Female Reproductive System by hetal vithalani
Not for commercial purpose
just a personal notes .....
Ovary
Ovary
functional uinit - folicle
follicle consists of an an oocyte surrounded by granulosa and theca cells
- LH acts on THECA cells to induce androgen production
-FSH stimulates granulosa cell to converst androgen to estadiol
-Estradiol surge induces an LH surge which lead to ovulation
after ovulation the ressidul folicle becomes a corpus leteum
primary secretes progesterone
homorrhage in to a corpus luteum -> cyst
degeneration of follicales results in follicular cysts small numbers of follicular cysts are common in women and have no clinical significance.
Ovarian Tumors
Germ Cell Tumors
GERM CELL TUMORS
in women of reproductive age
Tumor subtyes mic tissues normally produced by germ cells.
Fetal tissue - cystic teratoma and embryonal carcinoma
Oocytes - dysgerminoma
Yolk sac - endodermal sinus tumor
placental tissue - choriocarcinoma
cystic teratoma
1. cystic tumor composed of fetal tissue derived from two or three embryologic layers
2. benign, but presence of immature tissue or somatic maliganacy indicates maligant potential.
struma ovarii is a teratoma composed primarily of thyroid tissue.
dysgerminoma
1. tumor composed of large cells with clear cytoplasm and central nuclei most common malignant germ cell tumor
2. testicular counterpart is called seminoma, which is a relatively common germ cell tumor in males.
good prognosis reponds to radiotherapy
serum LDH may be elevated
Endomdermal sinus tumor
Malignant tumor that mimics the yolk sac most common germ cell tumor in children
serum AFP is often elevated
schiller - duval bodies are classically seen on histolgy
Choriocarcinoma
malignnt tumor composed of trophoblasts and syncytiotropoblasts mimics placental tissue but villi are absent
small hemorrhagic tumor with early hematogenous spread
High b-hcg is characteristic s may lead to thecal cysts in the ovary
poor response to chemotheraphy
Embryonal carcinoma
malignant tumor composed of large primitive cells
aggressive with early metastasis
cystadenocarcinoma - is the only one has psammoma bodies
A 47-year-old woman has noted a pressure sensation, but no pain, in her pelvic region for the past 5 months. On physical examination there is a right adnexal mass. An ultrasound scan shows a 10 cm fluid-filled cystic mass in the right ovary. A fine needle aspirate of the mass is performed and cytologic examination of clear fluid aspirated from the mass reveals clusters of malignant epithelial cells surrounding psammoma bodies. Which of the following neoplasms is she most likely to have?A Endometrioid carcinomaB Serous cystadenocarcinomaC Malignant mesotheliomaD Mature cystic teratomaE Tubal adenocarcinoma
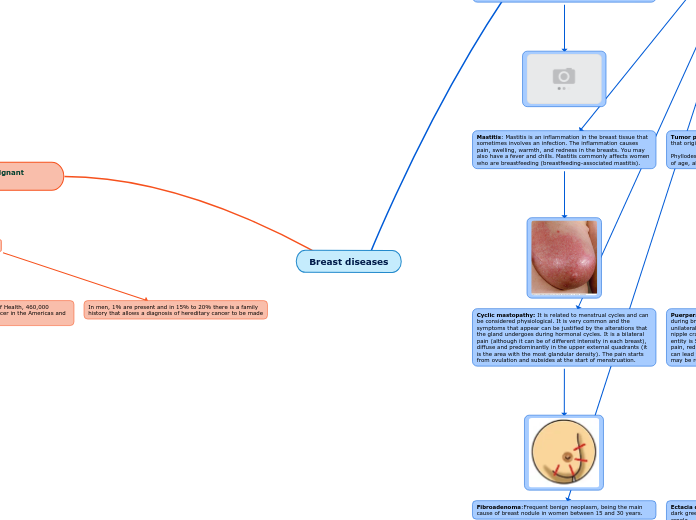
Surface Epithelial tumors
- most commen overian tumor (70%)
derived from coelomic ( overy line )
- two kinds (both can be benign or maligant or borderline)
1. serous tumors are full of watery fluid
2. Mucinous tumors are full of mucus like fluid
benign tumors (cystadenomas ) are composed of a single cyst - all benin tumore symptoms )
Maligant tumors (cystaadenocarcinomas) are composed of complex cysts with a think , shaggy lining most commen in post menopausal women
clinically presentation
vague abdominal symptoms or signs of compression (urinary frequency)
borderline tumors have both kind of characteristic
BRCAI mutation carriers have an increased risk for serous carcinoma of the overy and fallopian tube
Polycystic ovarian Disease
- multiple ovarian folicular cysts due to hormone imbalance
-reproductive age
- high LH and Low FSH (LH :FSH >2)
Increased LH induces excess androgen production from theca cells resulting in hirsusim ( hair like man)
- androgen is converted to estrone in adipose tissue
- estrone feedback decrese FSH resulting in cystic degenration of folicles
-high levels of circulating estrone increase risk for endometrila carcinoma
- obbies young women, infertility, oligomenorrhea and hirsutism - some have insulin resistance and may develop type 2 diabetes in later life
Endometrium And Myometrium
Endometrium is the mucosal lining of the Uterine cavity
Myometrium is the smooth muscle wall underlying the endomerium
Endometrium is hormonally sensitive
growth of the endometrium is estrogen driven
preparation of the endometrium for implantation is progestrone driven
shedding occurs with loos of progestrone support
Leiomyosarcoma
Leiomyosarcoma
- maligant
smooth muscle arising from the myometrium
arises de novo - does not come from liomyomas
in post monoposal women
gross exam often shows a single lesion with areass of necrosis and hemorrhage
mitotic activity and cellular atypia
Leomyoma
-Benign neoplastic profliferation of smooth muscle arising from myometrium most common tumore in female
-prementopausal women
often multiple
enlarge during pregnancy
shrink after menopause
asymptomatic
The cause of uterine fibroids is unknown, but evidence suggests that their growth is tied to estrogen.
