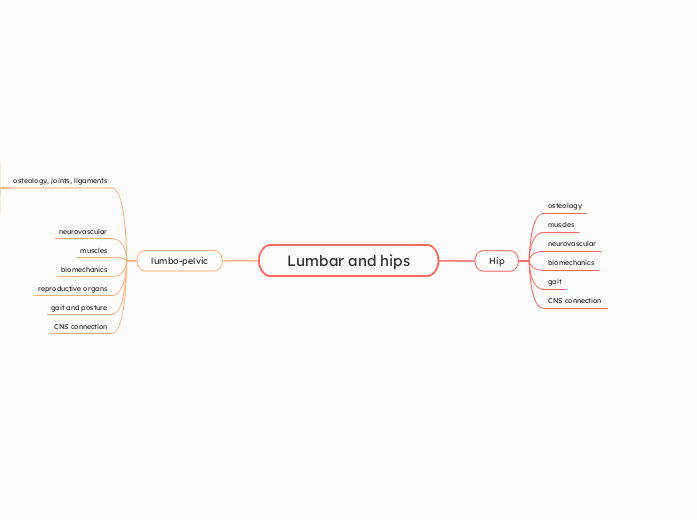
Lumbar and hips
lumbo-pelvic
CNS connection
Basal Ganglia Influence
movement initiation, modulation, and coordination, contributing to the overall goal-directed movement of the pelvis and lower limbs.
influence behavioral control and movement planning, indirectly affecting movement efficiency and precision.
Cerebellar Influence
smooth and coordinated control of trunk and pelvic movements, essential for balance and gait.
vermis and the flocculonodular lobe of the cerebellum are the primary regions responsible for these functions, known as the spinocerebellum (for trunk control) and vestibulocerebellum (for balance control).
Blood Supply to the Pelvis and Lower Extremities
Middle cerebral artery
supplies the more lateral brain regions, including those associated with the upper extremities.
anterior cerebral artery
supplies the blood flow to the medial portion of the brain, including the pelvic region of the motor and sensory homunculi
Motor Output
exit the spinal cord at the level of the pelvis (anterior spinal cord) and control muscles involved in pelvic and lower limb movements
reticulospinal tract also plays a role in postural control and helps with gross limb movements.
anterior corticospinal tract
Sensory Input to the Pelvis
Pathways
pain and temperature travels via the spinothalamic tract.
light touch and proprioception follows the dorsal column-medial lemniscal pathway.
relayed through the dorsal portion of the spinal cord
L1 to L3
gait and posture
Muscle Activation During Gait:
Foot and Tibial Movements in Relation to Pelvic Control
pronation of the foot during the early stance phase of walking leads to internal rotation of the tibia
Pelvic Rotation and Muscular Control:
internal rotation of the tibia causes internal rotation of the femur
Internal rotation of the pelvis occurs as the stance leg's hip internally rotates, especially during the early stance phase when the foot is pronating.
pelvic rotators (obliques, internal and external rotators) help coordinate pelvic rotation in the horizontal plane
Hip Muscles and Pelvic Movements:
Hip abductors, such as the gluteus medius, are crucial for frontal plane stability, helping prevent excessive pelvic drop on the opposite side
stance phase, the hip flexors (like the iliopsoas) are active to prevent excessive posterior pelvic tilt, while the hip extensors (like the gluteus maximus) control anterior pelvic tilt and stabilize the pelvis.
Hip flexors and extensors play a key role in controlling pelvic tilt and rotation
Pelvic Movements in Gait
Pelvic Movements in the Frontal Plane (Adduction and Abduction):
At weight acceptance (initial stance phase), the left iliac crest drops below the right, reflecting pelvic adduction of the right hip.
pelvic on femoral adduction and abduction during weight-bearing and swing phases.
Pelvic Tilting in the Sagittal Plane
Posterior pelvic tilt (backward tilt)
anterior pelvic tilt (forward tilt of the iliac crests)
Pelvic Rotation in the Horizontal Plane
external rotation (clockwise)
Internal rotation (counterclockwise)
reproductive organs
Female Reproductive Organs
round ligament and ovarian ligaments
secure the uterus and ovaries.
broad ligament
connects the sides of the uterus to the pelvic walls and supports the uterus, ovaries, and uterine tubes.
