av Kaitlyn Malone för 5 månader sedan
68
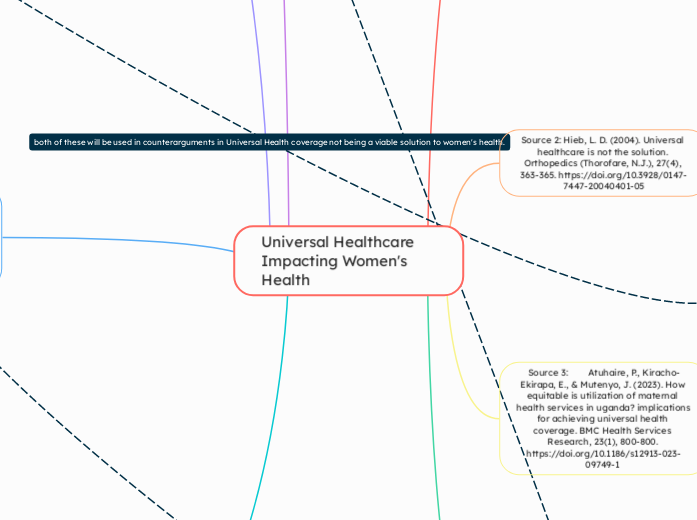
Annotated Bibliography Mind Map
In a universal healthcare system, disparities in breast cancer treatment pathways are influenced by the presence of private health insurance and the level of patient awareness regarding their entitlements.