Endometrial Carcinoma
Endometrial carcinoma
- malignant
-most commen of female
-Postmenopausal bleeding
-via two different pathway
1. Hyperplasia - (75% ) cases, estrogen exposure late menopause, nuliparity, infertility with anovulatory cycles and obesity -around 60 year of age.
2. Sporadic (25%) carcinoma arises in an atropic endometrium with no evident precursor lesion - age is around 70 - papillary structure with psammoma body formation - p53 mutation is common and the tumore exhibits agrresive behavior
Endometrial Hyperplasia
Endometrial hyperplasia
hyperplasia of endometrial glands relative to stroma
occurs as consequence of unpopposed estrogen
- Post menopausal uterine bleeding
architectural growth pattern
absence of cellular atypia -> precursure to carcinoma
cellular atypia inverse relationship to carcinoma
Subtopic
Endometriosis
Endometrial glands and stroma outside of the uterine endometrial lining most likely due to retrograde menstrauation with implantation at ectopic site
presents as dymenorrhea and pelvic pain may cause infertility.
endometriousis cycles just like normal endometrium
most common site of involvment is the overy, which classically results in formation of a chocolate cyst
other sites of involvement include the uterine ligament (pelvic pain ) pouch of abdominal pain and adhesion) , fallopian tube mucosa (scarring increases risk for ectopic tubal pregnancy) implants classically appear as yellow brown "gun powder" nodules
involvement of the uterine myometrium is called adenomyosis
increassed risk of carcinoma at the site of endometriosis (overy)
Endometrial polyp
Endometrial polyp
Hyperplastic protrusion of endometrium
presents as abonormal uterine bleeding
can arise as a effect of tamoxifen, which has anti estrogenic effects on the breast but week pro estrogenic effects on the endomerium
Cronic Endometritis
Cronic Endometritis
cronic inflamation of the endometrium
lymphocytes and plasma cell
plasma cells are necessary for the diagnosis of chronic endometritis given that lymphocytes are normally found in the endometrium
causes includes relained products of conception chronic pelvic inflammatory disease such as chlamydia IUD and TB
abnormal utrine bleed, Pain, and infertility
Acute endometritis
Acute endometritis
bacterial infection of the endometrium
usally due to retained product of conception ex after baby or miscarriage
presents as fever abnomal utrerine bleeding and pelvic pain
Anovulatitory cycle
Lake of ovulation
Results in an estrogen driven proliferative phase without a subsequent progestrone driven secretory phase
proliferative glands break down and shed resulting in uterine bleeding
reprsents a common couse of dysfunctional uterine bleeding especially during menarche and menopose
ASHERMAN SYNDROME
ASHERMAN SYNDROME
Secondary amenorrhea due to loss of the basalis and scarring
result of overaggressive dilation and curettage ( D&C)
Cervix
Neck of the uterus
devides in to the exocervix and endocervix
endocervix is lined by single layer of columnar cells
junction between the exocervix and endocervix is called the transformation zone
Circival carcinoma
Invasive carcinoma that arises from the cervical epithelium
most commonly seen indiddle aged women
presents as vaginal bleeding especially postcoital bleeding or cervical discharge
key risk factor is high risk HPV infection
most common subtypes of cervival carcinoma are squamous cell carcinoma and adenocarcinoma
Advanced tumors often invade through the anterior uterine wall into the bladder. blocking the ureters. hydronephrosis with posternal failure is a common cause of death in advaced cervical carcinoma
Cervical Intraepithelial Neoplasis
Cervical Internaepithel Neoplasia
koilocytic change
disordered cellular maturation
neuclear atypia
increased mitotic activity within the cercical epithelium
Divided into grades based on the externt of epithelial involvement by immature dysplastic cells
CIN1 involves <1/3 of the thickness of the epitheliam
CIN II involves <2/3 of the thickness of the epithelum
CIN III involves slightly less than the entire thickness of the epithelum
carcinoma in situ CIS involves the enteire thinckness of the epithelium
CIN classically progresses in a stepwise fashon throgh CINI, CINII CIN III and CIS to become invasive squamous cell carcinoma
Progression is not inevitable
the higher the grade of dysplasia the more likely it is to progress to carcinoma and the less likely it is to regress to normal.