Vagina
serves as the passage for menstruation, childbirth
Uterus
terine artery supplies the uterus, while the uterine veins drain into the internal iliac veins
muscular organ where the fertilized egg implants and develops during pregnancy
Uterine Tubes (Fallopian Tubes)
carry oocytes from the ovaries to the uterus and are typically the site of fertilization
Ovaries
Male Reproductive Organs
Prostate Gland
role in sperm motility and protects sperm
Ejaculatory Ducts
deliver sperm and seminal fluid into the urethra.
Ductus Deferens (Vas Deferens)
passes through the inguinal canal
connects the epididymis to the urethra
Testes and Epididymis
testes are responsible for producing sperm and hormones, primarily testosterone. The epididymis stores and matures sperm cells.
Pelvic Force Couples:
Hip hiking
etc: right gluteus medius and left quadratus lumborum
Contralateral elevation of the pelvis
Posterior pelvic tilt
hip extensors and lumbar flexors.
Anterior pelvic tilt
hip flexors and lumbar extensors.
Lumbopelvic Rhythm:
Ipsidirectional rhythm
pelvis and lumbar spine rotate in the same direction
Contra-directional rhythm
pelvis and lumbar spine rotate in opposite directions
Sacroiliac (SI) Joint Movements:
Counternutation
Posterior rotation of the sacrum on the iliac bone, or anterior rotation of the iliac bone on the sacrum, or both.
Nutation
Anterior rotation of the sacrum on the iliac bone, or posterior rotation of the iliac bone on the sacrum, or both.
Pelvic Osteokinematic Movements
distal segment relative to the proximal segment
Pelvic Floor
Anatomy
Fascia
Forms a supportive layer around pelvic structures
Covers superior and inferior aspects of the pelvic diaphragm muscles
Levator Ani Muscles
Iliococcygeus
Elevates pelvic floor
Pubococcygeus
Supports pelvic viscera
Puborectalis
U-shaped loop around the anorectum
helps maintain fecal continence and plays a role in bowel movements
Coccygeus (Ischiococcygeus)
Forms part of the pelvic floor
Structure
Lesser Pelvis
Separated by the musculofascial pelvic diaphragm
Surrounded by the inferior pelvic girdle, supporting the pelvic cavity and perineum
Greater Pelvis
Contains inferior abdominal viscera, providing protection
Surrounded by the superior pelvic girdle
Functions
Pump for Circulation
Aids in lymphatic fluid circulation from the legs back to the heart
Stability
Fixes the trunk for extremity movement
Sexual Function
Allows relaxation for penetration and contraction for orgasm
Sphincter Control
Controls the urethra, vagina, and anus
Support for Internal Organs
Supports the pelvic and abdominal viscera
neurovascular
nerves
lumbosacral trunk
veins
Internal iliac veins
drains the blood from the pelvic organs and pelvic wall
Ovarian veins (in females)
drain deoxygenated blood from the ovaries and return it to the heart
Parietal median sacral vein
provides small branches that supply the pelvis
internal iliac veins
drain via the superior rectal vein
arteries
Superior gluteal
passes between lumbosacral trunk
Inferior gluteal
exits pelvis vis greater sciatic foramen
Middle Rectal
descends in pelvis to inferior part of rectum
Uterine
crosses ureter superiorly to reach cervix
Prostatic branches
Descends to prostate
Artery to ductus deferens
runs to ductus deferens
Inferior vesical
gives rise to prostatic artery
Obturator
runs antero-inferiorly on obturator fascia
Superior vesical
pass to superior aspect of bladder
Umbilical
superior aspect of urinary bladder
Anterior division of internal iliac
Passes anteriorly along lateral wall of pelvis
Internal iliac
Passes medially over pelvic brim and descends into pelvic cavity; often forms anterior and posterior divisions
Median sacral
Descends close to midline over L4 and L5 vertebrae, sacrum, and coccyx
Superior rectal
Crosses left common iliac vessels and descends into pelvis
Gonadal
Ovarian
Crosses pelvic brim
Testicular
Traverses inguinal canal and enters scrotum
osteology, joints, ligaments
pelvic girdle
functions
