Acid-Base Disorders
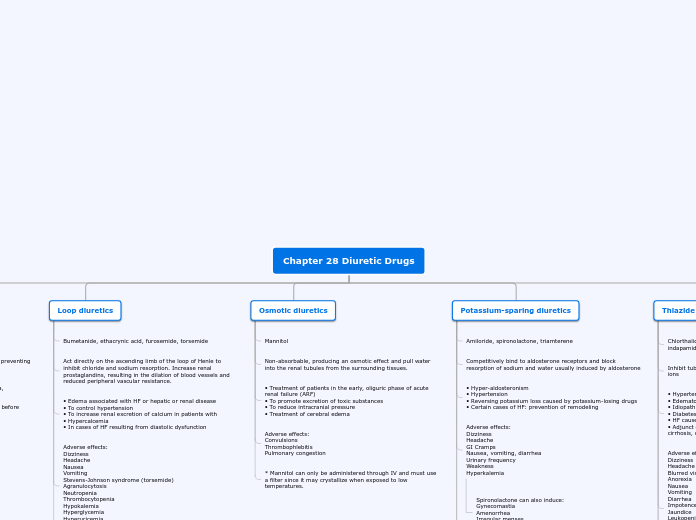
pH > 7.45
Alkalemia
Respiratory
Hyperventilation
Secondary response:
Bicarb generationCellular buffering & RenalHepatic failure
Distress
Pregnancy
Pain
Anxiety
Hypoxemia
CNS lesions
Metabolic
Gain of bicarb or loss of H+
Secondary response:
Decreased ventilationCl- resistant
Stimulates Aldo
Severe hypokalemia
RAAS, Adrenal tumors
Cl- sensitive (volume depleters)
Vomiting
Loop, Thiazide Diuretics
Decreased ECV
Increased RAAS
Increased Aldo
Decreased H+, K+
pH < 7.35
Acidemia
PCO2
> 45
Compensatory response to respiratory acidosis
Causes
Miscellaneous
Obesity
Hypoventilation
Pulmonary
Parenchyma
Airway
Neuromuscular
Central
Anesthetics
Infection
Stroke
Compensatory Rate
4 Bicarb per 10 pCO2
Chronic Respiratory Acidosis (Single Disorder)
1 Bicarb per 10 pCO2
Compensation not as good: needs to regenerate bicarb
Acute Respiratory Acidosis (Single Disorder)
< 35
Compensatory response to metabolic acidosis
(Hyperventilation)
HCO3
> 28
Mixed
< 24
Metabolic Acidosis (Single)
Anion Gap
> (10-12)
High AG
Delta Ratio
>3
High AG + concurrent met. alk or pre-existing comp. resp acid
1-2
Pure High AG Acidosis
<1
High AG & Normal AG acidosis
<0.4
Hyperchloremic normal anion gap acidosis
Osmolar Gap
> (10-15)
Think ingestion
Propylene glycol
Ethylene glycol
Produces glycolic, oxalic acids
EtOH
Methanol
Methanol/formaldehyde intoxicatoin
Produces formic acid
Rx: Dialysis
10-15
MUDPILES
Salicylates
Also causes respiratory alkalosis (BRS phys)
Lactic acid
Hypoxia
Rx: Pressors
INH
TB Rx
Young women, Suicide
Paraldehyde
DKA
Acetoacetic acid
B-OH-butyric acid
Rx: Insulin
Uremia
Typically doesn't get that high because we dialyze before they get that sick.
GFR < 15-20
Rx: Dialyze
Malnutrition
10-12
Hyperchloremic
Urine anion gap
> -20
Renal
RTA of renal insufficiency
GFR usu. >15 ml/min
Hyperkalemic
Type 4 RTA
Hyporeninemic, hypoaldosteronemic distal RTA
Most common seen
Diabetic patients
You can generate a Type 4 RTA w/ drugs that limit Aldo fx on kidney
ACEARBAldo antagonistsKidney for some reason doesn't respond to aldosterone
OR aldosterone effects on kidneys are being blocked (drugs)
Hypokalemic
NH4CL Admin.
No change in Urine pH
Classical distal RTA
Type 1 (only because it was discovered first)
Proton back leak distally
Amphotericin B (makes holes)K+ leaks out (hypokalemic) to compensate
Urine pH < 5
Proximal RTA
Rare (Paraproteinemias --> Excessive amt of a single monoclonal gammaglobulin in the blood)
Waldenstrom's macroglobulinemia
AmyloidosisMultiple myelomaAbnormal protein damages the proximal tubule
Iatrogenic
CA inhibitors (Acetazolamide)GentamicinPart of generalized disorder of proximal tubular function known as --> Fanconi syndromeSelf-limiting
Problem w/ Bicarb reabsorption --> Serum bicarb load delivered to kidney reduces, so kidney can handle new steady state due to distal effects
Aldosterone action leads to hypokalemia
HCO3 not reabsorbed --> Na+ travels with it --> juxtaglomerular apparatus senses sodium load passing through --> secretes renin --> Angiotensinogen to Angiotensin I (by renin)--> AgI to AgII (by ACE) --> Vasoconstriction + Aldosterone stimulation --> sodium intake distally, potassium excreted --> hypokalemia
< -20
Extrarenal
Ext. loss of secretions in GI
Biliary
Pancreatic
Diarrhea