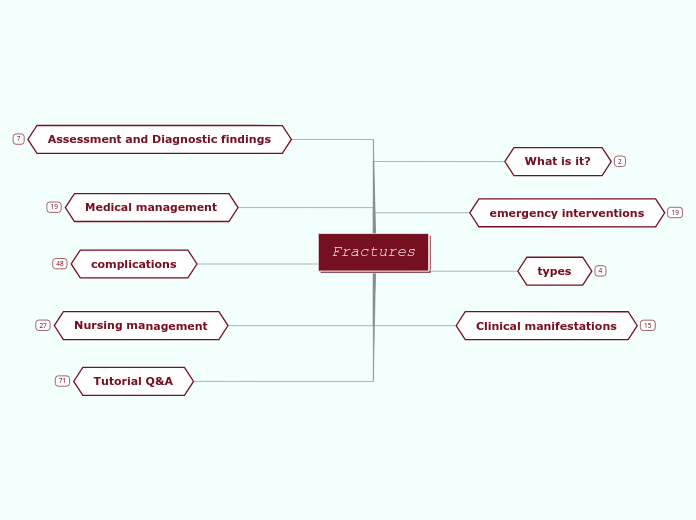
Fractures
Tutorial Q&A
Q16: Which assessment finding found while assessing a patient with a fracture who has traction requires immediate intervention?
D. Patient’s extremities have a capillary refill of less than 2 seconds
C. Patient uses the overhead trapeze bar to move around in the bed
B. Pin sites are free from drainage
A. The weights are freely hanging on the floor
Q15: A patient sustained a fracture to the femur. The patient has suddenly become confused, restless, and has a respiratory rate of 30 breaths per minute. Based on the location of fracture and the presenting symptoms, this patient may be experiencing what type of complication?
D. Hypovolemia
C. Fat embolism
B. Osteomyelitis
A. Compartment Syndrome
Q14: Your patient is 2 hours post-op from a cast placement on the right leg. The patient has family in the room. Which action by the significant other requires you to re-educate the patient and family about cast care?
D. Using a hair dryer on the cool setting to help with drying
C. Checking the colour and temperature of the right foot
B. Elevating the cast above heart level with pillows
A. Gently moving the cast with the fingertips of the hands every 2 hours to help with drying
Q13: Select all the signs and symptoms that will present in compartment syndrome?
E. Affected extremity feels cooler to the touch than the unaffected extremity
D. Feeling of tingling in the extremity
C. Pain relief with medication
B. Pallor
A. Capillary refill less than 2 seconds
Q12: What is the earliest sign of compartment syndrome?
D. Pulselessness
C. Parethesia
B. pain
A. Paralysis
Q11: Which statement by a patient, who just received a cast on the right arm for a fracture, requires you to notify the physician immediately?
D. "I've been using ice packs to reduce swelling."
C. "I can feel my fingers and move them."
B. "My pain is so severe that it hurts to stretch or elevate my arm."
A. "It is really itchy inside my cast!"
Q10: A 85-year-old patient has an accidental fall while going to the bathroom without assistance. It appears the patient has sustained a bone fracture to the left leg. The leg's shape is deformed, and the patient is unable to move it. The patient is alert and oriented but in pain. What will you do FIRST after confirming the patient is safe and stable?
D. Elevate the extremity above heart level
C. Administer pain medication
B. Immobilize the fracture with a splint
A. Apply an ice pack covered with a towel to the site
Q6, Q7, Q8, Q9
Q9 answer
A. Cover the fracture with a sterile dressing
Q8 answer
B. Compound Fracture
Q7 answer
D. Comminuted Fracture
Q6 answer
C. Oblique Fracture
with pictures, so answer them in the tut word
Q5: What kind of shock is most commonly found in a patient with fracture?
D. Septic shock
C. Neurologic shock
B. Cardiogenic shock
A. Hypovolemic shock
Q4: The fractured part should be elevated above the level of what organ?
D. kidney
C. liver
B. Heart
A. brain
Q3: Which one of the following is a nursing diagnosis for a patient with fracture?
D. Impaired breathing pattern
C. Acute pain
B. Situational low self-esteem
A. Risk for electrolyte imbalance
Q2: The most definitive diagnostic tool used in a patient with fracture is:
D. MRI
C. X-ray
B. SGPT and SGOT tests
A. Blood studies
Q1: The following are the different types of fractures EXCEPT for
D. Comminuted fracture
C. Closed fracture
B. Diagonal fracture
A. Open fracture
Nursing management
cast care education
management of swelling
gradual resumption of normal activities to protect limb from undue stresses
skin care
care for minor skin irritations
do not insert foreign objects inside the cast
to relieve itching
blow cool air from hair dryer
skin irritation from edge of cast
Describe techniques to promote cast drying
do not rest the cast on hard surfaces or sharp edges that can dent soft cast
do not cover cast
expose cast to circulating air
care plan
Risk of infection
Use aseptic technique during dressing changes, wound care, or handling or manipulation of tubes and drains.
Obtain specimens of wound drainage, sputum, blood, and urine in sterile containers.
Assess the incision and wound for redness, drainage, swelling, and increased pain:
Monitor temperature.