Supports pelvic viscera: Assists with abdominal functions and stability
Protects pelvic organs: Includes bladder, reproductive organs, intestines
Muscle attachment: Provides attachment for muscles of locomotion and posture
Weight transfer: Transfers weight to lower limbs via sacroiliac joints
Weight-bearing: Supports body weight during standing and sitting
Basin-shaped ring of bones
connects vertebral column to femurs
Composed of sacrum and innominate bones (ilium, ischium, pubis)
Sacrum articulates with ilium at SI joints
ligaments
Sacrospinous ligament
Connects the sacrum to the ischial spine, also contributing to pelvic stability
Sacrotuberous ligament
Attaches the sacrum to the ischial tuberosity, helping to stabilize the pelvis and limit movement
Iliolumbar ligament
stability to the lumbosacral junction
joints
Sacrococcygeal joint
where the sacrum and coccyx meet
Pubic symphysis
connects the left and right pelvic bones
Sacroiliac joint
connection between the spine and pelvis
pubis
Forms front part of the pelvic girdle
Supports lower body
Protects internal organs
Pecten Pubis (Pectineal Line)
Oblique ridge on the superior pubic ramus
Pubic Tubercle
Prominent swelling at lateral end
Pubic Crest
Thickening at the anterior part of the pubis
Inferior Ramus
Contributes to obturator foramen
Superior Ramus
Forms part of acetabulum
forms the lower and anterior part of each side of the hip bone
ischium
Provides support for sitting posture
Facilitates muscle attachment
Protects pelvic viscera
Lesser Sciatic Notch
Between ischial spine and tuberosity
Greater Sciatic Notch
Superior to ischial spine
Ischial Spine
Small pointed projection
Ischial Tuberosity
Large protuberance, supports weight while sitting
Ramus
Forms part of obturator foramen
Body
Contributes to acetabulum
forms the lower and back region of the hip bone
illium
Supports upper body weight
Provides attachment for muscles
Connects to sacrum for weight transfer
AIIS
Anterior Inferior Iliac Spine
ASIS
Anterior Superior Iliac Spine
Muscle and ligament attachments
Auricular Surface
Articulates with the sacrum (SI joint)
Iliac Fossa
Attachment for iliacus muscle
Iliac Crest
Superior border
ends at PSIS
Largest of 3 hip bones
hip and thigh
thigh
Sensory Control
Fasciculus Gracilis: This tract is responsible for carrying fine touch and proprioception signals from the thigh, helping the brain recognize the thigh's position in space and its movement relative to other body parts.
Anterolateral Tract: This pathway carries pain and temperature information from the thigh, allowing the brain to interpret sensations like discomfort or heat.
This cortex is involved in more complex processing of the sensory information, specifically for storing and processing spatial and tactile memories related to the thigh.
inferior MCA branch also supplies blood to this part of the brain
After the sensory data from the thigh is processed in the primary sensory cortex, it is sent to the secondary somatosensory cortex.
The sensory information from the thigh, including touch, proprioception (awareness of position), and pain, is processed in this area of the brain.
located on the medial surface of the brain.
Compartments
Posterior compartment
Popliteal Fossa
behind the knee where the tendons of the hamstring muscles converge.
Sciatic Nerve (L4-S3)
Semimembranosus: A broad, flattened muscle located deep to the semitendinosus.
Semitendinosus: A tendinous muscle located medially to the biceps femoris.
Biceps Femoris: Consists of two heads (long head from the ischial tuberosity, short head from the femur). It is located laterally and flexes the knee.
Medial compartment
Innervation and Blood Supply:
Obturator Artery: Supplies blood to the medial compartment.
Obturator Nerve: Innervates the medial thigh muscles.
Obturator Externus: Laterally rotates the thigh.
Adductor Magnus: The largest muscle in the medial compartment, with dual innervation (adductor part by obturator nerve, hamstring part by sciatic nerve).
