The Heart!!
Heart Beat
Nervous System Influence
- The autonomic nerve system controls contractility and heart rate.
- The sympathetic nervous system of the ANS increases heart rate and contractility when norepinephrine is released which binds to receptors in cardiac muscle cells. This boosts pacemaker activity in the SA node and raises heart force of contraction.
- The parasympathetic nervous system of the ANS generates acetylcholine by attaching to receptors on cardiac muscle cells and is regulated by the vagus nerve which reduces heart rate. This reduces heart rate by lowering the SA node's pacemaker activity.
Physiological Events
- Atrial contraction is the result of the right SA node initiating an electrical impulse to start the heartbeat.
- The atria contractsas the impulse quickly passes through conducting pathways.
- Due to the impulse, the atria constrict (atrial systole), forcing blood into the ventricles.
- The impulse is delayed at the AVnode, enabling the atria to complete its contraction and ensuring the ventricles have sufficient blood before beginning contraction.
- The signal is transmitted to the ventricles via the Purkinje fibers (bundle of His), once the AV node is delayed.
- The right and left ventriclessupply the aorta and pulmonary artery with blood, this process is initiated by the impulse that causes the ventricles to contract, or enter ventricular systole.
- After contraction, the heart muscle relaxes (diastole) and chambers fill with blood before the next pulse.
Pacemaker Potentials
- Action potentials are produced automatically by SA nodes.
- Pacemaker Potentials: is defined as the membrane potential's gradual depolarization toward the action potential firing threshold. Both potassium ion efflux and sodium ion influx are responsible for this slow depolarization.
- Threshold: Calcium channels open to allow a quick influx of calcium ions into the cell when membrane potential reaches a particular threshold.
- Depolarization: The action potential rises as a result of the calcium ion influx quickly depolarizing the membrane potential.
- Repolarization: The membrane potential repolarizes when potassium channels open after depolarization, allowing potassium ions to leave the cell.
Regular Contractions
sk
Altering Cardiac Output
Norepinephrine Influence
r
Influences on Each Other
- Cardiac output (CO) = heart rate (HR) x stroke volume (SV)
- Increased cardiac output is a result of elevated heart rate or stroke volume.
- Increased cardiac output results from a rise in heart rate without a corresponding drop in stroke volume.
- Greater cardiac output will also arise from an increase in stroke volume in the absence of a corresponding drop in heart rate.
- A drop in cardiac output will result from a drop in heart rate or stroke volume.
Cardiac Output, Heart Rate & Stroke Volume
- Cardiac output: The quantity of blood that each ventricle pumps out in a minute
- Heart rate: The quantity of beats per minute. Both the sympathetic and parasympathetic nerve systems are in control of it. Typically, elevated sympathetic stimulation, which can occur during physical exertion or stressful circumstances, causes the heart rate to rise, while parasympathetic activity causes it to decrease. Heart rate can also be regulated due to age, chemicals, gender, etc.
- Stroke volume: The amount of blood that each ventricle pumps out throughout a heartbeat. Is affected by preload (the cardiac muscle's level of stretch), contractility (the force at which the fibers of the heart muscles contract), and afterload (the back pressure that arterial blood exerts). A greater stroke volume is typically the outcome of increased preload and contractility.
Cardiac Muscle Cells
Comparison with Skeletal Muscle
- Skeletal muscle is multinucleated, but cardiac muscle has a single nucleus per cell.
- Skeletal muscle cells lack the intercalated discs that connect cardiac muscle cells to facilitate quick transmission of electrical impulses.
- Cardiac muscle cells T tubules are wider and less than in skeletal muscle
- Self-excitatory cardiac muscle cells exist.
- The heart beats in unison.
- The extracellular fluid's Ca 2+ influx causes the SR's Ca 2+ release.
- Cardiac muscles are incapable of undergoing tetanic contractions.
- Aerobic respiration is the heart's primary means of energy production.
Unique Physiology
- The cardiac conduction system controls involuntary contraction.
- Before contracting, cardiomyocytes go through depolarization which occurs due to a massive influx of sodium ions which also shifts the membrane potential.
- The depolarization wave can enter the T-tubules through the cell membrane. Voltage-gated calcium channels open, causing stored calcium ions to be released into the sarcoplasm.
- Troponin molecules on thin filaments are bound by calcium ions. The actin filaments' myosin-binding sites become visible, causing the troponin-tropomyosin complex to change shape. Then, actin and myosin heads join to form cross-bridges, initiating muscle contraction.
