PD MedChem
Treatment of Symptoms
- inc DA --> hallucinations and delusions
- muscarinic/NMDA antagonists --> similar ADEs
- 1st: adjust meds w/o worsening PD motor symptoms
"Off" episodes
Istradefylline
-functionalized derivative of caffeine
-antagonist of adenosine A2a receptors
-potentiate the antiparkinsonian action of L-dopa
-useful in reducing "off" eps b/w doses
-dose adjust req w/ strong CYP3A4 inhibitors + impaired hepatic function
-CI w/ CYP3A4 inducers
-cause/exacerbate LIDs + psychosis
Hallucinations/Delusions
Pimavanserin: agonist of 5-HT, FDA for
hallucinations/delusions in PD pts
Metabolized by CYP3A4, strong inhibitors and inducers affect exposure
Prolongs QT interval --> avoid in pts at risk for cardiac arrhythmias
Atypical antipsychotics (2nd gen):
clozapine or quetiapine
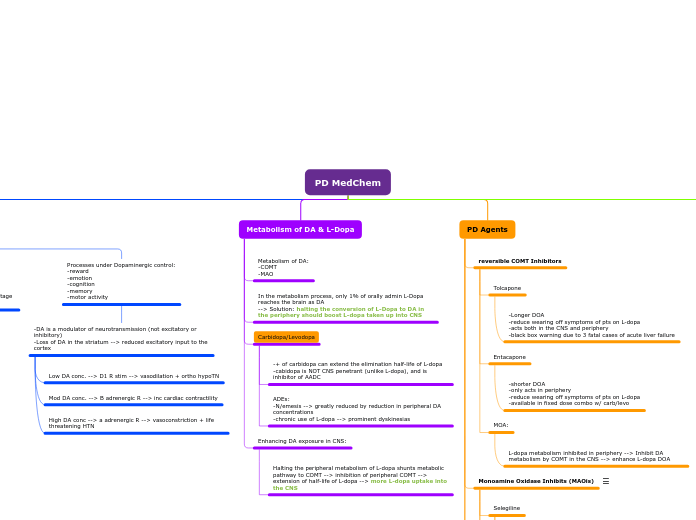
PD Agents
N-methyl-D-aspartate receptor
- Overactive glutamate transmission = L-dopa induced dyskinesias (LIDs)
- Excessive glutamate --> excitotoxicity
- NMDA is an ion channel found in nerve cells
- Amantadine an NMDA antagonists --> txt of LIDs in PD pts
- NMDA antagonists (PCP, ketamine) --> psychotomimetic effects
Amantadine
-NMDA antagonists
-treats L-dopa induced dyskinesias (LIDs) in PD pts
-similar in SAR to Alzheimer's drug memantine
-basic amine, protonated at physiologic pH
-lipophilic cage --> CNS entry
-ADEs: confusion, hallucinations
Muscarinic Acetylcholine Receptors
- Family of CGRPs that respond to the binding of ACh
- Dopamine and ACh have a reciprocal rs in the nigrostriatal dopamine pathway
- Normally dopamine suppresses cholinergic activity
- Removal of dopamine --> inc in ACh activity --> extrapyramidal symptoms (EPS) --> tremors experienced by PD pts
- Antagonists of muscarinic ACh receptors offer potential therapeutic benefit
- SAR: Similar to antihistamine disphenhydramine
- Most serious ADEs: sedation + mental confusion
Trihexphenidyl, benztropine
Dopamine Receptor Agonists
- neurodegeneration occurs w/ progressive PD --> fewer striatal nerve terminals available to decarboxylate L-dopa
- Solution: drugs that are CNS penetrant + directly stimulate DA receptors
- DA RA: longer DOA vs. L-dopa --> less likely to induce on/off effects/dyskinesias
- Other ADEs are inc relative to L-dopa, incl N/V, sedation, vivid dreaming and hallucination
- RA = receptor agonist
Non-ergot DA Receptor agonists
Rotigotine
-New D1/2/3 agonist delivered as transdermal path to provide 24hr coverage
-NOT affected by hepatic/renal/CYP-mediated so DDI are not sig
Ropinirole
-agonists of all D2 Rs and among the most commonly prescribed direct DA RA for PD
-metabolized by CYP1A2
Pramipexole
-agonists of all D2 Rs and among the most commonly prescribed direct DA RA for PD
Ergot Alkaloid
- Non-selective (5HT + adrenergic R activity)
- carry risk for serious cardiac complications
- newer non-ergot DA RA are generally safer alts
Cabergoline
-full D2 agonist + partial agonist at D3/4 w/ long half-life (48hrs)
Bromocriptine
-partial agonist at D2/3