Adductor Brevis: A short muscle beneath the adductor longus.
Adductor Longus: A flat muscle that forms the medial border of the femoral triangle.
Gracilis: Adducts the hip and flexes the knee.
Anterior compartment
Femoral Triangle
Contains the femoral nerve, artery, and vein.
Bound by the inguinal ligament, sartorius, and adductor longus
Innervation and Blood Supply
Femoral Artery
Femoral Nerve (L2-L4)
Supplies blood to the anterior thigh.
Provides motor innervation to the muscles of the anterior compartment
Key Muscles
Quadriceps Femoris
Vastus lateralis, vastus medialis, vastus intermedius
Primarily responsible for extending the knee.
Rectus femoris
Flexes the hip and extends the knee
The longest muscle in the body, running across the thigh
flexes, abducts, and externally rotates the hip, and also flexes the knee.
Iliopsoas
Composed of the iliacus and psoas major
powerful hip flexor.
Thigh Region
Gluteal fold
posterior
Hip joint
lateral
Inferior pubic ramus
medial
Inguinal ligament
anterior
Hip
Sensory Control of the Hip
Sensory Pathways
Fasciculus Gracilis: This tract carries fine touch and proprioception signals from the hip, giving the brain information about its position in space.
Anterolateral Tract: This pathway carries pain and temperature sensations from the hip.
Secondary Somatosensory Cortex
This part of the brain helps with spatial memory and tactile memory related to the hip,
information is further processed and stored in the secondary somatosensory cortex.
Primary Sensory Cortex
The anterior cerebral artery supplies the sensory cortex, ensuring the hip’s sensory input is effectively processed.
The sensory information from the hip is processed here, specifically related to touch sensations like shape, size, and texture.
primary sensory cortex, which is located on the medial surface of the brain.
Biomechanics
Gait
Hip Joint Kinematics in the Gait Cycle
Kinetics of the Hip Joint During Gait
Hip Adductors
Activation around 65-70% of the cycle to assist the hip flexors during the swing phase.
Activation at 10% of the gait cycle to assist the hip extensors.
Hip Abductors
Peak activation occurs around 10% of the gait cycle
work eccentrically to control the amount of pelvic drop (or contralateral pelvic depression) during the stance phase, especially between 0% and 10% of the cycle when the opposite leg leaves the ground.
Concentric activation around 70% of the gait cycle, assisting in lifting the femur upward and forward to prepare for the next step.
Eccentric activation around 45% of the gait cycle to limit excessive hip extension.
Hip Extensors (Gluteus Maximus):
activated concentrically in the early stance phase (about 10% of the gait cycle) to extend the hip.
Reverse Actions
External rotation of the hip is observed as contralateral backward pelvic rotation.
Internal rotation of the hip is observed as contralateral forward pelvic rotation.
Hip abduction is seen as contralateral pelvic elevation (the opposite side of the pelvis lifts).
Hip adduction is seen as contralateral pelvic depression (the opposite side of the pelvis drops).
Transverse Plane
It then undergoes another round of internal rotation from **60% to the end of the cycle.
The hip undergoes internal rotation from 0% to 30% of the gait cycle, followed by external rotation from 30% to 60%.
Frontal Plane
Then, the hip adducts again from 65% to 100% of the cycle.
From 20% to 65%, the hip abducts (moves away from the midline).
The hip adducts from 0% to 20% of the cycle (the leg moves toward the midline).
Sagittal Plane
In the swing phase, the hip flexes again from 50% to 80% of the cycle and remains in flexion until the cycle begins again.
During the stance phase, the hip gradually extends from about 10% to 50% of the cycle, reaching a maximum of about 10 degrees of extension.
At the start of the gait cycle, the hip is in approximately 30 degrees of flexion.
Muscle Force
When the angle is closer to 0 degrees, the muscle generates small torques but large translational forces, potentially leading to joint instability or pain.
When a muscle's angle of application is closer to 90 degrees relative to the lever (the femur), it generates large torques and small translations (movements along the joint).
Reverse Actions at the Hip
If the hip flexors are activated, they will flex the hip joint. If the pelvis is fixed and the femur moves, the result is pelvic tilt.