- Muscle contraction results from the myofilaments sliding when cross-bridges are produced.
Anatomical Feautures
- Cardiac muscle cells are short and fat
- Intercalated Discs: intercalated discs are made up of desmosomes and gap junctions which are specialized junctions that connect the cells of the heart. The heart can contract in unison due to these structures, which speed up communication among nearby cells.
- Branched Structure: Cardiac muscle cells are branched. This branching improves the electrical and mechanical coupling efficiency by enabling more interaction between cells.
- Single Nucleus: A single (or maximum two), big nucleus is found in the center of each cardiac muscle cell
- Myofibrils: myofibrils are present in cardiac muscle cells; these are made up of sarcomeres. Sarcomeres, are composed of thick and thin filaments ,made of both myosin and actin. Sarcomeres cause striated appearance.
Congestive Heart Failure
When cardiac function declines, the sympathetic nervous system in CHF becomes hyperactive, increasing heart rate and contractility. However, prolonged sympathetic activity might quicken the illness's progression and worsen CHF symptoms.
Congestive heart failure (CGF) is the heart's inability to pump blood effectively. Heart rate and contractility are controlled the sympathetic and parasympathetic nervous systems.
Treatment
- Medication (ACE inhibitors, beta-blockers, diuretics), lifestyle changes (exercise, nutrition), and surgery (heart transplant, pacemaker).
Pathophysiology
- Reduced cardiac output, impaired pumping efficiency, and fluid retention.
- Fluid from pulmonary capillaries is forced into the alveoli by pulmonary congestion, which is a rise in pressure.
- Because the right ventricle is unable to pump blood effectively, systemic congestion results in increased pressure in the systemic veins.
- This causes fluid to build up in the body's tissues and organswhereas,pulmonary congestion directly affects the lungs.
Classifications
- Pulmonary congestion resulting from left ventricular failure is known as left-sided heart failure.
- Symptoms include wheezing, coughing, or shortness of breath
- Failure of the right ventricle resulting in systemic congestion is known as right-sided heart failure.
- Symptoms include edema, buildup of fluid in the stomach or swollen legs
Risk Factors and Causes
- Coronary Artery Disease (CAD): Heart failure occurs due to decreased blood supply to heart muscles from constriction or obstructions in the coronary arteries.
- Hypertension: Constant high blood pressure can put a lot of strain on the heart, making it weaker and eventually fail.
- Previous Heart Attack: Damage to the heart muscle can damage the heart's ability to pump blood effectively.
- Diseases of the Valvular Heart: Dysfunction of valves can lead to stress or excessive volume in the heart, which can result in heart failure.
- Cardiomyopathy: Dilated or hypertrophic cardiomyopathy can damage the cardiac muscle and cause heart failure.
- Genetics, sedentary lifestyle, obesity, and smoking are also risk factors.
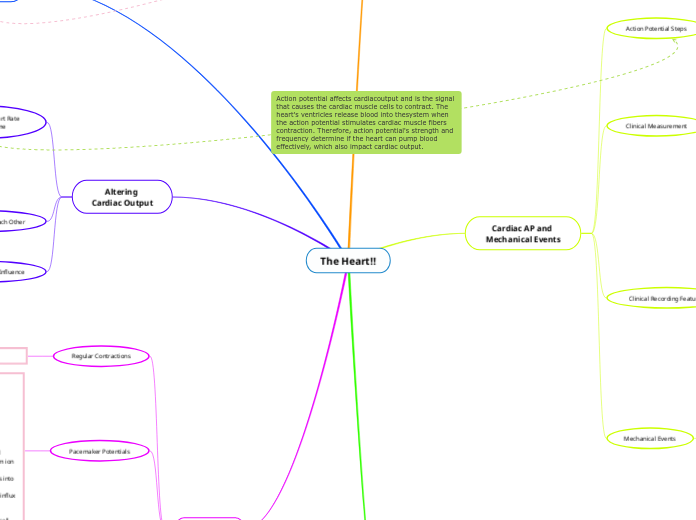
Cardiac AP and Mechanical Events
Mechanical Events
- Systole: The heart's contraction phase, which causes blood to be expelled from the chambers.
- Diastole: The relaxation phase during which blood can enter the chambers.
- Blood is forced into ventricles by atrial contraction, which raises atrial pressure (atrial systole).
