive media campaigns by organizations like the Heart and Stroke Foundation to raise awareness and funds. The Government of Canada, along with public health bodies, disseminates crucial information on preventing cardiovascular diseases and recognizing symptoms of heart attacks and strokes.