If the hip abductors are activated and the femur is free to move, the result is hip abduction. If the pelvis is free to move instead, the result is contralateral pelvic elevation
Flexion: Accompanied by a spin of the femoral head within the acetabulum.
External rotation: Accompanied by an anterior glide.
Abduction: Accompanied by an inferior glide of the femoral head.
Movement at the Hip Joint
Internal/External Rotation: The hip rotates inward (internal rotation) or outward (external rotation).
Abduction/Adduction: The hip moves away from (abduction) or toward (adduction) the body's midline.
Hip adduction: Occurs when the pelvis drops on the opposite side (contralateral pelvic drop)
Hip abduction: Occurs when the pelvis is lifted on one side (contralateral pelvic elevation).
Flexion/Extension: The hip can flex (bend forward) or extend (move backward).
Muscles
Hip Flexors
Psoas Minor
small muscle, often absent, assists the psoas major.
iliacus and psoas major muscles form the iliopsoas, the main flexor of the thigh at the hip joint.
Gluteal Region
Deep Muscles
Innervation of Deep Muscles
Inferior Gemellus & Quadratus Femoris: Innervated by the nerve to quadratus femoris.
Superior Gemellus & Obturator Internus: Innervated by the nerve to obturator internus.
Piriformis: Innervated by the nerve to piriformis.
Quadratus Femoris
most inferior deep gluteal muscle, contributing to lateral rotation
Obturator Internus
Works with the gemelli to rotate the thigh laterally
Gemelli (Superior & Inferior)
lateral rotation of the thigh.
Piriformis
laterally rotates the thigh.
dividing the gluteal region into superior and inferior parts
Superficial Muscles
Innervation of Superficial Muscles
Actions: All the superficial muscles (except gluteus maximus) are involved in thigh abduction and internal rotation, while the gluteus maximus is primarily involved in hip extension.
Inferior Gluteal Nerve: Innervates the gluteus maximus.
Superior Gluteal Nerve: Innervates gluteus medius, minimus, and TFL.
Tensor Fascia Lata
tightens the fascia lata and assists in abduction and medial rotation of the thigh
anterior aspect of the iliac crest
Gluteus Medius & Minimus
stabilizing the pelvis during walking/running
between the gluteus maximus
Gluteus Maximus
powerful hip extensor
largest and most superficial muscle
spans from the iliac crest (superiorly) to the gluteal fold (inferiorly), and medially to the midline of the body
Sensory Innervation
Superior Gluteal Nerve and Inferior Gluteal Nerve
Occasionally contribute to innervation
Sciatic Nerve
Through the nerve to the quadratus femoris, innervates parts of the posterior capsule.
Obturator Nerve
Provides innervation to the anterior and posterior capsules
Femoral Nerve
Innervates the anterior aspect of the hip joint
Osteology
Hip Joint
round ligament of the femur
inserts into the fovea capitis of the femur. It also carries blood vessels to the femoral head.
rises from the transverse acetabular ligament
acetabular notch
pening inferiorly, bridged by the transverse acetabular ligament.
femur is the only bone in the thigh
Posteriorly
Medial and lateral supracondylar lines (continuations of the lips)
Lateral lip (continuous with the gluteal tuberosity).
Medial lip (continuous with the spiral line).
Anteriorly
Smooth surface
Shaft (Body)
Extends from the intertrochanteric line to the femoral epicondyles
Proximal Region
Intertrochanteric line and crest
Greater and lesser trochanters
Head and neck
Proximal Femur
Gluteal Tuberosity: Attachment site for the gluteus maximus muscle
Pectineal Line: Ridge leading to the base of the lesser trochanter.
Spiral Line: Extends toward the lesser trochanter, continuous with the intertrochanteric line.
Trochanteric Fossa: Depression between the neck and the greater trochanter.
Intertrochanteric Crest: A bony ridge between the greater and lesser trochanters on the posterior side.
Lesser Trochanter: Smaller projection on the posteromedial side at the neck-shaft junction.
Greater Trochanter: Large projection on the lateral and posterolateral side, superior to the neck.
