par Wagle Prathana Il y a 10 mois
50
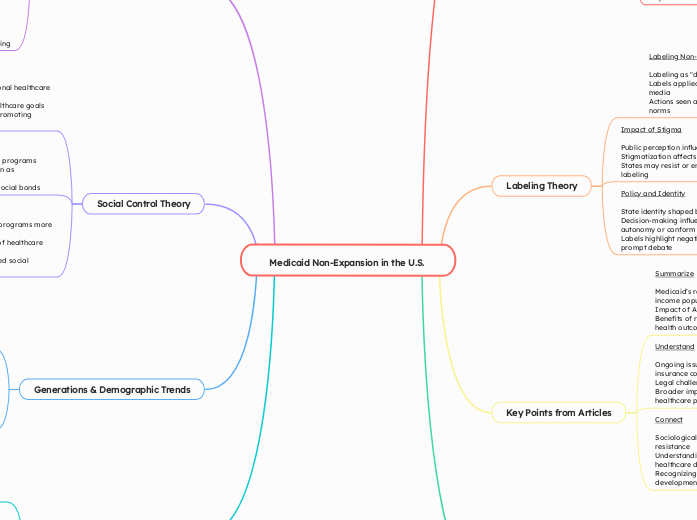
Medicaid Non-Expansion in the U.S.
The decision of some U.S. states to not expand Medicaid is influenced by various factors, including administrative challenges, financial concerns, and ideological opposition. Administrative hurdles involve the complexity of program management and increased bureaucratic demands, while financial concerns revolve around the long-term costs and budgetary impacts on the state.