- Ventricular contraction raises pressure inside ventricles, causing blood to be ejected into the aorta and pulmonary artery (ventricular systole).
Clinical Recording Features
Electrocardiograms (ECGs) show physiological processes related to heartbeat, such as atrial and ventricular depolarization and repolarization. The ECG waves are indirect indicators of the pressure and volume changes that occur within the heart chambers as a result of these electrical events occurring at the same time as mechanical events such atrial and ventricular contraction.
- Atrial depolarization is represented by the P wave from the SA node
- Ventricular depolarization occurs during the QRS complex
- Ventricular repolarization occurs during the T wave, it is slower than depolarization
- The P-R interval is from the start of atrial excitation to the start of ventricular excitation
- The complete depolarization of the ventricular myocardium occurs during the S-T segment.
- The interval between start of ventricular depolarization and ventricular repolarization is the Q-T interval.
Clinical Measurement
- The electrical activity of the heart is recorded by an electrocardiogram, or ECG.
- Different phases of the cardiac action potential are represented by PQRST waves.
Action Potential Steps
Action potential affects cardiac output and is the signal that causes the cardiac muscle cells to contract. The heart's ventricles release blood into the system when the action potential stimulates cardiac muscle fibers contraction. Therefore, action potential's strength and frequency determine if the heart can pump blood effectively, which also impact cardiac output.
- Phase of rapid depolarization: The influx of sodium via rapid voltage-gated channels.
- Plateau phase: Long-term depolarization is caused by a balance between calcium influx and potassium efflux.
- Phase of repolarization: The membrane potential recovers to resting levels due to potassium efflux.
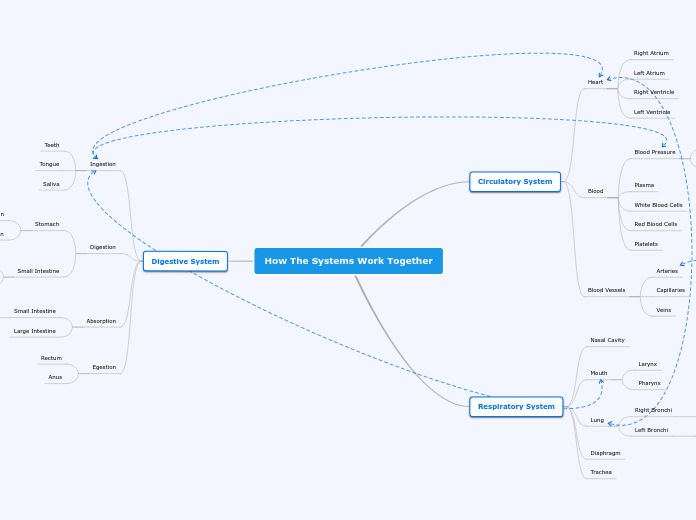
Anatomy and Physiology
Systemic Circuit
oxygenated blood travels from the heart to body tissues and organs
Pulmonary Circuit
deoxygenated blood travels from the heart to lungs to become oxygenated
Coronary Circulation
- The heart muscle receives oxygen-rich blood from the coronary arteries.
- Deoxygenated bloodis taken in by coronary veins and returned to the right atrium.
Valves Structure and Function
c
Layers Around the Heart
Pericardium: double-walled sac that encloses the heart. The fibrous pericardium is the superficial portion of this sac (tough dense connective tissue layer). The serous pericardium is located deep within the fibrous pericardium (thin double layered membrane). Within the fibrous pericardium, its parietal layer borders the surface. The visceral layer continues across the exterior heart surface, connecting major arteries leaving the heart.
Heart Wall: Epicardium (outer layer), myocardium (middle layer), endocardium (inner layer)
Chambers Unique Features
Atria: Receiving chambers with thin walls that receive blood from the lungs (left atrium) and body (right atrium).
Ventricles: Pumping chambers that are muscular and thick-walled that pump blood from the heart to the body (left ventricle) and the lungs (right ventricle).
Blood Pathways
- The right atrium of the heart receives deoxygenated blood through the superior and inferior vena cava
- The tricuspid valve allows blood to pass into the right ventricle.
- Blood is pushed from the right ventricle to the pulmonary valve into the pulmonary artery and ultimately reaching the lungs for oxygenation
- Through the pulmonary veins, oxygenated blood is returned to the heart through the left atrium.
- The mitral valve allows blood to enter the left ventricle.
- Eventually, it is pumped into the aorta via the aortic valve and distributed to the body tissues