Neck: Narrower than the head, connects the head to the trochanters.
Head: Rounded, with a circular indentation called the fovea capitis.
Pubic Bone and Pelvic Girdle
pubic symphysis is the fibrocartilage plate that articulates the right and left pubic bones anteriorly
Pubic crest, pubic tubercle, and pectineal pubis are located on the superior surface of the superior pubic ramus
pubic bones and inferior/superior pubic rami form the anterior half of the obturator foramen
ramus connects the pubic body to the ilium
Vascular Supply
internal iliac artery
obturator, superior gluteal, and inferior gluteal arteries
contribute to the blood supply
medial circumflex femoral artery
Damage to this artery can lead to avascular necrosis of the femoral head
provides the majority of the blood supply to the femoral head
Ligaments
Ischiofemoral Ligament
It is the weakest of the three ligaments and limits internal rotation during hip rotation
Arises from the ischial part of the acetabular rim and attaches to the posterior base of the greater trochanter.
Located at the posterior part of the joint capsule.
Pubofemoral Ligament
It limits extension, abduction, and possibly external rotation
Attaches to the body and superior ramus of the pubic bone, blending with the inferior band of the iliofemoral ligament.
Located in the lower anterior part of the joint capsule.
Iliofemoral Ligament (Y-Ligament)
It limits hyperextension and external rotation during extension
Attaches from the anterior inferior iliac spine (AIIS) and the adjacent ilium to the greater trochanter and intertrochanteric line.
Knee and lower leg
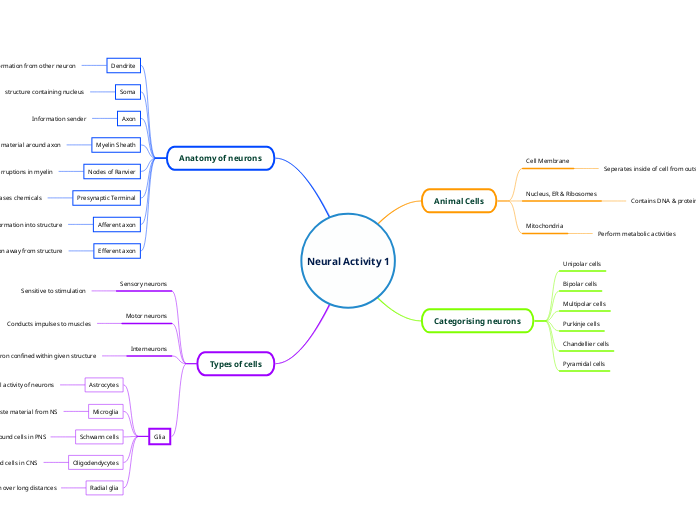
CNS connection
Basal Ganglia's Role in Knee Movement
Stop pathway (indirect pathway): Inhibits movement, helping you stop unwanted movements, such as preventing unnecessary knee flexion at rest.
Go pathway (direct pathway): Facilitates movement by reducing inhibition. This allows you to initiate knee movement when desired.
basal ganglia helps in the initiation, termination, and inhibition of movement, influencing voluntary movement like knee flexion and extension.
Cerebellar Influence on the Knee
The cerebellum communicates ipsilaterally with the spine, meaning information from the lower extremity (knee) remains on the same side of the body.
Spinocerebellum: This part of the cerebellum receives input about unconscious proprioception (joint and muscle position sense) via the posterior spinocerebellar tract. It helps smooth and coordinate movements like walking and ensures accurate landing of the knee during gait.
The cerebellum plays a crucial role in movement coordination, refining movement quality, and maintaining balance.
Motor Control of the Knee
Myotomes for Knee Muscles:
Knee flexors (e.g., hamstrings) are controlled by spinal nerve levels L5-S1.
Knee extensors (e.g., quadriceps) are controlled by spinal nerve levels L2-L4.
Motor Plan Creation
the lateral corticospinal tract transmits the signal to the spinal cord, where it crosses over to the opposite side at the pyramids of the brainstem.
The brain's premotor areas initiate a motor plan, which communicates with the knee portion of the homunculus in the primary motor cortex.
