SMART Goals
Fine motor
In 4 weeks, patient will score less than 33.3 seconds total on the 9-hole peg test to indicate improvement in hand dexterity and make strides towards typing with both hands
Range of Motion
In 3 weeks, patient will improve dorsiflexion active range of motion by 5 degrees, to help prevent foot drop and thus fall risk during gait.
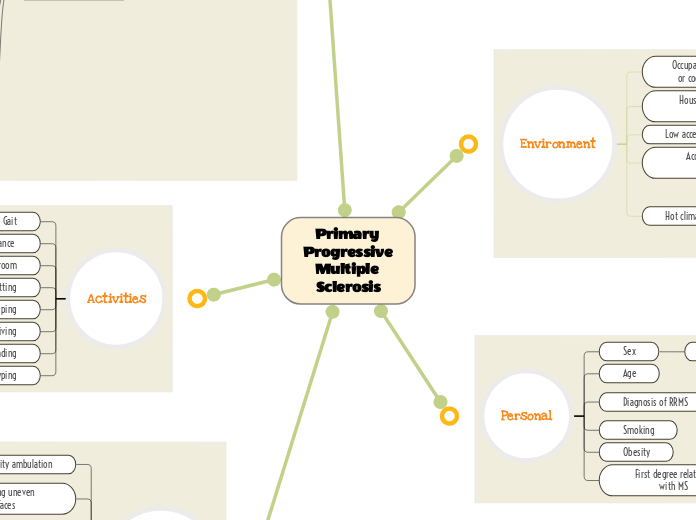
Deficits of PPMS
Loss of smell
Neurophysiology: damage to white matter in subcortical structures may affect smell due to the connections that the olfactory tract makes with the limbic system (amygdala, hypothalamus)
Neuroanatomy: limbic system, olfactory cortex
Weakness
Objective measure: MMT and ROM of anterior tibialis, extensor hallucis longus, extensor digitorum longus, as well as muscles of the shoulder, brachium and antebrachium
Guides POC to see extent of patient's weakness and to set intensity and modality of exercises given to pt
Neuroplasticity: use it and improve it, use it or lose it, intensity matters, interference
If the patient has a steppage gait due to foot drop, it would interfere with learning a new gait pattern that involves active use of the weak dorsiflexors
Making sure that the exercises that work the weaker muscles aren't too easy, and the patient feels challenged
If you don't target the weak dorsiflexion and hemiparesis, it will atrophy and get worse
Focusing on the weaker side of the body to improve its functions and recruitment
Neurophysiology: the corticospinal tract travels through CNS white matter structures that may be damaged due to MS, in the spinal cord and brainstem
Efficacy of muscle contractions depend on this tract running through myelinated structures
Neuroanatomy: Corticospinal tract
Left arm hemiparesis
Foot drop
Ambulation (dynamic balance)
Practice parameters
The training for dynamic balance should be blocked at first to improve her foundations of gait then be transferred to random to mimic a variety of surfaces she'll encounter in her environment
Outcome measure: DGI
Determine what other parts of ambulatory activities the patient struggles with
Walking on level surface, changing gait speed, gait with horizontal and vertical head turns, gait with pivot turn, stepping over and around obstacles, walking up stairs
Neuroplasticity: salience matters, transference,
When patient improves dynamic balances over firm surfaces, we can transfer her over to compliant surface ambulation to help her deficit of ambulating over uneven surfaces outside of the clinic.
Emphasizing that if ambulation improves, patient will be able to do more independent tasks by herself such as grocery shopping and socializing with friends.
Neurophysiology: if there are problems processing information from the sensory tracts, the motor tracts will have problems integrating the proper ambulation pattern. In addition, with possible damage to the corticospinal tract, the patient experiences hemiparesis which further impedes gait skills.
Neuroanatomy: corticospinal tract, DCML tract
Loss of taste
Neurophysiology: damage to the higher centers of gustation such as the cranial nerve 7 nuclei in the pons or the gustatory cortex will impede the patient's ability to sense taste.
Neuroanatomy: gustatory cortex, pons cranial nerve 7 nucleus
Primary Progressive Multiple Sclerosis