HPV
HPV - Virus -in transformation zone
infection is usally eradicated by acute inflammation persistent infection leads to an incresed risk for cervical dysplasia.
risk cin depends on HPV type, which is determinded by DNA sequencing
High risk -HPV types 16, 18, 31, 33
Low risk - HPV types 6 and 11
High risk HPV produce E6 and E7 proteins which result in incresed destruction of p53 and Rb, respectively, Loss of these tumor supperssor proteins increases the risk for CIN
Vagina
canal leading to the cervix
mucosa is lined by non keratinizing squamous epithlium
Vaginal Carcinoma
Vaginal Carcinoma
carcinomaarising from squamous epithelium lining vaginal mucosa
usally related to high -risk HPV
precursor lesion is vaginal intraepithelial neoplasia (VAIN)
when spread to regional lymph nodes occurs cancer from the lower 2/3 of vagina goes to inguinal nodes and cancer from the uper 1/3 goes to reginonal iliac nodes
A 30-year-old woman has taken oral contraceptives for a year. For the past 3 weeks she has noted vaginal bleeding that is not severe, but it occurs nearly every day. On pelvic examination, there is a 0.8 cm polypoid mass noted to extend outward from the endocervical region. The ectocervix appears normal. The uterus is normal in size. The adnexa have no palpable masses. A biopsy of this lesion is performed. Which of the following pathologic findings is most likely to be found on microscopic examination of this lesion?A Endocervical adenocarcinomaB Clear cell adenocarcinomaC Microglandular hyperplasiaD Sarcoma botryoidesE Endocervical polypF Follicular cervicitis
answer is Microglandular hyperplasia
Embryonal Rhabdomyosarcoma
Embryonal Rhabdomyosarcoma
malgnant Mesenchymal proliferation of immature skeletal muscle
Rare
presents as bleeding and a grape like mas protruding from the vagina or penis of a chold usaly <5 year of age
also known as sarcoma botryoides
cell exhibits cytoplasmic cross striatrions and positive immunohistochemical staining for desmin and myogenin
Clear cell Adenocarcinoma
Malignat proliferation of glands with clear cytoplasm
rare but feared, complication of DES vaginal adenosis
Discovery of the complication -abnomality of gynecologic tract
due to DES uses
Adenosis
Adenosis
young women exposed diethylstibestol (DES) in utero
focal presistence of columnar epithelium in the uper 1/3 of vagina
during developent squamous epithelium from the lower 2/3 of the vaginal grow upward to replace the columnar epithelium lining of the uper 1/3 of the vagina
Vulva
Anatomicaly includes the skin and mucosa of the female genitalia external to the hymen
labia majora
labia minora
mons pubis
and vesibule
Lined by squamous epithelium
Extramamary Paget Disease
malignant epithelial cells in the epidermis of the vulva
pruritic
ulcerated valvar skin
carcinoma in situ - no underlining
nipples are also associated
paget cells are PSA +Keratin + and s100_
melanoma is PSA + Keratin and S100+
Vulvar Carcinoma
Vulvar carcinoma
Carcinoma arising from suqmous epithelioum lining the vulva
-Rare cancer
Leukoplakia - Biopsy may be required to distinguish carcinoma from other causes of leukoplakia
Posibility of HPV - 16 & 18
none HPV exist too -due to cronic inflamation and irritation eventually lead to carcinoma -women >70
Arises from Vulvar intraepithelial neoplasis
dysplastic precursor lesion - kilocytic change
nuclear atypia
increase mitotic activity
Lichen Simplex chronicus
Lichen Simplex Chronicus
hyperplasis of the vulvar squamous epithelium
presents as leukoplakia with thick leathery vulvar skin
due to cronic irritation and scraching
no reisk of suqmous cell carcinoma
Lichen Sclerosis
Lichen Sclerosis
Thining of epidermis and fibrosis of the dermis
Present with white patch
common in post menopausal women
autoimune etiology
benign but associated with a slightly increased risk for squamous cell carcinoma
Condyloma
Condyloma
Neoplasm of vulvar skin often large
Due to
HPV 6 or 11 -koilocytes
Syphlis (condyloma latum)
Sexually transmited
Bartholin Cyst
Bartholin Cyst
one bartholin gland is present on each side of the vaginal canal and produces mucus like fluid that drains via ducts in to the lower vestibule.
common in women at reproductive age
painful cystiv lesion at the lower vestibule adjacent to the vaginal canal