Sensory Input to the Knee
Proprioception & Dermatomes
Pain and temperature sensations travel through the spinothalamic tract.
Proprioception (joint position sense) typically travels via the dorsal columns.
Dermatomes
Posterior knee: S1 & S2
Lateral knee: L5
Anterior knee: L4
Medial knee: L3
Sensory information from the knee comes from joint proprioceptors (which provide information on knee position) and the skin around the knee.
gait
Kinematics
Muscle Activation During Gait
Eccentric Hamstrings Activation
Hamstrings activate eccentrically during the second half of the swing phase to decelerate the lower leg, preparing for controlled foot placement during the next gait cycle.
Hip Flexor Momentum in Swing
The primary driver for knee flexion in the swing phase is the momentum generated by the hip flexors. This momentum is transferred to the lower leg to clear the foot off the ground.
Eccentric Quadriceps Activation
Later in the stance phase, when the knee extends, the quadriceps activation is minimal as it is a passive motion driven by body momentum
During loading response (heel strike to foot flat), the quadriceps control knee flexion under the force of gravity, preventing excessive knee collapse.
Swing Phase (Approx. 40% of the Gait Cycle):
Terminal Swing (75-100% of the gait cycle):
The knee flexors (hamstrings) are activated eccentrically in the latter half of the swing phase to decelerate the shank and control the knee's motion as it prepares to land
Initial Swing (60-75% of the gait cycle):
This flexion is mainly driven by the hip flexors, which generate momentum that is transferred from the thigh to the lower leg (shank).
Maximum knee flexion of around 60 degrees occurs during this phase.
The knee continues to flex to allow the foot to clear the ground.
Stance Phase (Approx. 60% of the Gait Cycle)
Mid Stance (15-40% of the gait cycle)
During this phase, the quadriceps show minimal activation because the extension is more passive, driven by body motion rather than active muscle contraction.
As the body moves forward, the knee extends. This extension is largely driven by the forward momentum of the trunk and pelvis, as the foot remains fixed to the ground.
Pre-Swing (40-60% of the gait cycle):
The knee flexes again slightly, preparing for the toe-off (when the foot leaves the ground).
Loading Response (0-15% of the gait cycle):
Quadriceps Activation: The quadriceps work eccentrically to control this flexion and resist the external flexion moment generated by gravity (which acts posterior to the knee joint).
The knee flexes further to absorb the initial impact and body weight as the foot makes contact with the ground.
Initial Position
The knee starts in about 5 degrees of flexion.
biomechanics
Arthrokinematics:
Patellofemoral Joint
During flexion, the patella glides inferiorly (downward).
During extension, the patella glides superiorly (upward).
patella acts as a pulley for the quadriceps muscle, increasing the moment arm and improving the force output during knee extension.
Screw-Home Mechanism
Contributors
Slight external rotation of the tibia.
Slight lateral pull of the quadriceps.
Tension in the ACL.
Shape of the medial femoral condyle (longer and more curved than the lateral condyle).
slight lateral rotation of the tibia during knee extension, allowing the knee to "lock" in place.
Role of the Cruciate Ligaments
Posterior Cruciate Ligament (PCL
Becomes taut during knee flexion.
Function: Limits posterior glide of the tibia relative to the femur and anterior glide of the femur relative to the tibia.
Anterior Cruciate Ligament (ACL)
Becomes stretched during knee extension.
Function: Limits anterior glide of the tibia relative to the femur and posterior glide of the femur relative to the tibia.
Closed-Chain Movements
During flexion, the femur glides anteriorly.
During knee extension, the femur glides posteriorly.
When the femur moves relative to the tibia (e.g., during squat), the roll and glide occur in opposite directions.
Open-Chain Movements
During flexion, the tibia glides posteriorly.
During knee extension, the tibia glides anteriorly.
When the tibia moves relative to the femur (e.g., during leg extension), the roll and glide occur in the same direction.
Knee Osteokinematics (Range of Motion)
Abduction/Adduction: These motions do not occur actively at the knee but can be available passively by about 6 degrees.