-1st direct DA RA used in the txt of PD
Monoamine Oxidase Inhibits (MAOis)
- MAO-A/B both capable of oxidizing DA
- Long-acting, Irreversible, non-selective inhibitors of MAO-A/B are CI w/ L-dopa due to the risk of inducing hypertensive crises (cheese effect)
- SELECTIVE inhibitors are required***
- Ex of non-selective: phenelzine or tranylcypromine
Safinamide
-Modulate dopaminergic & glutamanergic signaling via multiple mechanisms:
-MAO-B inhibition (reversible, 1000x selective for MAO-B)
-modulation of certain Na/K channels
-use: reduce "off" time and extend "on" time without dyskinesias in pts taking carb/levo
-no effect on BP/HR
-CI w/ certain antidepressants due to risk of serotonin syndrome
-Metabolism: non-p450 mediated
Rasagiline
-Class/MOA same as above
-DOES NOT produce amphetamine metabolites
Selegiline
CYP-mediated N-dealkylation produces amphetamine metabolites --> POTENT vasoconstrictors
-Selective** irreversible inhibitor of MAO-B
-SAR: terminal alkyne is the functional group that forms the covalent bond w/ protein
reversible COMT Inhibitors
MOA:
L-dopa metabolism inhibited in periphery --> Inhibit DA metabolism by COMT in the CNS --> enhance L-dopa DOA
Entacapone
-shorter DOA
-only acts in periphery
-reduce wearing off symptoms of pts on L-dopa
-available in fixed dose combo w/ carb/levo
Tolcapone
-Longer DOA
-reduce wearing off symptoms of pts on L-dopa
-acts both in the CNS and periphery
-black box warning due to 3 fatal cases of acute liver failure
Metabolism of DA & L-Dopa
Enhancing DA exposure in CNS:
Halting the peripheral metabolism of L-dopa shunts metabolic pathway to COMT --> inhibition of peripheral COMT --> extension of half-life of L-dopa --> more L-dopa uptake into the CNS
Carbidopa/Levodopa
ADEs:
-N/emesis --> greatly reduced by reduction in peripheral DA concentrations
-chronic use of L-dopa --> prominent dyskinesias
-+ of carbidopa can extend the elimination half-life of L-dopa
-cabidopa is NOT CNS penetrant (unlike L-dopa), and is inhibitor of AADC
In the metabolism process, only 1% of orally admin L-Dopa reaches the brain as DA
--> Solution: halting the conversion of L-Dopa to DA in the periphery should boost L-dopa taken up into CNS
Metabolism of DA:
-COMT
-MAO
Dopamine Receptors
In the basal ganglia circuitry, there are 2 pathways from the cortex: direct & indirect.
- Direct enables movement
- Indirect inhibits movement
Processes under Dopaminergic control:
-reward
-emotion
-cognition
-memory
-motor activity
-DA is a modulator of neurotransmission (not excitatory or inhibitory)
-Loss of DA in the striatum --> reduced excitatory input to the cortex
High DA conc --> a adrenergic R --> vasoconstriction + life threatening HTN
Mod DA conc. --> B adrenergic R --> inc cardiac contractility
Low DA conc. --> D1 R stim --> vasodilation + ortho hypoTN
Inhibitory D2 (D2, D3, & D4)
Coupled to Gi/o, decrease cAMP, inc K current and dec voltage gated Ca currents
Excitatory: D1 type (D1 & D5)
Coupled to Ga2, activating the cyclic AMP-PKA pathway
Subtopic