Clinical example:
The client was a 28-year-old Maori female admitted to the mental health ward for depression, anxiety and suicidal ideations. The client was visibly anxious after having dinner in the dining room with other clients for the first time since admission. Using nursing observation skills, I noticed she was shaking, breathing heavily and sweating, upon talking to the client she stated she had racing thoughts, nausea and a feeling of impending doom. Using empirical knowledge of anxiety, I concluded that she was experiencing an exacerbation of anxiety.
As the client was unable to settle herself, I decided an intervention was required. As it was indicated, I discussed giving PRN lorazepam to lessen her symptoms. She declined this as she stated that her family are against pharmaceuticals and prefers a more natural intervention for her mental health. Considering this cultural value, I used my own personal experience with anxiety to empathise with the client’s feelings. I was able to share tips for reducing anxiety that have worked for me such as breathing and exercise. Utilising the personal ways of knowing helped further develop a therapeutic relationship with the client through shared experiences.
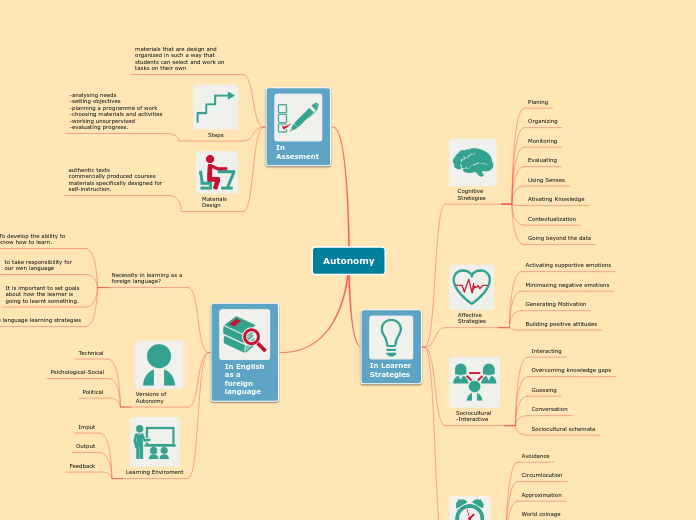
The client states her goals are to be able to go into the supermarket without experiencing an anxiety attack, and not requiring medication for her chronic depression/anxiety. This was the client’s own definition of good health despite having chronic mental health issues, which may be different to a nurse’s definition of well-health. Allowing the client to make their own decision to decline or accept medication is underpinned by the ethical way of knowing, through autonomy. A patient keeping autonomy would allow mental and spiritual health, therefore physical health is maintained for the best holistic outcomes of the client.
To decrease the client’s anxiety a change in environment was needed, in the dining hall it was very loud and overstimulating. By moving to her room, a manipulation in environment created a more appropriate space for reducing anxiety and peace. By closing the curtains, turning on calm music and practicing deep breathing this created an external space conductive to calmness. Knowledge of creating a peaceful environment is supported by the aesthetic ways of knowing, as all aspects of the individual must be considered to provide holistic care.
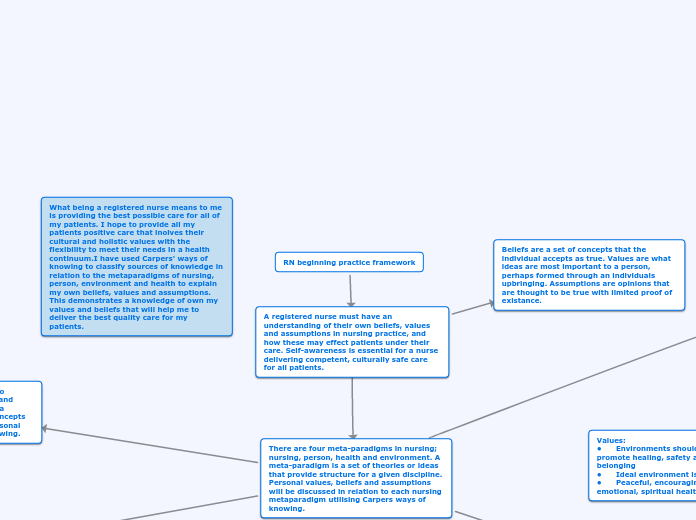
What being a registered nurse means to me is providing the best possible care for all of my patients. I hope to provide all my patients positive care that inolves their cultural and holistic values with the flexibility to meet their needs in a health continuum.I have used Carpers' ways of knowing to classify sources of knowledge in relation to the metaparadigms of nursing, person, environment and health to explain my own beliefs, values and assumptions. This demonstrates a knowledge of own my values and beliefs that will help me to deliver the best quality care for my patients.
RN beginning practice framework
A registered nurse must have an understanding of their own beliefs, values and assumptions in nursing practice, and how these may effect patients under their care. Self-awareness is essential for a nurse delivering competent, culturally safe care for all patients.
Beliefs are a set of concepts that the individual accepts as true. Values are what ideas are most important to a person, perhaps formed through an individuals upbringing. Assumptions are opinions that are thought to be true with limited proof of existance.
There are four meta-paradigms in nursing; nursing, person, health and environment. A meta-paradigm is a set of theories or ideas that provide structure for a given discipline. Personal values, beliefs and assumptions will be discussed in relation to each nursing metaparadigm utilising Carpers ways of knowing.
Environment
The environmental aspect focusses on the surroundings that effect the patient. A person’s health and wellbeing may be influenced by internal or external environments. Internal environments involve physiological, psychological, spiritual and sociocultural status. External factors may involve location, economic status, social interactions and culture. The environmental relationship to health is known by empirical knowledge, as the impact of negative environments is supported by extensive scientific research. This is evident in housing situations, as people in cold, damp and overcrowded houses are more likely to experience illness than those living in warm, dry and sufficient housing. A person’s environment should be stable, peaceful and promote healing. Aesthetic ways of knowing are also used, as providing a person-centred approach to creating a peaceful environment is important for individual healing needs.