Rotation: Internal and external rotation is only possible when the knee is flexed. External rotation typically has about 30 degrees, while internal rotation is about 15 degrees.
Extension: The knee can extend beyond 0 degrees, usually up to about 5-10 degrees.
Flexion: The knee can flex up to about 140 degrees in most people.
Menisci Functions
Reduce friction during joint movement.
Act as shock absorbers, although eccentric muscle contractions are more critical in absorbing shock.
Increase the concavity of the tibial condyles to better distribute weight.
Reduce compressive stress on the articular cartilage.
Ligamentous Laxity and Knee Flexion
Rotation (internal and external) in the knee is only possible when the knee is flexed because the ligaments tighten with extension.
As the knee extends, the ligaments become taut (tightened) due to their anatomical positioning posterior to the knee joint axis.
muscles
Pes Anserine Muscles
These muscles are important for stabilizing the knee, especially on the medial side.
Gracilis
Sartorius
Knee Flexors:
Muscles:
Hamstring Group (Primary Knee Flexors):
flex the knee and extend the hip
Biceps Femoris
Semitendinosus
Semimembranosus
innervention
sciatic nerve innervates the muscles responsible for knee flexion.
Knee Extensors
Muscle
Sartorius Muscle:
assists in internal rotation of the knee and flexion of the hip joint. It also contributes to stabilizing the medial aspect of the knee.
Quadriceps Femoris (Primary Knee Extensors):
These muscles work together to extend the knee joint during movements like standing, walking, and running.
Vastus Intermedius: Situated between the vastus lateralis and vastus medialis.
Vastus Medialis: Located on the inner side of the thigh.
Vastus Lateralis: Located on the outer side of the thigh.
Rectus Femoris: A central muscle that also assists with hip flexion.
Innervation
femoral nerve innervates the muscles responsible for knee extension.
joints and ligaments
Menisci:
The popliteus muscle has attachments to the lateral meniscus.
The semimembranosus muscle attaches to the medial meniscus.
C-shaped fibrocartilage structures
thicker on the outside and thinner on the inside
Provide proprioception
Improve congruency
Reduce localized pressure
Ligaments of the Knee:
Posterior Cruciate Ligament (PCL):
Limits posterior translation of the tibia relative to the femur (prevents the tibia from sliding backward).
Anterior Cruciate Ligament (ACL):
Limits anterior translation of the tibia relative to the femur (prevents the tibia from sliding forward).
Lateral Collateral Ligament (LCL):
Limits varus stress (prevents the knee from being pushed outward).
Medial Collateral Ligament (MCL)
Limits valgus stress (prevents the knee from being pushed inward).
Knee Joint Articulations
Patellofemoral Join
The articulation between the patella (kneecap) and the femur (specifically the patellar groove of the femur).
Femorotibial Join
The articulation between the distal femur (femoral condyles) and the proximal tibia (tibial plateau).
osteology
Q Angle (Quadriceps Angle)
typically ranges between 10 to 15 degrees, but anything greater than 20 degrees is considered abnormal.
formed between two lines:
from the center of the patella to the center of the tibial tuberosity (where the patellar ligament attaches).
from the ASIS (anterior superior iliac spine) to the center of the patella.
Knee Alignment
Varus
bow leg, this is when the tibia turns inward relative to the femur, causing the knees to point outward
Valgus
knock knee, this is when the tibia turns outward relative to the femur, causing the knees to point inward.
Tibia and Fibula
Fibula:
not involved in the knee joint. It serves mainly for muscle attachment and stability of the leg but does not contribute to the knee's articulation.
Tibia (Shank of the Leg):
medial tibial plateau is C-shaped, and the lateral tibial plateau is O-shaped,
proximal tibia has a tibial plateau, which consists of the medial and lateral condyles, where the femur articulates.
Distal Femur
Patella
patella sliding superiorly during knee extension and inferiorly during knee flexion.
posterior surface of the patella is shaped to fit into the patellar groove (or trochlear groove) of the femur
patella is a sesamoid bone
Condyles and Epicondyles
condyles
articulate with the tibial plateau
epicondyles
bony prominences located just above the condyles, serving as attachment points for muscles and ligaments.