Impaired physical mobility
Consult with the physical therapist, about appropriate weight-bearing techniques and mobility aids
Encourage isometric, active, and resistive ROM exercises to all unaffected joints on a schedule consistent with the rehabilitation program and as tolerated.
Determine the type of assistive devices the patient will require for ambulation in anticipation of discharge
Acute pain
Maintain immobilization and support of the affected part. Elevate the affected extremity.
Apply ice packs for 20 to 30 minutes every 1 to 2 hours.
Administer opioid analgesics every 3 to 4 hours around the clock for the first 24 hours after surgical reduction or pin placement.
complications
factors inhibit healing
Weight bearing prior to approval
Inadequate immobilization and infections
Extensive local trauma and bone loss
smoking and co-morbidities
Avascular necrosis
Age >40 years
late complications
Complex Regional Pain Syndrome
Avascular Necrosis of Bone
The patient develops pain with movement that progresses to pain at rest.
occurs when the bone loses its blood supply and dies
may occur after a fracture with disruption of the blood supply to the distal area
Delayed Union, Nonunion, and Malunion
fat embolism syndrome
primary clinical manifestations
petechial rash
neurologic compromise
hypoxemia
may occlude the small blood vessels that supply the lungs, brain, kidneys, and other organs
occur when fat emboli enter circulation following orthopedic trauma, especially long bone (e.g., femur) fractures
paralysis
weakness with movements
paresthesias
faint pulse
pulselessness
numbness feeling
pallor
pale skin tone
When the pressure within an affected compartment rises above normal, perfusion to the tissues is impaired, causing cell death, which may lead to tissue necrosis and permanent dysfunction
characterized by the elevation of pressure within an anatomic compartment that is above normal perfusion pressure
An anatomic compartment is an area of the body encased by bone or fascia that contains muscles, nerves, and blood vessels.
early complications after surgery
DVT and PE
associated with reduced skeletal muscle contractions and bed rest.
compartment syndrome
“five Ps”
pain, pallor, pulselessness, paresthesias, and paralysis
independent functioning and self-esteem.
encourage Participation in activities of daily living (ADLs)
Restlessness, anxiety, and discomfort
reassurance, position changes, and pain-relief strategies
compromised neurovascular state
edema
controlled by elevating the injured extremity and applying ice as prescribed.
Medical management
pharmacological
antibiotic
to prevent infection
Cap Augmentin
analgesics
used to relieve pain and inflammation
Tab Chymoral
Tab Diclo ID
Immobilization
After the fracture has been reduced, the bone fragments must be immobilized and maintained in proper position and alignment until healing occurs
fracture reduction
open reduction
Internal fixation devices (metallic pins, wires, screws, plates, nails, or rods) may be used to hold the bone fragments in position until solid bone healing occurs.
where the fracture fragments are exposed surgically by dissecting the tissues.
closed reduction
accomplished by bringing the bone fragments into anatomic alignment through manipulation and manual traction
the manipulation of the bone fragments without surgical exposure of the fragments.
used in both open and closed fractures
restoration of the fracture fragments to anatomic alignment and positioning
Assessment and Diagnostic findings
magnetic resonance imaging (MRI)
used in the assessment of soft tissue injury
used in intra-articular fractures
computed tomography scan (CT, CAT scan)
used to help visualize areas of complex anatomy
x-ray
effectively evaluate most fractures and dislocations
Clinical manifestations
Ecchymosis
because of trauma and bleeding into the tissues
Hypovolemic shock
more frequently noted in pelvic fractures and open femoral fracture
resulting from hemorrhage
numbness
Crepitus
caused by the rubbing of the bone fragments against each other.
shortening
muscle spasms can cause the distal and proximal site of the fracture to overlap, causing the extremity to shorten
deformity
detectable when the limb is compared with the uninjured extremity.
Displacement, angulation, or rotation of the fragments
pain
pain is increased due to muscle spasms, which can also minimize further movement of the fracture
types
An open fracture (compound, or complex, fracture)
skin or mucous membrane wound extends to the fractured bone.
A closed fracture (simple fracture)
does not cause a break in the skin
emergency interventions
RICE
used to relieve pain and swelling and promote healing and flexibility
stands for: Rest, Ice, Compression, and Elevation.
in ED
The fractured extremity is moved as little as possible to avoid more damage.
The clothes are gently removed, first from the uninjured side of the body and then from the injured side.
for open fractures
Splints are applied for immobilization
wound is covered with a sterile dressing to prevent contamination of deeper tissues
determine the adequacy of peripheral tissue perfusion and nerve function
The neurovascular status distal to the injury should be assessed both before and after splinting
Adequate splinting
immobilization of suspected part
for upper extremities :
arm may be bandaged to the chest, or an injured forearm may be placed in a sling.
for long bones in lower extremities :
bandaging the legs together, with the unaffected extremity serving as a splint for the injured one.
Joints proximal and distal to the fracture also must be immobilized to prevent movement of fracture fragments.
if a fracture is suspected, the body part must be immobilized before the patient is moved.
What is it?
occur when the bone is subjected to stress greater than it can absorb
complete or incomplete disruption in the continuity of bone structure