Nightingale’s environmental theory states that the nurse’s role in patient recovery is to change their environment to the ideal conditions for the body to heal. My role would be to discuss the patient’s environment and educate on how to improve the patient situation for best health. It must be considered that my knowledge of different environments may be limited, and the patient will be best able to understand their environment. This education should be delivered in a non-judgemental manner, as my definition of a good environment may differ to my patients, and it may be difficult for a person to change their environment.
Assumptions: • My values and experiences will be different to those of my patients
• My knowledge of different environments may be limited
• The patient will best understand their own environment
Beliefs: • Environments may be internal or external
• A persons environment directly influence their health
• It may be difficult for a person to change their environment for better health
Values: • Environments should be stable and promote healing, safety and a sense of belonging
• Ideal environment is warm, dry, clean
• Peaceful, encouraging physical, emotional, spiritual health
Health
Health is a dynamic process of wellness and illness defined by the client’s perception of their wellbeing. A person’s health is not static and differs over an individual’s lifespan. Health is much more than physical wellbeing, and involves supporting the patient’s social, spiritual and mental health for best health outcomes. Patient’s determine their own definition of health and this may vary between cultures which the nurse should respect. These values, beliefs and assumption have been formed through aesthetic and ethical ways of knowing. The ethical value of autonomy has allowed me to comprehend that patients decide their definitions of health and make their own decisions to best maintain their own mental, spiritual and family health. Aesthetic ways of knowing are utilised through the holistic consideration of all components of a patient. Through my nursing journey I have learnt that health may exist with the presence of disease. It is possible to be healthy while living with a chronic disease which I, as a nurse, am able to help support patients to maximise their wellbeing. I believe my role as a nurse is to work closely with patients to determine their own definition of health and goals. I support these goals with health promotion and education to empower the patient to manage their own health, while being flexible to change as per the health continuum.
Assumptions: • Cultural definitions of health may differ
• Patient decides what health means to them
Values:
• Te whare tapa wha • Healthcare should provide disease prevention education to improve health
• Promoting best level of health for all
Beliefs: • Health is not static and exist on a continuum
• Health may exist in the presence of disease
Person
The person metaparadigm focuses on the receiver of care as an individual, considering their social, spiritual and physical needs. This may also involve incorporating family into healthcare if the patient wishes. Each person has been shaped by their experiences and therefore hold different values and beliefs, especially within healthcare. Previous negative experiences in healthcare may impact the ability to form a therapeutic relationship with a client, however, Carpers personal ways of knowng may help a nurse to overcome this. I use knowledge from my own personal experience with building relationships in a professional setting to overcome these barriers, often using active listening skills to build rapport. In my nursing style, I strongly focus on creating a therapeutic relationship with my patients. Having a therapeutic relationship my patient to discuss their cultural, physical and spiritual needs and work in partnership to care plan for best outcomes. My beliefs are supported by Rodger's client-centred therapy theory, which states best outcomes are achieved when interventions are structured for the needs of the client and allow participating in care planning. By having a strong therapeutic relationship with a client, the best interventions to support them may be decided.
Assumptions: • Nurses own values/beliefs should be addressed to not impact patient care
• Patient participation in care will improve overall wellbeing
Beliefs:
• A person’s culture will impact their needs, values and beliefs in healthcare
• There may be barriers to forming a therapeutic relationship due to previous healthcare experiences
Values: • Holistic care
• Therapeutic relationships
• Family/Whanau impact
• Empathy
Nursing
Assumptions: • Nursing care is dynamic, and changes with individual needs
• Nursing care is best with a holistic, patient centered approach
Beliefs: • Effective communication with clients and interdisciplinary team is essential for best outcomes
• Evidence based practice is essential for enabling health
• Being respectful of an individual’s dignity, culture and values is essential for providing culturally safe care • The individual decides their own health needs
Metaparadigm definition and discussion
At the beginning of my journey, I believed that nursing was simply taking care of biomedical needs. The role of a nurse is a complex art that incorporates science and research while providing care that considers the person's needs, beliefs and values for best possible health outcomes. Nursing involves Carpers' aesthetic and empirical ways of knowing. Nursing practice is underpinned by a range of sciences and evidence-based research, therefore demonstrating the use of empirical knowledge. Science is utilized to have an understanding of the biomedical situation and develop interventions to address any issues for physical wellbeing. Nursing is both a process and product. Aesthetic ways of knowing are incorporated through a holistic approach involving consideration of the patient situation, culture and developing an individualized care plan. Maslow's theory supports the aesthetic ways of knowing, as the theory states that concentrating on individual self-efficacy, self-actualisation and free will allows people to fufil potential and therefore maximise wellbeing. This allows for me to consider all aspects of the individual, apply science to understand the situation and form interventions that will support the patients physical and mental health.
Nursing values: • Respect and support
• Manakitanga
• Autonomy and independence
• Knowledge and skills
• Advocacy
• Equitable care • Science underpins nursing practice
Carpers' ways of knowing is a tool to classify sources from which beliefs and knowledge has been formed within a clinical practice setting. The four concepts in Carpers' way of knowing are; personal empirical, ethical and aesthetic knowing.
Aesthetic: Considers all elements for a patient-centered holistic approach
Ethical: a development in moral and ethical codes for self and nursing practice
Empirical: Knowledge found from objective facts, science and research applied for evidence-based practice
Personal: knowledge gained through personal experience, self-assessment, observation and relationships